Circulation 1: Arterial and Venous Supply
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
What is allowed to cross and not cross across the Blood Brain Barrier?
The BBB is selectively permeable
→ lipid soluble substances can readily enter via diffusion
→ glucose and amino acids cross slowly by carrier mediated transport
→ Lipid insolube/polar substances are restricted
What are the three structures that form the Blood Brain Barrier? How do you know if these structures are damaged
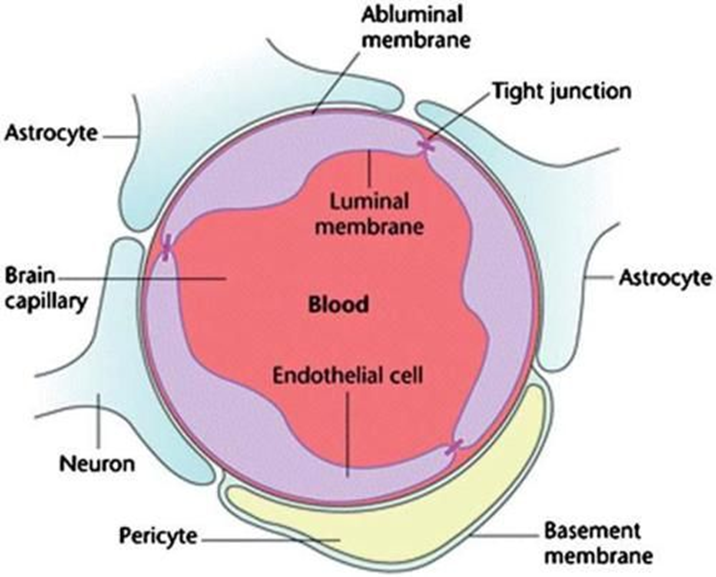
The BBB is formed by three main structures
→ Capillaries are lined by non-fenestrated endothelial cells with tight junctions
→ Basement Membrane
→ Astrocytes, a glial cell of the brain, have their foot processes wrap vessels to help form the barrier
A lesion to the blood brain barrier can result in increase in contrast in the brain following administration of contrast
Where in the brain is the Blood Brain Barrier absent?
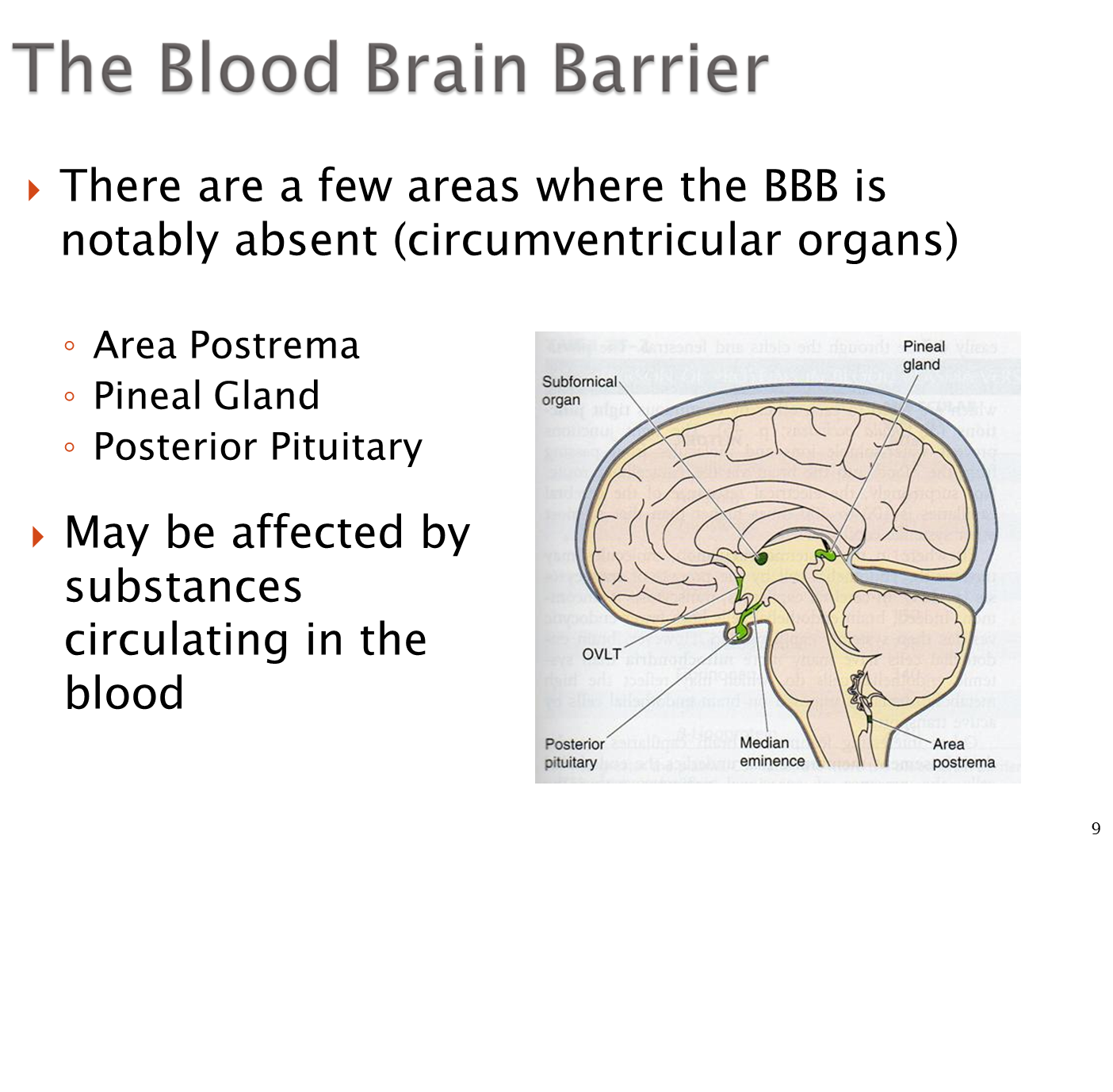
There are three major areas of the brain where the blood brain barrier is absent
→ Area Postrema - chemoreceptor trigger zone or the area responsible for vomiting, absent in order to sample toxins in the blood
→ Pineal Gland
→ Posterior Pituitary
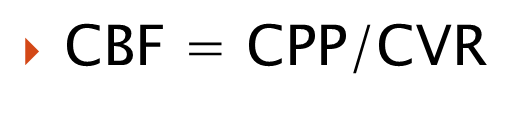
What is the equation for cerebral perfusion pressure? Cerebral blood flow?
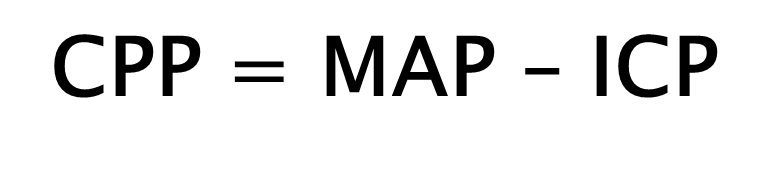
1) Cerebral Perfusion Pressure is equivalent to mean arterial pressure and intracranial pressure
→ CPP is the pressure gradient driving blood into the brain tissue
2) Cerebral blood flow is the actual volume of blood passing through the brain per unit time and is affected via autoregulation
→ calculated as cerebral perfusion pressure/cerebral vascular resistance
→ our body can autoregulate the cerebral vascular resistance in order to maintain a consistent cerebral blood flow
How does our body autoregulate cerebral vascular resistance?
