CHP 7 neurological system disorders
1/111
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
112 Terms
frontal lobe main elements (3)
precentral gyrus: primary motor cortex for voluntary muscle activation
prefrontal cortex: controls emotions, judgements, higher-order cognitive fxn
premotor cortex: planning movements
brocas area: motor aspect of speech
parietal lobe elements
postcentral gyrus: primary sensory cortex for integration
receives fibers conveying touch, prop, pain, and temp from opposite side of body
temporal lobe (3)
primary auditory cortex: receives/processes auditory stimuli
associative auditory cortex: processes auditory stimuli
wernicke’s area: language comprehension
limbic system
consists of…
limbic lobe
hippocampal formation
amygdaloid nucleus
hypothalamus
anterior nucleus of thalamus
instincts and emotions contributing to preservation of individual
basic functions:
feeding, aggression, emotions, endocrine of sexual response, long-term memory formation
subcortical white matter
what
elements (3)
myelinated nerve fibers located centrally
elements
corpus callosum: connects hemispheres to allow communication
projection fibers: connect cerebral hemispheres with other portions of brain and spinal cord
association fibers: connect different portions of cerebral hemispheres, allowing cortex to function as integrated whole
basal ganglia
masses of gray matter deep within cerebral hemispheres
basic function:
initiates voluntary movement, controls postural adjustments, refines coordination, forms and stores motor plans, and produces dopamine
disorders associated:
parkinson’s disease: reduced dopamine production
huntington’s chorea: degeneration of caudate nucleus
thalamus
sensory nuclei: integrates and relays sensory information from body, face, retina, and taste receptors to cerebral cortex (no smell)
motor nuclei: relays motor info from cerebellum and globus pallidus to precentral motor cortex
hypothalamus
integrates and controls functions of autonomic NS and neuroendocrine system
maintains body homeostasis
substantia nigra
large motor nucleus connecting with basal ganglia and cortex
important for motor control and muscle tone
pons
connects medulla oblongata and midbrain for passage of ascending and descending tracts
basic functions:
controlling autonomic fxn (pain and arousal)
relay system
REM sleep
medulla oblongata
acts as vital cardiac, respiratory, and vasomotor center
controls reflex actions (vomiting, swallowing, gagging, coughing)
important for head movements and gaze stabilization
cerebellum
anterior, posterior, and flocculonodular lobes
functions:
proprioceptive regulation (posture and voluntary movement)
motor planning, timing and coordination
trunk control, balance, equilibrium, muscle tone
common disorders:
friedreichs ataxia
spinocerebellar ataxia
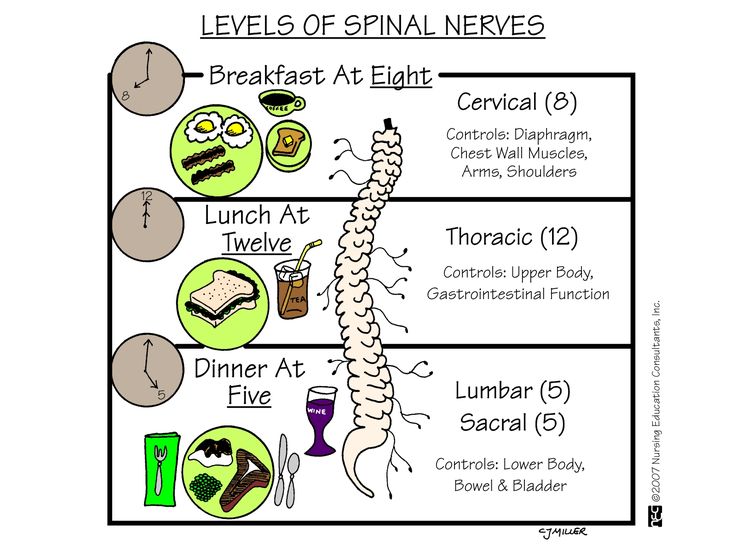
spinal cord
five sections:
cervical C1-C8
thoracic T1-T12
lumbar L1-L5
sacral S1-S5
**coccygeal: not SC but nerve roots that form cauda equina
ventral (anterior) horn = efferent (motor) neurons
dorsal (posterior) horn = afferent (sensory) neurons
ascending and descending tracts
ascending tracts (4)
sensory pathways from body to brain
ascending = afferent = after (posterior)
types:
dorsal columns/medial lemniscal: convey sensations of prop, kinesthesia, vibration, pressure, and discrimination (tactile & prop)
spinothalamic: conveys sensations of pain, temperature, and crude touch (tactile)
spinocerebellar: unconscious prop, touch, and pressure from lower body
spinoreticular: deep and chronic pain
descending tracts (4)
motor pathways from brain to body
types
corticospinal: cross at medulla > contralateral voluntary motor control
vestibulospinal: muscle tone, antigravity muscles, postural reflex
rubrospinal: contralateral
reticulospinal: preparatory and movements for activity and postural control
complete cord lesion: UMN
complete bilateral loss of all sensory modalities
bilateral loss of motor function with spastic paralysis below level of lesion
loss of bladder and bowel
central cord lesion
UMN
caused by hyperextension
more UE deficits than LE
LOSS
bilateral loss of pain and temp
bilateral loss of motor function
KEEP:
prop and discriminatory sensations
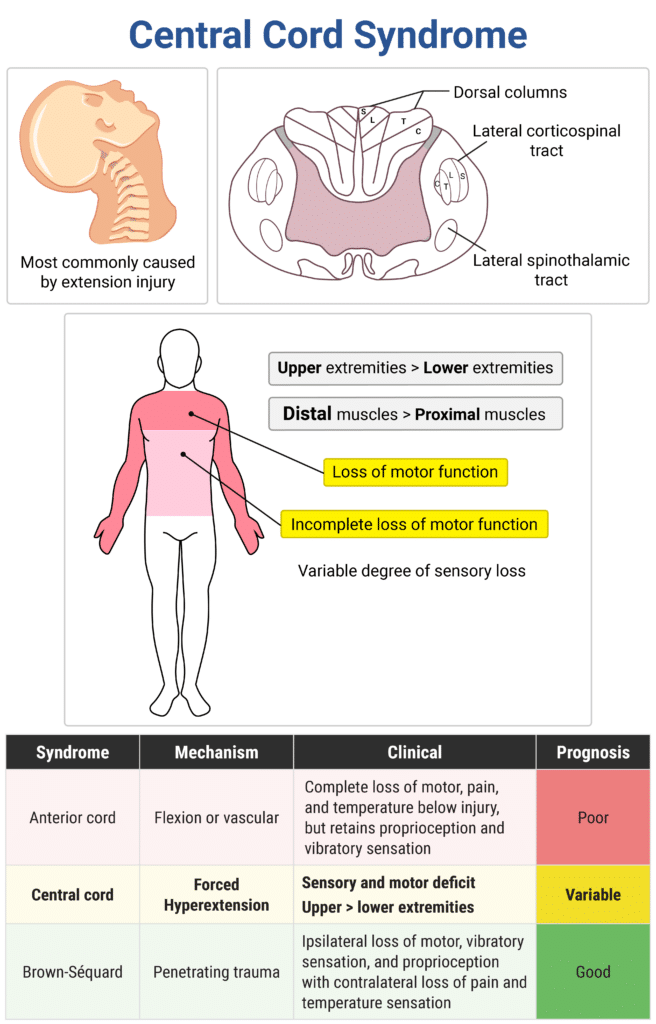
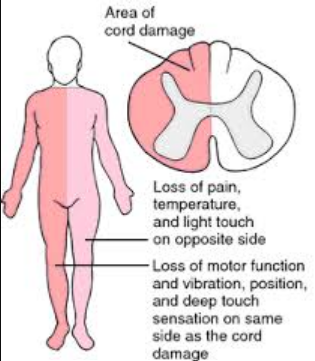
brown-sequard syndrome
UMN
caused by trauma resulting in hemisection of spinal cord (one side is injured, vertical)
LOSS
ipsilateral loss of tactile discrimination, pressure, vibration, and prop
ipsilateral loss of motor function and spastic paralysis BLOI
contralateral loss of pain and temp
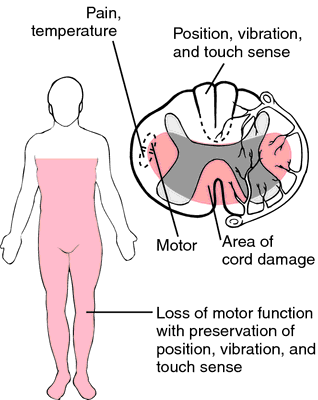
anterior cord syndrome
UMN
caused by flexion injuries
hemisection of cord (horizontal) loss of anterior cord
LOSS
bilateral motor function w/spastic paralysis BLOL
bilateral pain and temp
KEEP
prop, kinesthesia, vibration
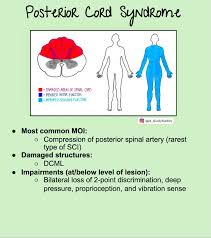
posterior cord syndrome
UMN
least frequent
loss of dorsal column bilaterally
LOSS
bilateral prop, vibration, pressure, stereognosis, discrimination
KEEP
motor function, pain, temp, light touch
cauda equina
LMN
loss of long nerve roots at or below L1
incomplete lesion common
potential for regeneration (up to 1yr)
RESULT
flaccid paralysis with no spinal reflex activity
flaccid paralysis of bladder and bowel
conus medullaris
LMN
injury of sacral cord and lumbar nerve root
LOSS:
LE motor and sensory loss
