MED SURG Exam 3 Kidneys
1/138
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
139 Terms
kidneys
The kidneys are the principal organs of
the urinary system.
the kidneys function to...
-Regulate the volume & composition of
extracellular fluid (ECF): fluid exchange is a critical component of kidneys
-excrete waste products from the body: filtration from the glomerulus
-Regulate BP: RAAS
-Produce erythropoietin: without it there are no stem cells to build RBCs=anemia!!
-activate vitamin D: allows calcium to be absorbed
-regulate acid-base balance: metabolic vs respiratory
Renin-Angiotensin-Aldosterone System (RAAS)
•Renin is secreted in response to HYPOtension
•Renin activates angiotensinogen to angiotensin
•Angiotensin I is converted to angiotensin II by ACE in the lungs
•Angiotensin II stimulates the release of aldosterone: causes reabsorption of Na and water and vasoconstriction thus increased BP
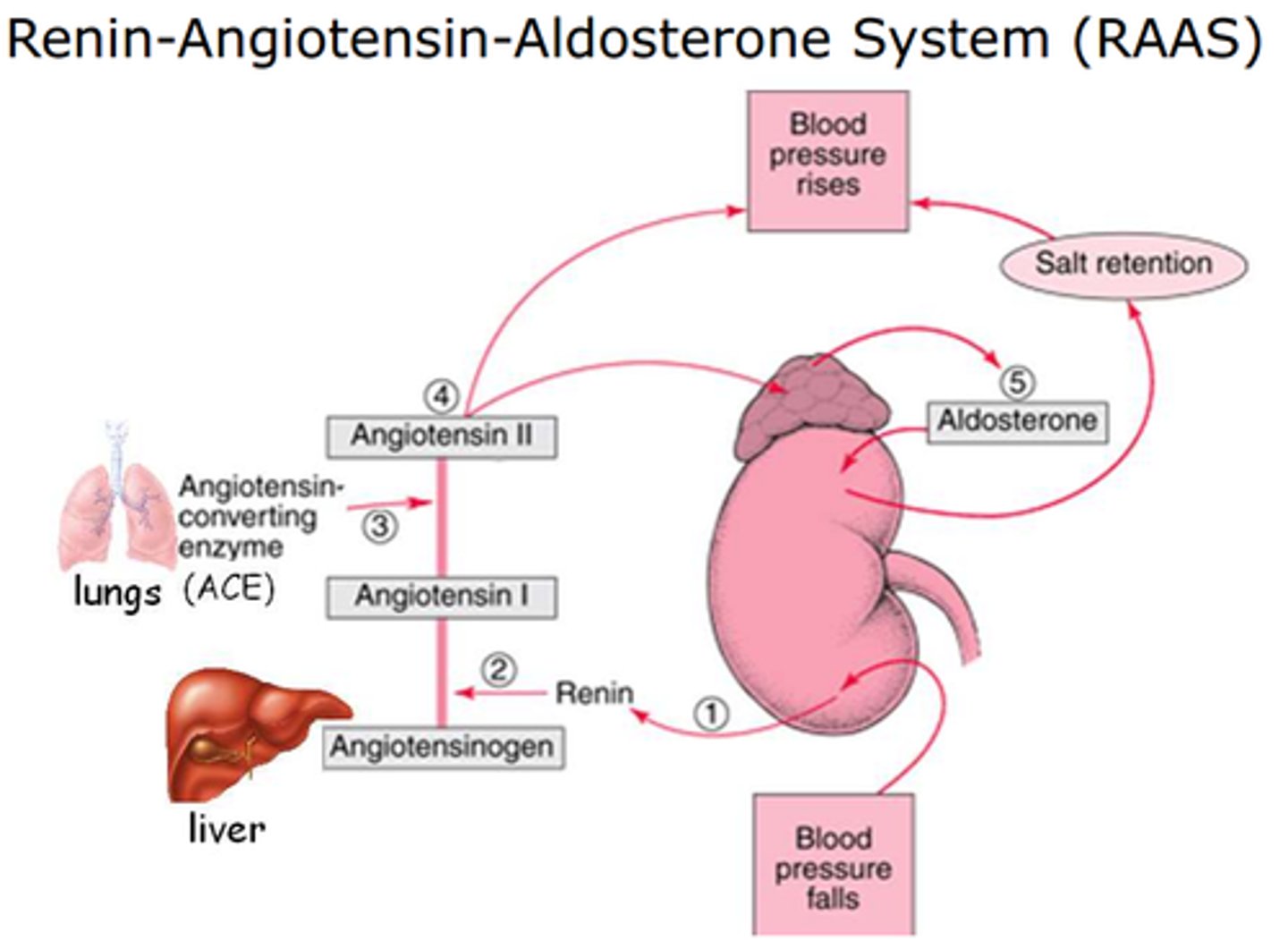
overproduction of the RAAS system
-leads to kidney disease
-LOWER with ACEI**
The nephron is the function unit of the kidney
-Each kidney has approx. 1,000,000 nephrons
-The kidneys receive 20-25% of cardiac output
GFR
-(glomerular filtration rate) The rate at which the kidneys filter blood
-Normal GFR = >90 mL /min (90-120)
BUN
-Blood Urea Nitrogen (BUN)
-Normal: 6-20 mg/dl
-fluctuates with dehydration/hydration/hyper/hypovolemia
creatinine
-normal: 0.6-1.3 mg/dl
-Creatinine is a more sensitive indicator than BUN
**more indicative of renal function
BUN to creatinine ratio
BUN to Creatinine ratio should be 10-20:1
creatinine clearance
-87-139 mL/min
-ALSO draw a blood sample and compare to get eGFR (estimated)
-the most sensitive indicator of renal function
-Creatinine clearance approximates the GFR: if creatinine clearance is 98 then GFR IS 98!!!
