EXAM #1
1/108
Earn XP
Description and Tags
Lectures 1-6
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
109 Terms
Autism Spectrum Disorder (ASD)
A neurodevelopmental disorder that impacts how an individual interacts and communicates with other; it also includes restricted, repetitive behaviors, interests, and activities.
T or F
The definition of autism varies from state to state.
True
Key Features of ASD
Social Communication & Interaction
Social-emotional reciprocity
Nonverbal communicative behaviors
Understanding/ developing/ maintaining relationship.
Restrictive Repetitive Behaviors (RRBs)
Stereotyped or repetitive movements, use of objects, or speech
Insistence on sameness
Highly Restricted interests abnormal in intensity or focus
Hyper-or Hypoacitvtiy to sensory stimuli
Classifications of ASD
DSM-Diagnostic & Statistical Manual of Mental Disorders
ICD: International Classification Of Diseases
IDEA: Individuals with Disabilities Education Act
DSM-Diagnostic & Statistical Manual of Mental Disorders
Published by APA
Provides details of characteristics that classify individuals with varying diagnoses
Manual used by clinicians and researchers to diagnose and classify disorders
First edition published in 1952
Currently use DSM-5-TR (2022) – Autism Spectrum Disorder
ICD- International Classification Disorders
International Classification of Diseases (ICD)
An international standard diagnostic classification for a wide variety of health conditions
Published by the World Health Organization (WHO)
When we make a diagnosis, we draw a code from ICD
Currently use ICD-11
IDEA-Individual with Disabilities Education Act
In 1990, autism was added as a separate category of disability that may require special education services
Individual states have their own criteria for eligibility of special education service
In CA, Autism is a categorized as a developmental
disabilityThe autism must adversely affect a child’s educational performance
Why Classify for ASD?
To receive the specialized services that may most benefit them
For families/parents to help them understand what's happening with their child
To collaborate with other professionals
To provide/receive resources
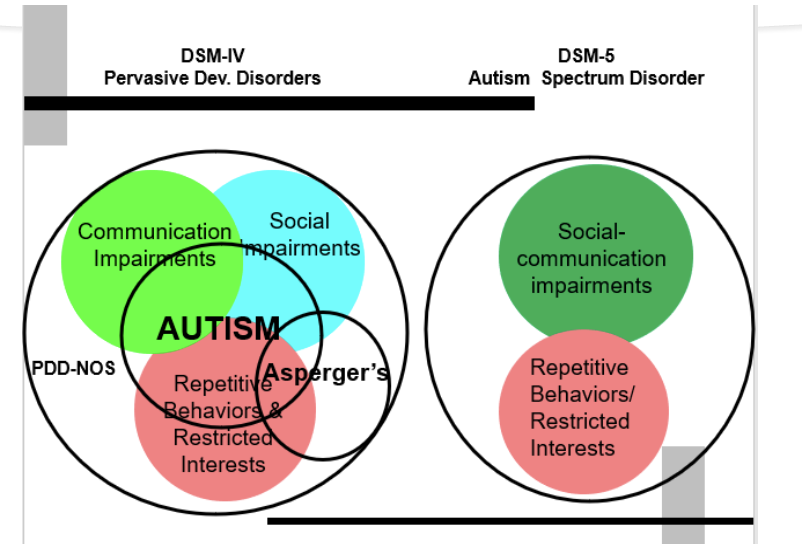
DSM IV
1994: DSM IV Autistic Disorder with the addition of Pervasive Developmental Disorder, Not Otherwise Specified (PDD-NOS), Asperger’s Disorder (or Asperger Syndrome), Rett’s Disorder (or Rett Syndrome) as separate disorders
Social with a bit of behavioral difficulties
An umbrella term
Pervasive Developmental Disordered (PDD)= category of a DSM IV & no longer in use
DSM V
Autism Spectrum Disorders; eliminated Pervasive Developmental Disorder,
Not Otherwise Specified (PDD-NOS), Asperger’s Disorder (or Asperger Syndrome), Rett’s Disorder (or Rett Syndrome) as separate disorders (All classified as ASD.They are all part of the spectrum; they are not separate disorders, just different sides of the spectrum.
Autism: term derived from Greek word autos for “self”
1911 › Swiss psychiatrist Eugen Bleuler used autism to refer to one group of symptoms he observed in adult schizophrenia.
During the 1940's – 1960’s autism was viewed as a childlike version of adult psychosis or schizophrenia
DSM IV & DSM V Classification Differences
DSM IV
Pervasive Developmental Disorders
communication impairments
social impairments
These 2 can’t be separated
Asperger’s
Repetitive behaviors/ restricted interests
DSM V
Autism Spectrum Disorder
Social- communication impairments
Repetitive behaviors/ restricted interests
Asperger’s Disorder Diagnostic Criteria (DSM-IV)
Qualitative impairment in social interaction (at least 2)
Restricted repetitive and stereotyped patterns of behavior, interests, and activities (at least 1)
No clinically significant general delay in:*
Language (single words by 2 years, phrases by 3 years)
Cognitive development
Self-help/adaptive behavior skills
*criteria that distinguishes it from Autistic Disorder (separate diagnosis)
T or F
The “Refrigerator mother” theory is a cause for autism spectrum disorder.