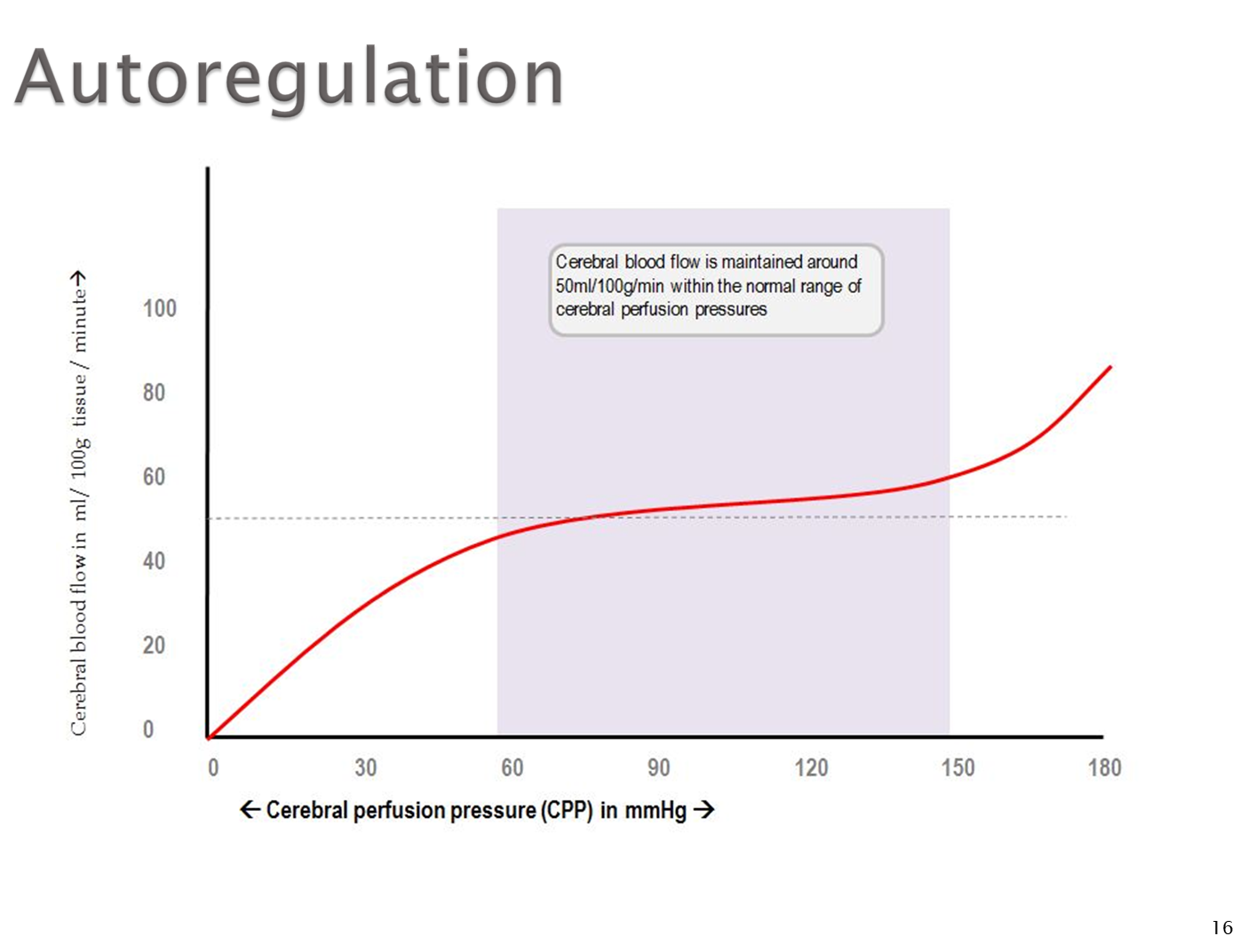
Autoregulation of cerebral vascular resistance allows us to maintain a constant cerebral blood flow. The major thing our body does is change vessel diameter
1) Dilation leads to increased blood flow while constriction leads to decreased blood flow
2) pCO2 is a major determinant of cerebral perfusion
→ when pCO2 is high, there is vasodilation to increase cerebral blood flow
→ when pCO2 is low, there is vasoconstriction to decrease cerebral blood flow
How does autoregulatory curves shift for cerebral blood flow?
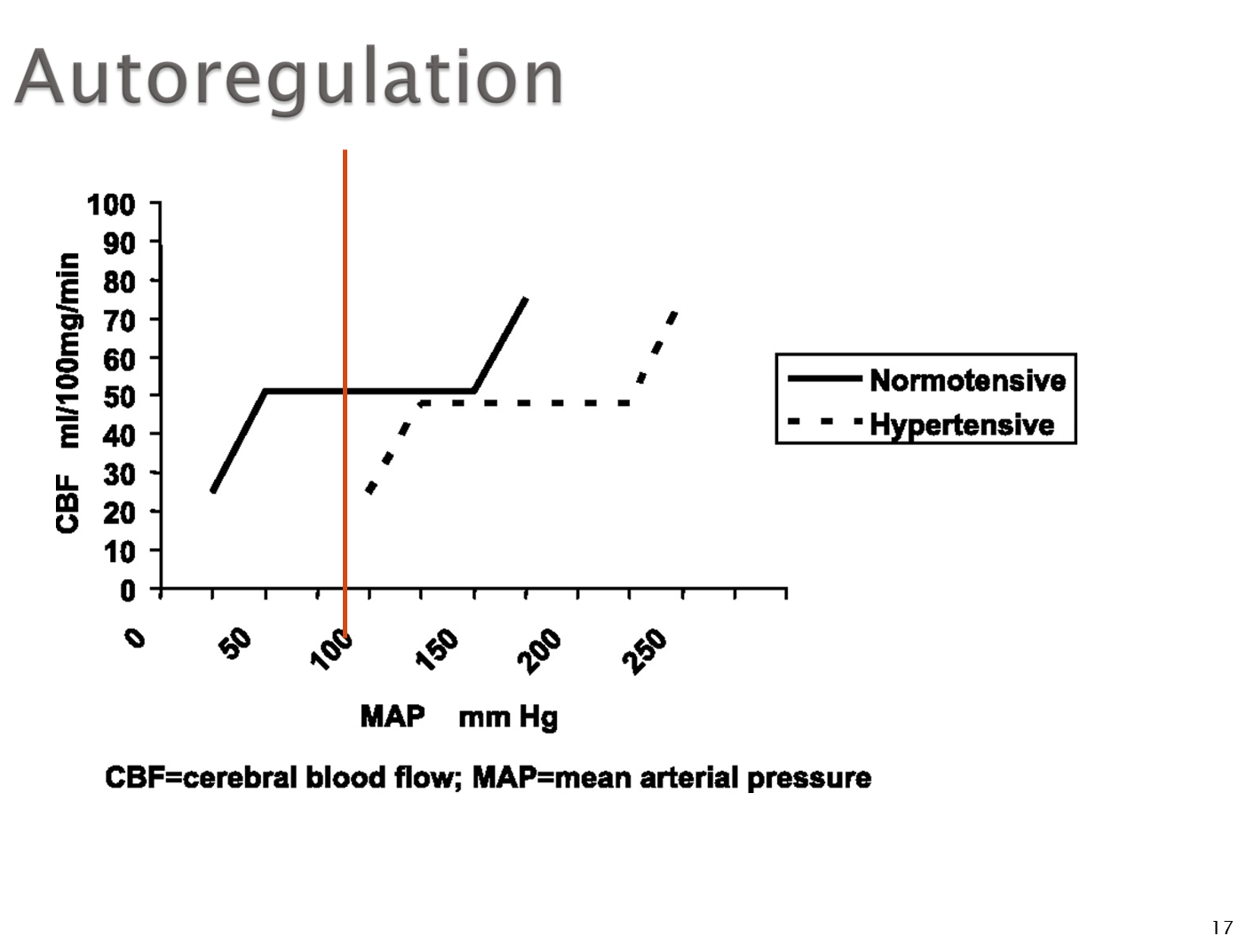
Patients who are chronically hypertensive will have a shift in their autoregulation curve to the right
1) patients with high blood pressure will have a body that is used to a higher cerebral blood flow than other patients
→ if you were to drop the hypertensive patient’s mean arterial pressure you can affect their cerebral blood flow
What is the Extracranial Vascular Supply?
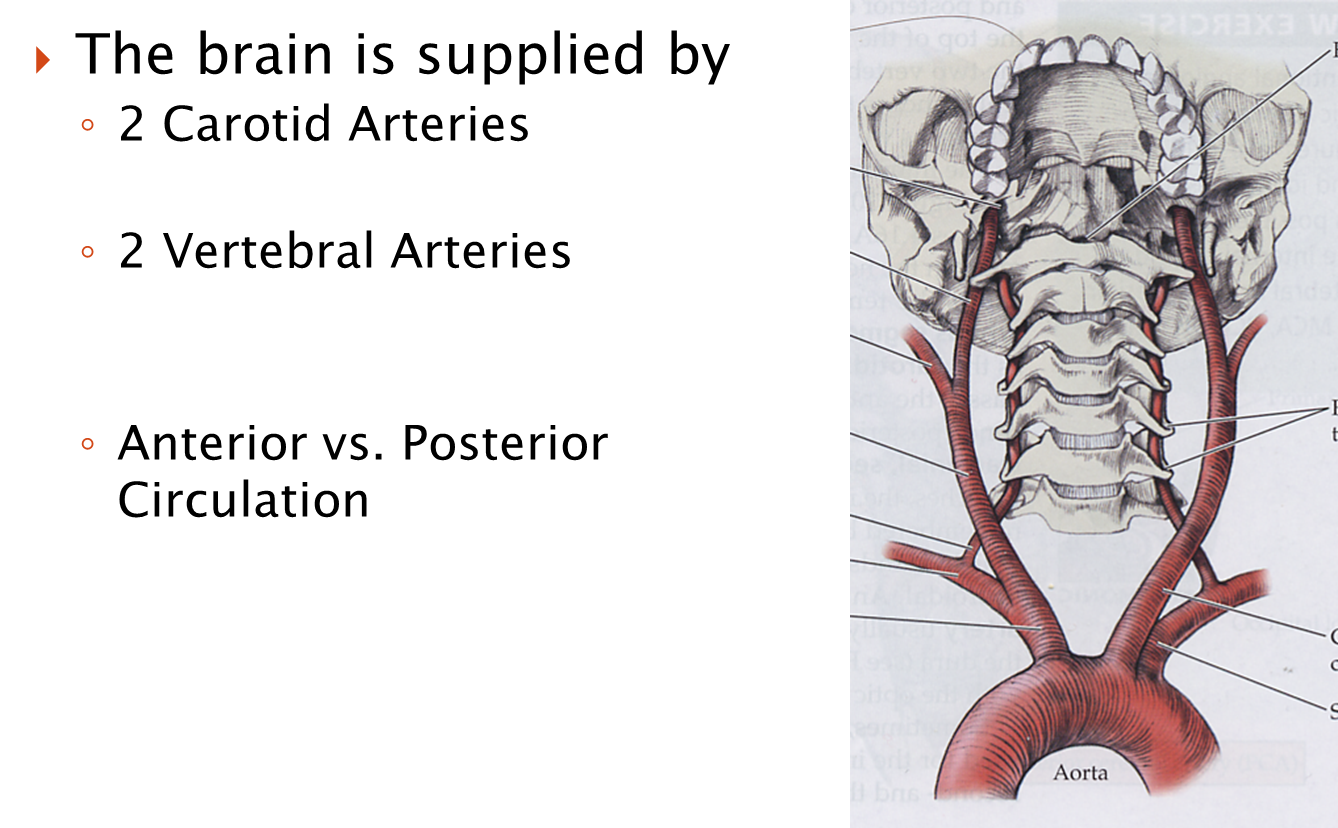
The brain is supplied by four major vessels
1) 2 Carotid Arteries
→ the right common carotid branches off the brachiocephalic trunk while the left common carotid branches directly off the aortic arch
→ these carotids will ascend to the level of C3-C4 where they branch into the internal and external carotids. Importantly the internal carotid will not branch
→ external carotid will make eight major branches
2) 2 Vertebral Arteries
→ vertebral arteries are branches of the subclavian arteries where they travel through the transverse foramen of the cervical vertebrae
→ around C2 they enter the foramen magnum
What is the Circle of Willis?
