Exam 4: Feline Liver Diseases
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms
what are the major liver diseases in cats
hepatic lipidosis
neutrophilic cholangitis
lymphocytic cholangitis
fluke associated cholangitis
portosystemic shunt or other vascular anomalies
generally define hepatic lipidosis in cats
the most common liver disease
metabolic syndrome that manifests with hepatocellular lipid overload
cytosolic distension with triglyceride causes intracellular dysfunction and extracellular compression of the canaliculi → cholestasis
what is the pathophysiology of hepatic lipidosis in cats
obligate carnivores
anorexia causes negative energy balance
lipids are mobilized to the liver to compensate for the energy deficit, but some cats inefficiently metabolisze triglycerides
occurs more in heavier cats
what defines primary hepatic lipidosis
anorexia due to decreased food availability , administration of non-palatable food, or stressful event
what defines secondary hepatic lipidosis
most common form
underlying disease such as pancreatitis, diabeters, cholangitis, chronic enteropathy, CKD, neoplasia causing anorexia
hospitalization causing anorexia
what is the typical clinical presentation of cats with hepatic lipidosis
middle aged (can occur in any age)
history of hypo/anorexia, vomiting, weight loss, diarrhea or lethargy
PE showing lethargy, mental obtundation, dehydration, hhepatomegaly, icertus
what is the adapted west haven grading scale for hepatic encephalopathy in cats
I= mild decrease in mobility and/or apathy
II= severe apathy (including mental obtundation) and or mild ataxia
III= combination of hypersalivation, severe ataxia, head pressing, blindness, and circling
IV= seizures and stupor or coma
how might hepatic lipidosis present on CBC
non specific changes
RBC= mild non-regenerative anemia ± poikilocytosis ± Heinz bodies
WBC ± mature neutrophilic leukocytosis
how might hepatic lipidosis present on biochemistry
most common and earliest abnormality is very increased ALP
hyperbilrubinemia, increased ALT and AST occur as progresses and with other disease
decreased K, Mg, Phos and mild hyperglycemia
GGT normal unless other disease
mild/moderate low albumin and high globulin may be present
how are ancillary diagnostics used for hepatic lipidosis
urine sediment frequently contains lipid
coagulation parameters may become progressively abnormal
ultrasound shows characteristic diffusely hyperechoic and large liver
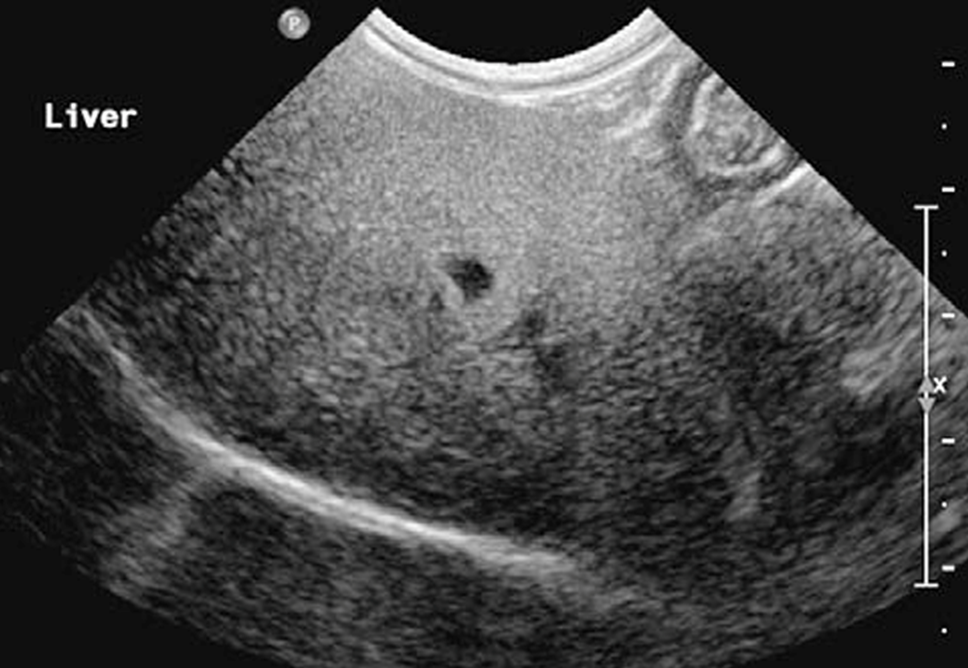
what disease is this a characteristic appearance for
hepatic lipidosis (hyperechoic)
how does hepatic lipidosis present on cytology
>80% hepatocytes contain lipid
unless there is a concern for primary hepatobiliary disease, a biopsy is not needed
give K1 before performing FNA
how is cholangitis generallyd escribed in cats
most common necro-inflammatory hepatobiliary disease
involves the portal system and biliary tract
inflammation of the bile ducts
what are comorbidities seen with cholangitis in cats
pancreatitis
inflammatory bowel disease
when a cat has cholangitis, pancreatitis, and IBD, what is the term used
Triaditis
what are the three subtypes of feline cholangitis
Neutrophilic (acute or chronic)
lymphocytic
Chronic fluke associated
what are the clinical signs of neutrophilic cholangitis
acute= fever, vomiting, inappetence, dehydration, jaundice, abdominal discomfort, hepatomegaly