areflexic bowel and bladder
autonomic nervous system (ANS)
involuntary muscles (smooth muscle, heart, glands)
helps maintain homeostasis
two division:
sympathetic: fight or flight, emergency response, incr BP, inhibits peristalsis
parasympathetic: converses and restores, slow HR, decr BP, peristalsis
modulated by brain centers
descending autonomic system: hypothalamus, lower brain stem
cranial nerves
cerebrospinal fluid
clear fluid that provides mechanical support (cushion), controls brain excitability by regulating ionic compo and exchange of nutrients
normal pressure: 70-180 mm/H2O
total volume: 125-150 cc
hydrocephalus: abnormal accumulation of CSF in ventricles > pressure on brain
brain blood supply (4)
carotid system
vertebrobasilar system
circle of willis
venous drainage
neurons
vary in size and complexity
cell body, dendrites, axons, myelin, synapses, nodes of ranvier, neuromuscular junction
disorders:
myasthenia gravis: disorder of NMJ
TYPES:
nuclei: compact groups in PNS
projection: CNA
axon bundles: spinal
neuroglia: support, production
UMN: motor from brain to brain
LMN: motor from brain to body
nerve fibers:
A: large, fast. myelin
Alpha: prop, somatic motor
Beta: touch, pressure,
Gamma: motor
Delta: pain, temp, touch
B: small, myelin, slow
C: smallest, no myelin, slowest
UMN lesion
location: CNS
structures: cortex, brainstem, corticospinal tract, spinal cord
disorders: stroke, TBI, SCI
sx:
hypertonia, velocity-dependent
hyperreflexia, clonus, babinski response
muscle spasms
bilateral, contralateral, ipsilateral weakness or paralysis; impaired or absent voluntary movements
disuse atrophy
LMN lesions
location: peripheral NS
structures: anterior SC, spinal roots, peripheral nerves, CN
disorders: Polio, guillain-barre, PNI, peripheral neuropathy
SX:
hypotonia, flaccidity
hyporeflexia
fasciculations
limited distribution of strength
neurogenic atrophy, severe wasting
weak or absent voluntary movements if nerve impacted
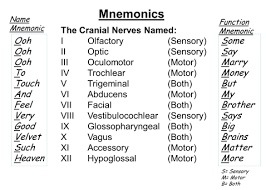
cranial nerves
12 pairs
olfactory: sensory, smell
optic: sensory, vision
oculomotor: motor, eyes movement
trochlear: motor, eye movement
trigeminal: both, chewing, head sense
abducens: motor, eye mvmt
facial: both, facial sensation and motor
vestibulocochlear: sensory, hearing & balance
glossopharyngeal: both, swallowing, head sense, taste, lungs, parotid
Vagus: both, voice, swallowing, taste, heart, vessels, lungs, bowels
accessory: motor, trap (neck)
hypoglossal: motor, tongue
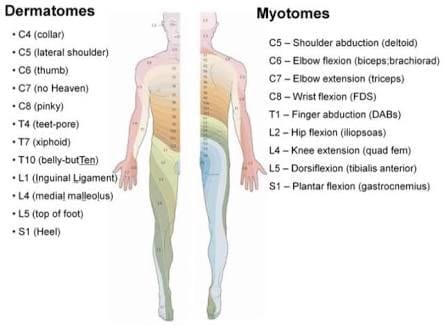
dermatomes and myotomes
dermatomes: sensory distribution along the skin
myotomes: nerve distribution for skeletal muscles
spinal reflexes
what
types (5)
involuntary response to stimuli
basic, specific, predictable
provide basis for unconscious motor function and basic defense mechanisms
types:
stretch (myotatic)
stimulation with muscle stretch
maintain muscle tone, support agonist muscle, provide feedback about muscle length
inverse (myotatic) stretch:
stimulation with muscle contraction
provide agonist inhibition, dim force of agonist contraction
gamma reflex loop
stretch reflex forms part of loop
allow muscle tension to come under control > regulating level of tension in muscle
flexor (withdrawal)
stim with cutaneous sensory stim to large flexor muscles
protective withdrawal to remove body part from harmful stimuli
crossed extension
stim with noxious stim and reciprocal action of antagonist (flexors on one side excited > extensors on same side inhibited)
coordinates reciprocal limb ax (gait)
CVA
disease of cerebral vasculature in which there is failure of blood and oxygen to the brain, causing brain death
types:
transient ischemic attack (TIA):
mini stroke, transitory stroke that lasts for few minutes; warning stroke
sx usually disappear within the hour (may persist 24hr)
numbness, weakness to face, arm, or leg (one side); confusion, slurred words, vision difficulty, LOB
ischemic stroke
most common due to embolism or thrombosis of cranial arteries
hemorrhagic stroke
bleed secondary to hypertension or aneurysm or AVM
SX:
abrupt unilateral signs (weakness, vision loss, sensory changes)
contralateral manifestation
specific sx determined by site of stroke
FAST
F = face drooping
A = arm weakness
S = speech difficulty
T = time to call 911
diagnosis: cerebrovascular imaging & diagnostic testing
medical care: antithrombotic, thrombolytic therapy (t-PA)
stroke sx by artery
middle cerebral (MCA): contralateral hemiplegia, hemianesthesia, hemianopsia
aphasia, unilateral neglect, bilateral apraxia (left MCA) or left apraxia (right MCA)
internal carotid (ICA): sx similar to MCA
anterior cerebral (ACA): contralateral hemiplegia, grasp reflex, incontinence, confusion, apathy
posterior cerebral (PCA): homonymous hemianopsia, thalamic pain, hemisensory loss
vertebrobasilar: dysarthria, dysphagia, emotional instability
left vs right hemisphere functions
LEFT:
movements of right side
process sensory info from right
visual reception from right
visual verbal processing
bilateral motor praxis and auditory reception
verbal memory, speech, process verbal auditory
RIGHT
movement of left side
sensory info from left
vision on left
visual spatial, nonverbal memory, attention, emotional lability, interpreting abstract info, nonverbal auditory
left motor praxis
traumatic brain injury (TBI)
open or closed trauma from fractures, trauma to blood vessels, nerves, or meninges, hemorrhage, edema, etc.
