37. Parathyroid and Calcium/Phosphorus Disorders
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
True or false: Calcium and phosphorus are regulated by the same mediators to maintain homeostasis.
true
What are the mediators of calcium and phosphorus?
P
C
V
P
parathyroid hormone
calcitonin
vitamin D
PTH related protein
In homeostasis, how are calcium and phosphorus related? What does this mean?
inversely; if calcium increases, phosphorus decreases and vice versa
What cells sense the decreased Ca levels? What do they secrete in response to this?
chief cells; parathyroid hormone (PTH)
What organs will PTH act on?
bone, intestine, and kidney
What is the affect of PTH on bone?
causes bone resorption (osteolysis) releasing Ca and PO4 into circulation (increases serum Ca and PO4)
What is the effect of PTH on the intestines?
promotes Ca resorption from the intestinal lumen (increases serum Ca)
What is the affect of Ca on the kidney?
promotes Ca retention and encourages PO4 excretion through urine (increases serum Ca and decreases PO4)
What cells sense the increase in Ca? What do they secrete in response to this?
c-cells; calcitonin
What is the affect of calcitonin on bone?
promotes bone production so decreases serum Ca and PO4
What is the affect of calcitonin on the intestine?
decreases intestinal absorption of Ca (decreases serum Ca)
What is the affect of calcitonin on the kidney?
tells kidney to waste Ca in the urine and retain PO4 (decreases serum Ca and increases PO4)
Overall, what is the net goal of calcitonin?
decrease serum Ca levels (PO4 will increase)
What are the key signals for the kidney to transform vitamin D?
decreased Ca and increased PTH
On what organs does vitamin D have an effect?
bone and intestine
What is the effect of vitamin D on the bone?
stimulates osteolysis so increases serum Ca and PO4
What is the effect of vitamin D on the intestine?
stimulates it to resorb Ca and PO4 so increases serum Ca and PO4
What are the big inhibitors of vitamin D?
increased Ca and PO4
What does binding of insulin to GLUT 4 receptor cause?
stimulates movement of K+ and PO4 intracellularly
What effect will massive amounts of tissue necrosis have on PO4?
will cause it to increase
What will the affect of hemolysis have on PO4 levels?
increases it
During lactation, what is lost in the milk?
Ca and PO4
What three fractions compose total calcium?
I
P
C
ionized or free calcium (~50%)
protein bound calcium (~40-45%)
calcium complexed with salts (~5-10%)
What percent of calcium is bound to albumin?
80%
What percent of calcium is bound to globulins?
20%
bioactive and available form of calcium which results in clinical signs of hypercalcemia
ionized calcium
How should elevations in total calcium be further investigated?
by performing an ionized calcium
What form of hyperparathyroidism is typically responsible for hypercalcemia? What is its effect?
primary hyperparathyroidism; increased Ca and decreased PO4
What is usually the main cause for the primary hyperparathyroidism? What are they often? What do they produce?
chief cell adenoma or carcinoma; functional tumors; PTH
What is humoral hypercalcemia of malignancy (HHM) also known as? What is its affect?
pseudo-hyperparathyroidism; increases Ca
What is the mechanism of action in HHM?
neoplastic cells produce PTHrP, which has a similar effect as PTH and thus has the same effects of PTH
What neoplasias are associated with PTHrP production?
A
L
V
anal sac gland adenocarcinoma (AGASACA)
lymphoma
various carcinomas
What should be run in pseudo-hyperparathyroidism? What is contained in this?
malignancy profile; PTH, iCa, PTHrP
What disease acts through the mechanism of PTHrP also? What does it do?
schistosomiasis; increases Ca
What is the process of hypervitaminosis D (vitamin D toxicosis), leading to hypercalcemia?
supplementation with vitamin D or vitamin D rodenticides → increased Ca and PO4 absorption from the gut and bone (increases Ca and PO4) → metastatic mineralization of tissues (kidneys, lungs, gut)
What is the mechanism of action of granulomatous disease in causing hypercalcemia?
acts through the vitamin D mediated mechanism (causes increased Ca and PO4)
What is the main form of granulomatous disease that causes hypercalcemia?
fungal disease (blastomycosis, cryptococcosis, histoplasmosis)
What is another type of granulomatous disease that causes hypercalcemia?
pulmonary angiostrongylosis
In horses, how will acute or chronic renal diseases appear?
increased Ca levels and WRI or decreased PO4
True or false: In health, the kidneys of equids excrete large amounts of Ca due to the lack of vitamin D mediated absorption of calcium through the gut and dietary intake.
true
What is the most common pattern of acute or chronic renal disease in dogs and cats?