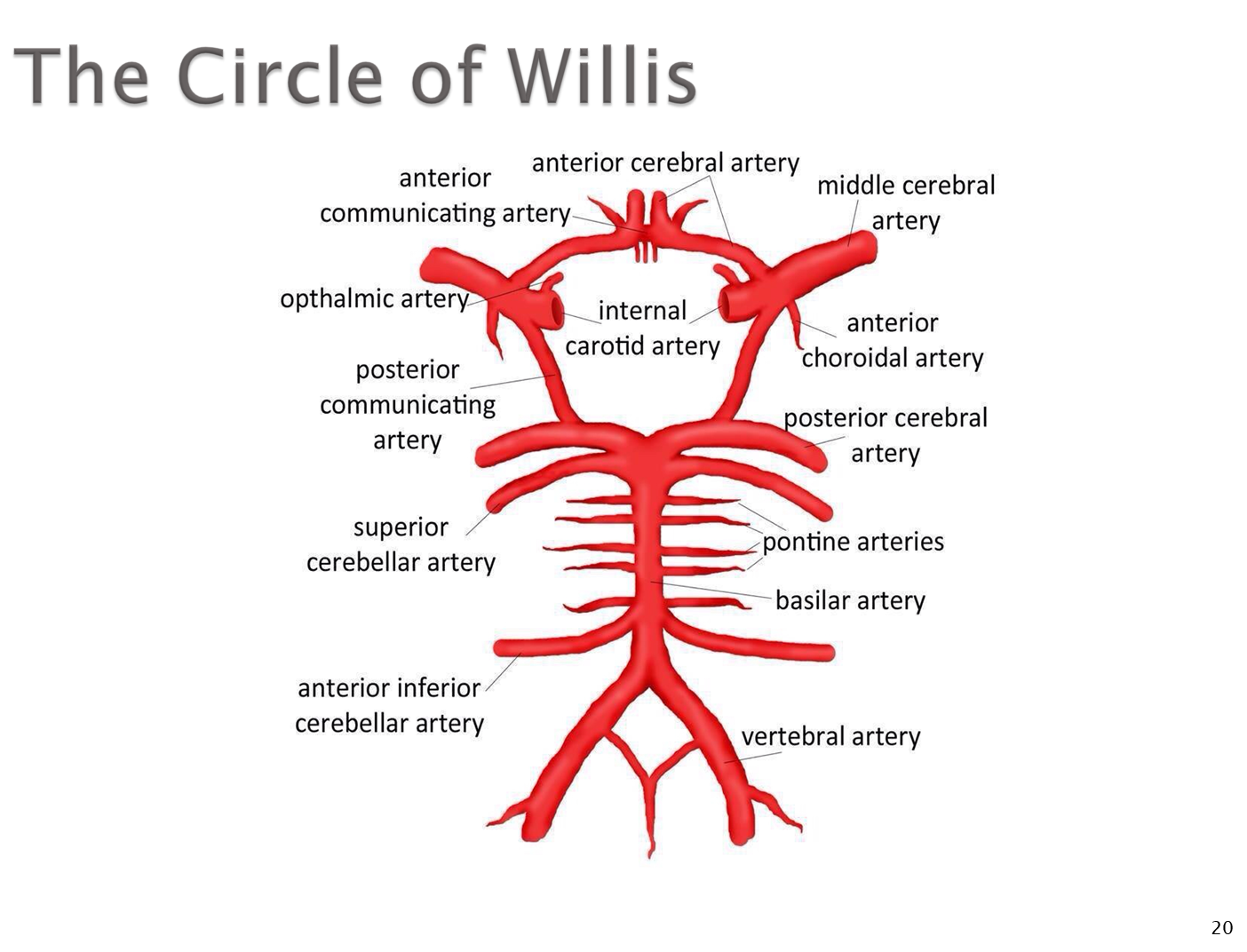
The internal carotid arteries and vertebral arteries will form the Circle of Willis in the brain
1) The internal carotid arteries will form the anterior circulation
→ will divide into the anterior cerebral artery (ACA) and middle cerebral arteries
→ the ACA and MCA are connected to one another via ACOMM or anterior communicating arteries
2) the vertebral arteries will form the posterior circulation
→ the vertebral arteries will branch to form PICA or posterior inferior cerebellar arteries
→ the two vertebral arteries will fuse together to form a single basilary artery at the level of the pons. Here they will immediately form the anterior inferior cerebellar artery (AICA)
→ the basilary artery will divide into the two sets each of the superior cerebellar arteries and posterior cerebral arteries