open: damage from penetration of skull (bullet)
closed:
rapid acceleration or deceleration
blunt external force to head
SX:
concussion (loss of consciousness)
cerebral contusion/laceration/edema
hemiplegia, abnormal reflexes, fixed pupils
coma, decorticate or decerebrate rigidity
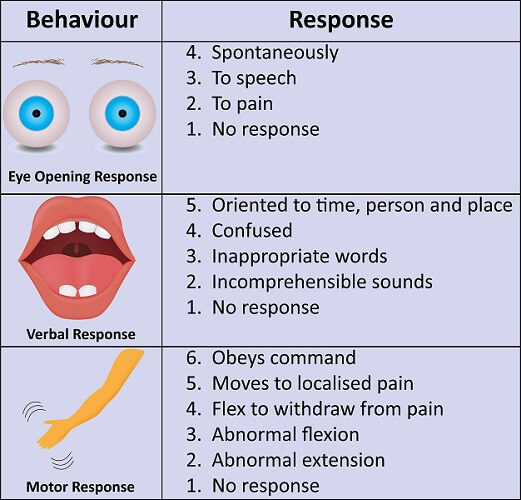
Glasgow Coma Scale
15-point scale of levels of consciousness done at initial eval
DOMAINS
eye opening
verbal response
motor response
indicates class of brain injury (mild, moderate, severe)
admin right after initial injury
SCORE: 3 domain criteria will be scored and totaled
8 or less = severe TBI
9-12 = moderate TBI
>13 = mild TBI
higher the score = milder the TBI
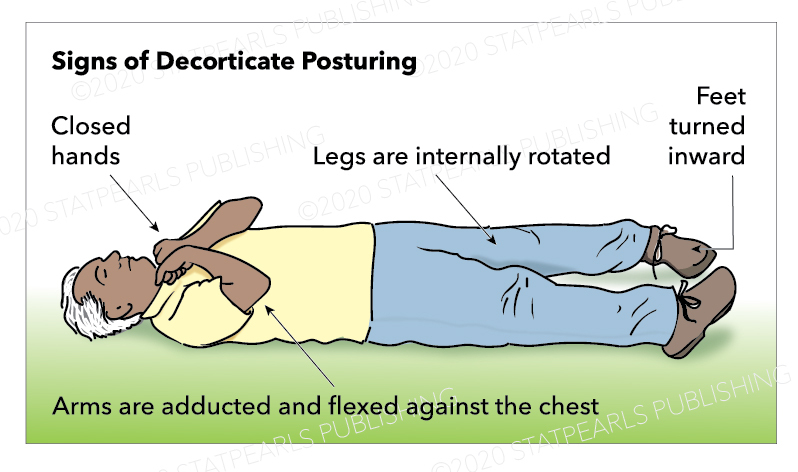
decorticate rigidity
UE in spastic flexion w/IR and add
LE in spastic extension w/IR and add
corticospinal tracts
associated with better outcomes
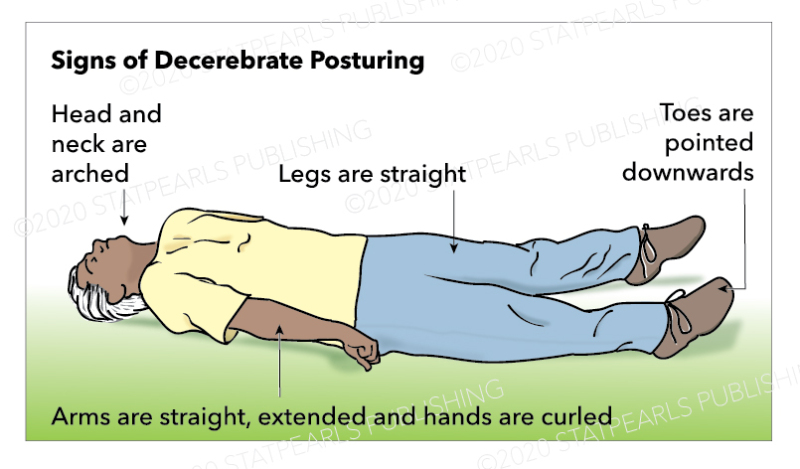
decerebrate rigidity
brainstem and extrapyramidal tracts
poorer prognosis
both UE/LE in spastic extension, add, IR
wrists and fingers flexed
ankles plantar flexed with feet inverted
trunk extended
head retracts
Rancho Los Amigos Levels of Cognitive Functioning Scale
clinical tool used to rate how people with brain injury are recovering
10 levels
main groups
RLA levels 1-3 = total assistance
EVAL: short, quiet, PROM, observation, GCS, RLA
GOALS: prevent contracture, encourage ax, facilitate progress, caregiver ed
TX: caregiver ed, sensory stim, positioning, casting/splint, dysphasia management, self-reg
RLA levels 4-6 = confused
EVAL: basic comprehensive (physical, cognitive, vision, perception, ADL)
TX: rehab/compensatory approach
repetitive practice and mods/adaptations
RLA levels 7-8 = automatic or purposeful
RLA levels 9-10 = pretty much INDP, complex cognition differences
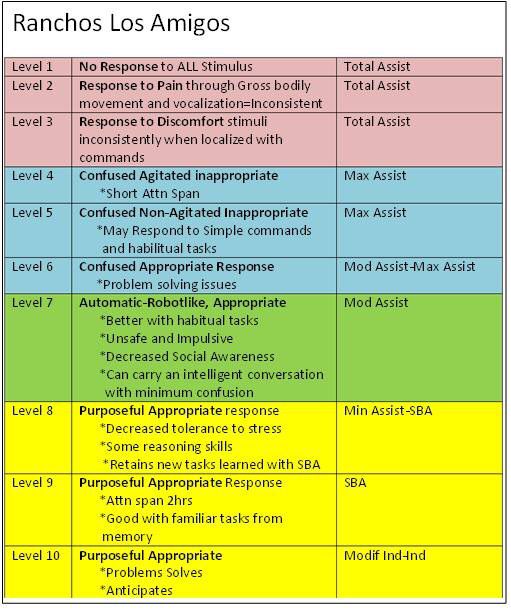
Rancho level I
No response: Total assistance
no response to ALL stimulus
total assist
OT:
EVAL: short, quiet, PROM, observation, GCS, RLA
GOALS: prevent contracture, encourage ax, facilitate progress, caregiver ed
TX: caregiver ed, sensory stim, positioning, casting/splint

Rancho Level II
Generalized Response: Total assistance
GENERALIZED response to pain through gross bodily movement
inconsistent & non purposeful
OT:
EVAL: short, quiet, PROM, observation, GCS, RLA
GOALS: prevent contracture, encourage ax, facilitate progress, caregiver ed
TX: caregiver ed, sensory stim, positioning, casting/splint

Rancho Level III
Localized Response: Total assistance
LOCALIZED response to discomfort, inconsistently
turn towards or away from auditory, visual, or pain
withdrawal
may visual track, react to visual (blink)
discomfort > pulls at restraints and tubes
inconsistent response to stimuli
responds more to familiar people
may respond to simple commands
OT:
EVAL: short, quiet, PROM, observation, GCS, RLA
GOALS: prevent contracture, encourage ax, facilitate progress, caregiver ed
TX: caregiver ed, sensory stim, positioning, casting/splint, dysphasia management, self-reg
Rancho Level IV
Confused/Agitated: Maximum assistance
alert and anxious
purposeful attempt to remove restraints, aggressive, mood swings, eloping attempts, uncooperative to tx
SAFETY RISK!!
purposeless basic motor ax
BADLs, sitting, standing, bed mobility
attention = seconds
4 your own safety, please calm down
Rancho Level V
Confused, Inappropriate, Non-agitated: Maximal A
alert, not agitated, wanders, not oriented, frequent brief sustained attention
inappropriate = no manners, tool misuse, sexual comments
absent goal-direct problem solving, unable learn new info
dirty dan, only thing on his mind, can’t change
requires frequent cues and structure
i’m going to count to 5 and you better behave!