WRI to decreased Ca and increased PO4
Acute hypercalcemic renal failure has been reported with what toxicosis?
raisin and grape toxicosis
What percent of dogs with chronic renal failure are hypercalcemic?
10-15%
Hypercalcemia associated with multiple myeloma is a ________ mechanism
different
What is the mechanism multiple myeloma uses to cause hypercalcemia? What is the value of iCa expected to be?
causes increased binding of calcium to globulins which increases the total calcium; WRI
What is the mechanism leading to hypercalcemia caused by hypoadrenocorticism?
not well known
What are the potential effects/clinical signs of hypercalcemia?
N
M
C
M
C
G
B
nephrogenic diabetes insipidus (polyuria)
metastatic mineralization (law of mass action)
calcium urolithasis
muscle tremors and weakness
CNS signs (depression, coma, seizures)
GI stasis
bradyarhythmias
According to the law of mass action, if Ca X PO4 is greater than what value is your patient at risk for metastatic mineralization of the tissues?
> 70
According to the law of mass action, if Ca X PO4 is greater than what value is your patient undergoing active mineralization?
> 100
What are the first tissues to mineralize?
K
L
G
kidneys (exacerbates renal disease)
lungs
GI tract
True or false: The law of mass action is the reason as to why low phosphorus diets or phosphate binders are a component of small animal prescription renal diets.
true
What is the most common cause of mild hypocalcemia?
hypoalbuminemia
Why does hypoalbuminemia result in hypocalcemia?
albumin is one of the major proteins that bind calcium, therefore a loss of albumin results in a loss of calcium
What is the effect of hypoparathyroidism?
decreased Ca and increased PO4
What forms of hypoparathyroidism cause hypocalcemia?
P
P
primary due to a damaged parathyroid gland
pseudo due to decreased PTH receptor sensitivity to calcium (grass tetany)
What is the effect of hypovitaminosis D?
decreased Ca and decreased PO4
What are reasons for hypovitaminosis D?
C
P
V
chronic renal disease
protein losing enteropathies (PLE)
vitamin D deficiency
occurs in ruminants grazing on lush spring pastures
hypomagnasemia (grass tetany)
What is the affect of grass tetany on calcium? How does it do this?
decreases it; produces a functional hypoparathyroid state (decreased PTH sensitivity)
What can. calcium mobilization associated with milk production result in? What is this called?
hypocalcemia; milk fever/puerperal tetany (eclampsia)
When are cattle most at risk for milk fever?
post parturient
When are small ruminants most at risk for milk fever?
peak lactation with multiple kids
What dogs are more likely to be at risk for milk fever?
small breed dogs with large litters
What is the affect of ethylene glycol toxicosis?
decreases Ca and increases PO4
What is the mechanism of action that ethylene glycol uses to cause hypocalcemia?
oxalates formed by metabolism of ethylene glycol bind calcium in the tubules → precipitates → renal injury
How does acute pancreatitis lead to hypocalcemia?
saponification of adipose
How does a urinary tract obstruction lead to hypocalcemia?
MOA not understood, but may be related to the increase in phosphorus
What is the effect blister beetles have on calcium? In what species does this occur?
causes hypocalcemia; horses
What are the clinical signs associated with hypocalcemia?
M
A
H
A
H
S
F
muscle fasciculations
anxiety, restlessness, or confusion
hypersensitivity to touch
aggression
hyperthermia
seizures and or tetany (ruminants will bloat)
face rubbing
What are three causes of hyperphosphatemia?
