chronic kidney disease
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
what is chronic kidney disease (CKD)
slowly-developing progressive and irreversible loss in kidney function that can occur over months or years
difference between CKD and AKD (acute kidney disease)
AKD is reversible whereas CKD involves irreversible damage
in CKD, reduction of kidney function must be present for over 3 months
what are the causes/factors that increase risk of CKD
increasing age - 65+
family history
african-caribbean or south asian ethnicity
kidney infections - less common
inflammation (glomerulonephritis) - less common
urinary blockages
prolonged use of certain meds like NSAIDs
long term conditions like diabetes
heart disease
obesity (BMI>30)
high cholesterol/ high fat diet
high blood pressure
symptoms of CKD
high blood pressure
changes in urinary frequency e.g. particularly at night
changes in appearance of urine
leg/ankle/hand oedema
tiredness/lack of energy
erectile dysfunction
weight loss/poor appetite
muscle cramps
headaches
shortness of breath
nausea and vomiting
metabolic taste in mouth
as the kidney function progressively declines, what happens to:
symptoms
size of kidneys
symptoms worsen gradually
shrink in size the more damaged they become

how is CKD classified
5 stages:
stage 1 = mildest
stage 5 = severe with poor life expentency if left untreated
end-stage kidney disease
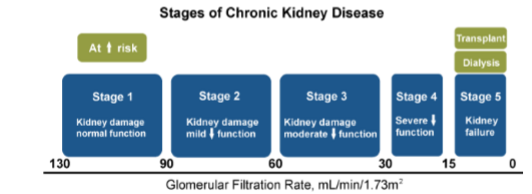
describe the GFR in early stage kidney failure
GFR may be normal or higher:
>90 for stage 1
60-89 for stage 2
how might early kidney failure develop
due to changes in blood flow to parts of kidney caused by local damage or blockages (e.g. kidney stones) could affect renal function
true or false: in early stage kidney failure, there is no obvious symptoms and blood/urine tests can be normal
true
when looking at blood/urine tests/kidney function tests, what indicates middle stage kidney failure
abnormal levels of waste products in blood
GFR may be decreased → 30-59 for stage 3
what symptoms does the patient experience with middle stage kidney failure
increase in urine freq
increased BP
weakness, fatigue and shortness of breath
in middle stage kidney failure, what increases the risk of cardiovascular disease
increased BP
why might patient with middle stage kidney failure feel weak, tired and shortness of breath
because anaemia may develop as erythropoetic function of kidney decreases
what is the GFR in later stage kidney failure
15-29 for stage 4
what are the symptoms in later stage kidney failure
increased BP
increased urination freq
increased tiredness/reduced appetite
what is the GFR for end-stage kidney disease
GFR < 15 for stage 5
true or false: in end-stage kidney disease, kidney function is reduced to 20-25% of its capacity
false - reduced to 10-15%
what happens in end-stage kidney disease
waste products are not adequately filtered
excess water not removed
what treatment options can be given to end-stage kidney disease
dialysis
kidney transplant
how is CKD diagnosed
by carrying out routine screening of patient with recognised risk of developing kidney problems
creatinine blood tests are used to identify CKD - what is creatinine
normal waste product produced from creatine generated from muscle metabolism
why does higher blood levels of creatinine indicate a lower GFR
because normally in a healthy functioning kidney, creatinine is transported through bloodstream to kidneys where most of it is filtered out and disposed of it in urine
what is the normal blood creatinine levels in:
males
females
males: 59-104 μmol/L
females: 45-84 μmol/L
what does blood creatinine levels > 104μmol/L in males or 84μmol/L indicate
severe kidney impairment - need for dialysis
what is creatinine clearance
