Ocular drug delivery systems
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
What are ophthalmic drugs?
Drugs that are used for diagnosis and treatment of ocular diseases
What are some examples of ophthalmic products?
Eye drops, lotions, suspensions, ointments, contact lens solutions, ophthalmic inserts
What are some local conditions that may be treated by ocular drug delivery?
Glaucoma, cataract macular degeneration
What are some systemic conditions that may be treated by ocular drug delivery?
Can arise from diabetes (diabetic retinopathy), hypertension e,g., bleeding, optic neuropathy
What is the main route of drug delivery for ocular?
Local drug delivery - not a significant portal for systemic
What are the advantages of ocular drug delivery?
Reduces systemic effects and reduces required dosage
What are some disadvantages of ocular drug delivery?
Patient compliance can be poor and eye can be sensitive to application of medicines
What is the anatomy of the eye?
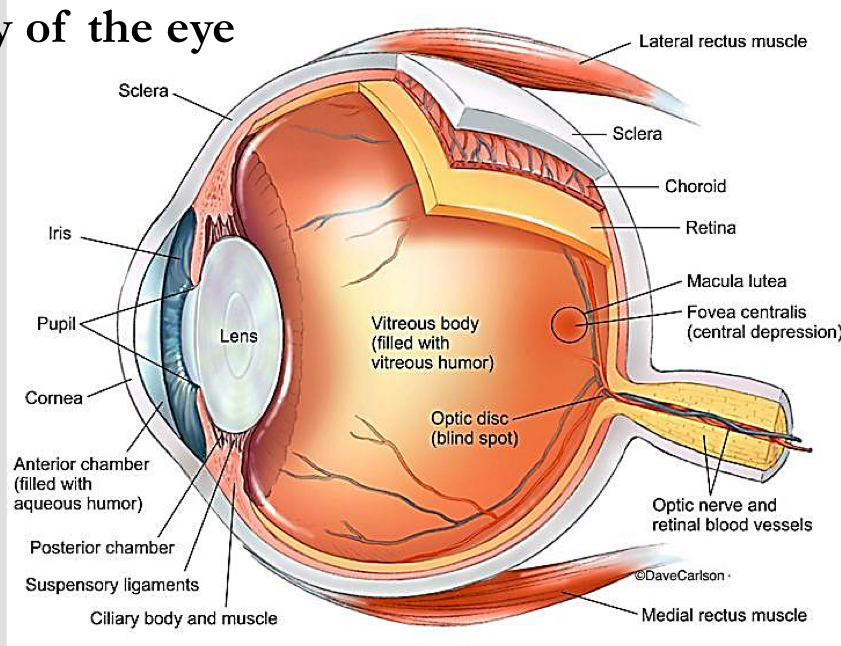
What is the choroid in the eye?
Highly vascularised connective tissue that provides a blood supply to the eyeball and contains a viscous vitreous media
What is an important factor for ocular delivery in relation to the size of the eye?
Size:size/volume ratio of applied dose is key
What is the main pathway for diffusion of drugs into the eye?
Cornea
What are the properties of the cornea?
0.5-0.7mm thick and has 6 different layers, has no blood vessels to nourish it, stratified epithelium
What is the structure of the cornea?
Epithelium and endothelium rich in lipids, stroma has high water content
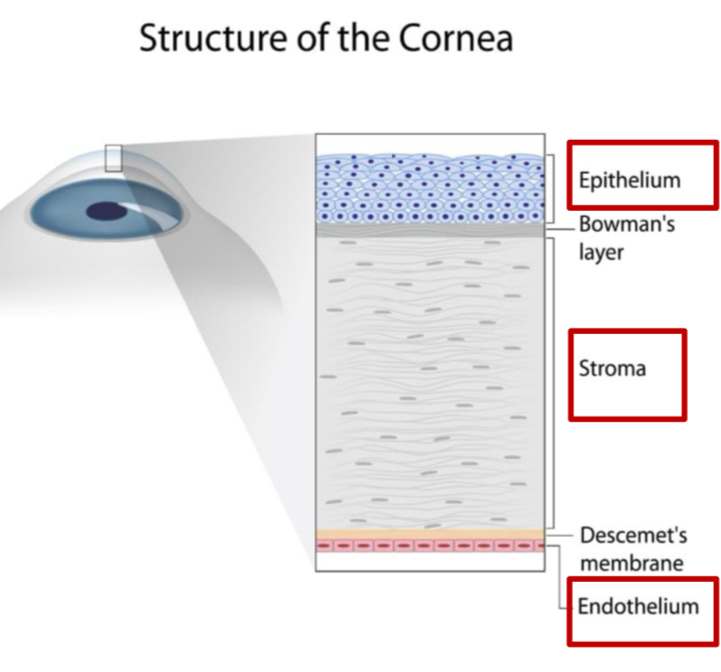
What are the properties of the epithelium in the cornea?