process of obtaining creatinine clearance
-24 h specimen of urine
-1st void 7 am = discard it
-every pee from then until the end of 24 h pee last time and collect in container over ice throughout the process
-send urine to lab AND draw a blood sample for comparison
-estimate creatinine clearance by looking at VOLUME and AMOUNT of creatinine!!!
-compare/contrast to get eGFR (hopefully between 90-120)
nephrolithiasis
-kidney stones
-can occur anywhere in the renal system from the beans, ureters, bladder, and to the urethra
information about kidney stones
-Approx. 1-2 million cases annually in US
-Highest incidence in the US Southeast & Southwest followed by the Midwest
-More common in summer season
-dehydration plays a role: drink 1-2 L of clear liquids daily to PREVENT renal calculi
-More common in Caucasians than African Americans
-Most prevalent between Ages 20 and 55
-More prevalent if genetic history exists
etiology of renal calculi: urinary pH
-the higher the pH (alkaline), the less soluble are calcium and phosphate: alkaline urine grows calcium and phosphate stones!! **we'd want to make the urine acidic to prevent (cran juice)
-the lower the pH (acidic) the less soluble are uric acid and cystine: acidic urine grows uric acid and cystine stones!! **we'd want to make the urine alkaline to prevent (potassium citrate)
etiology of renal calculi: bacterial infections
-we can see urea-splitting bacteria (Proteus, Klebsiella, Pseudomonas, some staph) contributing to stone formation
-bacterial infections cause renal calculi and renal calculi cause bacterial infections: they EXACERBATE each other!!
-Infected stones can be seen (indwelling caths, neurogenic bladder, urinary retention)...these need to be removed.
-those who have UTI's are more prone to having calculi and the opposite
calcium phosphate renal calculi: causes
-8 to 10%
-Predisposing factors: alkaline urine!! (want to make it more acidic; drink cranberry juice)
-Primary hyperparathyroidism: causes resorption of calcium outside the bones, increasing calcium levels, potentially causing stones **fix this to fix stone formation
therapeutic measures for calcium phosphate stones
-Treat underlying cause
-Increase Hydration (really for all types of stones)
-Cranberry Juice to make more ACIDIC
-Increase Foods high in Calcium: NOT calcium supplements....eating foods high in calcium binds with oxalate in the vasculature to prevent oxalate from binding in the kidneys causing stones
-Decrease Sodium: we want to increase the intravascular volume, sodium pulls water out of the vascular and into the interstitial spaces
-Decrease food high in animal protein: protein is hard on the kidneys, and there's more potential for stone stasis
calcium oxalate renal calculi: causes
-70 to 80%
-Family history
-INDEPENDENT of urinary pH!!! drink a lot of fluid (juice, water, OJ...doesn't matter what you drink just drink a lot of it...except alcohol)
-Idiopathic hypercalciuria and hyperoxaluria
therapeutic interventions for calcium oxalate renal calculi
-Increase hydration, decrease oxalates
-Decrease sodium and animal protein
-Thiazide diuretics: pulls calcium in and sodium out to decrease the chances of calcium binding with oxalate and forming stones
-Avoid Vitamin C Supplements (can increase oxalate levels)
-Increase calcium in foods but not calcium supplements
decrease foods high in oxalate to lessen formation of calcium oxalate stones
-Spinach, rhubarb, asparagus
-Nuts, Cabbage, tomatoes, beets
-Chocolate, tea
-Worcestershire sauce, parsley
uric acid renal calculi: causes
-5 to 8%
-Male, especially Jewish males
-GOUT
-acidic urine: make it more alkaline!!
-genetics
**too many purines coming in or not getting rid of enough uric acid (either an issue with the renal system or an ingestion habbit)
therapeutic interventions for uric acid renal calculi
-Increase Hydration
-Decrease urinary concentration of uric acid
-Alkalinize urine with K citrate - (binds K out- potassium is an acid)
-Give allopurinol: decreases formation of crystals from excess urine and rids uric acid...helps with gout too
-Decrease urinary purines
avoid foods high and moderate in purines for uric acid stones
-Sardines, herring, mussels
-Meat based soups
-Organ meat - sweetbreads, kidney, liver
-Game - goose, venison
cystine renal calculi: causes
•1 to 2%
•Genetic predisposition
•Defective absorption of cystine in GI tract and kidney: so it is transferred to the renal calculi (meatus of the kidneys) and stones form
•Acidic urine: make it more alkaline!!
therapeutic interventions for cystine renal calculi
•Increase hydration
•Alpha penicillamine and tiopronin to prevent cystine crystallization: binds cysteine so it can go through the GI tract without being absorbed in the vascular system and kidneys
•K citrate to alkalinize the urine (bind K/acid out)
struvite renal calculi causes
-10 to 15%
-3-4 times more common in women than men
-always after UTI (usually Proteus)
-alkaline Urine: want to make more acidic
therapeutic interventions for struvite renal calculi
-Antimicrobials
-Acetohydroxamic acid (Lithostat) indirectly lowers urine pH.
