Ch9: Muscles and muscle tissue
1/59
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
What are the muscle Types using two classifications
What is their special characteristics
Voluntary
Skeletal :
Striated
Elongated cylindrical
multinucleated
Involuntary:
Cardiac :
Striated
Branches at intercalating discs
Mononucleated
smooth :
Non-striated
Sheet like
Elongated
Spindle shaped cells
mono nucleated
What is the special name of muscles cells in which type of muscles and why in those types ?
What prefixes belong to muscles
Muscle cell is called muscle fiber in smooth and skeletal muscle but not in cardiac because they are elongated
Myo and mys and sarco
What are the characteristics of a muscle tissue (4)
What does each mean
Excitability /responsiveness,
Ability to receive and respond to a stimulus by changing membrane potential
Extensibility : Ability to extend / stretch
Elasticity : ability of muscle to recoil to resting length after stretch
contractility : ability to shorten forcibly when stimulated
What are the functions of muscles (4)
Produce movement
Maintain posture and body position
Stabilizes joints
generate heat
What serves the muscle with it’s needs
where do they pass through
how do they reach to all the cells
How do skeletal muscles differ from other types
The muscle is served with :
One nerve
One artery
One / more veins
They pass through the central part of the muscle
They branch through connective tissue sheaths
Each muscle fiber of skeletal muscle is served with a nerve ending to control it’s voluntary action unlike cardiac and smooth which can sometimes not have one
What is the function of connective tissue sheaths (5)
Supporting each cell
holding together the muscle
prevent the muscles from bursting during strong contractions
Transmit pulling force to bone to be moved
Provide routes for entery and exit of Blood vessles and nerve fibers
What are muscle sheaths continuous with
they are continuous with each other
They are continuous with aponeurosis and tendons connecting to the muscle
What are the connective tissue sheath types
What do they surround
what are they made of
What is a fascicle
Epimysium :
Surrounding the whole muscle
Dense irregular CT
Sometimes blends with other neighboring facia
Perimysium :
Surrounding each fascicle
Dense irregular CT
Endomysium :
Surrounding each muscle fiber
Areolar CT
A fascicle group of muscle fibers surrounded by perimysium
At how many points do muscles attach to bones
What are the names of those points
what is the difference
where is the location
Towards where does motion of muscle occur
At least at two points
Two types :
Insertion :
The attachment to a bone that can move
Distal
Origin :
The attachment to a bone that can’t move or moves less
proximal
The muscle’s insertion moves towards the muscle’s origin
What are the types of muscles attachments
Characteristics of the attachment
Types if applicable
Between what does attachment occur generally
Which type is common and why
Muscle attachment:
Direct/ fleshy attachment :
Epimysium of muscle is fused to the periosteum of the bone or the perichondrium of the cartilage
Indirect attachments :
Epimysium of muscle fuses to Dense Regular which connects to periosteum (all of which are CT)
Through two types :
Tendons : rope like
Aponeurosis: Sheet like
Occurs generally between connective tissues one that belongs to the muscle (epimysium) and other that belongs to bone (periosteum) and mostly something in between (tendon / aponeurosis ) which are also connective tissues
Indirect attachment is better because
It doesn’t require much space
can withstand abrasion from bones unlike muscles
What are the most important organelles of the muscle fiber and what are their normal cell equivalents
How were the muscle fibers formed
Organelles :
Sarcolemma : Plasma Membrane of a muscle fiber
Sarcoplasm : Cytoplasm of a muscle fiber
Sarcoplasmic reticulum : endoplasmic reticulum
Glycosomes : Granules that store glycogen which produces glucose when muscle needs
Myoglobin : Red pigment that Stores Oxygen
hundreds of embryonic cells fuse to form one muscle fiber
What are the specialized structures of muscle fiber
Sarcoplasmic reticulum
T-tubules
Myofibrils
Myofibrils :
What are they made of
What is that made of
What are they ?