3) the basilary artery will connect to the internal carotids via the posterior communicating arteries
What happens to the Anterior Cerebral Artery?
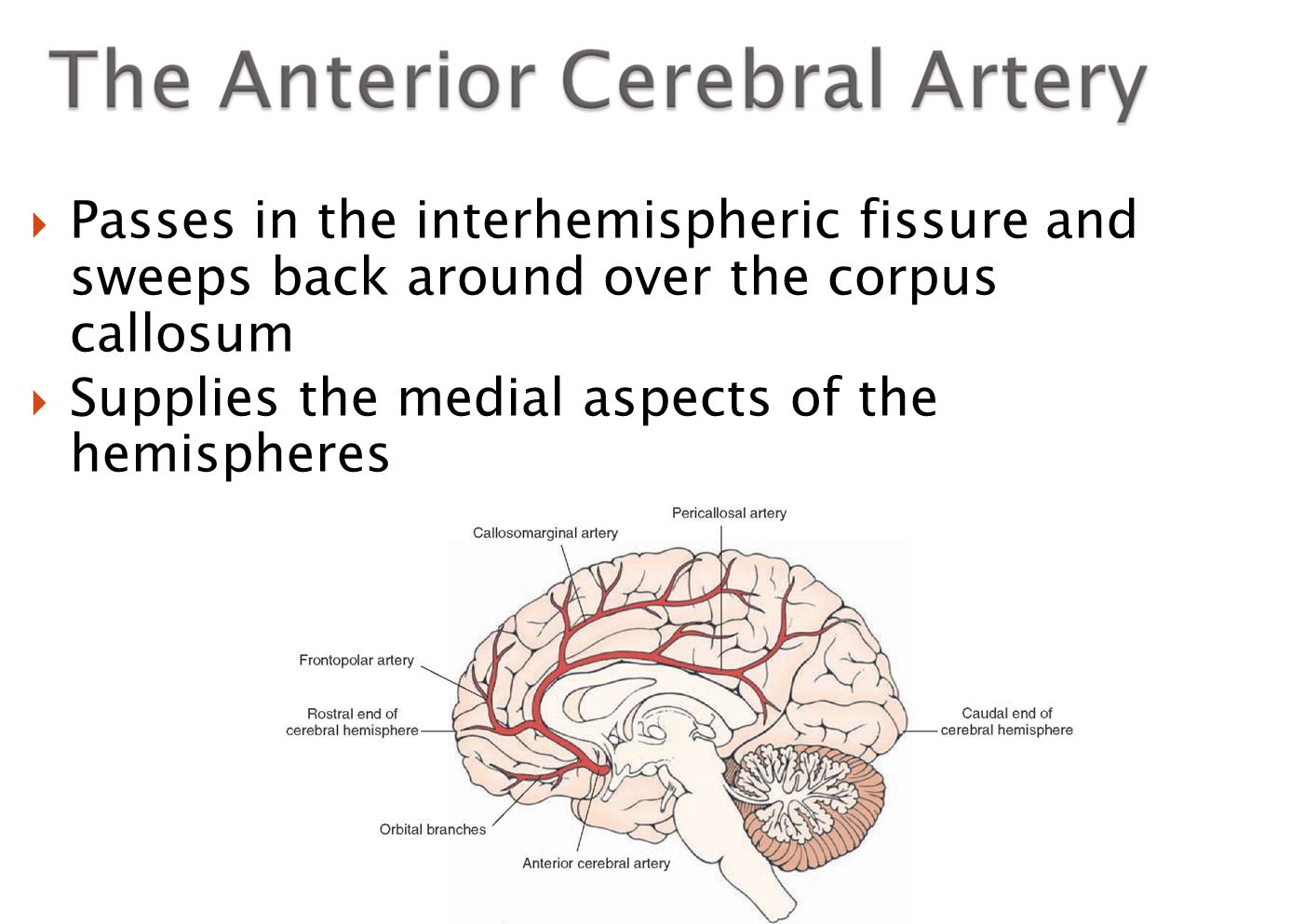
The Anterior Cerebral artery will pass on either side of the falx cerebri and sweeps around over the corpus callosum
→ supplies the medial aspects of the hemispheres
What happens to the Middle Cerebral Artery
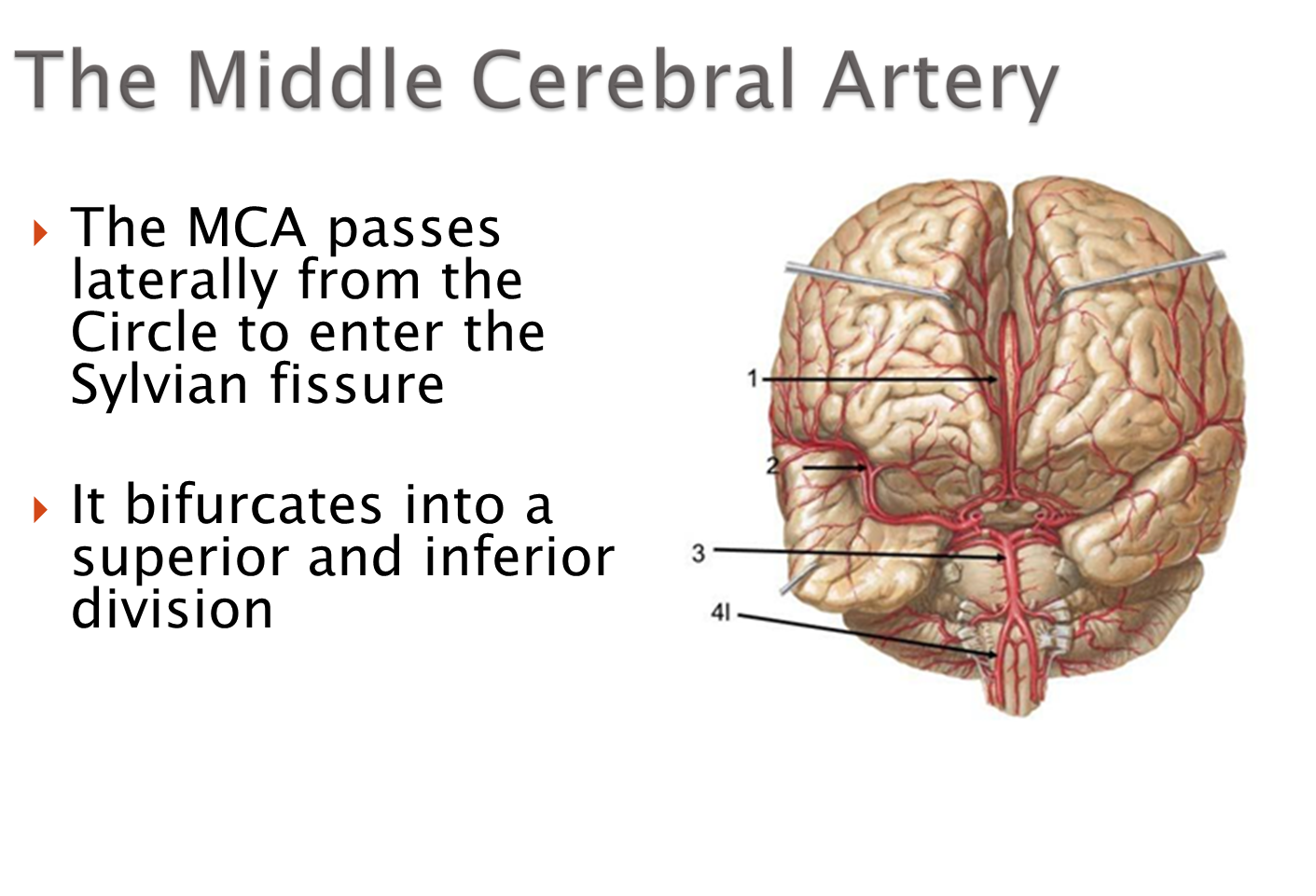
The middle cerebral arteries passes through the Sylvian Fissure/Lateral Fissure where it bifurcates into a superior and inferior division
What happens to the Posterior Cerebral Arteries?
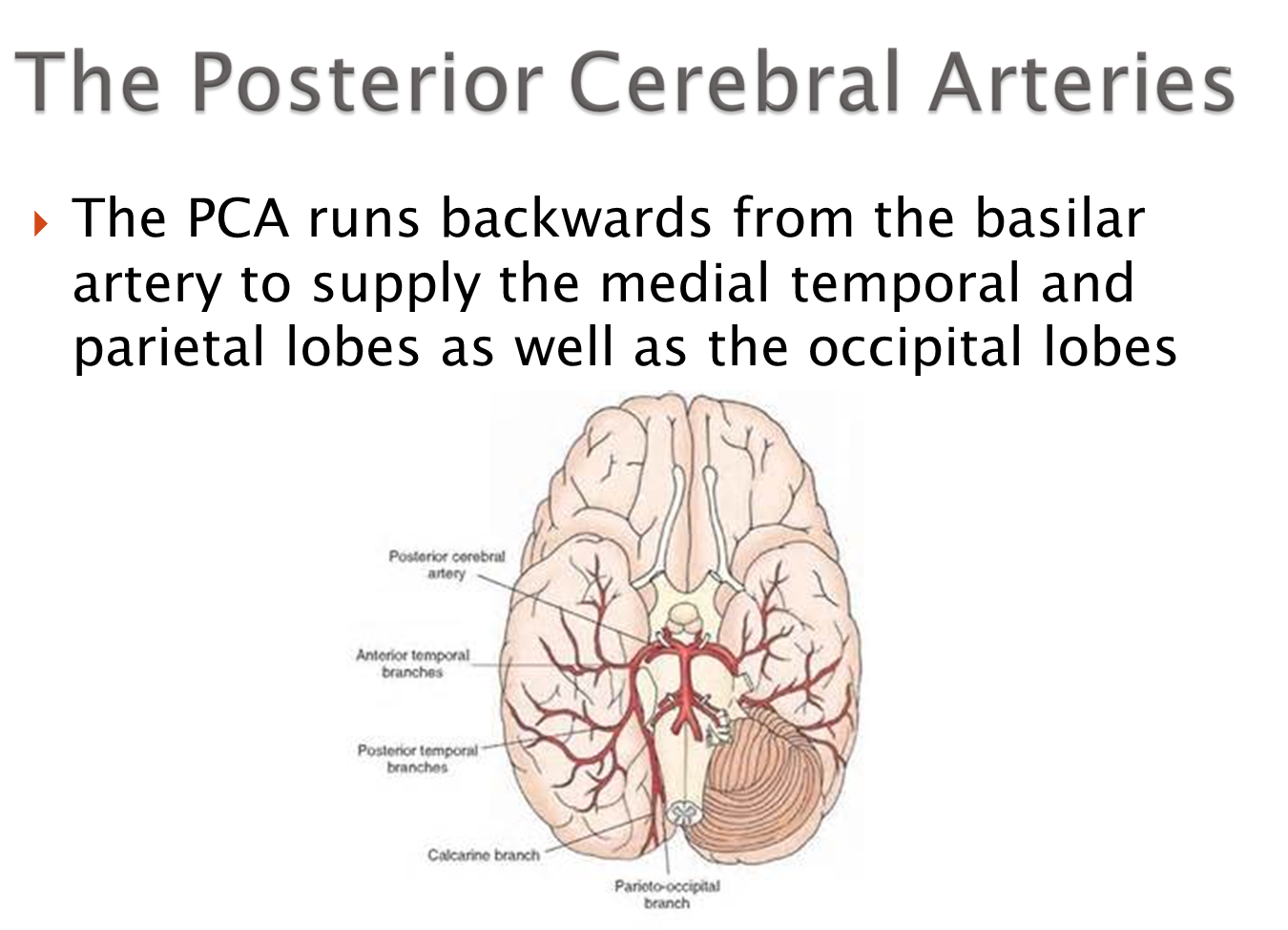
The PCA runs backwards to supply the medial temporal and parietal lobes and occipital lobs
What are the Deep Penetrating Vessels?