-Surgical removal
-Acidify urine: cranberry juice
-HYDRATION: which is also good for UTIs!!
symptoms of kidney stones
-Severe back and/or flank pain
-hematuria
-May see nausea and vomiting
-Colicky, intense pain as it passes through the ureter
-May see signs of shock- cool, moist skin
-Ureterovesical junction (UVJ): pain may radiate into the testicles, labia or groin
static stones people may experience
-more colicky pain which excruciating pain as the stone moves
-with stasis of stones there can be renal occlusions resulting in infection or AKI
most people pass stones d/t fluid and movement
:)
diagnosis of renal calculi: urinalysis
-check pH, check for WBC's, RBC's
-assessing for hematuria and crystalluria
diagnosis of renal calculi: Labs
BUN and creatinine, WBC, Urinalysis, urine culture, creatinine clearance
diagnosis of renal calculi: ultrasound
usually when they find the stone
diagnosis of renal calculi: CT scans
-Most common dx tool now used is noncontrast helical CT scan
-once we've done ultrasound and suspect a stone we do CT
diagnosis of renal calculi: cystoscopy
-lighted scope, to inspect the interior of the bladder (cysto means bladder)...looking for the stone
-generally not done unless stone seen on CT as this is INVASIVE
-General or local anesthesia.
intravenous pyelogram
-(pyelo means kidney)
-Confirms site and size or stone
-Done with IV contrast
-Do not perform on patients with known kidney failure as the kidneys can't handle the contrast.
retrograde pyelogram
x-ray of the urinary tract with much less dye than an IVP
conservative treatment for removal of renal calculi
•Increase hydration
•Alpha Adrenergic Blocker (Flomax) to relax smooth muscle in ureter
•Pain management, helps patient move around and hopefully move the stone
•if less than 5 mm, will usually pass conservatively
**this is what we DESIRE**
Endourological procedure or Lithotripsy if
•If stones are too large (5 mm or larger)**done rapidly to prevent AKI from blockage, we do NOT want urine stasis
•Stones with symptomatic infection
•Stones causing impaired renal function
•Stones causing persistent pain, nausea or paralytic ileus
•Patient is unable to be treated medically
•Patient has only one kidney
Removal by Cystoscopy endourologic procedures
*this process could include going in with a scope either through the GU system or percutaneously, lithotripsy or open surgical removal*
*with catheter into meatus of kidneys, grabbing the stone and removing it after dye injected and we know exactly where the stone is*
-Stones in bladder removed by cystoscopy: visualized and removed
-Stones in Ureter and renal pelvis may be removed by uteroscopic procedures
-Larger ones by cystolitholapaxy: crushed by a lithotrite then the bladder irrigated to remove fragments
-Stones in the renal pelvis may need percutaneous nephrolithotomy (PNL)
percutaneous nephrolithotomy (PNL)
-nephroscope inserted through a sinus tract into the the kidney pelvis
-stones crushed using ultrasound, or laser...
-then washing to remove fragments
-The nephrostomy tube is left in place to remove fragments and make sure the ureter isn't obstructed
Removal of renal calculiby lithotripsy
-May be done by ultrasonic lithotripsy, electrohydraulic lithotripsy, laser, or shock-wave lithotripsy
-Hematuria common after lithotripsy procedures- bright red turning dark to smoky over time
-Antibiotics for two weeks
-Self retaining stent left in place for 1-2 weeks to promote passage of sand
-May need re-treatment if stone is large
stent placement post-lithotrypsy
-less pliable than a catheter
-prevents spasm along the ureter walls
-sediment post lithotripsy is irritating to the ureters which causes pain...stent placed to alleviate that
-may be left in for 7 to 10 days
pt education about urine color post lithotripsy
-the urine color may be bright red and transition to dark red/smokey color
-this is NORMAL
collateral damage from lithotripsy
-the muscle, kidneys, and tissue take an ultrasonic hit from the procedure
-if my patient was urinating and now they aren't or there is a significant decrease over several hours I am concerned about a BLOCKAGE... this places pressure on the kidneys leading to an AKI status post lithotripsy (renal EMERGENCY)
Nursing care S/P lithotripsy: plan
-Pain management
-ID obstructions
-Patient ed to reduce the re-occurrence
Nursing care S/P lithotripsy: nursing interventions
-Bed rest, hydration,
-Turn q2hr to facilitate moving of the stone
-Strain Urine: send stone to lab to determine the cause and make a plan from there
-Patient education regarding diet, testing urine for ph (make urine acidic or alkaline as needed)
-may require regular urinalysis
Urinary Tract Infections (UTI)
-Typically the urinary tract above the urethra is sterile...
-Women have shorter urethras so more UTI's than men...
-E. coli most common causative agent...