False; this theory should be debunked
DEF: The medical establishment came to blame mothers' (parents') lack of nurturing as the cause of autism for most of the 20th century.
DSM -V Diagnostic Criteria #1 KNOW **
Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history:
Deficits in social-emotional reciprocity,
EXAMPLES:abnormal social approach and
failure of normal back-and-forth conversation;
to reduced sharing of interests, emotions, or affect;
to failure to initiate or respond to social interactions.
Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example,
from poorly integrated verbal and nonverbal communication;
to abnormalities in eye contact and body language or deficits in understanding and use of gestures;
to a total lack of facial expressions and nonverbal communication
Deficits in developing, maintaining, and understanding relationships, ranging, for example,
from difficulties adjusting behavior to suit various social contexts;
to difficulties in sharing imaginative play or in making
DSM -V Diagnostic Criteria #2 *** KNOW **
Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history (examples are illustrative, not exhaustive; see text):
Stereotyped or repetitive motor movements, use of objects, or speech (e.g., simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases).
Insistence on sameness, inflexible adherence to routines, or ritualized patterns or verbal nonverbal behavior (e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns, greeting rituals, need to take same route or eat same food every day).
Highly restricted, fixated interests that are abnormal in intensity or focus (e.g., strong attachment to or preoccupation with unusual objects, excessively circumscribed or perseverative interest).
Hyper- or hypo-reactivity to sensory input or unusual interests in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement).
Severity Levels for ASD (DSM-V) - only 1 question
Severity levels are specified for both Social communication and Restricted, repetitive behaviors
Level 3: “Requiring very substantial support”
Level 2: “Requiring substantial support”
Level 1: “Requiring support”
Social Communication/Interaction
Level 1: Without supports, deficits cause noticeable impairments
Level 2: Marked deficits; impairments apparent even with supports in place
Level 3: Severe deficits that cause severe impairments in functioning
RRBs
Level 1: Significant interference with functioning in one or more contexts
Level 2: Appear frequently enough to be obvious to the casual observer and interfere with functioning in various contexts
Level 3: Marked interference with functioning in all spheres
Severity Levels of ASD (continued)
Severity is based on social communication impairments and restricted, repetitive patterns of behavior.
Symptoms must be present in the early developmental period (but may not become fully manifest until social demands exceed limited capacities, or may be masked by learned strategies in later life).
Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
These disturbances are not better explained by intellectual disability (intellectual developmental disorder) or global developmental delay. Intellectual disability and ASD frequently co-occur; to make comorbid diagnoses of autism spectrum disorder and intellectual disability, social communication should be below that expected for general developmental level.
A new DSM-5 Diagnostic Category
Under Communication Disorders in the Neurodevelopmental Disorders Section
SCD is characterized by a persistent difficulty with verbal and nonverbal
communication that cannot be explained by low cognitive abilitySymptoms include difficulty in the acquisition and use of spoken and written language as well as problems with inappropriate responses in conversation.
The disorder limits effective communication, social relationships, academic
achievement, or occupational performance. Symptoms must be present in early childhood even if they are not recognized until later when speech, language, or communication demands exceed abilities.
T or F
SCD and ASD can co-occur.
False; they can never co-occur
T or F
SCD can co-occur with other communication disorders like fluency, language, speech disorders.
True
SCD & ASD
SCD can co-occur with other Communication Disorders in the DSM-5 (language disorder, speech sound disorder, childhood-onset fluency disorder, unspecified communicationdisorder)
SCD is NOT "mild ASD"
While autism spectrum disorder (ASD) does encompass communication problems, it also includes restricted, repetitive patterns of behavior, interests or activities and gives equal weight to both communication issues and repetitive behaviors. ASD must be ruled out for SCD to be diagnosed
Social Pragmatic Communication Disorder: SCD
Impairments in social communication
mainly verbal
includes nonverbal
Social Pragmatic: ASD
Impairments in social communication and SOCIAL INTERACTION
Presence of restricted interest repetitive behaviors, insistence on sameness, or sensory
T or F
ASD can be co-morbid with all communication disorders but SCD.
True
What are Neurodevelopmental Disorders (List)
Intellectual Disability
Communication Disorders
Autism Spectrum Disorder
Attention-Deficit/ Hyperactive Disorder
Specific Learning Disorder
Motor Disorder
Other Neurodevelopmental Disorder
What constitutes a communication disorder? And which ones can co-occur with ASD?