How many myofibrils does each muscle fiber have and how are they arranged
myofibrils are made of a chain of sarcomeres that are linked end to end
They are made of myofilaments :
Thick filaments
Thin filaments
Many accounting up to 80 % of muscle fiber that are densely packed
What are striations
What are their types
draw the striations of a sarcomere
which to which striation structure makes up a sarcomere
Repeating series of dark and light bands evident along the length of each muscle fiber :
A Bands :
Extends along the thick filaments
I Bands :
The region with only the thin filaments
H-zone :
The central less dark region of thick filaments
M-line :
The line at the center of a thick filament formed by myomesin protein
Z discs : Zig zag lines at the center of I bands
A sarcomere is between Z-line to the adjacent Z-line
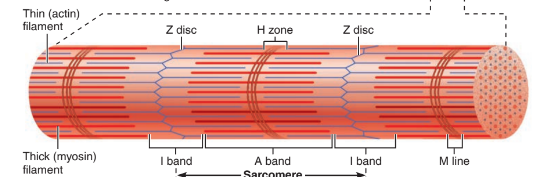
What is the smallest contractile unit of a muscle fiber
What striations does it have at which locations
a sarcomere
Between two successive Z-discs they have :
Half I band at each side next to Z discs
A band in center along thick filaments
H zone and M line at the center of A bands
Thick filaments :
What are they made of
What is that made of
As which enzyme does myosin act and which part of it exactly
what striation is possible because of it
What causes the H zone
What is the role of Myomesin and what striation does it form
300 Myosin molecules bundled together the tails facing inward and the heads facing outwards
Made of Six polypeptide chains :
2 heavy : twist to form the tail
4 light : form the 2 globular heads
attached to each other by a flexible hinge
The globular head acts as ATPase
This structure causes A band (thick filament with myosin heads) and the H zone (thick filament without myosin heads/thin filaments)
The H zone is caused by lack of myosin heads at the center of the thick filaments
Myomesin connects thick filaments of one myofibril to thick filaments of another and they form the M line which helps in alignment of myofibrils
Thin filaments:
What proteins is it made of
What are the subunits of this protein if any
Structure
what is the function of the subunits
what do they form only for 1
Made of protein actin and regulatory proteins:
Actin:
The subunits are G-actin (globular) :
Kidney shaped
Has a myosin binding site where myosin heads attach to during a contraction
They polymerize to form F-actin (filamentous)
One thin filament has two F-actin interwinding each other to form a helix
Regulatory proteins :
Troponin :
Is a globular protein
Has three subunits :
1 Binds to Actin filament : to bind
1 binds to Ca
1 Binds to tropomyosin : to help position tropomyosin on actin
Tropomyosin:
Long rod
Covers the actin filaments to block it’s binding sites and prevent contraction when not needed
How is the hexagonal arrangement viewed
Six thin filaments surround each thick filament
Three thick filaments surround each thin filament
What is the other type of filaments
What is it made of
how is it placed
what is it’s function and which part
Elastic filaments :
Made of Titin protein
Extends from Z discs through the center of the thick filament to connect to the M-line
The part of the titin that spans the I bands is extensible,
unfolding when the muscle stretches and recoiling when the tension is released
What are the other important proteins
Function of 1 and 5 only
What are their general functions
Dystrophin: Links thin filaments to integral proteins of sarcolemma which are anchored to the ecm
Nebulin:
myomesin
C-protiens
Intermediate (desmin) filaments extend from Z disc and connect each myofibril to the next one through the muscle fiber
Their general functions is to bind to filaments or sarcomeres and maintain their alignment
What is a disease related to the proteins above
To what family of diseases does it belong to
when do they appear
inheritance and gender
What causes it
cure
DMD : Duchenne muscle dystrophy
belongs to Muscular dystrophy family
appear during childhood (2-7)
sex linked recessive mostly to males
Caused by a defective gene for dystrophin which causes the sarcolemma to tear and allow Ca2+ to enter which causes muscle cells to go through apoptosis
