EOC - Medical Interventions
1/352
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
353 Terms
What is a Medical Intervention?
Anything that helps us prevent, diagnose, and treat our patients
Types of Medical Interventions
1) Prevention
2) Therapy & Rehab
3) Diagnostics
4) Surgery
5) Medical Devices
6) Pharmacology
7) Immunology
8) Genetics
Examples of Prevention
Screenings like colonscopies
Tests like lipid panels
(Anything that helps prevent a disease)
Examples of Therapy & Rehab
Physical Therapy
Rehabilitation
Recovery from injury
Occupational Therapy
Improve mental health
(treatment of recovery from disease/injury)
Examples of Diagnostics
CT Scans
PET Scans
Endoscopy
Biopsies
(Any test used to help confirm/rule out a disease/condition)
Examples of Surgeries
Appendectomy
Transplants
(Procedures to remove/repair parts of the body to fight off disease)
Examples of Medical Devices
Pacemaker
Catheters
Prosthetics
(Any instrument/machine that is intended for the usage of medical purpose)
Examples of Pharmcology
Ibuprofen
Acetaminophen
Adderall
(Drugs & Chemical that aid/affect the biological system)
Examples of Immunology
Vaccines
Allergy shots - reduces the sensitivity of immune system to certain allergens
(Treatments that use the immune system to fight off disease)
Examples of Genetics
Genology
(Studying how genes and traits are passed from one generation to the next)
1st step of sequencing
Isolate Target DNA
2nd Step of sequencing
Do PCR
Process: Polymerase Chain Reaction (PCR)
Materials:
Primers
"Start flag" for polymerase
Prepares target DNA for the rest of PCR
Thermal Cycler
Machine that does PCR
DNA Polymerase
Enzyme that adds nucleotides to target DNA
Builds DNA
Isolated Target DNA (From Step 1)
Product: Millions of target DNA
3rd step of sequencing
PCR again
Process: PCR repeated
Materials:
Same materials (From Step 2)
Fluorescently tagged free Nucleotides
Products: Differently sized fluorescently tagged strands of target DNA
4th step of sequencing
Gel electrophoresis to get data into computer graph
Process: Gel electrophoresis
Materials:
Automatic sequencer
Machine that does gel electrophoresis
Target DNA (From Step 3)
Fragments with fluorescent tags
Product: Graph with colored peaks
Auto-sequencer separates fragments and sends those fragments through a tube
Tube is positive at top and negative at bottom
Tube has lasers on bottom that reads fragments and uploads a peak on a computer graph
5th step of sequencing
Analyze Graph Data
Materials:
Graph (From Step 4)
Products: Complementary sequence of Target DNA
What base pair is blue?
Cytosine (C)
What base pair is green?
Adenine (A)
What base pair is black?
Guanine (G)
What base pair is red?
Thymine
RULES OF GRAPH ANALYSIS
1) One peak, one color = one base
2) Overlapped peaks = "N"
3) Bigger peaks between two is the one you read
4) Sections with a lot of "N's" get taken out (mostly at start or end)
(If a section with a lot of "N's" is in the middle of data, redo lab)
Bioinformatics
The application of computer technology to collect, store, and analyze biological data and information
BLAST
Basic Local Alignment Search Tool
What do BLAST results show?
Shows a database of similar sequences to that of the input sequence such as the patient sample to help figure out what organism is in the patient sample and, from that, find the disease the patient has
What are the several result values we're given from a BLAST?