Social (Pragmatic) Communication Disorder
Language Disorder
Speech-Sound Disorder
Childhood Onset Fluency Disorder
Unspecified Communication Disorder
** Can Co-occur with ASD*
Medical Diagnosis Vs Education Eligibility of ASD
Does not automatically entitle a student to special education services under the Individuals with Disabilities Education Act (IDEA)
Eligibility for special education services is based on an educational determination of a disability, which includes meeting not just the criteria for a specific disability (such as autism), but also finding that a student is in need of special services.
Who Diagnoses in Medical and Educational Settings
Medical
Diagnoses made by a doctor or other specially trained clinician by using symptom criteria set in the (DSM v)
Educational
is decided by a team comprised of various school professionals and a student’s parents.
The team must find that the student qualifies for services under IDEA.
To be eligible, IDEA requires that a student have at least one of 14 specified disabilities and be in need of special services. Autism is one of the 14 categories, but the definition of autism varies from state to state.
T or F
The definition for educational eligibility is the same in every state.
False, it varies from state to state.
T or F
Individual states have their own criteria for eligibility of special education services.
True
Medical Diagnosis Vs Education Eligibility: Impact on services
Medical
Treatment within the medical system usually consists of therapeutic interventions, such as behavior therapy, speech therapy, occupational therapy, individual counseling, or medication intervention to treat symptoms associated with ASD.
In the medical model, a diagnosis alone is usually sufficient to warrant treatment.
Cost: Varies depending on provider and insurance
Educational
require more than just a diagnosis; they require a finding that a student is in need of special services.
Once it is determined that services are needed, the particular services received will be determined by an Individualized Education Plan (IEP) team.
Services may include some of the same interventions as used in the medical system (for example behavior or speech therapy), as well as other supports (classroom and testing modifications, etc.) and specialized educational placements as determined by the IEP team.
Cost: Free for children/families in public schools
Medical Diagnosis Vs Education Eligibility: Summary
Parents have a variety of options regarding treatment and have to decide whether to pursue treatment through the medical system, the education system, or both
Educational and medical services can be pursued simultaneously, which is often the best strategy for children with Autism
T or F
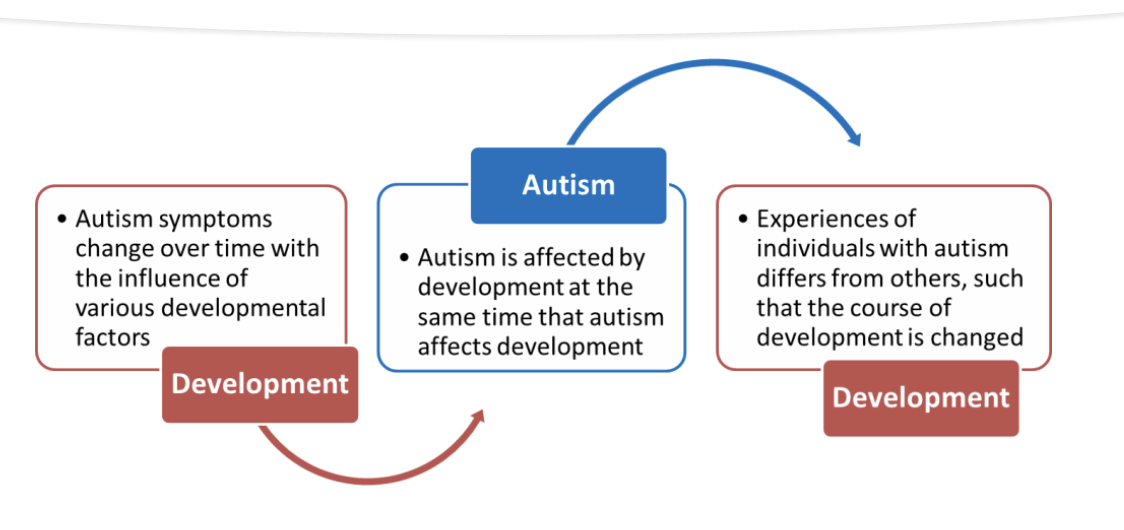
Development affects Autism, and Autism affects Development.
True
Autism as a Developmental Disorder
Development affects Autism, and Autism affects Development.
VIEW IMAGE
Prevalence Vs Incidence (Definitions)
Prevalence: The number of cases of a condition (or defined disorder) that exist at a particular time in a defined population
Ex: how many kids in the US have ASD today
Incidence: The number of new cases occurring in a population over a period of time
Prevalence Vs Incidence (Considerations)
Both prevalence and incidence estimates will be inflated when case definition is broadened and case ascertainment is improved
Time trends in rates can therefore only be gauged in studies that hold these parameters under strict control over time
Keep this in mind while reviewing rates of ASD
T or F
The prevalence of children identified with autism spectrum disorder is 1 in every 44 children.