Excludes macromolecules, radius of >1nm, only small drugs of MW of 350 or under/ions can permeate through via paracellular
What type of compounds can pass into the corneal epithelium via the transcellular route?
Lipophilic compounds
What types of molecules does the stroma layer allow into the cornea?
Hydrophilic molecules
What type of molecules does the stroma limit the penetration of?
Highly Lipophilic (Log P of 2-3) or large MW compounds
What is the corneal endothelium in direct contact with?
Aqueous humour
What impact does the corneal epithelium and the aqueous humour having direct contact have on molecules that can enter?
Resists permeation of Lipophilic compounds
What is the anterior chamber of the eye?
Space between cornea and eye - containing aqueous humour
What is aqueous humour in the eye?
Watery like liquid inside, made of water and collagen
What is the posterior chamber in the eye?
Between ligaments and lens
What do the suspensory ligaments do in the eye?
Changes thickness of the eye lens
What happens to suspensory ligaments as you age?
Loses their activity and therefore affects vision
What does the macula lutea do in the eye?
Helps to form the pictures that we see/our vision - links with the optic nerve to send signals to the brain
What happens if the optic nerve is damaged?
Signals cant be sent to the brain therefore reduces vision
What is an intravitreal delivery as a route of ocular drug administration?
Facilitated by injection e.g., a solution into vitreous humour of the eye between lens and retina
What is the intravitreal route mostly used for?
Anti-VEGF molecules or corticosteroids e.g., dexamethasone
What is VEGF?
Helps to form blood vessels in the body
Why are anti-VEGF molecules used in the eye?
Reduce amount of VEGF in the eye which can form blood vessels on the macula lutea and affects vision
What is a diagram highlighting different routes of administration into the eye?
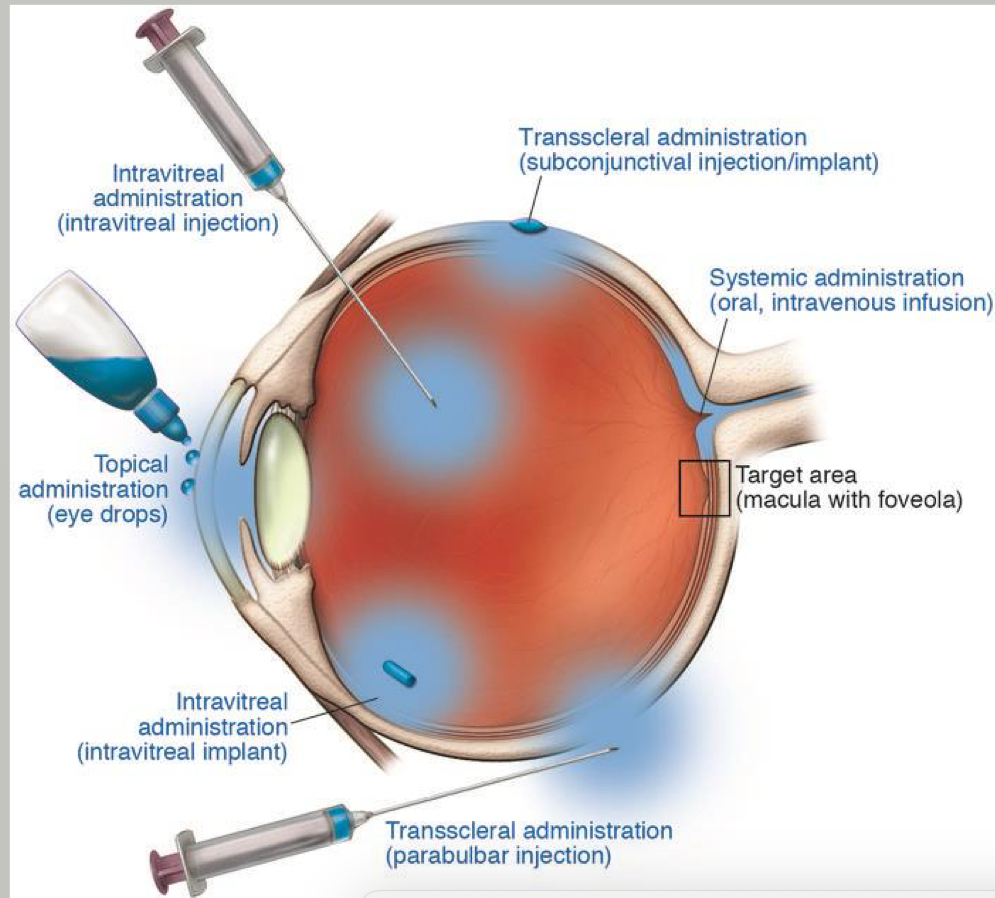
What is a Sub-Tenon’s injection?