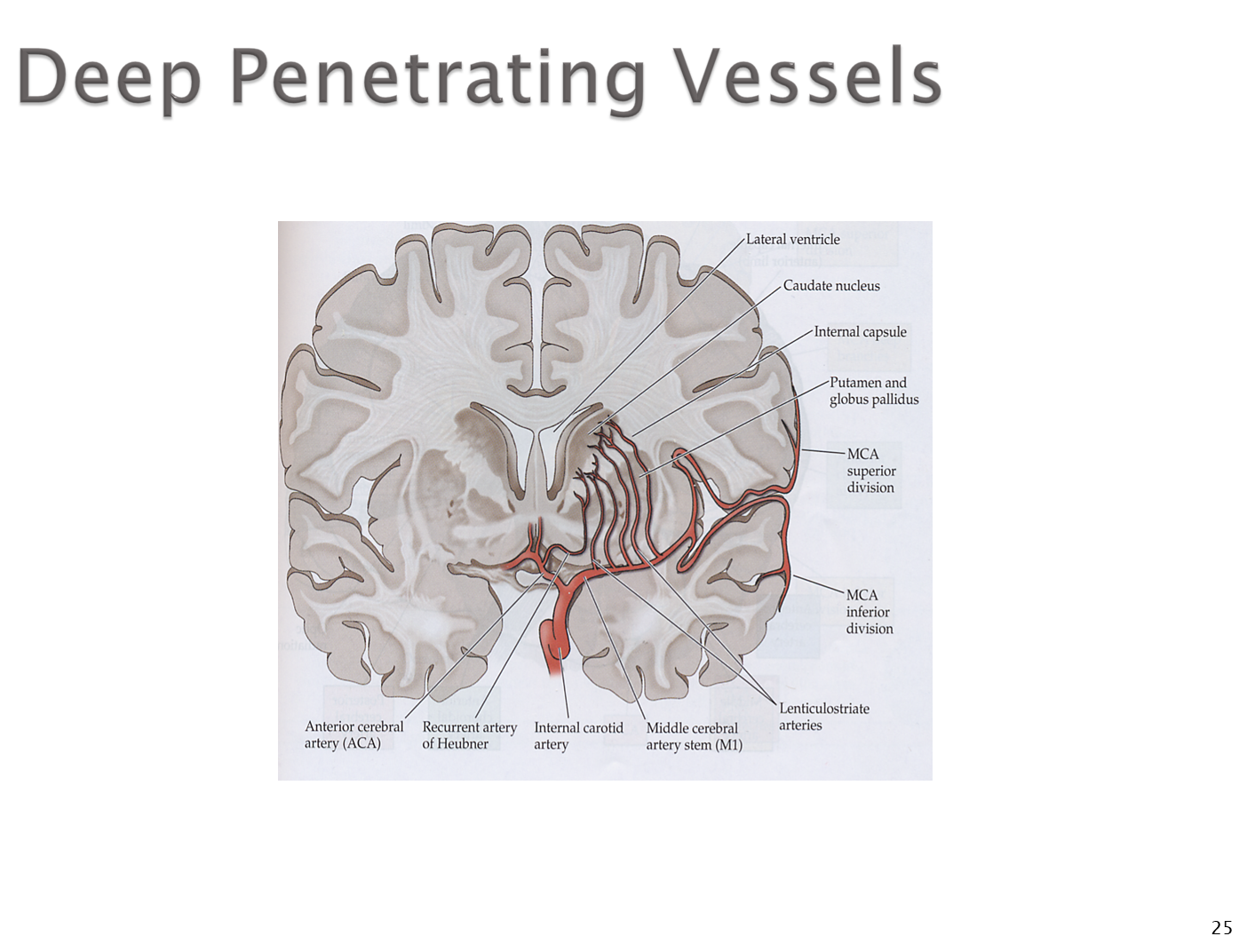
Deep Penetrating Vessels or lenticulostriate arteries will be small branches that branch off the main arteries from the Circle of Willis
Describe the Venous Anatomy of the brain
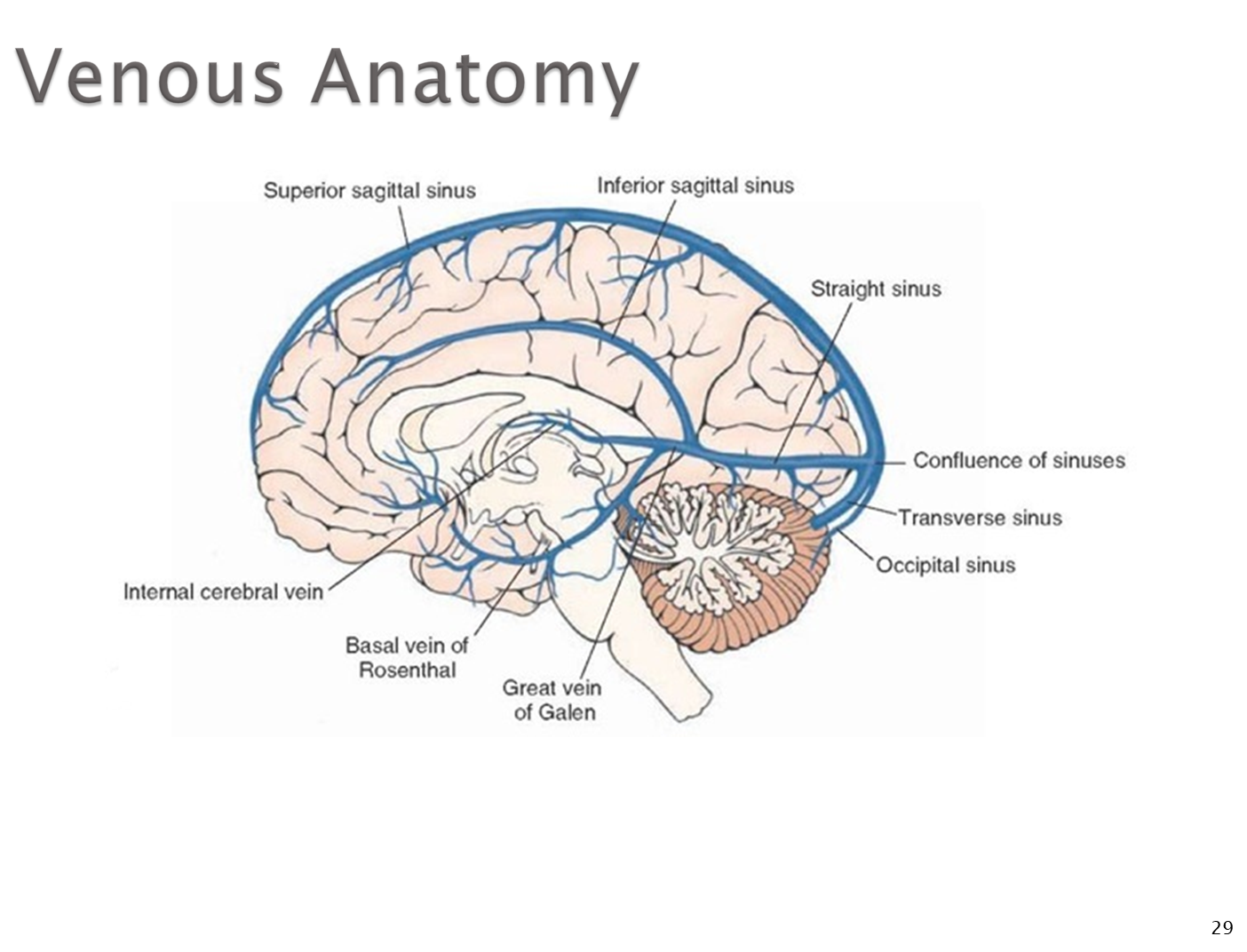
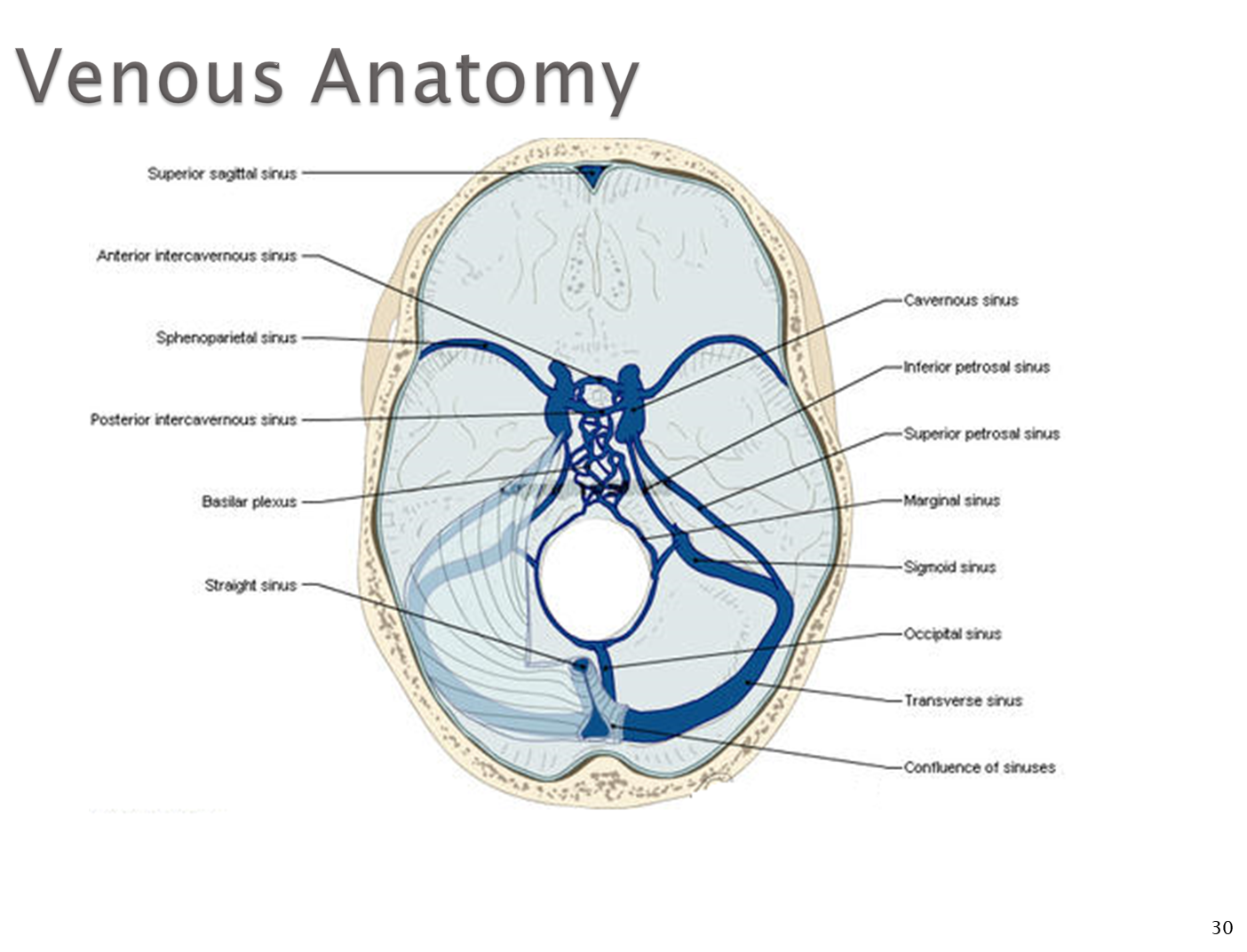
1) Running along the superior margin of the falx cerebri is the superior sagittal sinus
→ running along the inferior margin of the falx cerebri is the inferior sagittal sinus
→ these two are connected via the straight sinus which collects venous blood from other parts of the brain, especially the Vein of Galen which drains the deep brain tissue into the straight sinus
2) Blood flow out of the brain will collect in the confluence of sinuses where it will then flow out via the transverse sinus to the sigmoid sinus
→ the sigmoid sinus passes into the jugular vein which passes out via the jugular foramen
→ the jugular vein passes through along with CN 9-11 through the foramen
What is the Cavernous Sinus?