False; 1 in every 36 children
Prevalence of ASD in the US
About 1 in 36 children has been identified with autism spectrum disorder (ASD) according to estimates from CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network.
ASD is reported to occur in all racial, ethnic, and socioeconomic groups.
ASD is more than 4 times more common among boys than among girls.
About 1 in 6 (17%) children aged 3–17 years were diagnosed with a developmental disability, as reported by parents, during a study period of 2009-2017. These included autism, attention-deficit/hyperactivity disorder, blindness, and cerebral palsy, among others.
Ongoing monitoring and reporting help us identify trends and changes in the number of people with ASD over time. To see these trends and changes, we can look at ASD prevalence.
Across multiple years,
Across multiple data sources,
In different geographic locations, and
Among different demographic groups.
These findings can be used in local communities and nationwide to inform initiatives, policies, and research that help children and families living with ASD
5 Components of Prevalence of ASD in the United States (LIST)
Reported prevalence has changed over time
Reported prevalence varies by location
Reported prevalence varies by sex
Reported prevalence varies by race and ethnicity
Early identification has been increasing over time
Reported Prevalence has changed over time
The reported prevalence of ASD has been higher in recent years, and this trend is consistent across data sources.
It is unclear how much this is due to changes to the clinical definition of ASD (which may include more people than previous definitions) and better efforts to diagnose ASD (which would identify people with ASD who were not previously identified).
A true change in the number of people with ASD is possible and could be due to a combination of factors.
T or F
The ratio of boys to girls diagnoses with ASD is 1:3.8
True
Reported Prevalence varies by sex
ASD prevalence has been higher among boys than girls.
1:3.8 ratio of boys to girls for ASD
There are no clear explanations for this difference.
Boys may be at greater risk for developing ASD
ASD can have different signs and symptoms in boys versus girls.
This can contribute to differences in how ASD is identified, diagnosed, and
reported
Reported Prevalence varies by geographic location
ASD prevalence varies widely across geographic areas.
EXAMPLE: having hospitals nearby, vs. the nearest hospital or service being hours away.
No research has shown that living in certain communities increases the chance that a child will have ASD.
Geographic variation could, however, be related to differences in how children with ASD are identified and/or served in their local communities and how this information is collected and reported
Note: Location doesn’t necessarily impact it all about the access to diagnosis
Reported Prevalence varies by race & ethnicity
Per CDC data, over the years, more non-Hispanic white children are identified with ASD than non-Hispanic black or Hispanic children.
Some children with ASD may not be receiving the services they need to reach
their full potentialPrevious studies have shown that potential barriers to identification of children with ASD, especially among Hispanic children, include
Stigma,
Lack of access to healthcare services due to non-citizenship or low-income, and
Non-English primary language
As of 2018, the CDC's Autism and Developmental Disabilities Monitoring (ADDM) Network (ADDM) found no overall difference in the percent of Black, White, Hispanic, and Asian or Pacific Islander 8-year-old children identified with ASD.
In several locations, the percent of Hispanic children identified with ASD was lower compared with Black or White children.
Overall, decreasing racial/ethnic differences over time may be due to more effective outreach directed toward minority communities and efforts to have all children screened for ASD
T or F : The prevalence of ASD in the US
Early identification has been decreasing over time because of more early intervention sessions.
False; it has been increasing
Understanding Increased Prevalence
Some reasons for increased rates (increased prevalence)
better recognizing the symptoms
Improved Identification
Definition of Autism has been broadened
Children can now be diagnosed with more than one developmental disorder
T or F
Autism is caused by vaccinations.
False, Vaccines DO NOT cause Autism.
• studies have shown that there is no link between receiving vaccines and
developing ASD
T or F
Autism is caused by “Refrigerator Mothers”.
False; Autism IS NOT being caused by cold or distant mothers
• No evidence that indicate that ASD can be caused by poor or
improper parenting, an emotionally unavailable mother...
T or F
Autism is not caused by vaccines.
True
Causes of Autism
There are different levels of severity and combinations of symptoms in ASD, and there are probably multiple causes.