Max Score
Total Score
Query Coverage
Expect Value
Identity Value
Max Score
Highest local alignment score from query/input sequence to a sequence in the database
(Reflects the best match as a higher max score means better alignment)
Total Score
Sum of alignment score from query/input sequence to a sequence in the database
(Overall similarity between query/input sequence and aligned database sequence)
Query Coverage
Percentage of query/input sequence that overlaps with reference/database sequence
Expect Value ( E Value)
Number of hits we expect to see by chance
Helps to see if hits are unique or not
Lower the E-value, the more precise the hit is
Identity Value (Ident Value)
Percentage of base pairs that are the same between the query/input sequence versus the reference/database sequence
Query Coverage vs Identity Value Example
CCCCCCCCCC target
CCCACCACCC query/input
might be 100% query coverage 80% identity
Steps of an ELISA Test
1) Put in patient sample
2) Primary antibodies
3) Secondary antibodies
4) Substrate
5) Color Change (if pateint had antigen present)
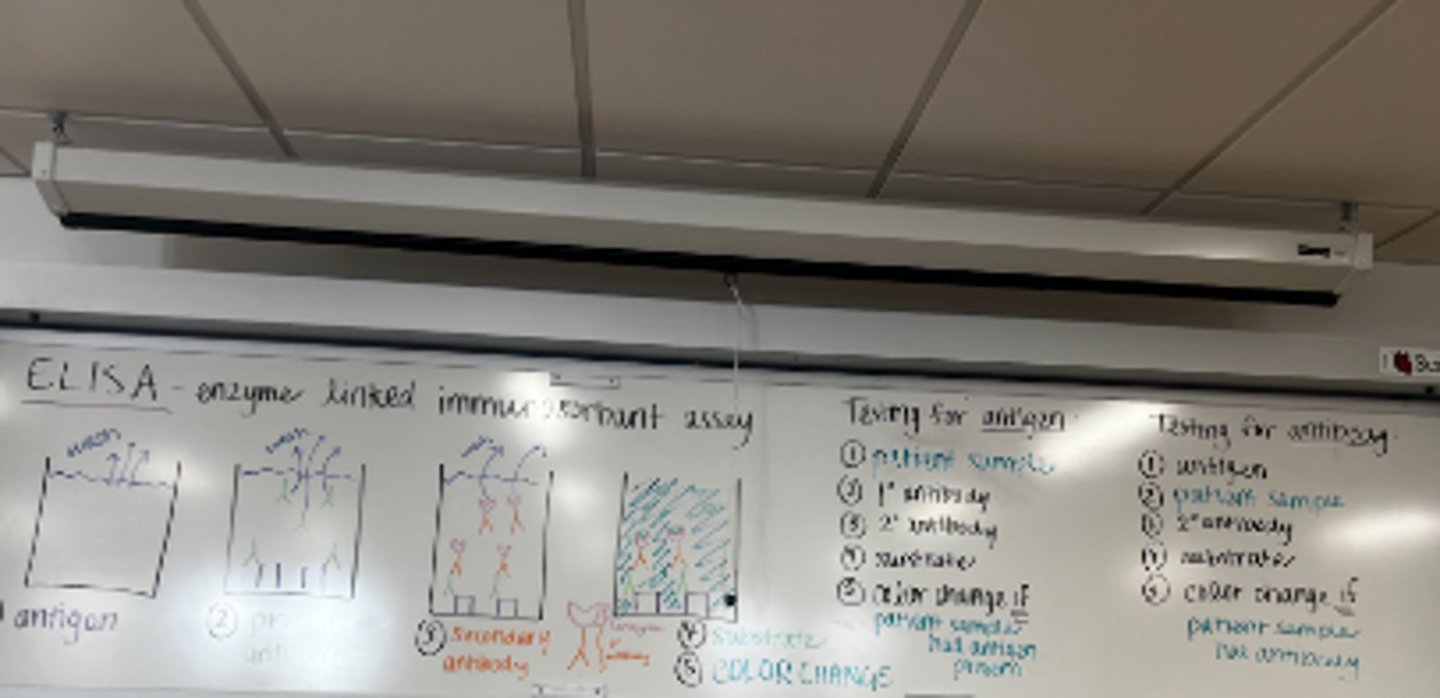
What does ELISA stand for?