amount of creatinine passed in the urine over 24hrs
does low or high creatinine clearance indicate CKD
low
normal creatinine levels are 500-2000 mg/24hr
what are creatinine levels used to calculate
eGFR (mL/min)
estimate for GFR
what is the formula used to calculate eGFR

what are the types of blood/urine tests for kidney function
urea blood and urine tests
albumin blood and urine tests
[high/low] blood urea indicates kidney dysfunction - why
high because urea is normally excreted in the urine
what is the normal urine urea level
165-583 mmol/24hr
what is albumin
major protein synthesised by liver which makes up 55-60% of total plasma protein
importance of albumin
many hormones, drugs and other molecules are carried in the bloodstream bound to albumin from which they must be released to exert biological activity
is albumin blood levels high or low why there is renal dysfunction
low albumin blood levels because it is excreted in urine cause hypoalbuminemia
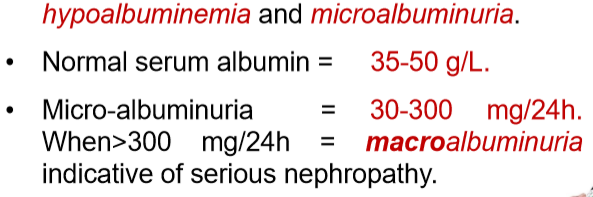
true or false: the urine albumin to creatinine ratio (ACR) is used as a kidney function marker
true
ACR ratio < 30mg/g = abnormal or normal
ACR > 30mg/g = abnormal or normal
ACR ratio < 30mg/g = normal
ACR > 30mg/g = abnormal → indicates early sign of kidney disease
why are urine dipstick tests not used anymore
urine dipstick tests are used to measure presence of protein in urine but not used due to unoptimal sensitivity and specificity
why is hyperkalaemia an indication of kidney damage
what is it
how can it occur
what are the symptoms
normal levels
high potassium levels
when GFR < 20-25 - kidneys have very reduced ability to excrete K+
malaise, cardiac arrhythmias
3.5-5mmol/L
why is hyperphosphatemia an indication of kidney damage
what is it
how can it occur
what are the symptoms
normal levels
high phosphate levels accumulating in blood
due to reduced urinary phosphate excretion when GFR is decreased
increased risk of CVD, itching
0.81-1.45 mmol/L
why is hypocalcaemia an indication of kidney damage
what is it
how can it occur
what are the symptoms
normal levels
deficiency of calcium in blood
calcitroil is active metabolite of vitamin D synthesised in kidney under control of parathyroid hormone (PTH) - this conversion is compromised when kidney function is impaired
CKD causes increase PTH levels which results in excessive resorption of Ca2) from bones → increased risk of bone fractures
why is metabolic acidosis an indication of kidney damage
what is it
how can it occur
what are the symptoms
normal levels
low plasma pH level < 7.35 and low HCO3- level
due to blood accumulation of sulphates, phosphates and uric acid, decreased NH4+ from proximal tubule cells alter enzyme acitivity
normal levels of serum bicarbonate is 22-29mmol/L
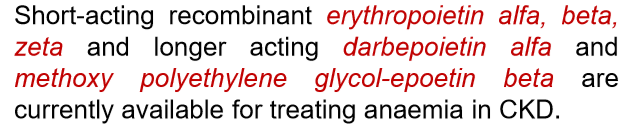
what causes iron deficiency anaemia (indication of kidney damage)
caused by reduction in renal erythropoietin synthesis
what is urine sediment abnormalities (indication of kidney damage)
urine sediments are red blood cells, cellular debris, fat and filtered proteins present in urine
these are the different imaging tests:
renal ultrasonography
(only answer the ones about the ones in bold)
what does this screen for
screens for kidney abnormalities, size, obstruction (stones) and tumours
(only answer the questions about the one in bold)
these are the different imaging tests:
renal ultrasonography
retrograde ureteroscopy
how is this performed
performed by inserting cystoscope into urethra and bladder → then injection of x-ray contrast medium through catheter into ureter and imagaging
true or false: retrograde ureteroscopy are useful for diagnosing renal stones
true
(only answer the questions about the one in bold)
these are the different imaging tests:
renal ultrasonography