The best scientific evidence available to us today points toward a potential for various combinations of factors causing ASD–
Multiple genetic components that may cause Autism on their own or possibly when combined with exposure to as yet undetermined environmental factors
Genetic Links
More than one gene (polygenetic)
Genetic similarities increase likeliness:
Identical Twins: 77%
Fraternal Twins: 31%
Siblings: 21%
Progress has been made toward understanding different environmental risk factors, and the clearest evidence involves events before and during birth, such as:
Advanced parental age at time of conception
Prenatal exposure to air pollution or certain pesticides
Maternal obesity, diabetes, or immune system disorders
Extreme prematurity or very low birth weight
Any birth difficulty leading to periods of oxygen deprivation to the baby’s brain
These factors alone are unlikely to cause autism. Rather, they appear to increase a child’s risk for developing autism when combined with genetic factors
List of Environmental Risk Factors
Happen before and during birth)
advanced parent age
extreme prematurity or very low birth weight
maternal obesity, diabetes, immune system disorder
Lack of oxygen to the brain
Specific chromosomal abnormalities
Fragile X
Down syndrome
~10% of children with ASD are also identified as having some other genetic or chromosomal disorder
T or F
The vast majority of cases of ASD are idiopathic.
True
Searching for the cause of ASD….
ASD is not caused by lack of love or inadequate parenting skills
Anything that affects the functioning of the CNS can trigger the symptoms of ASD
Knowing the cause is important for medical research and to help parents get appropriate genetic and medical information, but effective educational programs do not depend on pinpointing the exact cause
T or F
There are discrepancies in diagnostic tools related to the different genders.
True; most tools are made off boys symptoms.
Boys vs Girls: SIGNS & SYMPTOMS
Compared with boys, girls (without an intellectual disability):
Have less apparent restrictive interests and repetitive behaviors
how higher social motivation and greater capacity for friendship (may try harder to fit in)
Tend to internalize their emotions— which could spur anxiety, depression or eating disorders—in contrast to males’ externalizing behavior that shows up as hyperactivity or noncompliant behavior
May appear to have better play skills with others than boys do; in reality, they may be playing near others (not with them) and observing their behaviors --> "social camouflaging"
Boys vs Girls: Differences in how ASD is identifies, diagnosed and reported
The current ASD diagnostic tools and assessments were normed largely on boys, so they won’t identify some girls [e.g., Autism Diagnostic Observation Schedule (ADOS); 2017 International Meeting for Autism Research]
Girls may be overlooked or misdiagnosed with other conditions (e.g.such as obsessive compulsive disorder, anxiety disorder, depression and bipolar disorder).
Some girls are never diagnosed
Some girls are diagnosed as teenagers and adults
Lack of diagnosis, misdiagnosis, or late diagnosis impact social, emotional, vocational and academic development
T or F
Language performance is the same in both languages for bilingual autistic children.
True
Disparities in Bilingual Autistic children
Disparities in identification and diagnosis
Interactions with healthcare providers
Disparities in research participation
Scare body of literature with CLD clientele with and without ASD
Disparities in prevalence rates, age of identification, and comorbidity of children with ASD across racial, ethnic, and socioeconomic status groups
Disparities in service provision for ASD
Further discussion in assessment and treatment units
Differential Diagnosis
Differential diagnosis is the process of determining the presence or absence of a condition with appropriate consideration of which condition best explains a person’s presentation.
It takes into account, current symptoms as well as their developmental history and significant life events/trauma.
Generally, a clinician is looking for the best descriptor of a person’s presentation and needs, recognizing that sometimes, this means one diagnosis, and sometimes it means two or more
NEED TO RULE OUT ONE THING TO BE ABLE TO RULE ANOTHER ONE IN
Comorbidity
DEFINITION: two or more conditions that are present at the same time
Just as important as differentiating an appropriate diagnosis is recognizing when more than one exists
Impacts of common developmental and emotional disorders can include:
Social Functioning
Behavioral functioning
Emotional functioning
Language/ communicative functioning
Educational functioning
Executive Functioning
Because there is significant overlap in areas impacted, a trained clinician is needed to help put those pieces together for a child and their family.
There is also a gap in when we want to diagnose ASD and when we can diagnose other disorders.
Sources of Information in an assessment
Parent/Caregiver
• Detailed developmental history & current symptoms/concerns
• Parent interviewTeacher
• Data gathered prior to assessment, interventions tried and their effectiveness
• Teacher interviewDirect testing and observations
• Observations (in the classroom or other settings)
• Direct assessment/diagnostic interaction.
Additional Assessments in order to determine a true diagnosis of ASD
Assessing cognitive skills and adaptive functioning
• EX: brushing teeth; LIFE SKILLSAssessing receptive and expressive language, including pragmatic (social) language
Assessing of any sensory, fine motor, or physical needs/concerns
Comorbid Diagnosis
Possible question type: Which of the following is co-morbid with ASD….