Death
What are the type of sets of intracellular tubules that the muscle fiber has
What do they form
why is it called that way
2 types of sets :
Sarcoplasmic Reticulum
T-tubules
They form a triad
because it houses two terminal cisterns with a T-tubules in the center
What is the function of Sarcoplasmic reticulum
How do they run along what
Where do they communicate with each other and what does that form
Functions include :
Stores and regulates intracellular levels of Ionic Ca2+
Releases Ca2+on demand when muscle fiber is stimulated
They run longitudinally (same direction as myofilaments) along a Myofibril to surround it
they communicate with each other at two points :
H zones (forms a network of interconnecting tubules)
A–I band junction (forms the Terminal cisterns of Triad)
What are the T-tubules
What is the function of the T-tubules
they are invaginations of the Sarcolemma going down along the circumference of each microfibril which is continuous with extracellular space
They increase surface area which allows changes in membrane potential to occur fast so they act as voltage sensors
What is considered a contraction
when does shortening occur
when does contraction end and what is that stage called
What model explains whats stated up
What does it say
what happens to the striations during shortening
Formation of cross bridges (myosin heads binding to actin filaments)
only occurs if the force generated is greater than the opposite tension force
cross bridges become inactive (relaxed)
sliding filament model of contraction
It says that the myosin heads cause the thin filaments to overlap to a greater degree which causes shortening
Striations :
A band : length Doesn’t change but move closer to each other
I band : shortens
H zone : shortens / disappears
Z discs: distance between them decrease
What does excitable cell mean
examples
what are the types of signals
What is the type that we work with
1 benefit 1 drawback
cells that respond to external stimuli by changing their resting membrane potential.
two :
Muscle fibers
Neurons
Two types :
Electrical signal :
AP (action potential / nerve impulse) :
Travels long distance
cannot pass from cell to cell
Chemical signal:
Neurotransmitters (Acetyl-choline)
Can pass from cell to cell
Travels short distance
What are the types of Ion channels important for excitation and contraction of skeletal muscles
What are they opened with
What do they cause
The example that we are working with
Chemically-gated :
Opened by chemical messengers (AcH)
cause a small local depolarization which triggers voltage gated channels
ACh receptor
Voltage gated:
open or close in response to membrane potential changes (Action potential)
They cause the next voltage gated to open as they carry the message
Voltage gated K+ and voltage gates Na+
What gives the order for the skeletal muscle to contract
Where do they reside
how do they communicate
where
how many
Somatic motor neurons
They are present in the spinal cord except for brain and neck which is in the brain
The neurons have axons which branch alot as they enter the muscle then they branch to form a neuromuscular junction / motor end plate
near the center if the muscle fiber
each muscle fiber has 1 neuromuscular junction no more no less
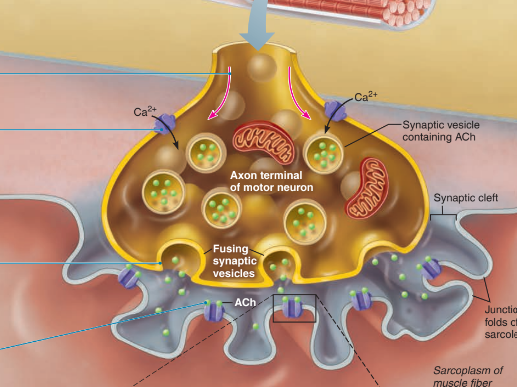
Draw the neuromuscular junction and label its parts
provide brief explanation of the parts
Axon terminal : end of the neuron
synaptic cleft : Fluid filled area rich in glycoproteins and collagen fibers
Synaptic vesicles : membrane bound granules that contain acetylcholine
junctional folds of sarcolemma : increase surface area
Note : Axon never touches the muscle
How are the steps that lead to contraction divided
Events at the neuromuscular junction
Excitation of a muscle fiber
Excitation contraction coupling
Cross bridge cycling
Events at the neuro muscular junction
What are the steps
Action potential arrives at the axon terminal
Ca2+ ion channels are opened which allows it to move into the axon terminal down it’s electrochemical gradient
Ca2+ entry causes ACh to be released by exocytosis.
ACh diffuses across the synaptic cleft and binds to ACh receptors on the sarcolemma.