Rancho Level VI
Confused, Appropriate: Mod A
inconsistently oriented, appropriate but confused
emerging awareness and recognition of self and others
NOT limitations, ONLY physical awareness
SBA for familiar learning, NO new learning
consistently follows simple directions
morning routine at 6 (brush teeth, wash face)
Rancho Level VII
Automatic, appropriate: Min A for Daily
consistently oriented to person & place
attend to familiar task for 30mins
NEW LEARNING
superficial awareness of condition
poor judgement, hard to problem solve, poor decision making about future, overestimates abilities
poor awareness to others (as emotional people)
go to school to learn new things at 7
Rancho Level VIII
Purposeful, appropriate: stand by
consistently oriented, indp routine
attend to & complete 60min tasks even w/distractions
able to recall, use memory aids for daily
aware of impairments, thinks of consequences, acknowledges others
depressed, irritable, self-centered
60mins airs at 8, wow that show makes me sad, i dont wanna die
Rancho Level IX
Purposeful, Appropriate: stand by on request
indp multi-task at least 2 hrs
assistive memory devices
abstract and complex thought with SBA on request
depression, easily irritable, self monitor appropriateness
9, help me remember that last bit to ending world peace
Rancho Level X
Purposeful, Appropriate: Mod Indp
multi task with periodic breaks
inpd health management (assistive devices)
inpd abstract and complex cognition
10, i am the whole picture, i am complete
concussion
mild TBI
a bump or jolt to either the head or the body that causes the brain to move rapidly inside the skull
may result in loss of consciousness 0−30mins
post traumatic amnesia (PTA) no longer than 24hr
imaging often show no damage
sx:
clumsy, slow, mood or behavior changes, vomiting, headache, dizziness, sensitivity, confusion
severe concussion: seek emergency services
drowsiness or inability to wake, loss con longer than 30s, pupils differ in size, headache gets worse, slurred speech
post-concussion syndrome
set of sx that may continue for weeks, months, or year after concussion
sx:
headache, fatigue, cognitive impairments, dizziness, depression, anxiety, impaired balance, sensory sensitivities, emotional problems
spinal cord injury (SCI)
nontraumatic or traumatic compression, shearing, or contusion to spinal cord
sx: vary depending on severity
spinal shock: 4-8wks, all reflex activity is obliterated BLOI > flaccid paralysis for time being
sensory deficits, loss bowel/bladder, loss temp control, decreased resp, sexual dysfunction, muscle tone changes
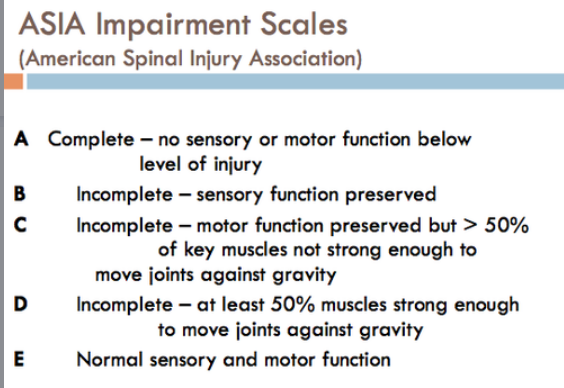
ASIA impairment scale
GRADE A: Complete, no motor or sensory
GRADE B: Sensory Incomplete, sensory but no motor function
GRADE C: Motor Incomplete, motor function is preserved below the neurological level, and the majority of key muscle groups have a muscle grade of less than or equal to 3/5
GRADE D: Motor Incomplete , motor function is preserved below the neurological level, and the majority of key muscle groups have a muscle grade of greater than or equal to 3/5
GRADE E: Normal; sensory and motor
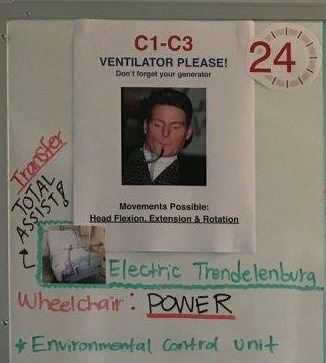
C1-C3 SCI
possible movements:
neck flex, etx, and rotation
limited movement of head and neck
functional capabilities:
ventilator dependent, unable to clear secretions (cough)
difficult or limited communication > AAC
total assist for ADLs and IADLs
total assist for bed mobility
indp use power chair with head or mouth controls
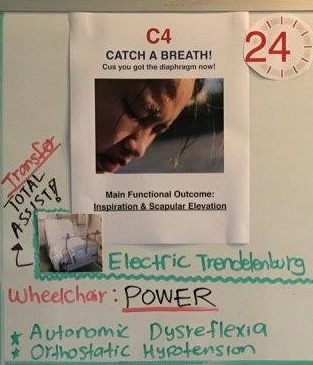
C4 SCI
PHYSICAL ABILITIES:
head & neck control
shoulder shrug (scapular elevation due to traps)
FUNCTIONAL GOALS
may require vent; assisted cough
operate power chair using head control, mouth stick, sip & puff or chin control
total assist for ADLs and IADLs, possible indp with AT for eating
total assist for bed mobility
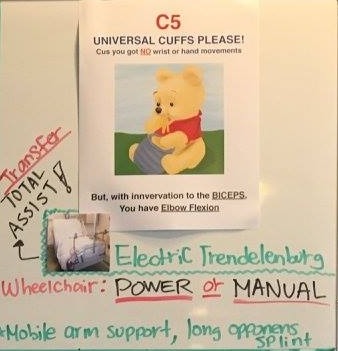
C5 SCI
PHYSICAL ABILITIES:
head & neck control, shoulder shrug (scapular elevation)
some shoulder control
elbow flexors (biceps, brachialis) able to
bend elbows & turn palms up
FUNCTIONAL GOALS:
with DME can be independent with eating & grooming
with caregiver assistance may be able to perform UE dressing & some bathing
total assist for mobility
power w/c
assisted cough
AE: universal cuff
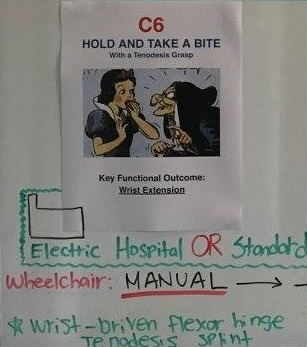
C6 SCI
PHYSICAL ABILITIES:
movement of head, neck, shoulders, arms & wrist
ADD: turn palms up & down & extend wrists
C6 wrist extensors: extensor carpi radialis longus & brevis)
tenodesis grasp!!
FUNCTIONAL GOALS:
DME, can be independent with eating & grooming & UE dressing
may need assist with LE dressing
some assist for transfers (slide board)
ultra light manual w/c or power for ease in community/uneven distances
AE: universal cuff, dressing stick, leg lifter, long-handled sponge
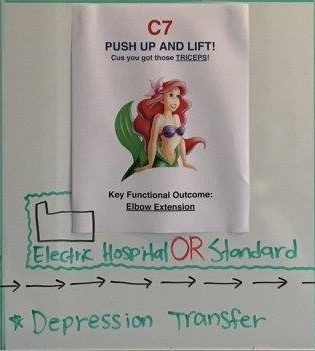
C7 SCI
PHYSICAL ABILITIES:
movement of head, neck, shoulder, arms, & wrist
elbow extensors (triceps)
FUNCTIONAL GOALS:
may need some or no assistance for ADLs and functional mobility
independent transfers
independent with manual w/c
C8 SCI
PHYSICAL ABILITIES:
movement of head, neck, shoulders, arms, ELBOWS!!, wrist, HANDS!!
added strength & precision of hands & fingers
C8: finger flexors (flexor digitorum profundus) to middle finger)
T1: small finger abductors (abductor digiti minimi)
FUNCTIONAL GOALS:
may need some or no assistance for ADLs and functional mobility
independent transfers
independent with manual w/c
T2-T12 SCI
PHYSICAL ABILITIES:
normal function head, neck, shoulders, arms, hands, fingers
increased use of rib & chest muscles
T10-12: more improvements in trunk control due to increased ab strength
FUNCTIONAL GOALS:
independent!! in self care (bowel & bladder), w/c push ups for pressure relief, bed mobility & transfers
manual w/c
load and unload w/c for driving with hand controls
L1-S5 SCI
FUNCTIONAL ABILITIES
gradual gain of hip, knee, foot movements
depending on level of injury, some degree of voluntary bladder, bowel, & sexual function returns
FUNCTIONAL GOALS
ambulate with specialized leg braces & walking device
functionality of ambulation depends on strength & movement in LEs
may use w/c for community mobility
SCI complications
respiratory complications! (pneumonia)
decubitus ulcer
orthostatic hypotension
rapid decr in BP when changing positions
DVT
autonomic dysreflexia: abnormal response to noxious stim resulting in extreme incr in BP, headache, sweating
usually pain or irritant BLOI
medical emergency
UTI
heterotopic ossification
cerebral palsy
caused by malformation of brain structures and/or injury to brain structures during prenatal, perinatal, or postnatal periods (until 2yrs)
four P’s (premature)
common causes
premature birth w/injury to brain
low birth weight
maternal infection or infant infection
hypoxia!!