retrograde ureteroscopy
CT scanning - uses computer-processed x-rays
why is there an allergy issue involving CT scans
because a dye is given to patient before the CT scan - dye contains iodine so always ask patients first if they are allergic to iodine
what imaging technique can be used in patients who cannot receive I/V contrast agents (iodine)
MRI scanning - uses powerful magnets and computer-processed radio waves
(only answer the questions about the one in bold)
these are the different imaging tests:
renal ultrasonography
retrograde ureteroscopy
CT scanning - uses computer-processed x-rays
x-ray scanning
what do x-rays reveal
opaque kidney stones
(only answer the questions about the one in bold)
these are the different imaging tests:
renal ultrasonography
retrograde ureteroscopy
CT scanning - uses computer-processed x-rays
x-ray scanning
renal radionuclide scanning
how does this work
uses MAG3 or DMSA chelated with 99mTc (gamma emitter) to confirm renal blood flow so is used for screening for renal artery stenosis
treatment of CKD
next couple of flashcards
what conditions do patients with CKD have a higher risk of developing
atherosclerosis and cardiovascular disease e.g. heart disease like hyperlipidaemia
true or false: there is no specific medicine for CKD management - it is more focused on preventing cardiovascular events and minimising further decline in renal function stage 5
true
treatment of CKD aims to control blood pressure - how
ACEIs e.g. ramipril, enalapril
ARBs (angiotensin II receptor antagonists) e.g. valsartan, losartan
monitoring serum K+ to check for hyperkalaemia
treatment of CKD aims to treat hyperlipidaemia - what med is used for this
statins e.g. atorvastatin
treatment of CKD aims to control oedema - what med is used for this
treated with loop diuretic e.g. furosemide
what is used to correct vitamin D deficiency
calcitriol replacement therapy
what can be given to reduce fatigue
treatment with i/v iron and erythropoeitin which normalises Hb
why are phosphate binders given
controls serum phosphate in CKD patients
when CKD patient reaches stage 5, renal replacement therapy is required - what does this involve
haemodialysis or peritoneal dialysis
renal transplant
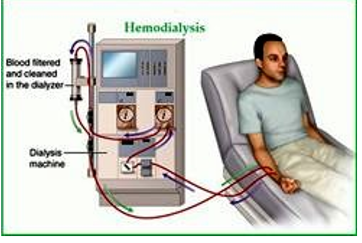
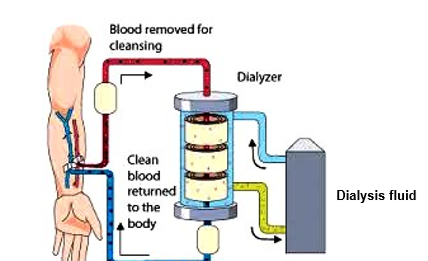
what is haemodialysis
method whereby waste products (e.g. creatinine and urea) and free water which build up in the blood can be removed in absence of adequate kidney function
how often is haemodialysis carried out per week
3 times a week
how is haemodialysis set up
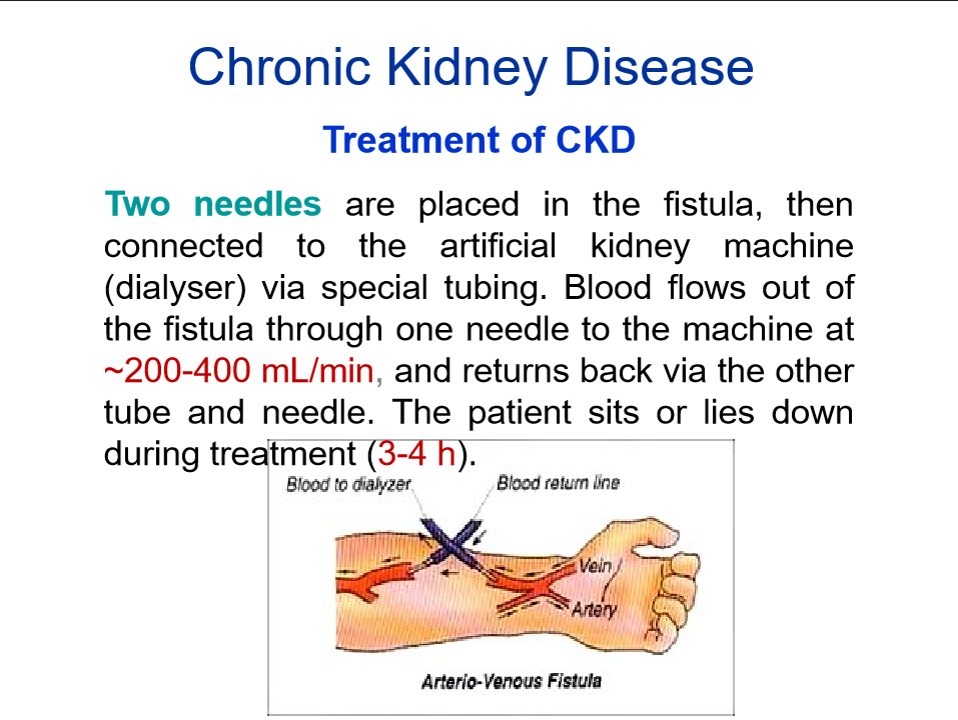
what is the main objective in haemodialysis
patients blood is pumped through dialyser and continuously fed with saline dialysate solution, ‘cleans’ it and then pumps it back into patients circulation
the dialyser consists of 2 compartments
blood
dialysate
separated by semi-permeable membrane
what drives the fluid from the blood from one compartment to another through the membrane
pressure gradient
what allows for the multiple use of dialyser by the same patient
the autoclean facility disinfects dialyser membrane and compartments
features of intensive home haemodialysis
what is peritoneal dialysis
uses patients peritoneal ‘barrier membrane’ across which excess body fluids and dissolved waste substances are exchanged by osmosis/diffusion from blood into peritoneal dialysis solution
fluid is introduced through permanent catheter in abdomen and drained after every night
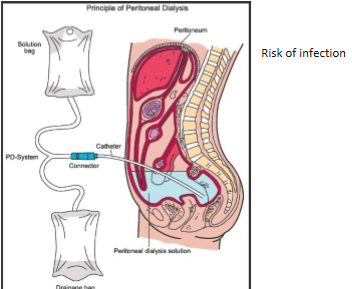
what is the peritoneal membrane
transparent serous membrane lining walls of abdominal cavity and enclosing digestive organs in abdomen
any fluid that escapes peritoneal capillaries into abdominal cavity is reabsorbed back into circulation via lymphatic