95. Physiology | Hematopoiesis
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Where does hematopoiesis occur in the fetus?
Yolk sac (blood islands), liver (erythropoiesis), bone marrow (2nd trimester)
Where does hematopoiesis occur in the infant?
Bone marrow of all bones; all red marrow is active
What bones are active in hematopoiesis in adults?
Flat bones (vertebrae, sternum, ribs, skull), proximal femur/humerus
Red bone marrow fx
Hematopoiesis
Yellow bone marrow fx
Fat storage
When does yellow bone convert to red bone marrow
Under stress
Red bone marrow loc
Ends of long bones, flat bones
Yellow bone marrow loc
Shafts of long bones
How is bone marrow cellularity estimated?
100 - age ±10%
What defines normocellular marrow?
Age-appropriate cellularity
What defines hypercellular marrow?
Greater than expected cellularity, too little fat
What defines hypocellular marrow?
Less than expected cellularity
What defines aplastic marrow?
Severely hypocellular or absent hematopoiesis
What are the three lineages seen in bone marrow?
Myeloid, erythroid, and megakaryocytic precursors
What is the monophyletic theory of hematopoiesis?
All blood cells derive from a single pluripotent hematopoietic stem cell
What surface marker identifies hematopoietic stem cells?
CD34+
What is extramedullary hematopoiesis?
Blood cell production outside bone marrow (e.g., liver, spleen, nodes)
What causes extramedullary hematopoiesis?
Bone marrow unable to meet blood cell production needs
What does CFU-E give rise to?
Erythrocytes
Which cytokine stimulates CFU-Meg to produce megakaryocytes?
Thrombopoietin (TPO)
What does CFU-GM give rise to?
Granulocytes (neutrophils, eosinophils), monocytes
What does CFU-Eo produce?
Eosinophils
What does CFU-B produce?
Basophils
What does CFU-L give rise to?
T and B lymphocytes
Which cytokine promotes stem cell proliferation?
IL-3
Which cytokine activates eosinophils and CFU-Eo?
IL-5
What does erythropoietin stimulate?
CFU-E to erythrocytes
Where is erythropoietin made?
Peritubular capillary endothelium of the kidney
Where is thrombopoietin made?
Kidney and liver
What stimulates B/T cell activation and mast/basophil development?
IL-4
What is the first stage in granulocyte development?
Myeloblast
What are the features of a myeloblast?
Large cell, basophilic cytoplasm, round nucleus, 3–5 nucleoli, no granules
What granules appear in promyelocytes?
Azurophilic (primary) granules
When do specific secondary granules begin forming?
Myelocyte stage
What defines a metamyelocyte?
Kidney-bean shaped nucleus, visible specific granules
What defines a band cell?
Horseshoe-shaped nucleus (seen in peripheral blood)
What defines a segmented PMN?
2–4 nuclear lobes (mature neutrophil)
When can eosinophils and basophils be distinguished?
Late myelocyte or early metamyelocyte stage
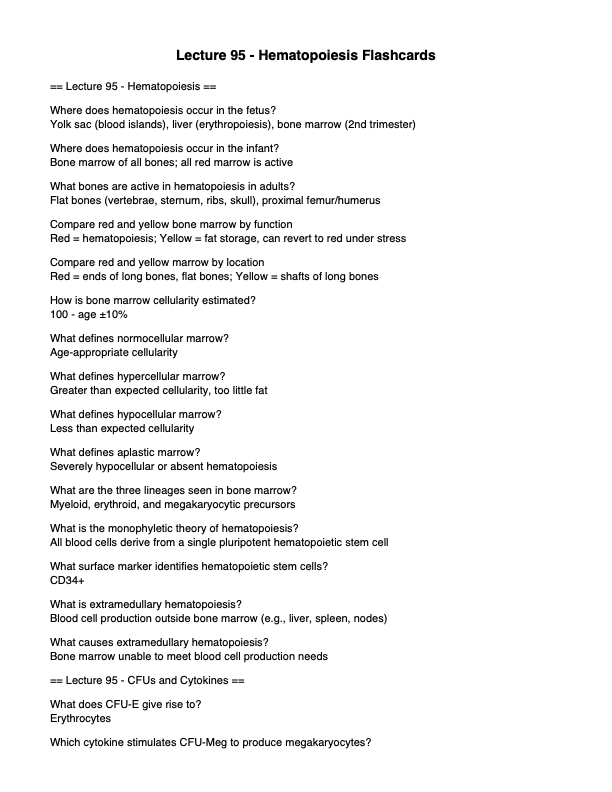
What is the first stage in erythropoiesis?