Neurodevelopmental Disorders:
Intellectual Disability
Language and Learning Disorders (e.g., dyslexia, hyperlexia)
Attention-Deficit Hyperactivity Disorder (ADHD)
Mental Disorders
Anxiety and Depression
Obsessive Compulsive Disorder (OCD)
Some genetic disorders are more common in children with ASD
Fragile X syndrome
Down syndrome
Duchenne muscular dystrophy
Co-morbid Diagnosis: ADHD
Inattention
Difficulties paying attention
Hyperactivity
Fidgety, restless, constantly on the go, talking excessively
Impulsivity; Not recognizing consequences of actions, interrupting others, engaging in risky or dangerous behavior, and/or aggression
Behavioral challenges that set them apart from peers
Interference with learning
Impaired Social Skills
Difficulty making friends, fitting in at school
Inability to figure out rules of social interaction and
engagement
Co-morbid diagnosis: Autism
Communication skills more impaired
Great challenges in deciphering body language, facial expressions, tone of voice, sarcasm, and other elements of non-verbal communication.
Difficulty with pragmatics language skills or those aspects of interpersonal communication such as all the unwritten rules of how to carry on a conversation.
Lack “theory of mind:: ability to imagine other people’s mind states including theory of thoughts, feelings, and intentions in order to anticipate how others will react or feel to certain events or actions
less capable of engaging and connecting with others
limited to no eye contact, no desire to share, and difficulties with joint attention
Presence of restricted and repetitive behaviors.
Early Signs & Symptoms
Autism caught in infancy (by 18 months of age); treatment highly effective
ASD hard to diagnose before 24 months
Symptoms often surface between 12 and 18 months
ASD symptoms present in some children by 12 months (on standardized cognitive /language measures, as well as more subtle measures of affect and social reciprocity)
Early detection of symptom onset (based on behavioral assessment) may not be possible before 12 months of age –> to date, there are no clear differences at 6 months
Risk can be established before 2 years in at least some children
T or F
Symptoms are set by the age of 3.
True
T or F
The average age of diagnosis is 3 with symptoms by age 2.
False, the average age is 4 with symptoms by age 3.
Regression and Autism
Infant sibling studies following children from 6 months
Close to half (10/24) of infant siblings later diagnosed with ASD “worsened” between 14 and 24 months (per Mullen scores and/or social communication) (Landa & Garrett Meyer, 2006)
86% (19/22) of infant siblings later diagnosed with ASD showed declines in social communication behaviors (gaze to face, social smile) after 6 months of age, with group differences becoming significant by 12-18 months (see next slide) (Ozonoff et al., 2010)
Behavioral signs emerge over time through a process of diminishment of key social communication behaviors (Ozonoff et al., 2010)
Regressive Autism
The term “regressive autism” (implying symptom onset pattern of regression following typical development) may not be appropriate in describing the vast majority of children with ASD who are reported to lose skills
Appears to be a few cases of acute regression (severe and sudden onset)
Significant delays in attainment of skills reported in children who lose skills
Loss of skills may occur more frequently but in a more subtle form than previously thought
Symptom onset in ASD may be best represented as a continuous phenomenon rather than categorical (regression/no regression)
“I don’t even call it regression anymore. I just think of it as onset: how symptoms start.”
Earliest Signs
Absence of normal behaviors—not the presence of abnormal ones (tough to spot)
Sometimes earliest symptoms misinterpreted as signs of a “good baby”
(quiet, independent, undemanding)Don't respond to cuddling, reach out to be picked up, or look at mothers when being fed
Things to Look out for:
Does an infant or toddler?
make eye contact (e.g., look at you when being fed)
smile when smiled at
respond to his or her name or to sound of a familiar voice
follow objects visually
point or wave goodbye or use other gestures to communicate
follow gesture when you point things out
make noises to get your attention
initiate or respond to cuddling
imitate your movements and facial expressions
reach out to be picked up
play with other people or share interest and enjoyment
ask for help or make other basic requests
Signs that child is at risk:
No big smiles or other warm, joyful expressions by six months or thereafter
No back-and-forth sharing of sounds, smiles or other facial expressions by nine months
No babbling by 12 months
No back-and-forth gestures such as pointing, showing, reaching or waving by 12 months
No words by 16 months
No meaningful, two-word phrases (not including imitating or repeating) by 24 months
Any loss of speech, babbling or social skills at any age
Signs that child is at risk in 2nd year:
Impairment in Social Interaction/Communication, Repetitive Behaviors & Restricted Interests:
Lack of appropriate eye gaze & lack of warm, joyful expressions
Lack of sharing interest or enjoyment & lack of response to name
Lack of showing gestures
Lack of coordination of nonverbal communication
Unusual prosody (little variation in pitch, odd intonation, irregular rhythm, unusual voice quality)
Repetitive movements with objects
Repetitive movements or posturing of body, arms, hands, or fingers
Signs in older children
Diagnosis in older children can be trickier:
Often, children have more mild symptoms that surface as their competencies are outpaced by social demands.