ACh binding opens chemically gated ion channels which allow K+ to move out and Na+ to move in at the same time which creates a local depolarization called (End plate potential)
ACh effects are terminated by acetylcholinesterase which breaks down acetylcholine to acetic acid and choline
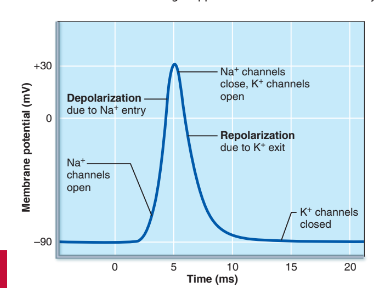
What are the steps of excitation of muscle fiber
What is a refractory period
What are the cellular conditions after the end of the stimulation
opening of chemically gated channels causes Endplate potential which is a local depolarization
Depolarization: opens voltage gated sodium channel which allows sodium to move in
sodium moving in causes depolarization by which + charge is increasing in the cell which also triggers the same gated channel to close
depolarization triggers potassium voltage gated channels to open
What is one disease related to ACh
what are it’s signs
what causes it
Myasthenia gravis
signs include drooping eyelids and muscle weakness
it is caused when immune system destroys ACh receptors
draw the graph that shows depolarization and repolarization
what is that one period and why is it important
what does repolarization restore and what does it not
What can cause problems with contraction
What fixes it
what is special about AP
Refractory period is the period of repolarization
it is important because no matter how strong the stimulation is the muscle cannot be stimulated until the refractory period has ended because the Na+ ion channels cannot be opened
repolarization only restore electrical conditions not the ionic conditions which is restored by the ATP-Na-K-pump
ionic imbalances ain’t a problem until thousand of contractions
Ionic imbalances are fixed with Na K+ ATPase
once started it cannot be stopped
What are the steps of excitation contraction coupling
what happens after contraction is done (opposite)
The AP is carried along the sarcolemma down the T-tubules
AP reaches the area of T-tubules that has terminal cisterns which causes the the voltage sensitive tubule proteins on the T-tubules to change shape
This shape change opens the Ca2+ release channels in the terminal cisterns, allowing Ca2+ to flow into the cytosol.
Ca2+ binds to troponin
troponin rolls tropomyosin to groove of actin helix exposing it’s binding sites which allows them to bind to thick filaments
myosin binds and the next step starts
After math :
The voltage sensitive tubules return to normal shape which closes the Ca2+ channels
Ca2+ is actively pumped back to sarcoplasmic reticulum
without Ca2+ troponin returns to normal and the tropomyosin blocks the binding sites of acting
How many Ca2+ is required to expose the binding site of the actin filaments ?
2 Ca2+ molecules are required to bind to troponin
Cross bridge cycle
upright myosin binds to actin
It has ADP and Pi
ADP and Pi leave causing myosin and the actin to move
ATP binds which cause the Myosin to detach from actin
ATP is hydrolyzed to ADP and Pi and the myosin head becomes upright ready to bind to another actin
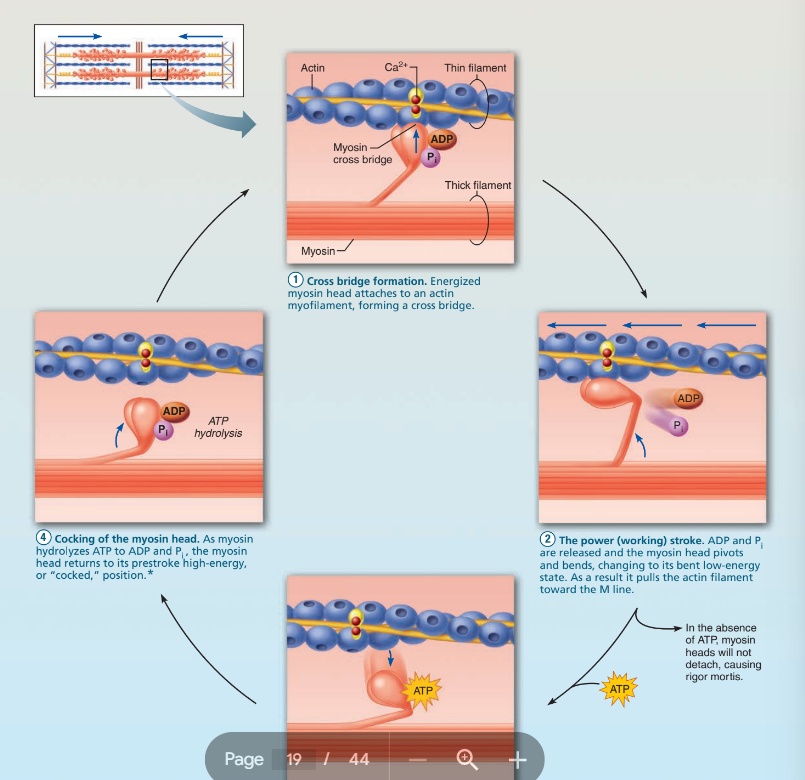
What is one disease related to that
what causes it
what are it’s sign
when does it end and why
rigor mortis
No ATP is present which means that the myosin head will not separate from the actin filament