UTI umbrella (complications upper and lower)
-urethritis
-Cystitis
-pyelonephritis: this is WORRYSOME**
cystitis (inflammation of the bladder): presentation
-Frequency and urgency
-Suprapubic pain
-Dysuria (painful or difficult urination)
-Foul-smelling urine
-Pyuria (urine that contains pus)
labs for cystitis
-Clean catch urine for WBC and blood
-Urine culture: tells us the best ABX to use
-If all negative, may be caused by irritants: feminine products, etc
cystitis nursing assessment: additional data
-Past health hx for previous UTI, kidney stones, structural problems, pregnancy, STDs, bladder cancer, benign prostatic hypertrophy
-Medications - use of antibiotics (can kill our good bacteria), anticholinergics and antispasmodics
-Recent surgical procedures and/or foley catheters
-History of elimination problems or obstruction
relief from dysuria d/t cystitis
-Medications
-ABX (sulfa)
-Antispasmodics
-Phenazopyridine (pyridium)
-pain meds
-Patient education on pyridium = orange urine, tears **NUMBS the bladder
-position for comfort, apply heat as needed
no recurrence of UTI
-Take all meds as directed (complete ABX)
-good hygiene practices, empty bladder before and after intercourse, void q 2-4 hrs
-adequate hydration
-avoid tight clothing: need loose, and cotton
-quick follow-up for recurrent symptoms bc you'll probably have another
pyelonephritis
-Inflammation of the renal parenchyma and collection system to include the renal pelvis
-probably have lower UTI first which was untreated or unchecked and traveled to parenchyma
-this is NOT good especially for the elderly as it is easy for this to become septic since 25-30% of blood runs through the kidneys
-often caused and exacerbated by dehydration
s/s with pyelonephritis
May be mild malaise to fever, chills, vomiting, flank pain, dysuria, and urinary frequency
treatment of pyelonephritis
-Mild cases may be treated as outpatient with abx up to 14 days: younger patients may need high dose ABX/IV antibodies...monitor closely
-Severe infection with dehydration and other complications need to be hospitalized, closely monitored and treated with IV abx to prevent sepsis **PO is NOT appropriate with geriatric pts
-dehydration, UTI, failure to thrive
Immune disorders of the kidney
-Glomerulonephritis (inflammation of glomeruli)
-Goodpasture's syndrome (cytotoxic autoimmune disease)
**either of these with acute onset, can cause an environment for an AKI
**since it's autoimmune, there will be periods of flare up and remission
Glomerulonephritis
-Inflammation of glomeruli: Can be ACUTE vs chronic
-bacteria creating abnormal immunoglobulin that is attacking the glomeruli
-Can cause sclerosis, scarring, and renal failure
chronic glomerulonephritis
-can develop over several years with no or very few symptoms.
-This can cause irreversible damage to your kidneys and ultimately lead to complete kidney failure.
-Long term use of NSAIDS can be a risk factor
acute onset of GN can be triggered by
-Strep throat*** ask if they've had strep throat...creates abnormal immunoglobulin and attacks kidneys
-Goodpasture's
-Lupus
s/s GN
-HTN/ Edema
-Hematuria: rusty/smokey appearance
-Proteinuria
-oliguria: very LITTLE output
**the glomeruli and loops are shutting down and there is an acute filtering issue
treatment (symptomatic relief) of GN
-Rest
-Sodium and fluid restrictions: less fluid is needed "right now"
-Diuretics
-Antihypertensives: if fluid overload is increasing BP
-Adjust protein as needed (if increased bun): protein is hard on the beans, so low protein is best
-Also may treat with immunosuppressant until inflammation stops...if continues, plasmapheresis to remove antibody complexes...
goodpasture's
-Cytotoxic autoimmune disease CHRONIC
-Rare, mostly in young male smokers **not sure why
s/s goodpasture's
-Pulmonary: Pulmonary insufficiency, crackles, rhonchi
-Renal: Hematuria, proteinuria, renal failure, elevated BUN and serum creatinine
**if new onset hemoptysis and hematuria then likely good indication of goodpasture's
treatment for goodpasture's
-corticosteroids
-immunosuppressants: and this is long-term tx...risk for INFECTION, will see certain WBC decreases
-plasmapheresis: remove abnormal Ig's
bladder cancer
-Most common cell type is transitional cell carcinoma
-transitional cells respond well to pressure
s/s bladder cancer
Gross, painless hematuria, may see frequency
classifying bladder cancer
-Jewett strong marshall system
-not TNM bc bladder transitional cells are so specialized
bladder cancer treatments
-Chemotherapy, Radiation, Immunotherapy
-Intravesical therapy
-Surgery
**often we use more than 1 (combo!)
intravesical therapy for bladder cancer
-responds really well to this method
-specialized catheter fills the bladder with topical chemo and if left in there for 1-2 hours
-the chemo gets absorbed into the transitional cells leading to really good outcomes
surgery for bladder cancer may involve
•a transurethral resection (TUR)
•laser surgery, or
•open loop resection
post-op care for bladder cancer
•Large amounts of water po
•I&O
•Avoid alcoholic beverages and stop smoking!