M
T
A
myopathies
tumor lysis syndrome
acromegaly
How do myopathies cause hyperphosphatemia?
induce injury or cause necrosis of skeletal myocytes releasing PO4 from the cell into the serum
How does tumor lysis syndrome cause hyperphosphatemia?
release of phosphorus from necrotic neoplastic cells
How does acromegaly cause hyperphosphatemia?
growth hormone increases tubular (kidney) resorption of PO4
What are two major reasons for hypophosphatemia?
F
P
fanconi syndrome
prolonged anorexia
hereditary defect reported in dogs (Basenji) that can be acquired
fanconi syndrome
What is the affect of fanconi syndrome?
causes decreased tubular resorption of glucose, amino acids, and PO4
Where is most magnesium found in the body? What percent?
bone; 60% of body stores
What percent of magnesium is found in soft tissue?
38%
What percent of magnesium is found in extracellular fluid and blood (plasma and RBCs)?
1-2%
What are the three major fractions of magnesium in the serum?
I
P
M
ionized or free magnesium
protein bound
magnesium complexed with salts
What percent of magnesium is ionized or free?
55%
What percent of magnesium is protein bound?
30%
What percent of magnesium is complexed with salts?
15%
What are the main causes for hypermagnesemia?
R
H
A
M
renal insufficiency or failure (decreased GFR)
hemolysis
administration of MgO, Mg(OH)2 in cattle, or MgSO4 in horses
milk fever
How does renal insufficiency or failure lead to hypermagnesemia?
decreased urinary excretion
How does hemolysis lead to hypermagnesemia?
shift of Mg from ICF to ECF
How does administration of MgO, Mg(OH)2 in cattle, or MgSO4 in horses lead to hypermagnesemia?
increased intestinal absorption of Mg
What is the main cause of hypomagnesemia?
hypoalbuminemia
What are other causes for hypomagnesemia?
P
G
E
I
K
B
prolonged anorexia or poor feed intake (cattle)
grass tetany (cattle or lactating mares)
enteric disease
increased GFR or osmotic diuresis
ketonuria
blister beetle (canthardin) toxicosis in horses
How does hypoalbuminemia lead to hypomagnesemia?
through hypoproteinemia
How does prolonged anorexia or poor feed intake (cattle), grass tetany (cattle or lactating mares), and enteric disease cause hypomagnesemia?
inadequate ruminal or intestinal absorption of Mg
How does increased GFR or osmotic diuresis and ketonuria cause hypomagnesemia?
excess excretion of Mg
What should be done if your patient is hypercalcemic or hypocalcemic?
perform an ionized calcium
What should be done if there are elevations in iCa?
malignancy panel (iCa, PTH, PTHrP)
What should be done if there are decreases in iCa?
treat and consider if further diagnostics are needed if persistent
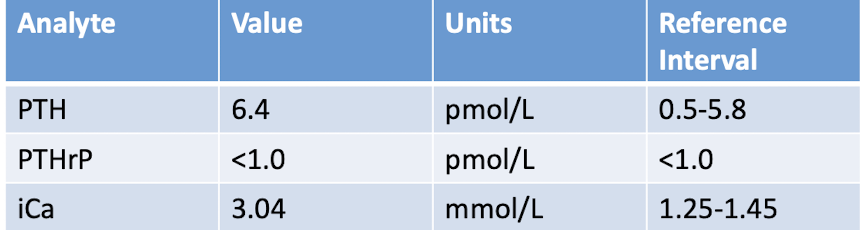
What are these results showing?
hypercalcemia due to a parathyroid related state
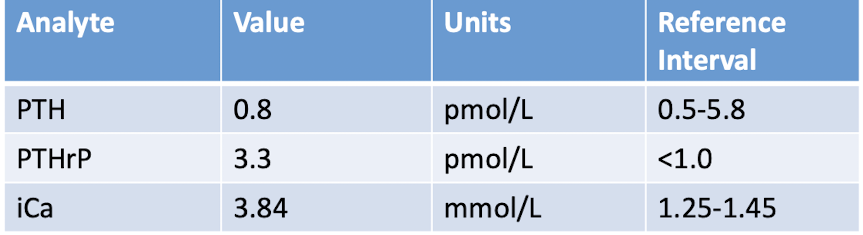
What are these results showing?
hypercalcemia due to humoral hypercalcemia of malignancy