Proerythroblast
What is the progression of stages in erythropoiesis?
Proerythoblast → basophilic erythroblast → polychromatophilic ery → normoblast (orthochromatophilic ery)
What is the progression of stages in macrophage development?
Monoblast → Promonocyte → Monocyte/Macrophage Development
What are the features of a proerythroblast?
Large nucleus, basophilic cytoplasm, 1–2 nucleoli
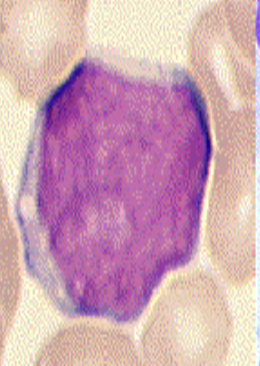
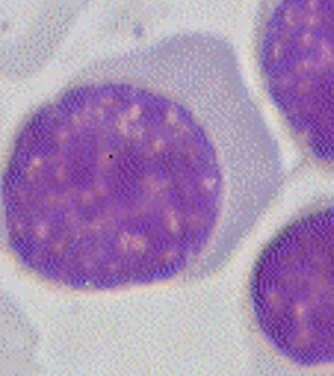
What is characteristic of a basophilic erythroblast?
Deep blue cytoplasm from ribosomes
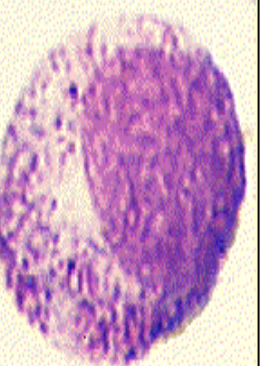
What is characteristic of a polychromatophilic erythroblast?
Mixed blue-pink cytoplasm due to hemoglobin and RNA
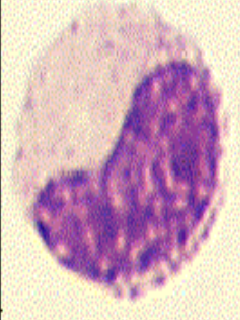
What defines a normoblast?
Small dense nucleus, pink cytoplasm
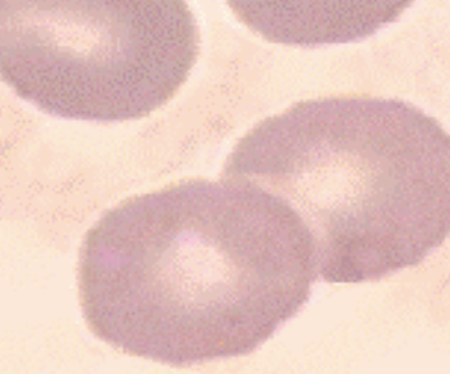
What defines a reticulocyte?
Anucleate, residual ribosomes, 1–2% in peripheral blood
What stimulates erythropoiesis?
EPO, GM-CSF, IL-3, IL-4
What differentiates a reticulocyte from a mature erythrocyte?
Reticulocyte has residual ribosomes; erythrocyte has no nucleus or organelles
What is the first precursor of platelets?
Megakaryoblast
What are the features of a megakaryoblast?
Large cell, single round non-lobed nucleus
What occurs in a promegakaryocyte?
Nucleus becomes multilobed
What defines a mature megakaryocyte?
Very large, multilobed nucleus, platelet demarcation zones
What are platelets derived from?
Fragments of megakaryocytes
What is the function of platelets?
Form primary hemostatic plug
What stimulates thrombopoiesis?
Thrombopoietin, GM-CSF, IL-3
What is stimulated by Thrombopoietin, GM-CSF, IL-3?
CFU-GEMM
What is the lifespan of a platelet?