dead people have fully contracted muscles even tho they are dead
after 3 days because the muscle proteins are broken down after death
What are the two main opposing forces called
Muscle tension : the force exerted by the muscle on the opposing force
Load: the weight of the object to be moved
What is a motor unit
what are the differences between different motor units
A motor unit consists of :
One motor neuron
all the muscle fibers it innervates
Differences in number of muscle fibers innervated in one motor unit :
Larger motor units focus on larger force production (calves)
smaller motor units focus on more precise movement (fingers)
what measures muscle contraction
what is the simplest type of contraction and what is it’s description
What are its phases and what occurs in them
what is unusual about the phases
a myogram
Muscle twitch: Muscle response to a single stimulation by which the muscle contracts quickly then relaxes
Three phases :
Stimulus
Latent period: Cross bridges begin to cycle but muscle tension not yet measurable
Period of contraction: number of active Cross bridges is increasing
period of relaxation: number of active Cross bridges is Decreasing
Note: different type of muscles have different period legnth
period of contraction is generally faster / shorter than the period of relaxation
Why is a muscle twitch not humanly
what contraction is of humans
what are it’s types
because it is sudden and produces robot movements
graded muscle contractions
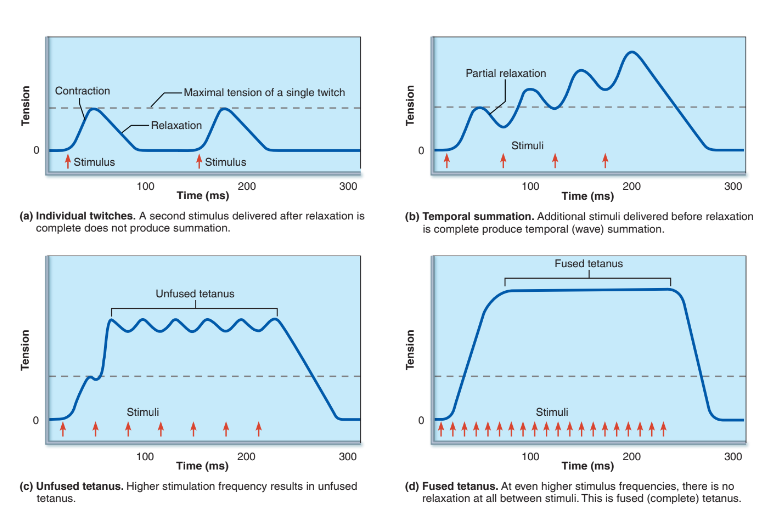
Temporal summation: Rate of firing of action potentials
Recruitment: Number of motor neurons that are activated
Temporal/wave summation :
What does it cause
What is the reason behind that function
What are the types draw their myograms
what types are rare and why
What is it’s primary function
is Increase in frequency of stimulation = stronger contraction by same muscles
because the second stimulus arrives before the Ca2+ is fully pumped back which means that the tension is still there which allows the second stimulus to ride on its back and produce stronger contraction
types are : in the picture
fused and unfused tetanus are rare because physiological mechanisms prevent it
To produce smooth, continuous muscle contractions
Recruitment
What is it also called
what is it’s function and how does it occur
How is it achieved in laboratory
what is threshold
what are the types of stimulus
why do different types exist
What principle dictates the recruitment and what does it explain
Multiple motor unit summation
Controls the force of contraction by :
Different motor units have different thresholds by which
According to stimulus intensity different motor units are recruited
Achieved by increasing voltage
Threshold is the point at which amount of depolarization required for the voltage gated channels to start an AP in muscle cells and start a contraction
Three types :
Subthreshold are APs that don’t cause contraction as they don’t cause depolarization enough to reach to threshold
threshold stimulus is the one that causes the first observable contraction
maximal stimulus is the strongest that causes all the muscle’s motor units to be recruited
because some acts don’t require that much force like muscles that maintain posture
Size principle :