A local anaesthetic near/beyond the equator performed using a cannula
Why are sub-tenons injections used?
To allow us to Administer medications in posterior segment inflammation
What drugs are usually used in the eyes a local anaesthetic?
Lidocaine 2% and bupivacaine 0.5% in equal proportion, with/without hyaluronidase 30-150iu/ml - usually a mixture vol of 3-5mL
What is an alternative to lidocaine-bupivacaine mixture?
Articaine - 2%
When are subconjunctival injections used?
Used to deliver anti-infective drugs or corticosteroids for conditions not responding to topical therapy
Where does the drug diffuse to when injected subconjunctivally?
Anterior and posterior chambers and vitreous humour
What volume of injections are used for subconjunctival injections?
1mL
Why should you take care when injecting drugs subconjunctivally?
blood vessels absorb the drug and ends up in systemic circulation
What is a diagram showing the tear production system?
Tears produced at rate of 5-9uL in a normal eye - basal tears are continuously secreted by lacrimal glands at average of 0.2
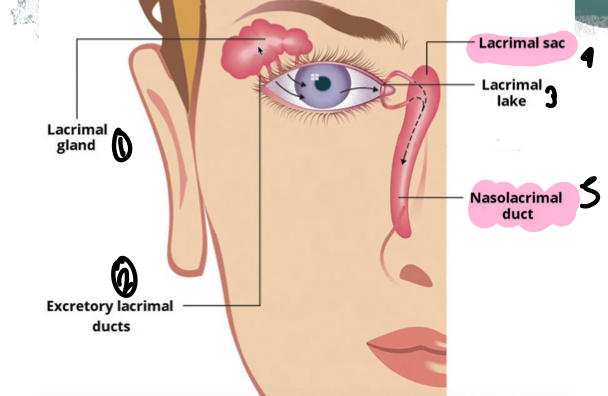
What do tears contain?
Lysozymes and immunoglobulins which have an anti-infectious activity
What does the combined mechanisms of lacrimal drainage and blinking mean for ocular administration?
Eye drops are rapidly cleared from conjunctival sac from around 4-23 minutes
What are the roles of the muscles around the eye?