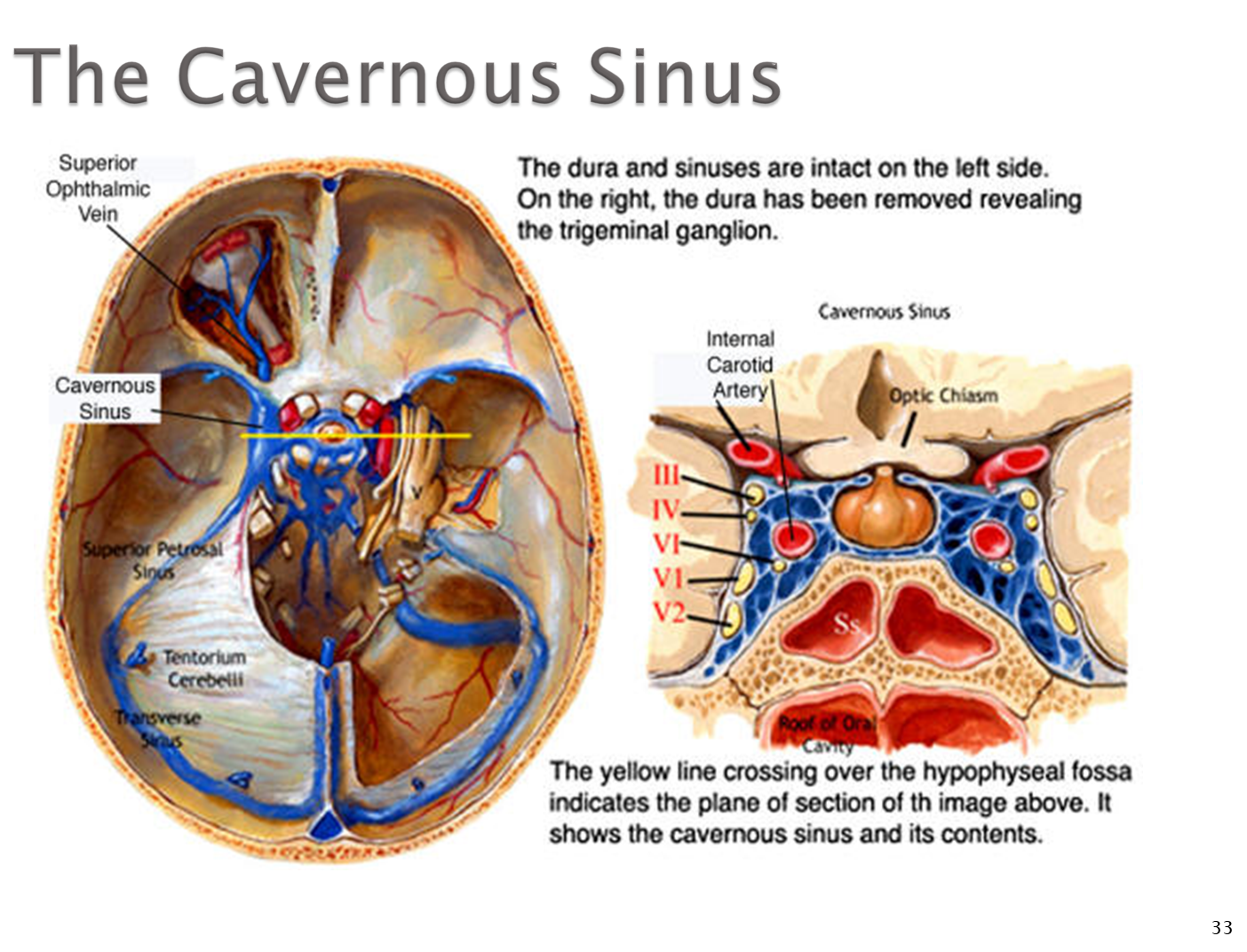
Cavernous Sinus is a collection of venous sinuses that lay around the sella turcica where the pituitary gland sits
1) many nerves and vessels will pass through the cavernous sinus
→ CN III, IV, V1 and V2, VI, and the sympathetic plexus from the thoracic and lumbar areas that wraps around the carotid artery
→ the Internal carotid artery will also pass through here
2) Cavernous Sinus Syndrome can back up blood flow causing the eye to protrude outward
→ can cause cranial nerve dysfunction for any cranial nerve exiting the cavernous sinus
What are Vascular Territories?
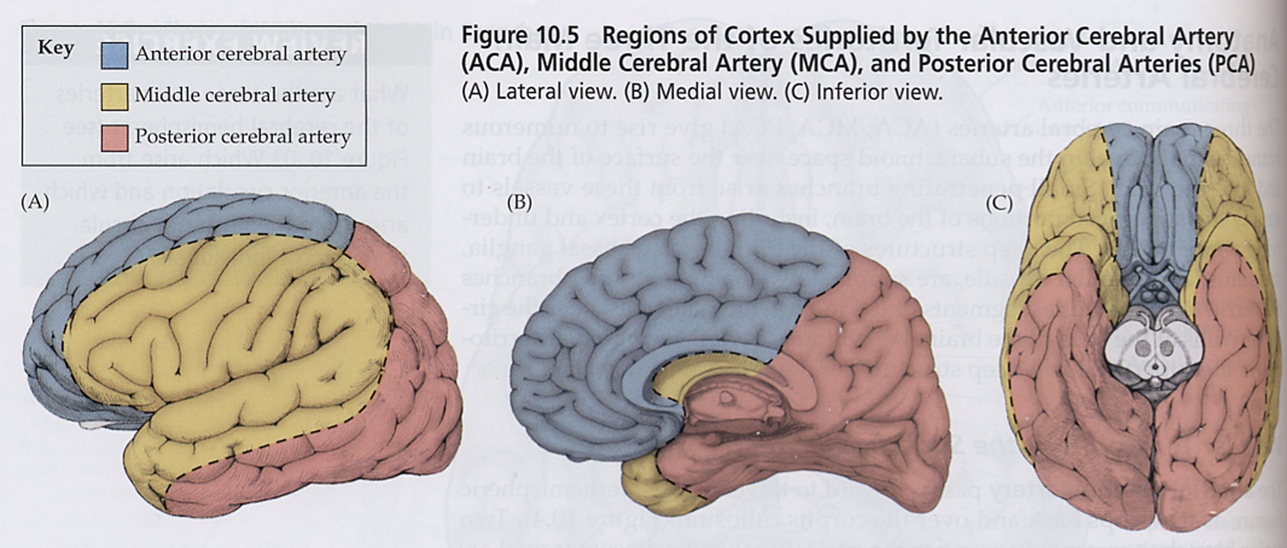
Vascular territories are regions of the brain supplied by a specific blood vessel
→ because of this, interruption of blood flow in a specific vessel typically presents the same regardless of person
What are the ACA Territory Symptoms?