chronic= overlaps clinically with acute but may be more insidious with waxing and waning clinical course
what lab abnormalities are seen with neutrophilic cholangitis
decreased PCV
increased WBC with left shift
Increased AST/ALT
increased GGT
± increased ALP
hyperbilirubinemia
± hyperglobulinemia, coagulopathy
how does neutrophilic cholangitis present on ultrasound
non-specific and may be normal
hyperechoic gallbladder contents, hyperechoic liver, enlarged pancreas
how does neutrophilic cholangitis present on bile cytology and culture
paired bile cytology and culture usually match but not always
E. coli most common
others include Enterococcus, Streptococcus, Clostridium, ect
what supplies are needed for pericutaneous ultrasound guided cholecystocentesis
22 g 1.5in needle or spinal needle
extension line
12-35cc syringe
EDTA tube for cytology
red top tube and culturettes for cultures
what is the technique used for percutaneous ultrasound guided cholecystocentesis
heavy sedation or general anesthesia
sterile surgical skin preparation
ultrasound guidance
right transhepatic approah
empty the gall bladder
check for leakage 2-6hrs later
what are the potential complications of cholecystocentesis
vasovagal response (be ready with IV cath, EKG monitoring, Blood pressure, ET tube, laryngoscope, atropine)
bile or septic peritonitis
hemorrhage → avoid the cystic artery
what are the pros to cholecystocentesis for cholangitis
confirmation of the diagnosis
necessary tool to design a treatment targeted correctly
what are the cons to performing a cholecystocentesis
complication risks
expensive
what is the etiology and association of lymphocytic cholangitis
loss of immune tolerance and targeting of bile ducts by the adaptive immune system
chronic pancreatitis often present
what is the typical presentation of lymphocytic cholangitis
cats of any age, breed or sex
history of chronic presentation with waxing and waning nonspecific clinical signs including lethargy, weight loss, hypo/anorexia, vomiting, polyphagia
PE showing hepatomegaly, icterus, ascites, poor body condition and muscle wasting, occasionally neuro signs
how does lymphocytic cholangitis present on bloodwork
± mild anemia
poikilocystosis commo
moderate to marked increased ALT and AST
± increased ALP and GGT
mild hyperglobulinemia
cyclic hyperbilirubinemia
how is lymphocytic cholangitis diagnosed
imaging, cytology of liver and bile non-specific
liver biopsy for histopathology required for definitive diagnosis
what is the occurance and signalment of cats presenting with congenital portosystemic shunts
less common than dogs
may occur in all breeds, though purebreeds may be at higher risk
what is the typically clinical presentation of cats with congenital portosystemic shunts
association with copper colored irius
neurological abnormalities present in most cats, but may wax and wane and induce or deteriorate after feeding
marked ptyalism is common
what are the lab abnormalities seen with congenital portosystemic shunts
CBC shows microcytosis
chem panel sees low BUN and infrequently low albumin and glucose. ALT and ALP can be normal to moderately increased
prolonged clotting times but often not correlated with clinical coagulopathy
UA shows low SG, ammonium biurate crystal s
how are congenital portosystemic shunts diagnosed inc ats
serum bile acids
abdominal ultrasound requires accuracy of operator
CT angiography standard imaging