This can be seen sometimes:
when a child goes to school for the first time
as academic demands increase,
as social play becomes less activity-based and more social/language based
exposed to a larger number and more diverse social community
Typical Development of Communication (3 stages)
Perlocutionary Stage
Illocutionary Stage
Locutionary Stage
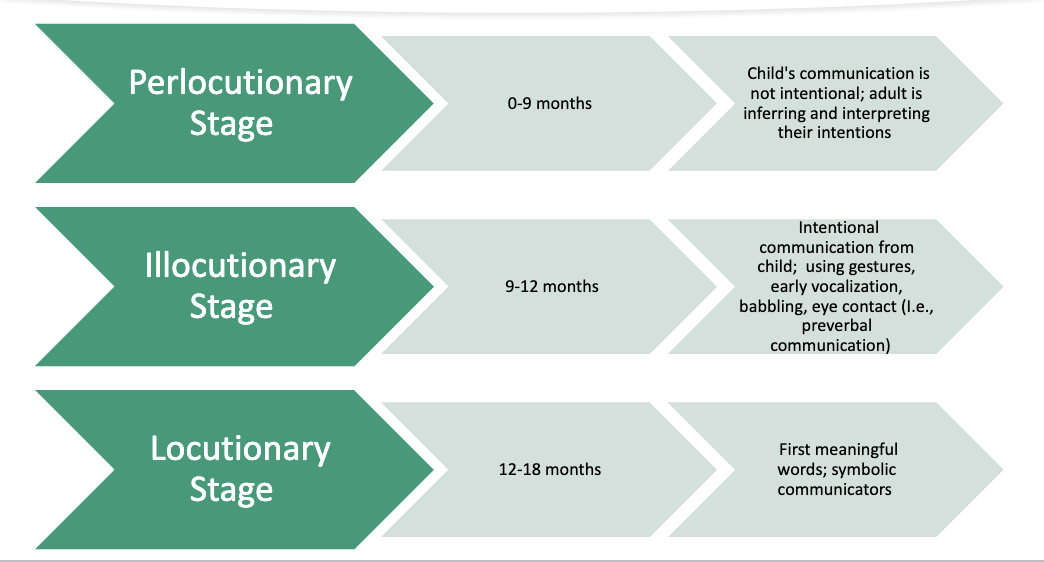
Perlocutionary Stage
0–9 months
Child’s communication is not intentional; adult is inferring and interpreting their intentions.
Reflexes
Illocutionary Stage
9–12 months
Intentional communication from child; using gestures, early vocalization, babbling, eye contact (ie. preverbal communication)
More intentional communication
Locutionary Stage
12–18 months
First meaningful words; symbolic communicators
The words and symbols have/carry meaning
Communicative Functions: Intentions/ Intentional Communications
Behavior regulation: indicating to adults that they want water by holding out the cup.
Social interaction: waving hi and bye; initiating a social game; requesting comfort (e.g., playing with the cup)
Joint attention: communicating to share interest on an object or event (e.g., showing adult that they have cup in their hand for the adult to notice – not really holding it out for adult to fill in it
What is included in prelingusitic communication?
Prelingusitc Comm: occurs before the use of words
EXAMPLES:
Eye Gaze
Shared Positive Affect
Sounds
Communicative non-word vocalizations
Gestures
Gestures
Non-vocal action that is directed to another person (involves the intent to communicate)
Ex: pointing
Joint Attention: DEFINITION
early social and communicative behavior
Early joint attention behaviors indicate the child’s growing awareness of the need to engage other people
2 Types of Joint Attention
Responding to joint attention (gaze following)
Initiating Joint attention (pointing to share interest)
Joint Attention & Language
Joint attention is an underpinning of language development for all children.
Failing to address vital social-cognitive elements results in language intervention that is ineffective and/or inappropriate
We need to build skills that will help development communication
Means for communication: degree to which learner has intact and efficient cognitive (e.g., perception, attention, memory), sensorimotor (e.g., hearing), and motor planning skills to use for processing languages (Kohnert, Ebert, & Pham 2021)
In typically developing children, there’s a high correlation between vocabulary size and time spent in joint attention activities with the mother:
In children with ASD, there are correlations between early joint attention skills and:
Language gains in early intervention
Language development during adolescence
Language & Communication
Words are symbols that represent concepts
Vast difference between building up a collection of symbols (I.e., words) and using these symbols for communicative intent
Knowing sounds, words, meaning, grammar, and the different ways to combine these linguistic features for syntactically and pragmatically appropriate combination is essential... But proficiency in a language requires the ability to use this knowledge for functional, real-time communication.
For an Autistic child, the ability to say words does not guarantee that he/she is able to use them to express intentions (thoughts, feelings, desires, or needs
Implication for intervention: The lack of understanding of the difference between having symbols (words) and using them to communicate sets up the individual for failure in language therapy
T or F
Social games are important.