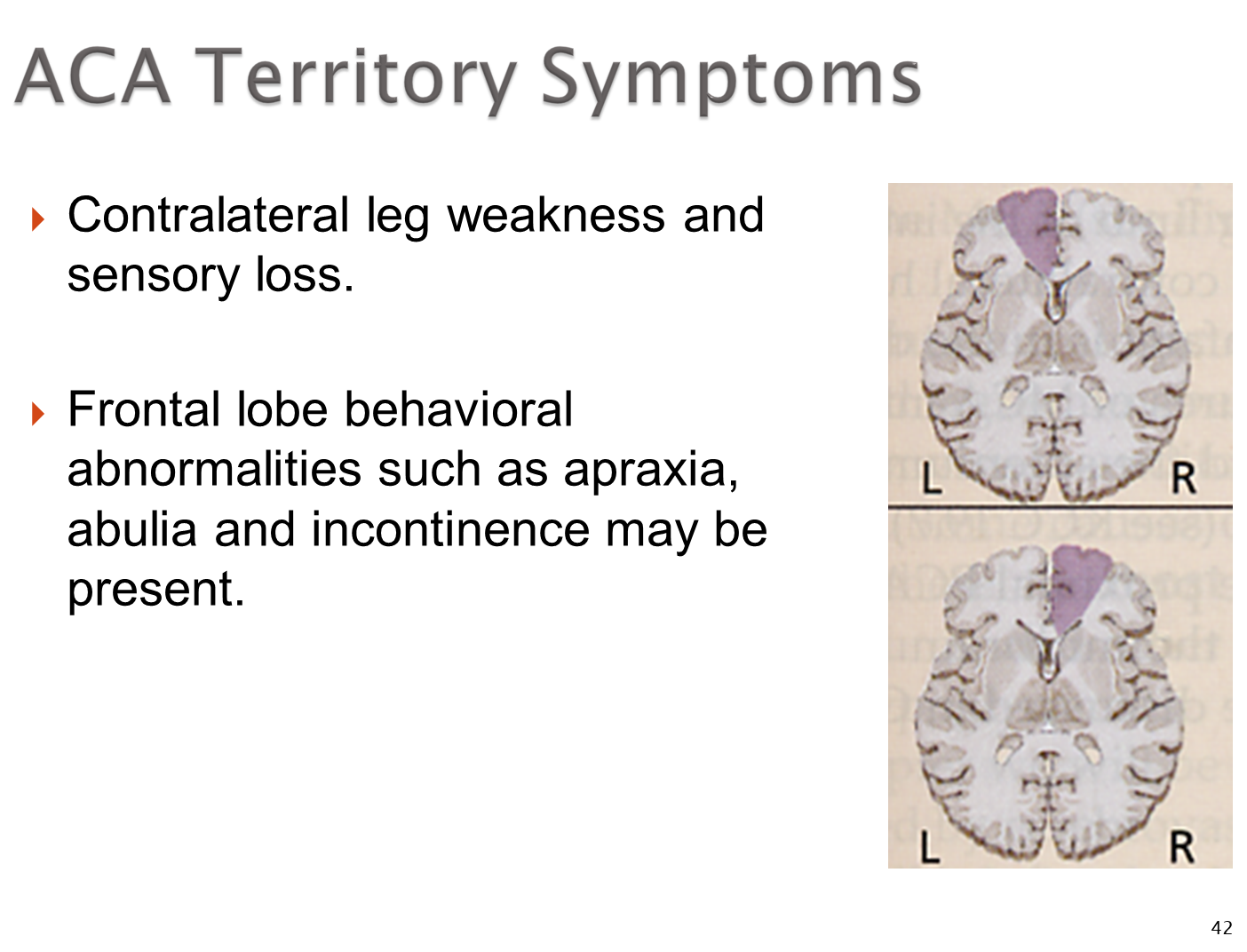
Having a stroke in the ACA will cause two major symptoms:
→ contralateral leg weakness and sensory loss
→ frontal lobe behavioral abnormalities such as apraxia and abulia
What are the MCA Territory Symptoms (Dominant vs Non-Dominant)
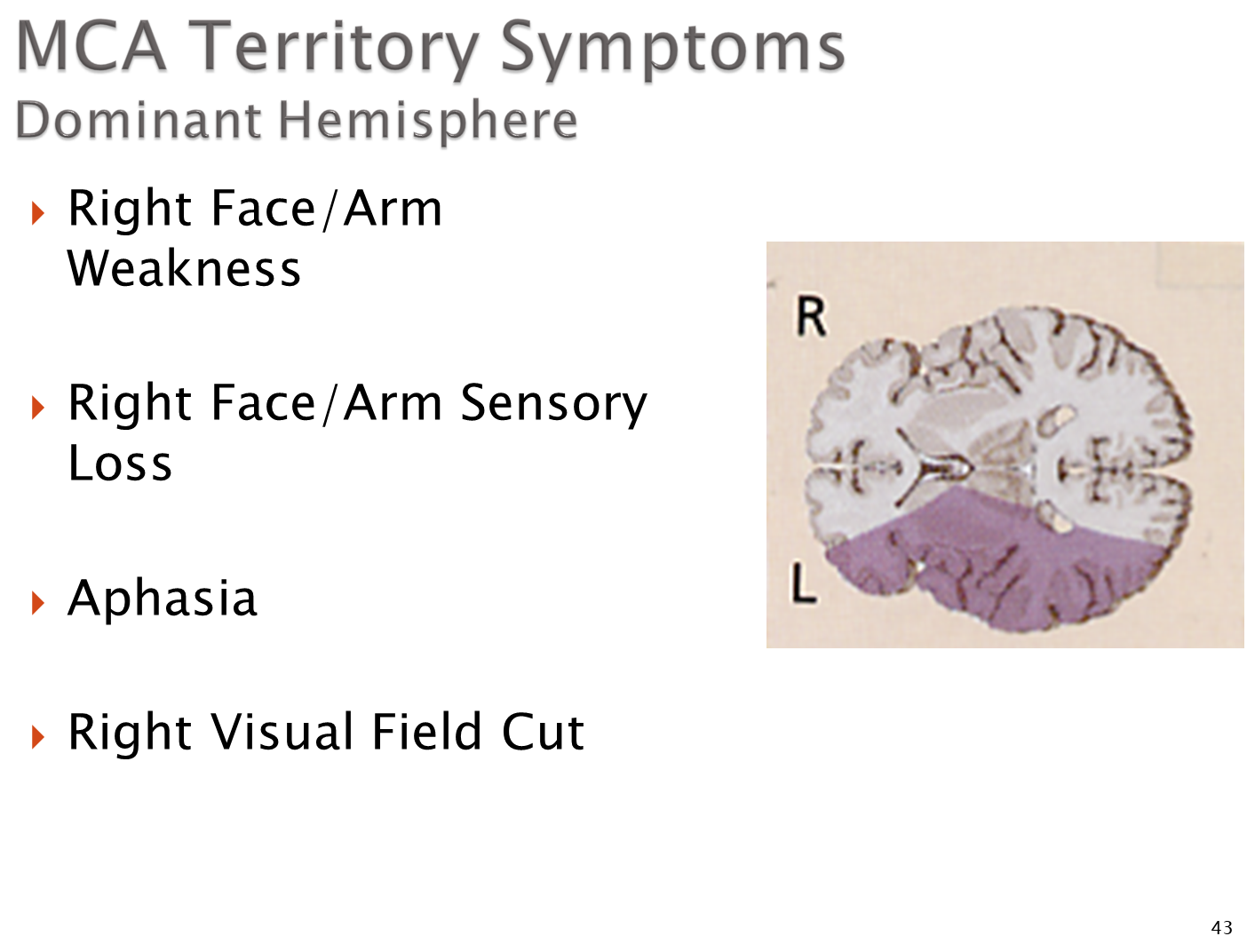
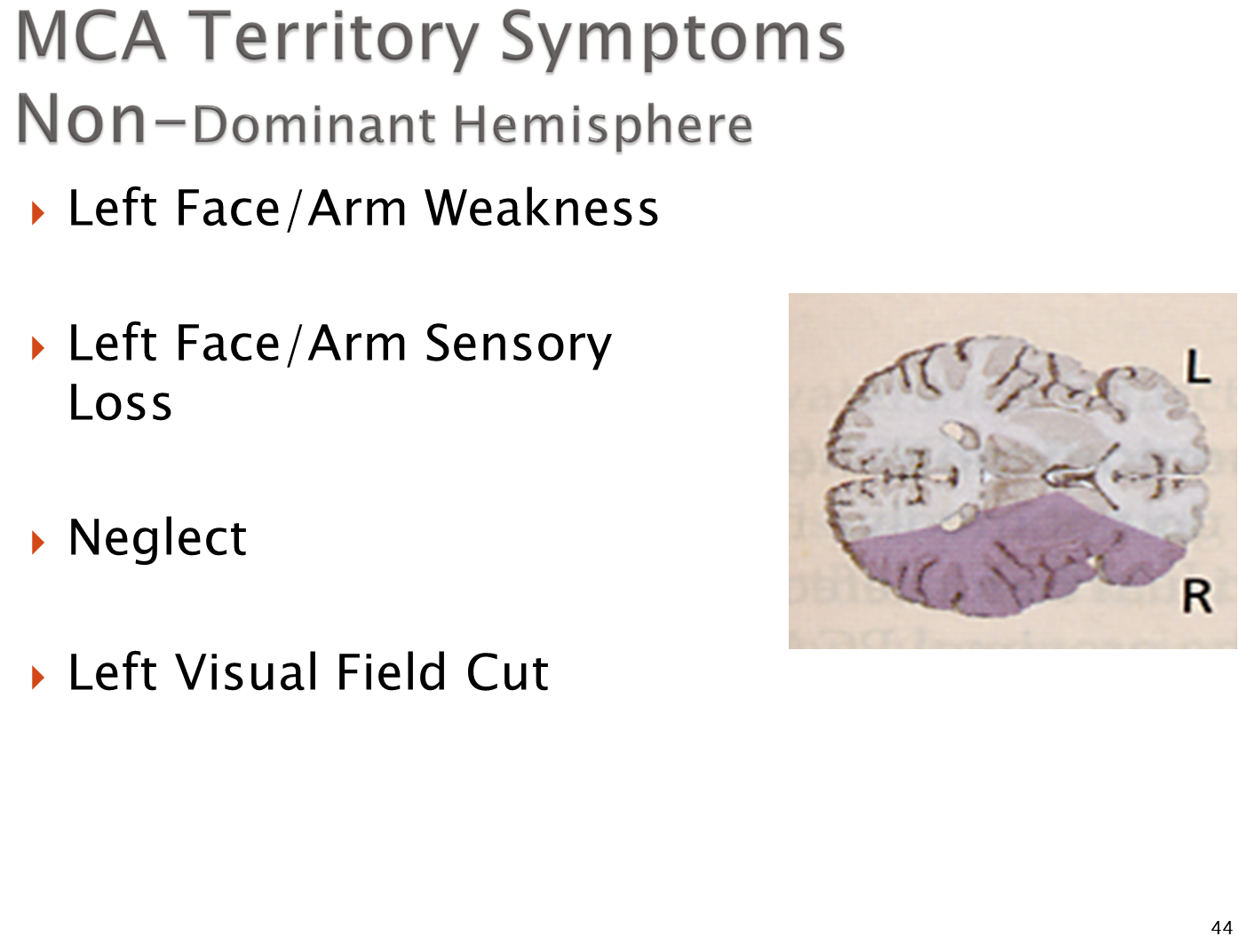
The MCA provides blood to the what is characterized as the dominant vs non-dominant hemispheres
1) Dominant - hemisphere for language which will be typically be the left side of the brain
→ right face/arm weakness
→ right face/arm sensory loss
→ aphasia - inability to communicate
→ right visual field deficit
2) Non-dominant - hemisphere on the opposite side used in spatial awareness and attention
→ left face/arm weakness and sensory loss
→ neglect - where the brain has no awareness of the non-dominant side of the body
→ left visual field cut
What are PCA Territory Symptoms