non progressive
comorbidities:
respiratory problems, seizure disorders, scoliosis, contractures, pressure sores
cognitive and language skills vary
early indicators:
hypotonia, spasticity, head lag, persistent primitive reflexes, no protective responses, clonus, global delay
types:
spastic, dyskinetic, ataxic, mixed
spastic CP
most common (88%)
increased muscle tone (hypertonia)
muscle spasticity: velocity-dependent resistance to stretch; stiffness upon movement
combo of hypo and hyper tone in different muscles
restricts voluntary movement, present at rest
white matter, pyramidal(UMN)
TYPES: hemiplegia, diplegia (preemie), quadriplegia (most severe)
dyskinetic CP
asphyxiation at birth (hypoxic ischemic encephalopathy)
abnormal muscle tone which may involve whole body
decr tone during sleep
changing pattern of muscle tone
involuntary movements often present
TYPES:
chorea
rapid, random, jerky movements
athetoid
slow, writhing, involuntary movements; wrist & feet
choreoathetoid
combo of slow and rapid
dystonic
involuntary muscle contraction with repetitive movements and abnormal posture
ataxic CP
cerebellum involvement
balance and coordination issues
abnormal voluntary movement
difficulty with trunk/limb position in space
often walk with unsteady gait, with a wide based gait
difficulty with precise coordination (overshooting)
Gross Motor Functional Classification System (GMFCS)
walks without limitations
walks with limitations
walks using hand-held mobility device
self-mobility with limitations; may use powered mobility
transported in manual wheelchair
Manual Ability Classification System (MACS)
handles objects easily and successfully
handles most objects but with somewhat reduced quality and/or speed of achievement
handles objects with difficulty; needs help to prepare and/or modify activities
handles limited selection of easily managed objects in adapted situations
does not handle objects and has severely limited ability to perform even simple actions
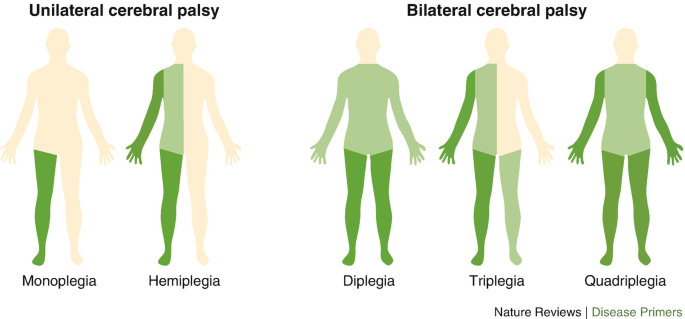
CP distribution
quadriplegia
all 4 limbs
diplegia
all four limbs; LEs more severely affected than UEs
hemiplegia
one side affected; UE usually more involved
triplegia
three limbs; usually UEs + LE
monoplegia
only one limb; usually UE
chorea
brief, purposeless, involuntary movements of distal extremities and face
dyskinesias
involuntary, nonrepetitive, but occasionally stereotyped movements affecting distal, proximal, and axial musculature
myoclonus
brief and rapid contraction of muscle or group of muscle
parkinson’s disease
long-term, slowly progressive movement disorder
may live 20-30 years, onset 40+
progressive loss of voluntary and involuntary motor function
CAUSE: hereditary > environmental
death of neurons of the substantia nigra (SN), specifically pars compacta (PC) portion, in the basal ganglia (BG), resulting in decreased production of neurotransmitter dopamine
lewey bodies contribute to PD
cardinal signs: TRAP
Tremor
Rigidity
Akinesia
Postural instability
TX:
pharma for dopamine
side effects > more as disease progresses, involuntary movements, become resistant
stages of parkinson’s
unilateral tremor, rigidity, akinesia, minimal or no functional impairment
bilateral tremor, rigidity or akinesia, w/or w/out axial signs, indp with ADLs, no balance impairments
worsening of sx
first sign of impaired righting reflexes, onset of disability in ADLs, can be indp
requires help with some or all ADLs, unable live alone w/out assistance, able to walk and stand unaided
unable to stand, walk, or perform ADLs, w/c and max a
neural tube defects
complex interaction of environmental and genetic factors, which contribute to malformation of brain, vertebrae, and spinal cord
lack of brain development, malformation of skull, malformation of vertebral arches
anencephaly: more severe malformation of skull and brain; no neural development above brainstem
encephalocele: malformation of the skull where portion of brain protrudes
spina bifida: most common
lack of folic acid may induce
onset: prenatal (within 26 days conception)
outcome: spontaneous abortion is common, infancy mortality high, better outcomes with frontal malformation
spina bifida
malformation of vertebral arches
types
occulta: bony malformation with separation of vertebral arches, no external manifestations
most common
occult spinal dysraphism (OSD): external manifestation (red birthmark, patch hair, dermal sinus, dimple)
sx: usually none, maybe slight instability, mild gait alterations, bowel/bladder problems
cystica: exposed pouch of spinal cord and meninges
meningocele: protrusion of sac through spine containing spinal fluid and meninges; no spinal cord protrusion
sx: slight instability, minimal functional impairments (no spinal cord protrusion)
myelomeningocele: protrusion of spinal fluid, meninges, and spinal cord (most common in lumbar)
sx: sensory and motor deficits occurring BLOL, paralysis BLOL, bowel/bladder incontinence (S2-S4)
tx: shunts, neonatal sac repair, therapy
neurogenic bowel
absence of innervation (bladder, urethra, and bowel)
bowel and bladder dysfunction present in all children with meningomyelocele
INTERVENTIONS:
- Clean Intermittent Catheterization
- Bowel Management
tethered cord syndrome
end of spinal cord adheres to one of lower vertebra > spinal cord stretched > damaged and interferes with blood supply to spinal cord.