True
Social Interactions: Social Games
Social games are important precursors to the development of social communication – Why
Caregiver and child engage in
Attention sharing
Affect sharing
Social reciprocity
The infant is also learning to
Regulate interaction
Anticipate what will come next
Infants with autism do not as readily engage in baby games as their typically developing peers do
Cascading effect in ASD:
Missing out on opportunities to engage in emotional regulation, affect and attention sharing, and social reciprocity, etc.
But also...
The neurons that would normal be used in these activities are not getting activated, and the new neural pathways are not being built
Recall:
Everything an infant experiences provides his/her brain with new information
As the different areas of the brain process the incoming information, neural pathways are
formed within and between areas of the brain
Speech Characteristics in ASD
Articulation
Distortions of some later-developing sounds may persist (e.g., s/l/r)
Possible difficulties with Prosody – 50% of kids show prosodic differences; intonation, rate, stress, infections, nasality..,
Stress, phrasing, hypernasality
Rate (slower or faster)
Difficulty regulating volume (loud or soft)
Intonation (monotone; flat)
Pitch (high)
Difficulties affect listeners’ perceptions of social and communicative competence
What predicts language?
Expressive Language
Cognitive Ability
Nonverbal cognitive ability
Initiating joint attention
Ability to imitate sounds and simple movements
comprehension/ receptive language
Having some spoken language
attention and social motivation
Receptive Language
Cognitive ability
Nonverbal cognitive ability
responding to joint attention
child gesture
Language Characteristics in ASD
Differences in learning the meaning of words
EX: non-literal languages
Differences in the USE of Language
May attain language skills but less able to use language to communicate
Pedantic speech style (“little professors”) -- overly formal communication style, inappropriate for the context (vocabulary, prosody, articulation)
Obsessive interests or idiosyncratic topics – and may discuss at length without regard to listener’s interest
Limited ability to use language to have and maintain conversations, despite expansive vocabularies
Conversational difficulties
Difficulty managing topics (perseveration, inability to read cues to change topic)
Difficulty listening, following rules of politeness, and supplying relevant information
Seek adults as conversational partners
Language learning differences can have a major impact on life for individuals with ASD. Parents, teachers, etc. must understand the effect of such differences so they can:
Understand why individuals with ASD do some of things they do
Design instruction and support systems to ensure that the language is learned more
completely
Language Characteristics in ASD: Echolalia
Echolalia is not always meaningless repetition
Focus on the communicative intent, not the echoed words, to understand what the person means
e.g., "it's circle time"
Repetitive Questions and Sentences
May repeat same message because it is the only way they know how to communicate it
Verbal rituals
Any use of language that is repetitive, insistent, and often expressed with intense emotion
May include echolalia, perseverative speech, incessant questioning
Echolalia
Repeating words/sentences others have said
Usually repeated with the same emphasis and quality as used by the original speaker
Usually echoed words/phrases are stored “in chunks” without analysis for meeting
Words/phrases may be echoed fluently while self-generated words are slow +labeled
2 types of Echolalia
Immediate Echolalia: repeating something you heard at that moment
EX: Clinician- “Where’s the ball” Client- “Where ball”
Delayed Echolalia: Repeating something you heard at home or before
EX: client- “Have a seat”: something his mom usually says
Communication Characteristics in ASD
Prelinguistic Communication
Delay in/no use of communicative gestures
Reduced/no communicative intentions (joint attention, initiated social interaction)
Minimal/lack of coordination of communicative means (coordinating eye gaze towards someone, pointing)
Inconsistent eye contact
Minimal/no prelinguistic vocalizations
Reduced age-appropriate play (e.g., infant social play)
Expressive/Receptive Language
Language Delay (not specific or universal in ASD)
Comprehension (may be depressed relative to production)
Tendency to use language for requests rather than commenting and generating novel messages
Conversation and Pragmatic Communication
Difficulty turn-taking, topic, perspective-taking
Routinized interactions
Perseverative topics
Self-directed conversation
Difficulty with reciprocal interaction
Difficulty with flexible discourse
Difficulty with shared conversation
T or F
Either delay or deviance still reflects the importance of early intervention.
True
Social-Emotional Development in ASD: Infancy
Infancy
Lack of reciprocal eye contact
Infrequent or absent social smile
May receive less pleasure from physical contact or be less likely to reach for or seek physical comfort from parents
Attachments may develop more slowly
Lack of response to name
Reduced interest/attention to human faces
Social-Emotional Development in ASD: Early Childhood
Early Childhood
Preference for objects over social interaction
Prefer solitary activities
Limited range of facial and body expressions
Difficulty with perspective taking
Less seeking to share enjoyment
Cooperative play uncommon
Social-Emotional Development in ASD: Adolescence
Adolescence
Difficulty with reciprocal social exchanges
Remain focused on own interests and pursuits
Play & ASD
Play is…
Voluntary
Pleasurable
Intrinsically motivating
Requires active engagement
Flexible
Non-literal