Change position of the eye
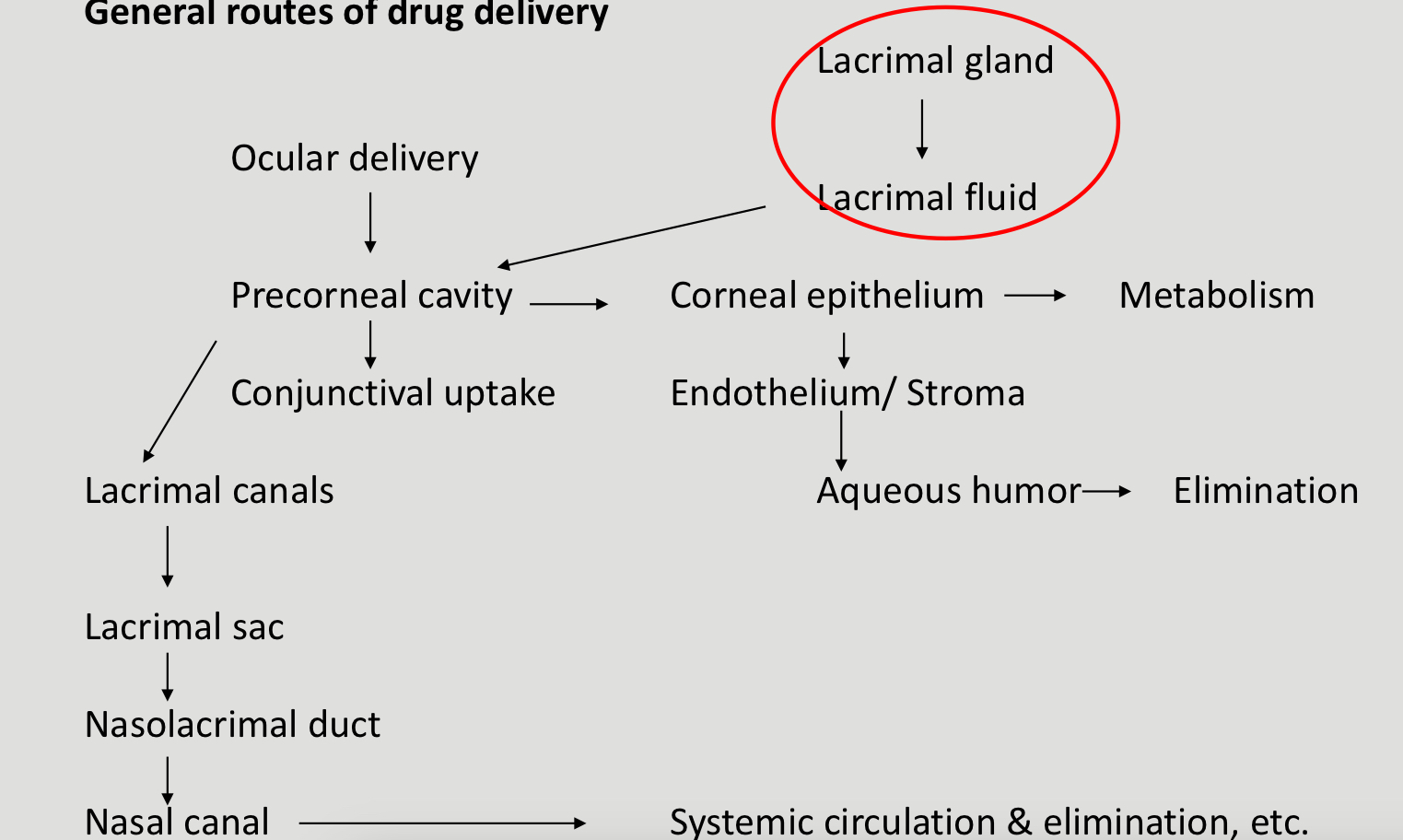
What is a diagram showing general routes of drug delivery in the eye?
What are some common disorders in the eyes?
Astigmatism, glaucoma, myopia, retinitis pigmentosa, blurred vision, hyperopia, blepharitis, corneal ulcer, photokeratitis, cataracts
What is glaucoma?
Abnormally high pressure in your eye that can damage the optic nerve
How does glaucoma develop?
Flow of aqueous humour through the drainage canal, drainage canal becomes blocked and fluid builds up - increased pressure damages blood vessels and the optic nerve
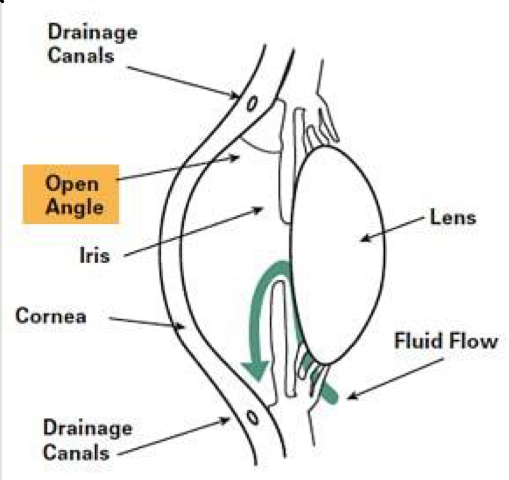
What is open-angle glaucoma?