may go undiagnosed until sx occur
sx:
visible signs > hairy patch, dimple, red mark
bowel/bladder difficulties, gait disturbances, feet deformities, low back pain, scoliosis
chiari type II malformation
more severe form
displacement of brainstem and cerebellum into spinal canal causing compression on spinal cord, cerebellum, and brain stem
common in meningomyelocele
sx:
trouble breathing, swallowing problems, weakness, arching of head backward
ventriculo-peritoneal shunt (VP shunt)
most common type shunt for hydrocephalus
divert CSF from ventricles to abdomen to be better absorbed
known to fail!!! early recognition is key
COMPLICATIONS:
blocked or infected
sx: extreme head growth, regression, change in UE fxn, decline in cog fxn, impaired vision, seizures, LOB
by 2-3 yrs half of shunts have failed and been replaced
muscular dystrophies
group of degenerative disorders resulting in muscle weakness and decreased muscle mass due to hereditary disease process
absent muscle protein dystrophin
blood test or biopsy to ID
onset: anytime, avg age > 5yrs
progression: may be rapid & fatal or stable (earlier the appearance of sx > more severe and rapid)
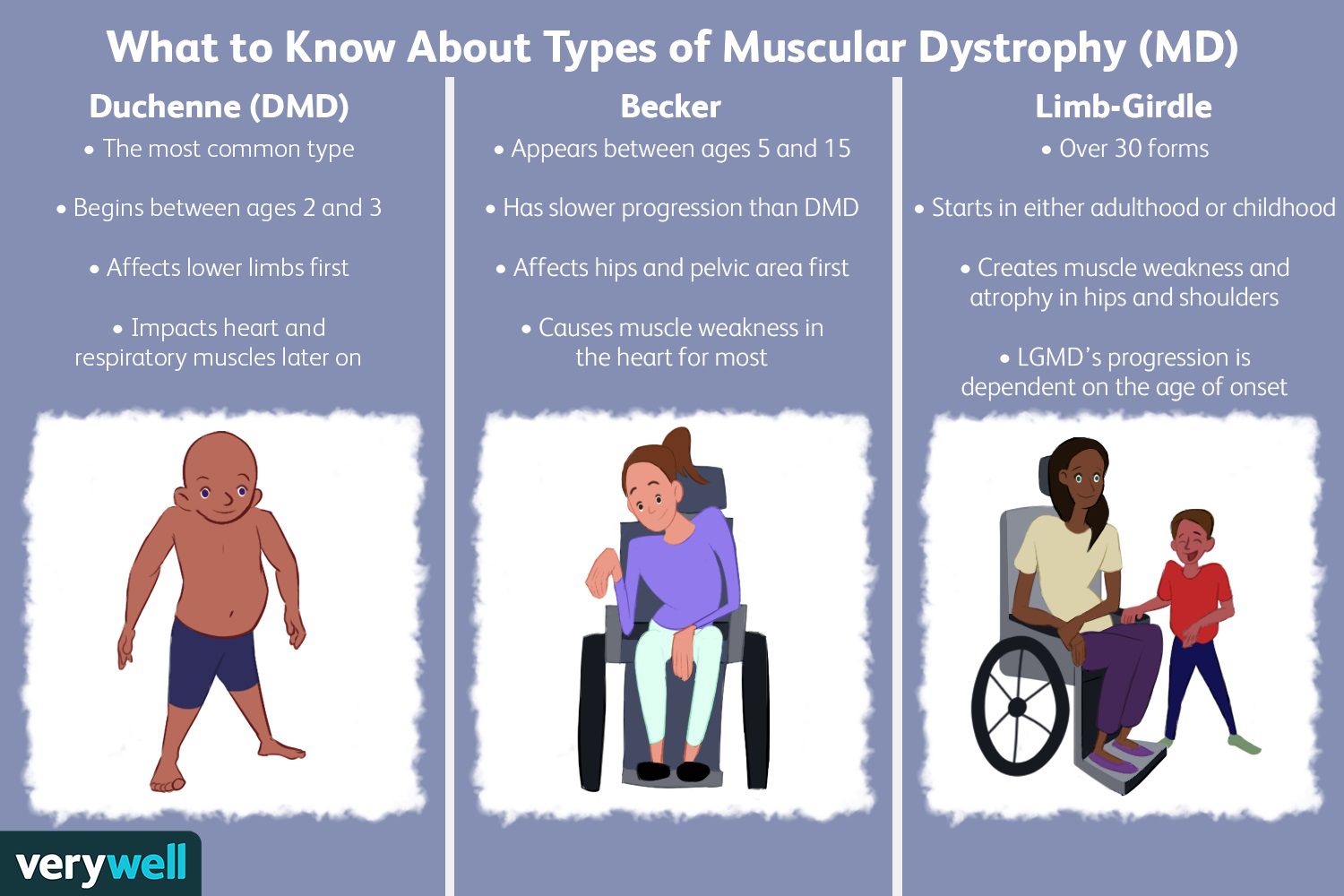
types
Duchenne’s (DMD)
fast
Becker’s (BMD)
slow
limb-girdle (LGMD)
onset late life, affects pelvis and shoulders, slow
facioscapulohumeral (FSHD)
early adolescence, slow
myotonic (DM)
emery-dreifuss (EDMD)
distal muscular dystrophy
oculopharyngeal muscular dystrophy
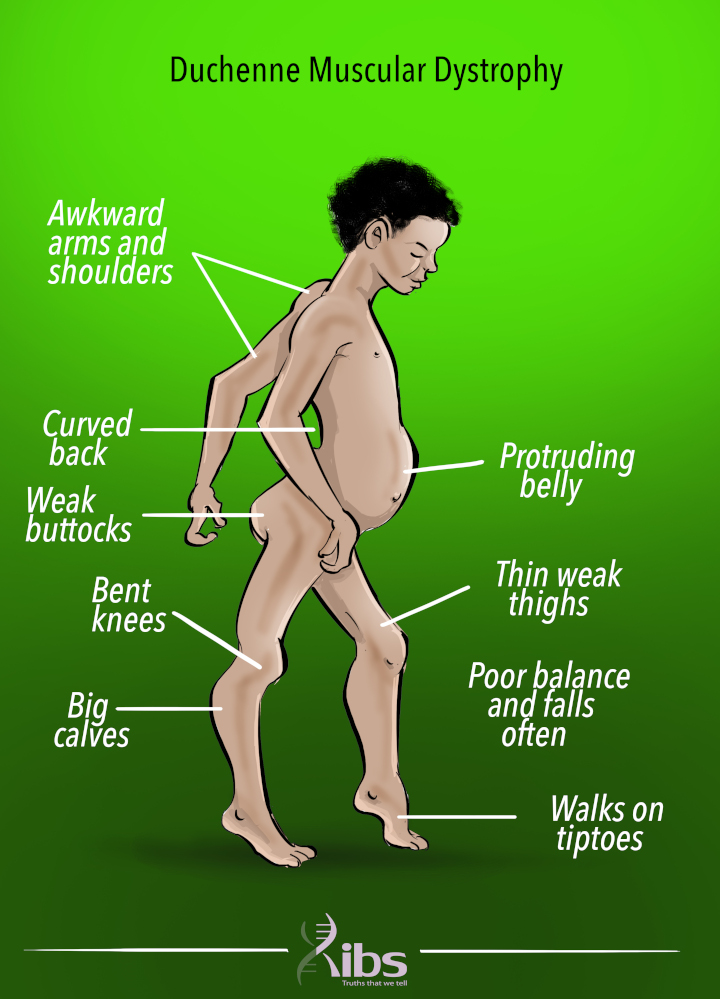
duchenne’s MD (DMD)
most common
boys!
detected btw 3-5yrs, survival rates > rarely beyond 20yrs
sx:
pseudohypertrophy (enlarged calf muscles)
weakness at proximal joints > sig fxnal mobility impairment
trendelenburg’s waddle
difficulty getting up from floor > Gower’s
muscle weakness in all voluntary (incl. heart and diaphragm)
behavioral/learning difficulties
becker’s MD
slower to progress than DMD, less severe, and less predictable
survival into late adulthood
sx:
loss motor fxn hips, thighs, pelvic, and shoulders
enlarged calves
cardiac system involvement
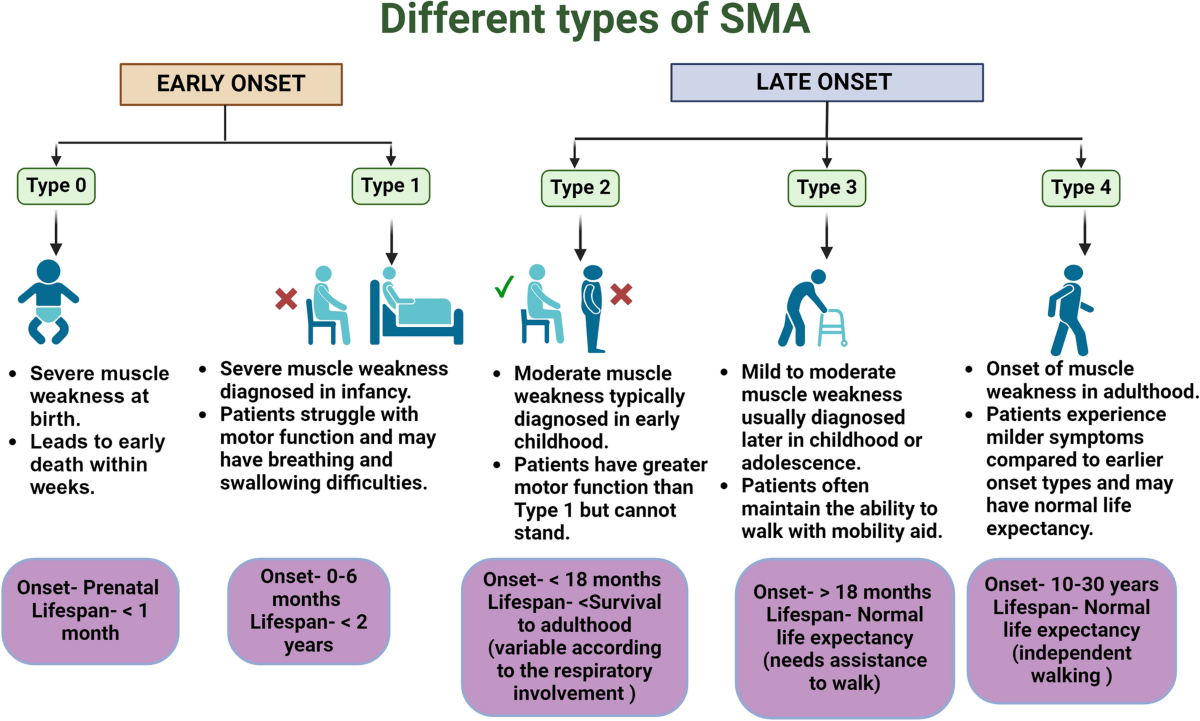
spinal muscular atrophy
weakness of voluntary muscles of shoulders, hips, thighs, and upper back resulting in spinal curvature
muscles for breathing and swallowing can be affected
age of diagnosis and onset determines severity and functional deficits
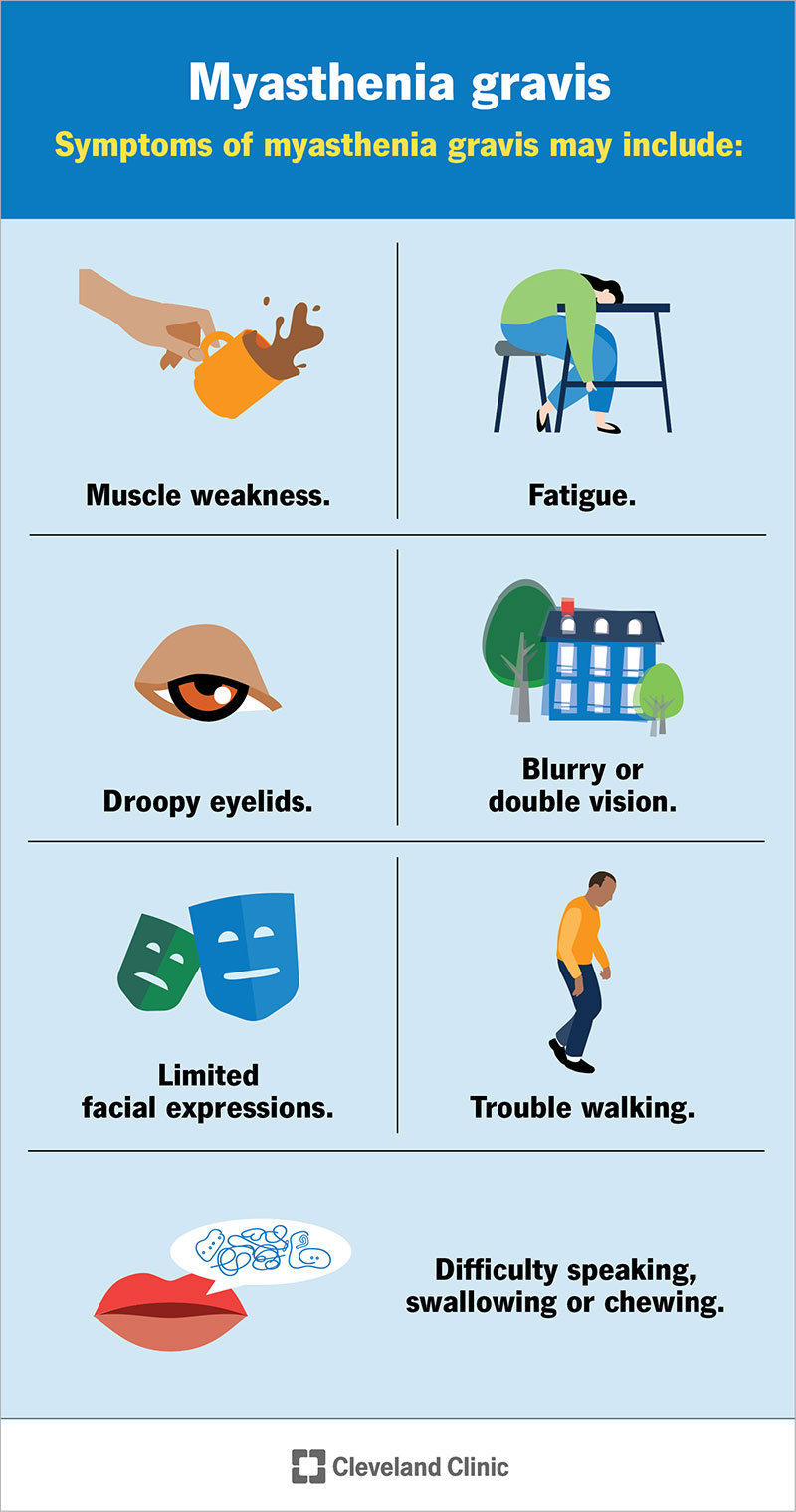
myasthenia gravis
disease caused by autoimmune attack on acetylcholine receptors at NMJ
initiating event unknown
onset & prognosis: any age, most often young women and older men, prognosis varies but usually progressive
can be congenital
sx:
ptosis, diplopia, muscle fatigue, dysphagia, and proximal limb weakness
sensation and deep tendon reflexes intact
sx fluctuate, relapsing periods
mysathenic crisis: progressive weakness, tachycardia, tachypnea, dysphagia, impaired speech, anxiety, decr respiratory fxn > seek emergency services!!