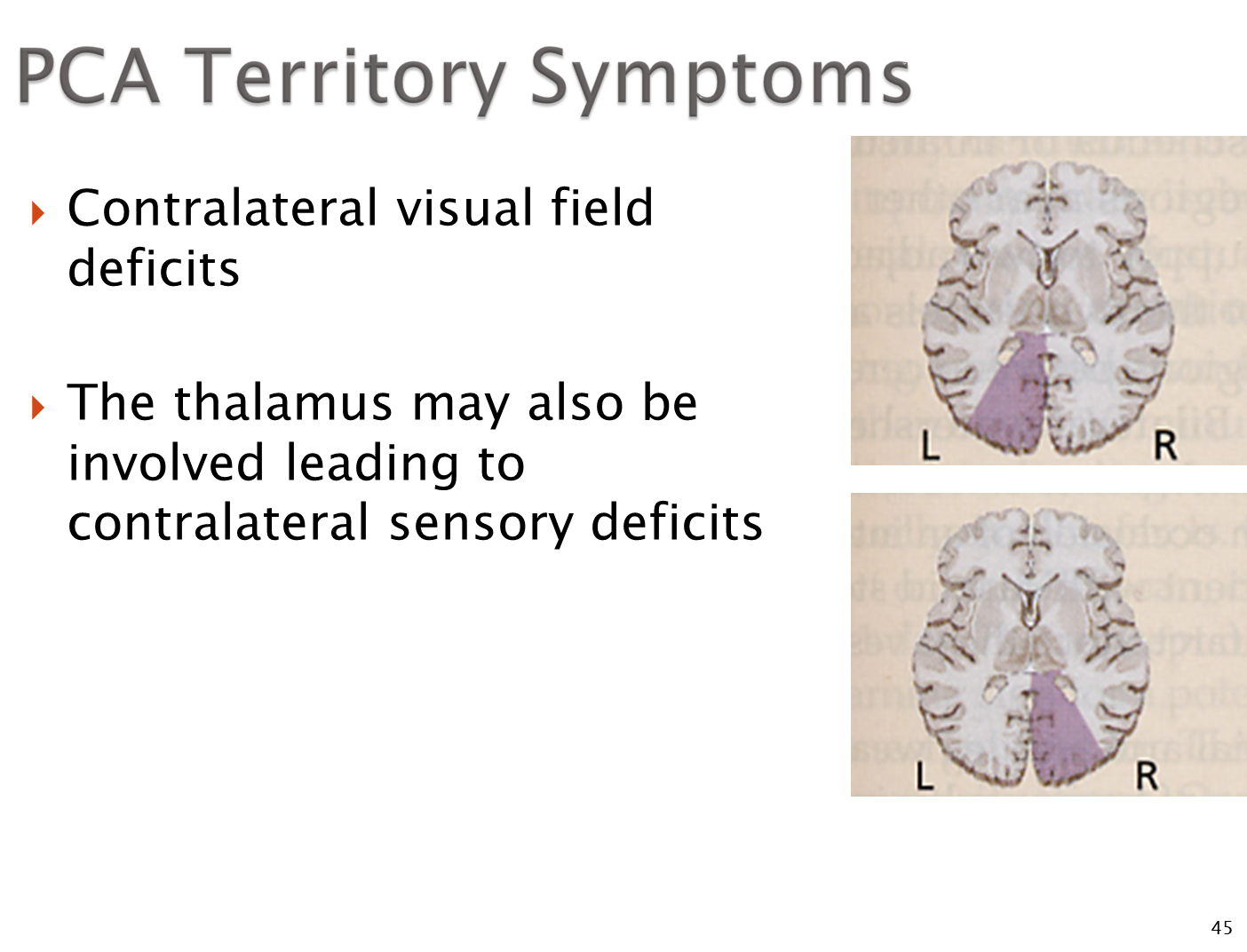
Stroke in the PCA can cause:
→ contralateral visual field deficits
→ because the PCA has branches that provide blood to the thalamus, there may be contralateral sensory deficits
What are Subcortical Territory Lesions?
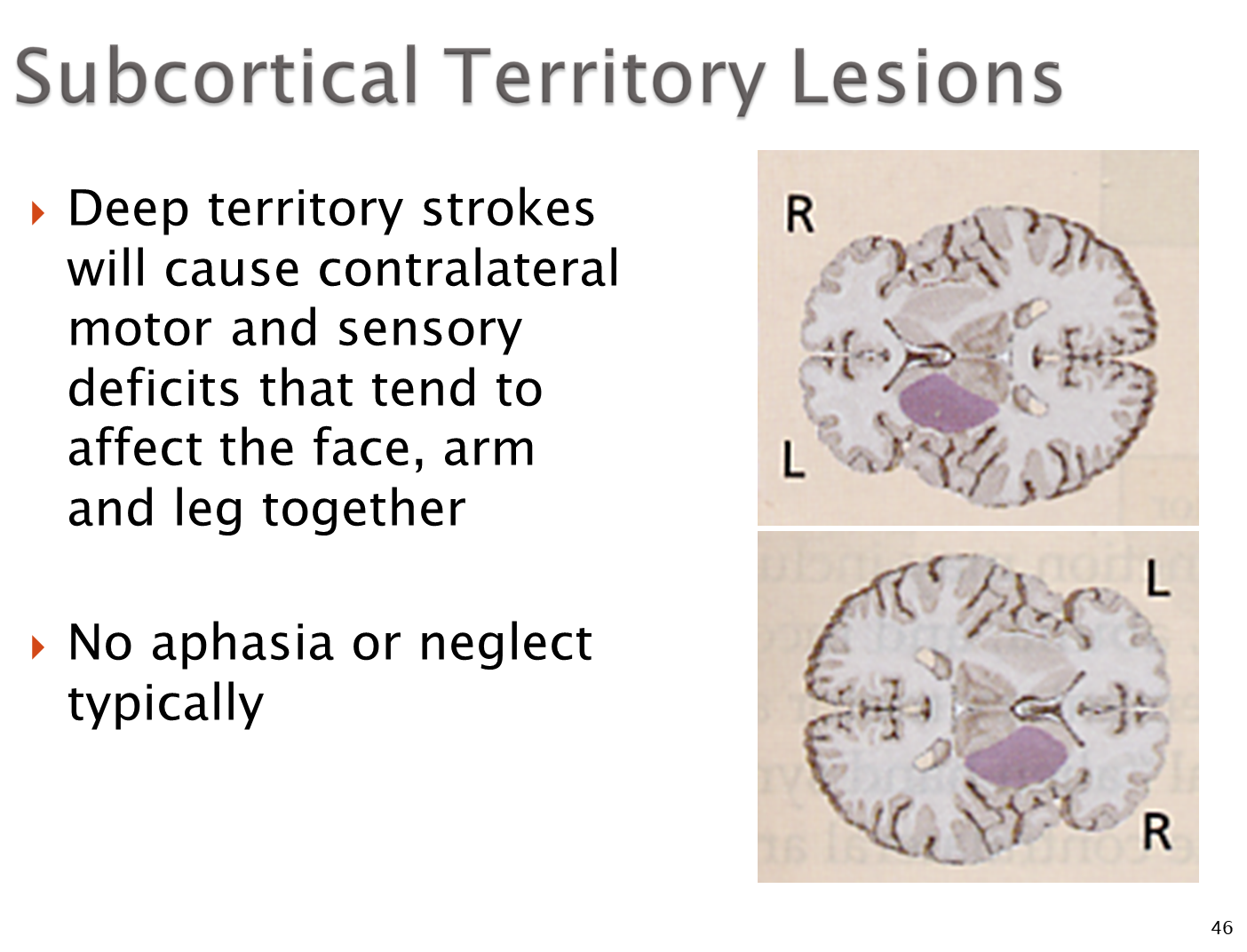
Strokes that affect the deeper parts of the brain that do not affect the cortex will cause contralateral motor and sensory deficits
→ importantly there is no aphasia as seen in dominant hemisphere MCA lesions or neglect as seen in non-dominant hemisphere MCA lesions
What are Brainstem Circulation Lesions?
Brainstem circulation lesions are more varied compared to other territory strokes
→ will frequently cause cranial nerve palsies
→ may cause Locked In Syndrome if there is a pontine lesion where patients appear to be asleep but patients are unable to move due to lesions affecting descending motor pathways but the sensory pathways/RAS are preserved