•Analgesics and stool softeners
•Sitz baths to relax muscles and decrease urinary retention
•Frequent routine cystoscopy is necessary.
urinary incontinence
-Incontinence (the involuntary leakage of urine)
-Occurs when the bladder pressure exceeds urethral closure pressure
-stress, urge, mixed, overflow
patho of bladder function
-When the detrusor ( muscle on the wall of the bladder) is triggered through parasympathetic input, bladder is emptied.
-Sympathetic nervous system constricts the internal urethral sphincter
-Normal bladder function means the detrusor and internal sphincter control the bladder.
-We see incontinence and / or inability to completely empty the bladder when we have neurogenic bladder.
urinary incontinence men vs women
-Women: more common (usually urge and stress incontinence or mixed)
-Men: usually overflow incontinence secondary to urinary retention (BPH)
Anything that interferes with bladder or urethral sphincter control can result in incontinence (DRIP)
(D) Delirium, dehydration, depression {geriatric considerations here}
(R) Restricted mobility, rectal impaction
(i) infection, inflammation
(p) polyuria, polypharmacy
tx for stress incontinence
(sudden increase in intra-abdominal pressure)
-Pelvic floor muscle training: kegels
-Bladder Training: practice holding in on the toilet
-Intake control: individualized to pt
-Weight loss if obese
*no approved meds for this*
tx for urge incontinence
(overactive bladder)
-Manage caffeine intake
-Strengthen pelvic floor muscles
-Medications: Anticholinergics & Antispasmodics ...decrease sphincter tone so do kegel exercises with these meds!!!
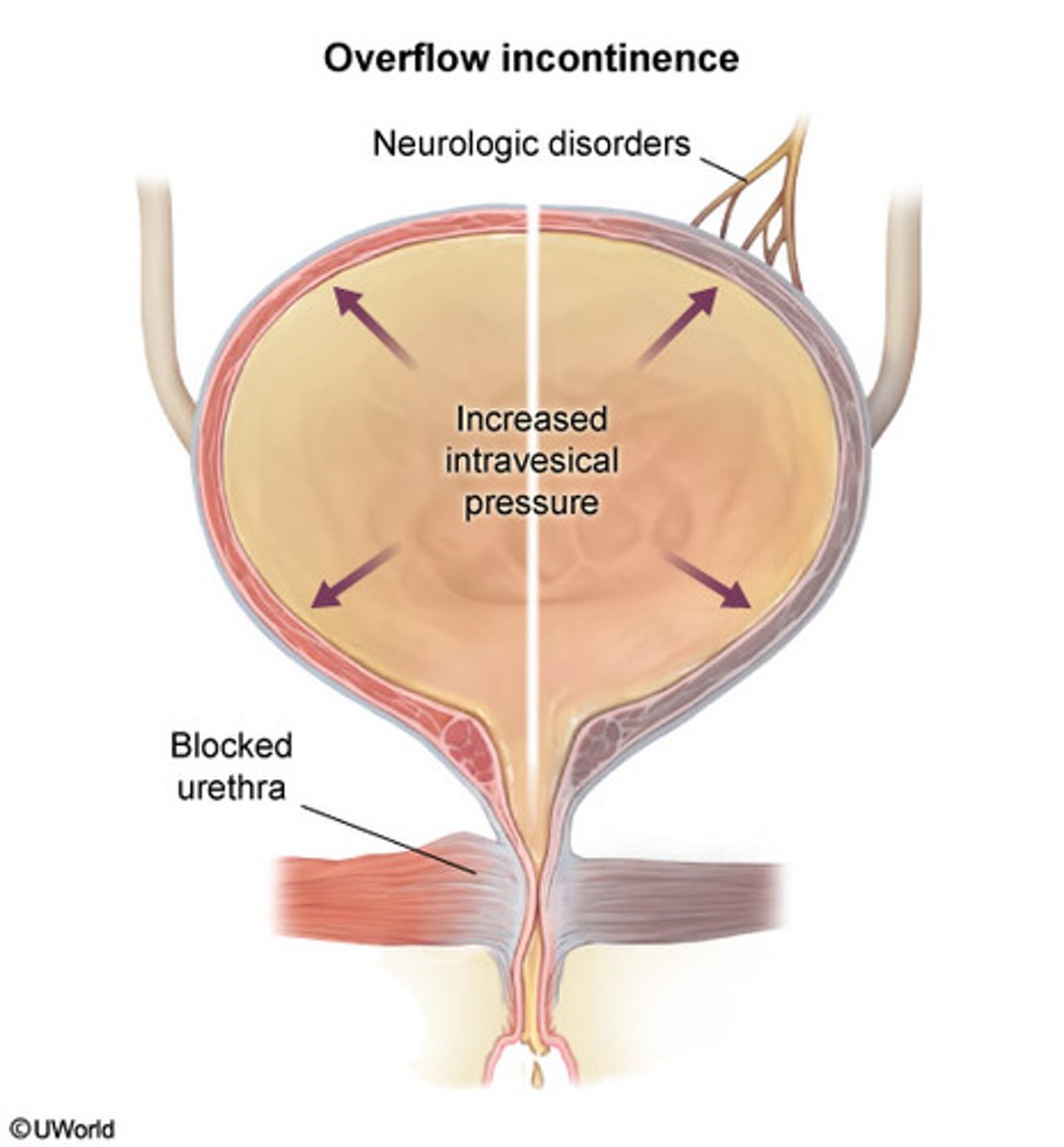
tx for overflow incontinence
-Pelvic floor muscle training
-Bladder Training
-Straight Catheters
-Medications: Alpha blockers (ex. Flomax for enlarged prostate...decrease the tone so they can empty the bladder...men with BPH can benefit from kegel exercises)
other tx for urinary incontinence
-Biofeedback
-Surgery: Sling or bulking to augment urethral resistance
stress incontinence
too little tone on the bladder and sphincter
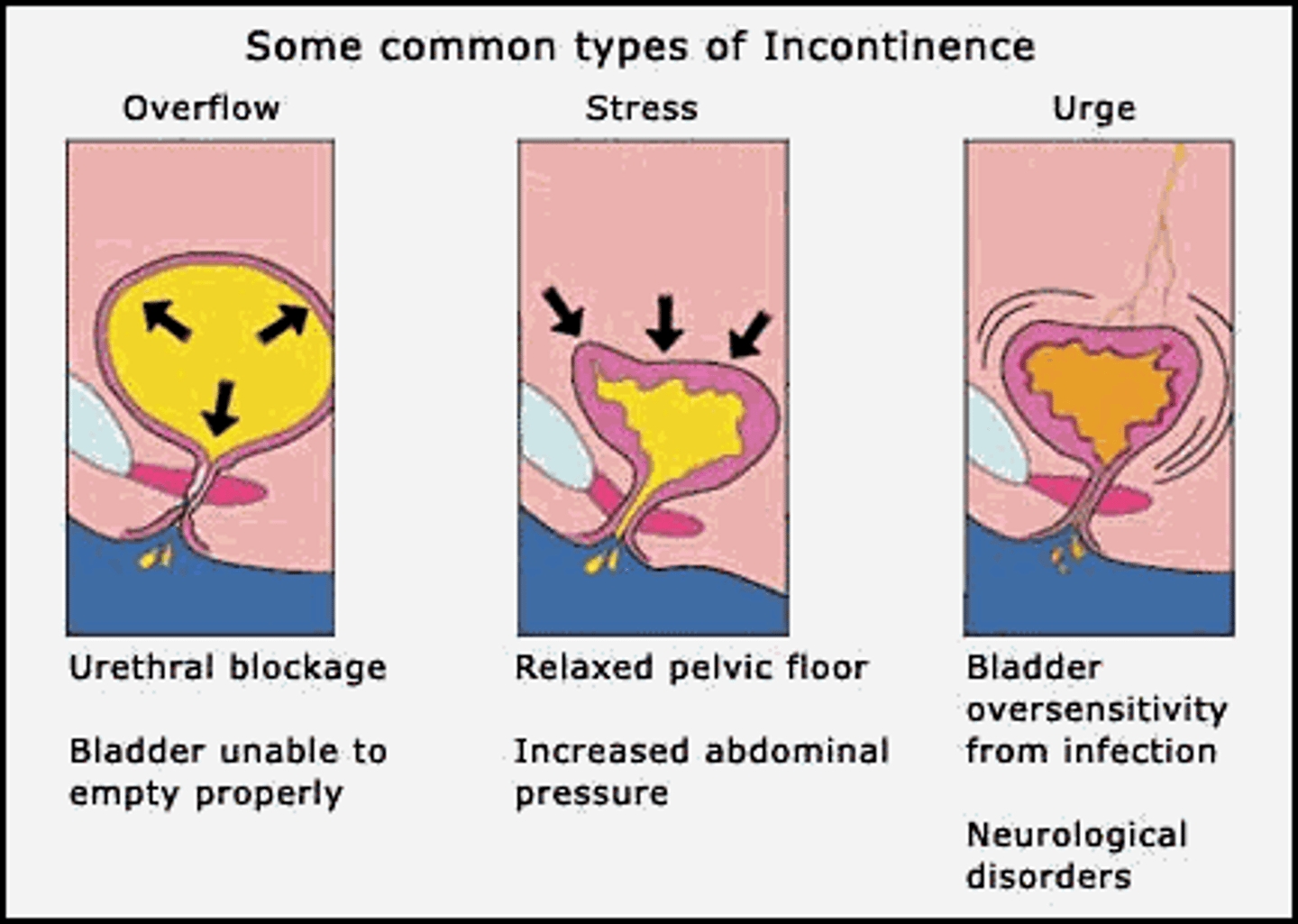
urge incontinence