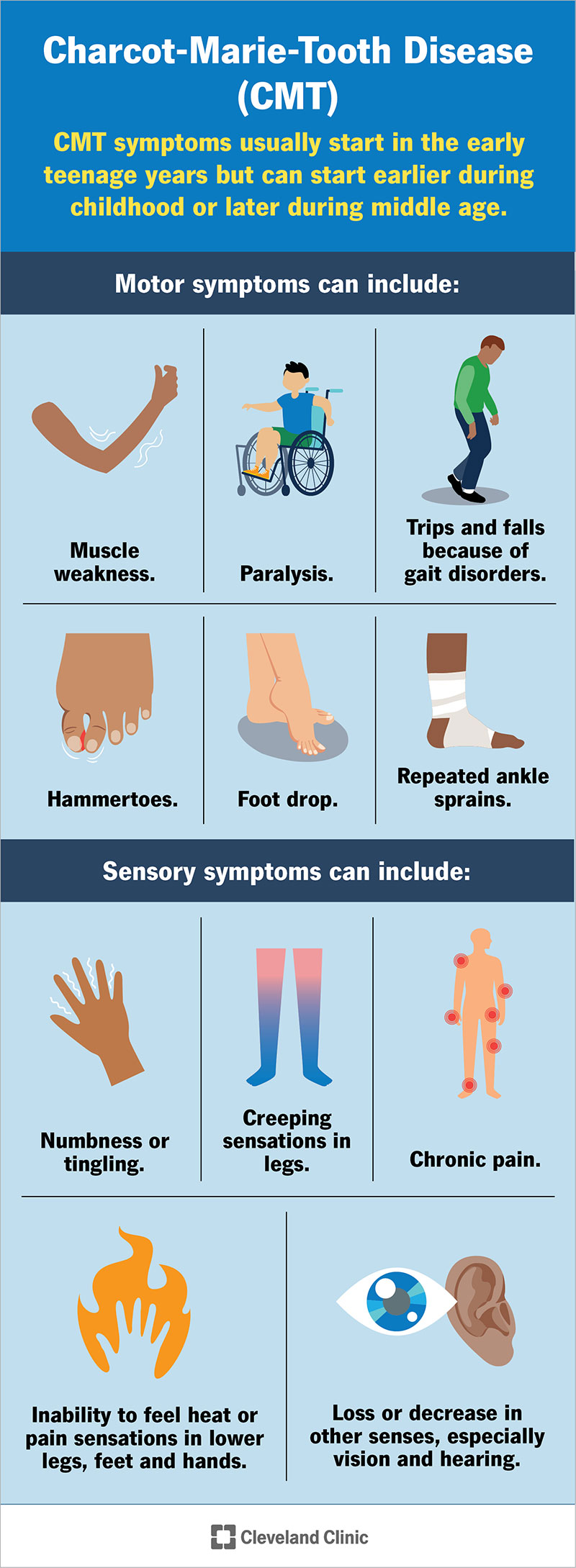
charcot-marie tooth disease
involves peripheral nerves marked by progressive weakness, primarily in peroneal and distal leg muscles
occurs in teen years or earlier
myopathies
sx similar to dystrophies but myopathies progress slowly with better prognosis
weakness of face, neck, and limbs
progressive supranuclear palsy (PSP)
rare brain disease causing
progressive problems with gait and balance
complex eye movements
cognitive impairments
classic sign: inability to coordinate eye movements causing blurry vision
other sx: altered mood, depression, apathy, progressive dementia
can be confused w/parkinsons however PDP is more rapid with NO tremors
huntington’s chorea
autosomal dominant disorder
onset & prognosis: insidious at middle age > progressive until end of life
sx:
choreiform movements and progressive ID
chorea movements (rapid, jerky, unpredictable)
psychiatric disturbances
impaired walking and balance
cerebellar/spinocerebellar disorders
lesions
degenerations
disorders
ataxia, dysmetria (under-overshoot mvmts), dysdiadochokinesia (inability perform rapid mvmt sequences), hypotonia, movmt decomp, intention tremors, nystagmus
cerebellar lesions:
strokes, tumor deposits, MS, alcoholism
spinocerebellar degenerations:
progressive ataxia due to degeneration of cerebellum, brain stem, spinal cord, peripheral n, and basal ganglia
types: spinal ataxias, cerebellar ataxias, multiple system degeneration
friedrichs ataxia: onset in childhood causing gait unsteadiness, UE ataxia, tremors, areflexia, scoliosis
Amyotrophic lateral sclerosis (ALS)
motor neuron disease of unknown etiology
more prevalent in men than women
average onset at 57, prognosis 2-5yrs
sx:
muscle weakness & atrophy. distally & asymmetrically
begins at hands
cramps precede weakness
spasticity, hyperactive deep tendon reflexes, dysarthria, dysphagia
sensory systems, eyes, urinary
medication management (2 FDA approved options)
tx focused on secondary complications (spasticity)

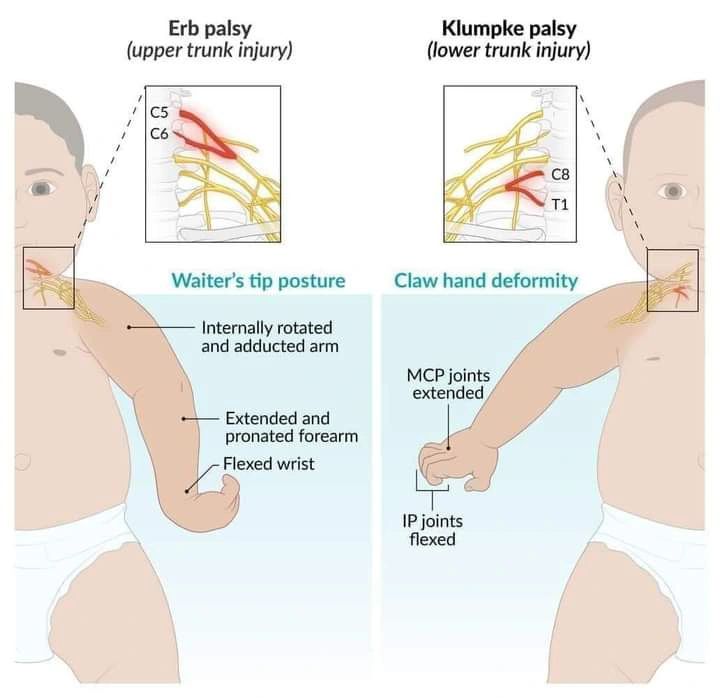
brachial plexus disorder
secondary to traction during birth, invasion of metastatic cancer, post-radiation tx, or traction injury
common in shoulder dystocia at birth
sx:
mixed motor and sensory disorders corresponding to limb
rostral (medial/proximal) injuries = shoulder dysfunction
caudal (lateral/distal) injuries = hand dysfunction
common injuries:
Erb’s palsy: paralysis of upper Brachial plaxus w/ C5-6 nerves
shoulder paralysis, arm cannot be raised, weak elbow flexion, weak scapula
6mos > contractures may form
waiters tip position: arm straight and wrist fully bent
Klumpke’s palsy: paralysis of lower BP w/ C7-8 and T1 nerves
rare compared to Erbs
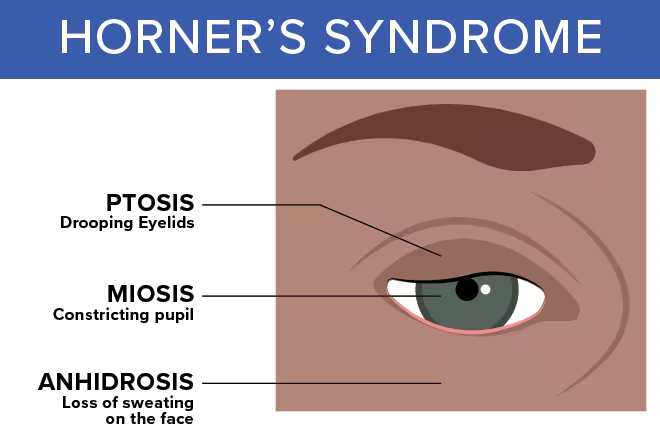
paralysis of hand and wrist with ipsilateral horners (miosis, ptosis, and facial anhidrosis)
limp hand and immobile fingers
horners syndrome
miosis
ptosis
facial anhidrosis
peripheral neuropathy