Larger motor units require larger stimulus due to higher threshold stimuli
Smaller motor units are recruited first then the larger then the largest
How does the body prevent fatigue with the recruitment characteristic
Different motor units are activated at different times and not at the same time with different muscle fibers in the same muscle belonging to different motor units
What helps muscles be ready for contraction quickly
What is it exactly
what causes it
what are its benifits
Muscle tone
Muscles are always slightly contracted but doesn’t produce active movements
spinal reflexes which activate some motor units then another continuously
4
helps maintain muscles healthy
ready to respond to stimulation
stabilize joints
maintain posture
What are the types of contractions
What are the differences between them
what is the subdivisions of one
What are their differences
One example on each
which one is stronger
Why is two important and where it is used
On what does the classification depend
Types:
Isotonic : generates enough force (more than the load) to shorten (thin filaments move)
Concentric:
Shorten and does work like picking up a book
Eccentric:
Generation of force when it is lengthening like walking down a steep hill
Eccentric is stronger by 50 %
Isometric : generates force but doesn’t shorten or lengthen because the load needs more force than the muscle can generate (no movement of thin filaments)
Isometric is important for maintaining posture and holding joints stationary while movement occurs at other joints
Classification depends if muscle changes length or not
Where does energy come from initially and how long does it last?
What is the condition for the contraction to continue
what are the sources of regeneration
How do they work
Speed
how long do they last
hydrolysis of stored ATP which lasts for only 4- 6 seconds
ATP hydrolysis should be = to ATP regeneration
Regeneration occurs by :
Direct phosphorylation of ADP by creatine phosphate
Creatine phosphate transfers a phosphate group to ADP to form ATP
Fast
10 seconds (2 to 3 times more than ATP)
Enzyme is creatine kinase
Anaerobic pathway :
Glycolysis occurs to break down glucose without the presence of oxygen to 2 pyruvate molecules to produce 2 ATP and if there is no oxygen the pyruvate is converted to lactic acid
Fast
Lactic acid diffuses to blood stream into liver so that it can be converted to energy by liver and kidneys
lasts for 30-40 seconds
Aerobic respiration :
Glucose is broken down to pyruvate which is then broken down to CO2 and Water and 30 ATP
really slow
What is the legnth of time the muscle can continue to contract using aerobic pathways called
at which point does muscles convert to anaerobic metabolism
aerobic endurance
Anaerobic threshold (when ATP is needed quickly and aerobic respiration cannot provide enough in that time)
What metabolic processes do those activities rely on :
Lifting a 200 kg bench press for 3 sets
lifting 30 Kg bench press for 30 sets
lifting a 200 kg bench press for 12 sets
Creatine phosphate
Aerobic damn u gettin a pump
anaerobic (u will never do it anyway)
What is muscle fatigue
why does it happen
what causes it to happen
What happens because of that cause
what is assumed as a cause but isnt
what types of activities cause fatigue at what speed and healing at what speed