-too much neurologic input; spasm
-too much activity
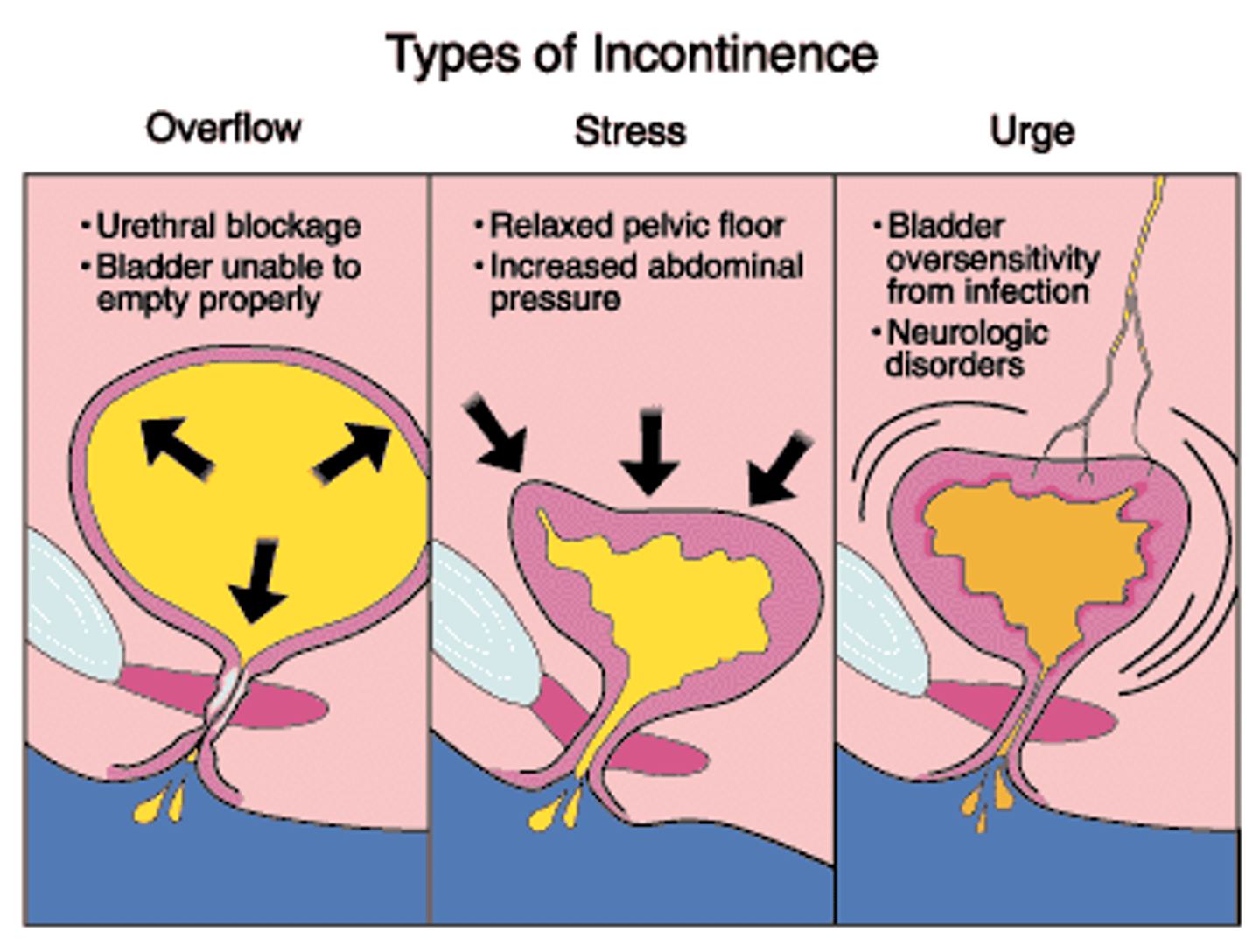
mixed incontinence
-too much activity AND too little tone
overflow incontinence
just can't hold it any more; obstruction, BPH
urinary retention
-Inability to empty bladder
-Occurs with or without incontinence
-caused by bladder outlet obstruction, or deficient detrusor contraction
bladder outlet obstruction
Common cause of outlet obstruction in men is an BPH benign prostatic hyperplasia
deficient detrusor contraction
Causes of deficient detrusor includes: sacral neurologic diseases, long-term diabetes, chronic alcoholism
Common drugs that can cause urinary retention
Anti-hypertensives (beta blockers), Anti-parkinsonian, Antihistamines (benadryl), Anticholinergics, Antispasmodics, Sedatives, Anesthetics
Causes of urinary retention Post op
•Hypervolemia/hypovolemia
•Atropine, anesthesia, sedatives: Decrease contractility of bladder and of the entire urinary tract
•Swelling and irritation post foley: urethral lining is irritated and inflamed...pre-disposing to decreased potential for urination