~10 days
Myeloblast
Promyelocyte

Myelocyte
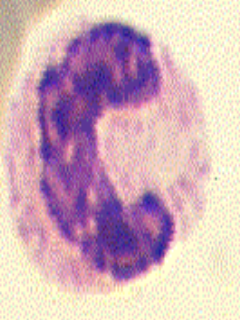
Metamyelocyte
Band
Segment

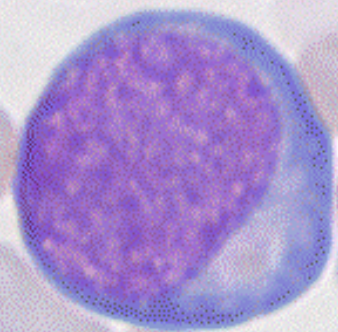
Proerythroblast
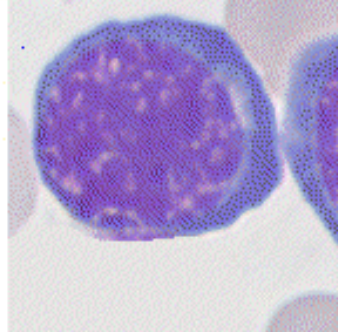
Basophilic Normoblast
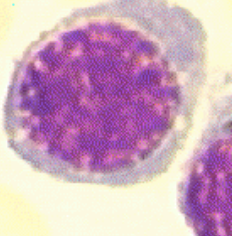
Polychromatic Normoblast
Orthochromatic Normoblast
Reticulocyte

Erythrocyte
A 72-year-old woman with fatigue and pallor is found to have anemia. Bone marrow biopsy shows increased erythroid precursors and elevated reticulocyte count. What is the most likely explanation for this marrow finding?
A. Iron-deficiency anemia
B. Megaloblastic anemia
C. Erythroid hyperplasia due to blood loss
D. Aplastic anemia
E. Leukemia
C
A. Iron-deficiency anemia – Would show ineffective erythropoiesis, not increased reticulocytes.
B. Megaloblastic anemia – Marrow may be hypercellular, but reticulocyte count is not elevated due to ineffective erythropoiesis.
C. Erythroid hyperplasia due to blood loss – Correct. Erythroid lineage expansion and reticulocytosis are signs of a compensatory response.
D. Aplastic anemia – Marrow would be hypo- or acellular.
E. Leukemia – Marrow would show blast predominance, not increased erythroid precursors.
A hematopathologist is evaluating a cell that contains both basophilic and eosinophilic cytoplasm (appears lilac/grey) and a smaller, coarse nucleus. This stage of erythroid maturation corresponds to which of the following?
Answer Choices:
A. Proerythroblast
B. Basophilic erythroblast
C. Polychromatophilic erythroblast
D. Normoblast (orthochromatophilic erythroblast)
E. Reticulocyte
C
A. Proerythroblast – Very basophilic, large nucleus, nucleoli present.
B. Basophilic erythroblast – Deep blue cytoplasm, no pink tint yet.
C. Polychromatophilic erythroblast – Correct. Cytoplasm stains grey/lilac due to mix of basophilia (ribosomes) and acidophilia (hemoglobin).
D. Normoblast – More eosinophilic (pink), nucleus is small and dark.
E. Reticulocyte – Nucleus is gone; still has some residual RNA (polychromasia on stain).
A 55-year-old man presents with easy bruising and a low platelet count. Bone marrow biopsy reveals a multilobulated cell with azurophilic granules and platelet demarcation channels. What is the most likely identity of this cell?
Answer Choices:
A. Megakaryoblast
B. Monoblast
C. Megakaryocyte
D. Promyelocyte
E. Pro-megakaryocyte
C
A. Megakaryoblast – Early precursor with non-lobulated nucleus.
B. Monoblast – Precursor to monocyte, no platelet production.
C. Megakaryocyte – Correct. Large cell, multilobulated nucleus, forms platelets via demarcation channels.
D. Promyelocyte – Early myeloid precursor, not platelet lineage.
E. Pro-megakaryocyte – Intermediate, but nucleus not yet multilobulated.
A medical student observes a bone marrow slide containing large cells with a non-lobulated nucleus and no cytoplasmic granules. These cells are committed to the thrombocytic lineage. Which cell is she most likely observing?
Answer Choices:
A. Pro-megakaryocyte
B. Megakaryocyte
C. Megakaryoblast
D. Promyelocyte
E. Erythroblast
C
A 3-year-old boy presents with persistent asthma and eczema. CBC reveals a normal leukocyte count but with elevated eosinophils and basophils. Which of the following interleukins is most associated with promoting eosinophil activation?
Answer Choices:
A. IL-2
B. IL-4
C. IL-5
D. IL-6
E. IL-1
C
A. IL-2 – Promotes T and B cell proliferation.
B. IL-4 – Stimulates B and T cells, development of mast cells/basophils, but not eosinophils.
C. IL-5 – Correct. Directly promotes CFU-Eo mitosis and activates eosinophils.
D. IL-6 – Involved in acute-phase response, not specific to eosinophils.
E. IL-1 – Promotes stem cell proliferation, but not eosinophil-specific.