when the muscle is unable to contract even though the muscle is still receiving a stimulus
preventative mechanisms stop contraction in order not to cause complete depletion (rigor mortis and muscle death)
many causes but include :
Ionic imbalances : no more K+ in and too many Na+ in cause no AP to happen
increased organic pi caused by ATP and CP breakdown : interferes with Release of other pi from Myosin heads and release of Ca2+ from SR
Decreased ATP more Mg2+ : Mg2+ normally binds to ATP but with low ATP they bind to voltage sensitive proteins of T-tubules which cause Ca2+ release to decrease
Decreased glycogen : no more energy
Lactic acid is assumed as a major cause but it isn’t it just causes pain
two types of activities :
Strenuous but fast : fatigue fast : heal fast
Slow developing fatigue : fatigue slow : heal slow
what happens after the activity is done
What are it’s events
what is it also called
Excess postexercise oxygen consumption returns muscle chemistry back
Muscle’s myoglobin are reoxygenated
muscle’s glycogen stores are refilled
lactic acid is reconverted to pyruvate by liver
ATP and CP reserves are resynthesized
also called paying back the debt to muscles for their huge favor (oxygen debt)
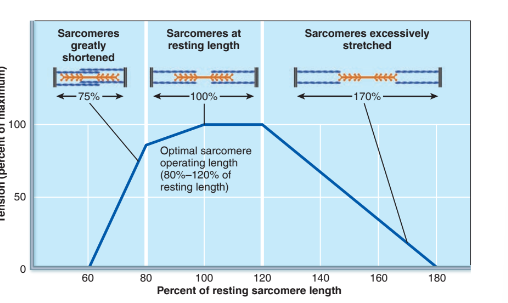
What does the force of a muscle contraction depend on
what is hypertrophy and what causes it
Depends on number of myosin cross bridges that are attached to actin which is affected by:
Frequency of stimulation : more = temporal summation = stronger
number of muscle fibers recruited
size of muscle fibers
degree of muscle stretch in picture:
More stretch = too far away from myosin heads to cause force
Less stretch = no where for actin filaments to go in center
Hypertrophy is caused by resistance exercises which causes enlargement of muscles
on what does the velocity and duration of contraction depend on
Muscle fiber type
size of the load
recruitment
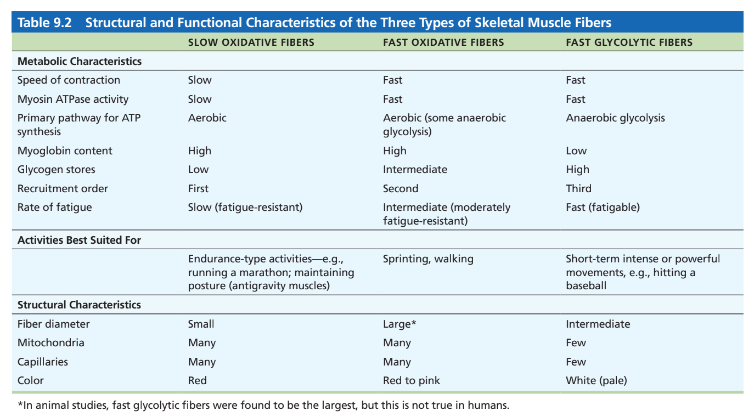
What does the classification of fiber types depend on :
Speed of contraction :
How fast does ATPase of myosin break down ATP
How quickly Ca2+ moves from cytosol to SR
it also show which pathway is used for generating ATP
Major pathways of forming ATP :
Glycolysis and CP or aerobic or both
What are the different types of muscle fibers
Compare them in
Speed of contraction
Myosin ATPase activity
primary pathway for ATP synthesis
Myoglobin content
glycogen stores
recruitment order
rate of fatigue
best suited activities
fiber diameter
mitochondria
capillaries
color
In the picture
What type of muscle fibers do muscles have mainly
what type of muscle does a motor unit have
they have a mixture between all three types but they depend on the person’s activity
they only have 1 muscle type
What are the different types of exercise
What do these exercises do to the body
Aerobic exercise (running to Qatar) :
More capillaries
More mitochondria
More myoglobin
in general they turn convert fast glycolytic to fast oxidative fibers
Resistance exercise (500kg / 3 sets) :
Fast oxidative to fast glycolytic
causes hypertrophy
return back to normal if stopped
What happens if muscles are not used
disuse atrophy (degeneration of muscles)
muscle fibers are replaced by fibrous connective tissue