multiple or single nerve affected due to variety causes
trauma, pressure paralysis, forcible overextension of joint, hemorrhage, diabetes M, lyme disease, vascular disease, malnutrition, alcohol abuse
sx:
sensory, motor, reflex, and vasomotor sx
pain, weakness, paresthesia at affected nerve area
tx focuses on underlying cause not neuropathy itself
guillian-barre syndrome
unknown cause
autoimmune disease that occurs after infection, surgery, or immunization (little evidence)
acute and rapidly progressing demyelination of peripheral nerves and spinal nerve roots
onset & prognosis: any age, 2-4wk recovery, most ambulatory in 6mos, half have mild neurological deficits
sx:
symmetric muscular weakness and mild distal sensory loss
distal to proximal, gradual loss
minor sensory signs (painful extremities)
deep tendon reflexes lost (sphincters spared)
respiratory failure and dysphagia in some cases
post-polio syndrome (PPS)
some motor neurons infected by polio recover, after years of stability > break down and cause muscle weakness
onset & prognosis: 15yrs after polio, slow progress w/good prognosis
sx:
new weakness, easily fatigued, muscle pain, joint pain, cold intolerance, atrophy
multiple sclerosis (MS)
slowly progressive CNS disease characterized by patches of demyelination in brain and spinal cord
onset, prevalence, prognosis
most often btw 20-30yrs (diagnosed in 30’s)
prognosis variable
diagnosed by sx criteria (maybe MRI for lesions)
multiple and varied neurologic sx with insidious onset
fatigue,
paresthesias of extremities, trunk, or face
weakness or clumsiness in leg or hand
visual distrubances
emotional disturbances
balance loss or vertigo
bowel/bladder dysfunction
cognitive changes (apathy, memory loss, inattention)
spasticity, incr reflexes, ataxia, tremors, pain
sexual dysfunction
courses:
relapsing remitting
secondary progressive: slow progress with plateau periods
primary progressive: no remission or flare-ups > steady progression
progressive relapsing: steady progression despite relapse/remission (keep getting worse episodes)
gate control theory
transmission of sensation at spinal cord level is controlled by balance btw large fibers and small fibers
activity at large fibers can block activity of small fibers
EX: massages for body pain
acute V chronic pain
acute
provoked by noxious stim and associated with underlying pathology (has a source)
signs: sharp pain w/sympathetic changes (incr HR, incr BP, pupil dilation, sweating, etc.)
resolves with tissue heal
control is associate with improve recovery, mobility, decr complications & readmission
chronic
persists beyond usual course of healing
present for greater than 6 mos with no underlying pathology
very debilitating and impede participation
referred pain
pain arising from deep visceral tissues that is felt in body region remote from site of pathology
tenderness and cutaneous hyperalgesia
EX: left arm pain with heart attack