•Supine position during surgery
**teach pt to ambulate!!
Indications for urinary catheterization
•Relief of retention: 300-500 mL and unable to go or haven't voided in 6 h post surgery
•Bladder decompression prior to surgery
•Surgical repair of urethra and other structures in that area or to facilitate healing
•Instill meds into bladder: intravesical therapy for bladder CA
•Measure I & Os
•Residual urines can be measured
•Assess for structural problems: BPH, UTI
•Sterile sample: for UTI
interventions to help pts void
-sit them up semi/high fowler's if not CI
-run warm water and put their hands in
AKI Acute Kidney Injury (formerly known as acute renal failure ARF)
-Rapid decline in renal function
-Progressive elevation in BUN & creatinine. (azotemia)
-Uremia = symptomatic azotemia
-Progressive elevation in potassium: stays in the vasculature with sodium going to interstitial spaces...more acidic and can lead to cardiac issues
-Often associated with oliguria
-When watching I & O's we need 30 mL/hour or 240 mL for 8 hour shift or call MD
**kidneys are damaged and not working properly
monitoring I & Os closely
-if <240 mL in 8 hr there is either not enough blood going to the kidneys or they are not filtering and making urine=AKI
-if you see a rapid decline where pt was urinating adequately then suddenly <30 mL/hr this is PROBLEMATIC for all pts
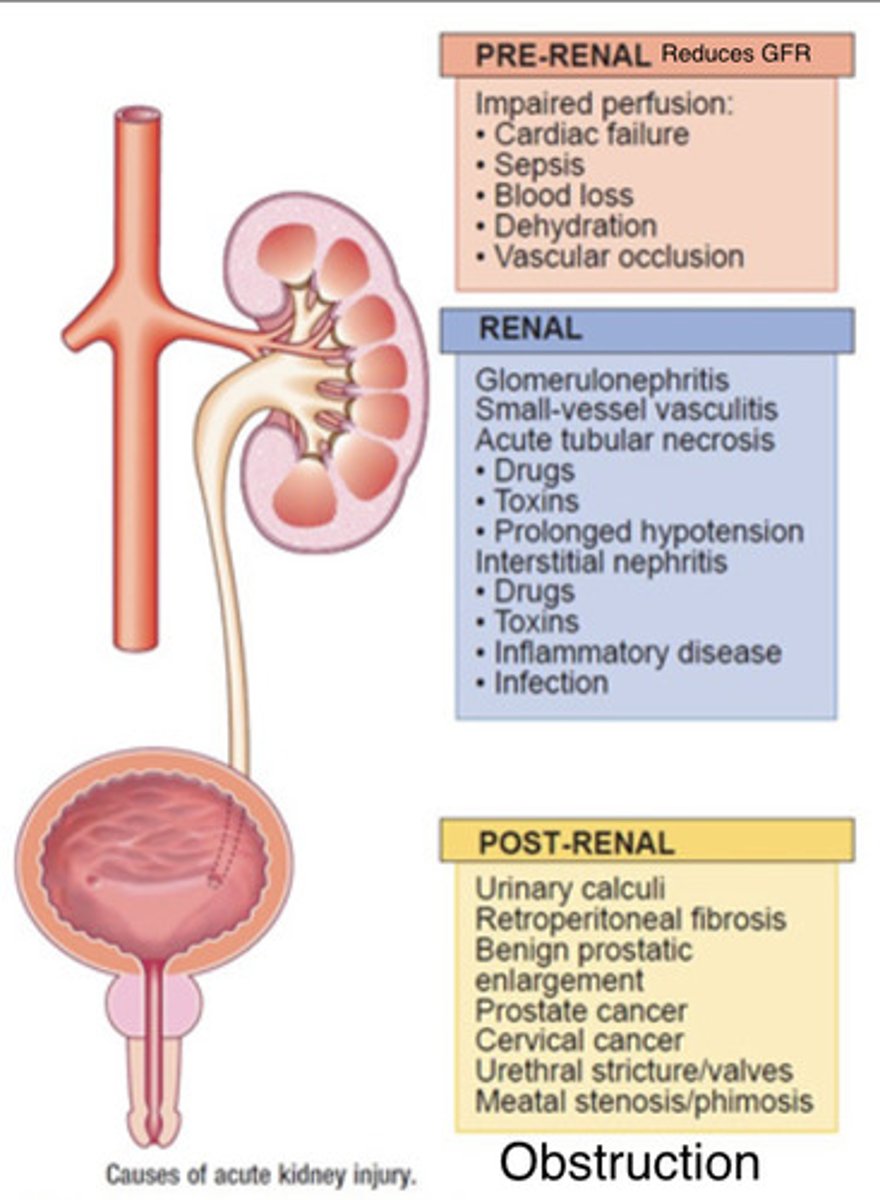
pre-renal causes of AKI
-Hypovolemia
-Decreased Cardiac Output
-Decreased Peripheral Vascular Resistance
-Decreased Renal peripheral vascular resistance
-Example: dehydration or low CO, not enough blood flow to perfuse the kidneys, so they acutely fail.
intrarenal causes of AKI
-Nephrotoxic Injury
-Interstitial Nephritis
-Malignant HTN, prolonged renal ischemia, thrombus formation...
-kidney cancer
-damage from lithotripsy
-glomerulonephritis
-Example: Acute Tubular Necrosis (not mobilizing within the renal system) Infection in the kidney, or maybe nephrotoxic medication regimen.
post-renal causes of AKI
-BPH (can't mobilize urine, increasing pressure), Bladder Cancer, renal calculi (blocking removal of urine), strictures....
-Example: Obstruction like benign prostatic hypertrophy or urethral scarring, causing urinary retention, stasis of urine
AKI phase 1: Oliguric phase
-secondary to a reduction in GFR
-glomerulus NOR loop of henle are working...no filtering, no urinating
oliguric phase is manifested by
-Changes in urinary output (less than 400 mL/24 hr) <30 mL/hr
-Fluid and electrolytes (↑ K, ↓ Na)
-Uremia
-(Fluid retention, 3rd spacing, neck veins distended-JVD, bounding pulses, edema, HTN, FLUID OVERLOAD)
**NOT passing urine
AKI phase 2: Diuretic phase
-Due to the high osmolality and the inability of the tubules to concentrate the urine.
-The nephrons are functioning but not at full capacity; only the loops are mobilizing fluids NO function from glomerulus yet