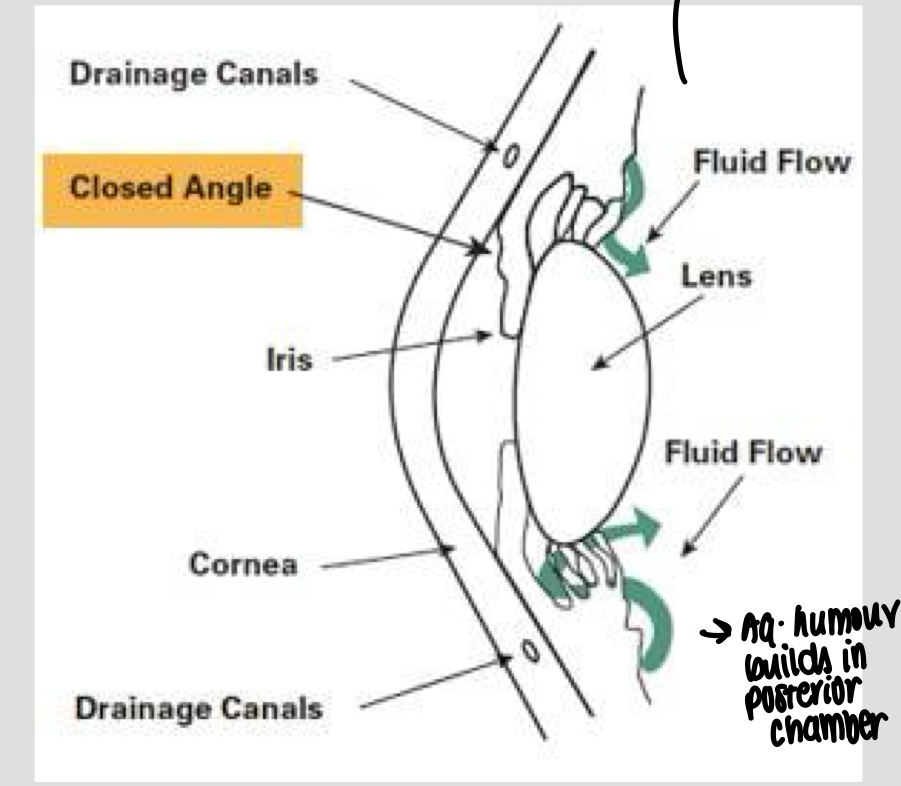
What is closed-angle glaucoma?
No gap between lens and iris - aqueous humour builds up in the posterior chambers
What are the main aims of pharmaceutical treatments for glaucoma?
Mostly reduce intra-ocular pressure
What are the drug classes for treating glaucoma?
Beta blockers, prostaglandin analogues/prostamides, sympathomimetics, carbonic anhydrase inhibitors and miotics
What are some examples of beta blocker eye drops to treat glaucoma?
Timolol maleate, betaxolol
What are some examples of prostaglandin analogues and prostamide eye drops for glaucoma treatment?
Latanoprost, tafluprost
What do sympathomimetic eye drops do for treating glaucoma?
Rdeuce aqueous humour formation and increase uveoscleral flow e.g., brimonidine tartrate/apraclonidine
What are carbonic anhydrase inhibitors for treating glaucoma?
Systemic drugs that reduce aqueous humour production - oral or IV administration but only for short term use
What is an example of a miotic used to treat glaucoma?
Pilocarpine - tablet/eye drops
What are intra-ocular devices?
Devices inserted into the patients eye and drug is released over a long period of time
What are the advantages of intra-ocular devices?
Release the drug at steady rate, allows accurate dosing, releases drug over a long period of time, reduction in systemic absorption, shows an increase in patient compliance as doesnt need to use an eye drop/ointment daily
What are the disadvantages of intra-ocular devices?
May need to surgically removed the implants, tissue toxicity of polymers which stay inside for a long time, patients may be reluctant to place solid objects in their eyes
What are examples of biodegradable solid devices for in the eye?
PVA, PVP, HPMC, PLGA, PCL
What is an advantage of non-biodegradable solid devices for ocular use?
Better dosing accuracy than soluble ones
What are non-biodegradable solid devices made from?
Ethylene vinyl acetate copolymers
What is macular oedema?
When fluid and protein deposits collect on/under the macula of the eye and causes it to thicken and swell