Enzyme Linked Immunosorbent Assay
Steps of an ELISA Test if testing for antibodies
1) Antigen
2) Patient sample
3) Secondary antibodies
4) Substrate
5) Color Change (If patient sample has antibody present)
Innate/Nonspecifc Immune system
First line of defense against invaders
Includes external barriers
(Skin, mucous membrane)
Includes internal defenses
(Phagocytes, antimicrobial proteins, attack cells)
Phagocytes
Surrounds and kills any invading cells
Types of phagocytes include:
Neutrophils
Most abudant type of WBC
Self-destruct after ingesting a pathogen
Natural Killer Cells
Can kill own cells if they're infected or are cancerous
Normal cells contain a special protein called MHC1
If a cell stops making MHC1, it's become infected
Natural Killer Cells detect this and then "poke" the infected cell
From that, the cell will go into apotosis or "programmed cell death"
Inflammatory Response
Redness
Swelling
Heating up
Pain
Histamine
Causes vasodilation (redness & heat at site of injury)
Heat increases metabolic rate of repairing
Causes swelling through increasing permability of blood vessels
Causes nearby capillaries to realease protein-rich fluids
Leukocytosis
Release of neutrophils from bone marrow
Adaptive/Acquired Immune System
Slow to act
Must first recognize pathogen before attacking it
Has ability to remember specific pathogens
Can fight throughout whole body at once rather than be restrictive
Deploys Humoral Immunity & Cellular Defenses
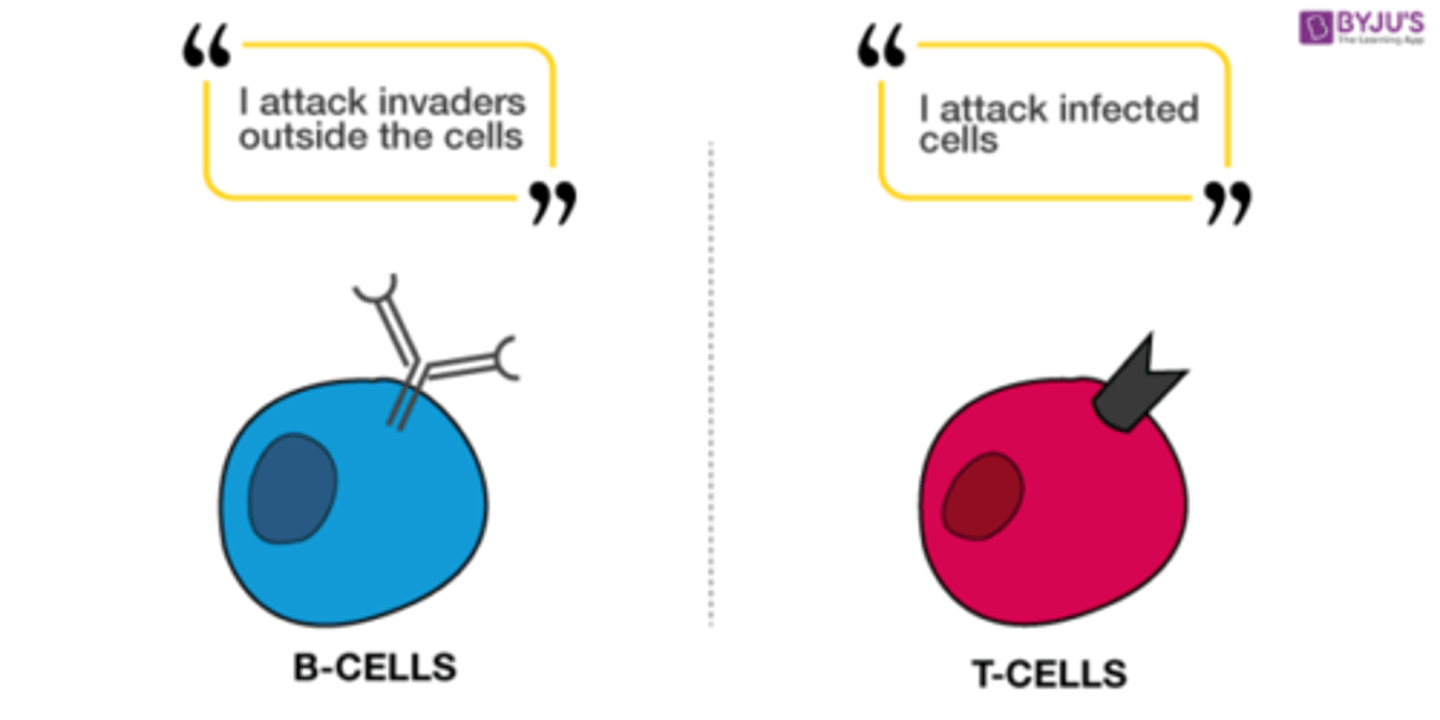
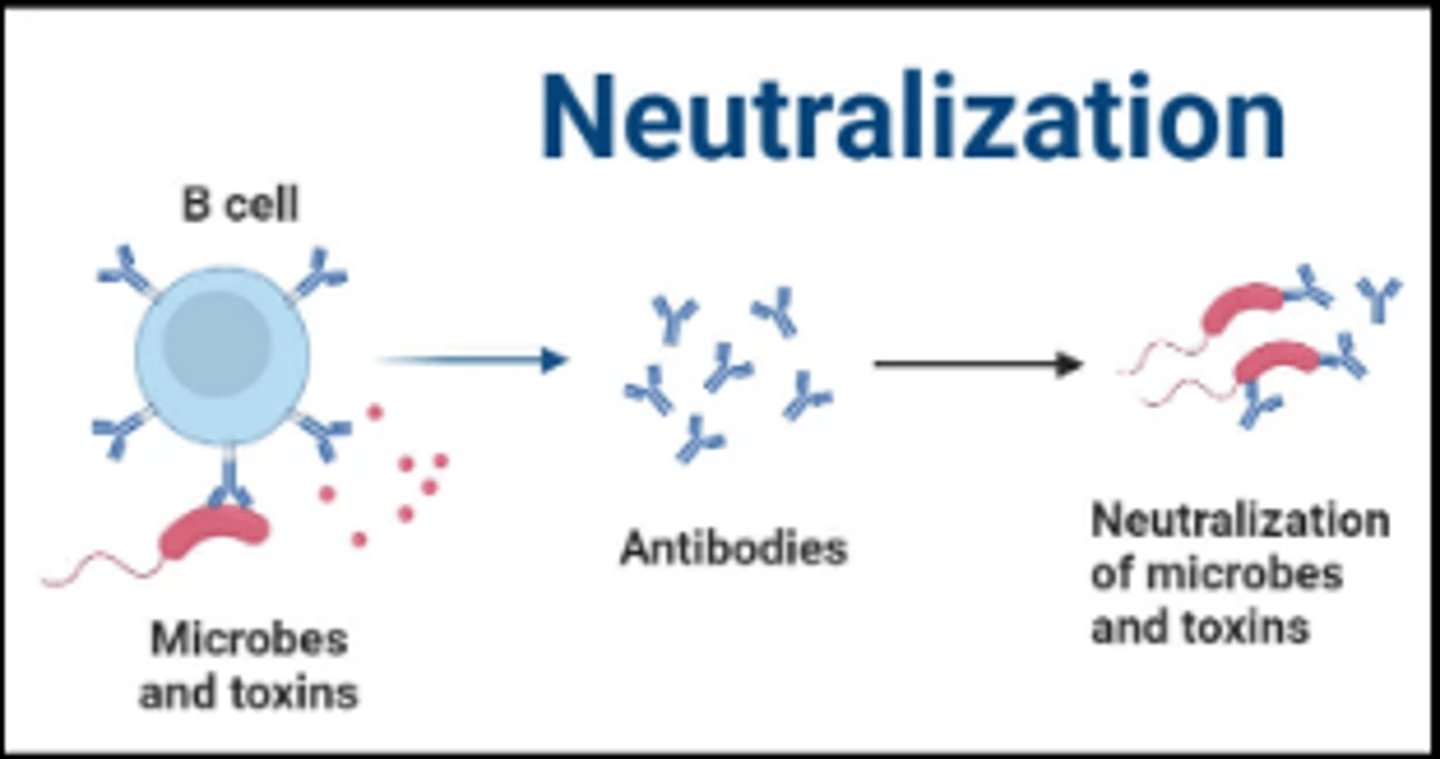
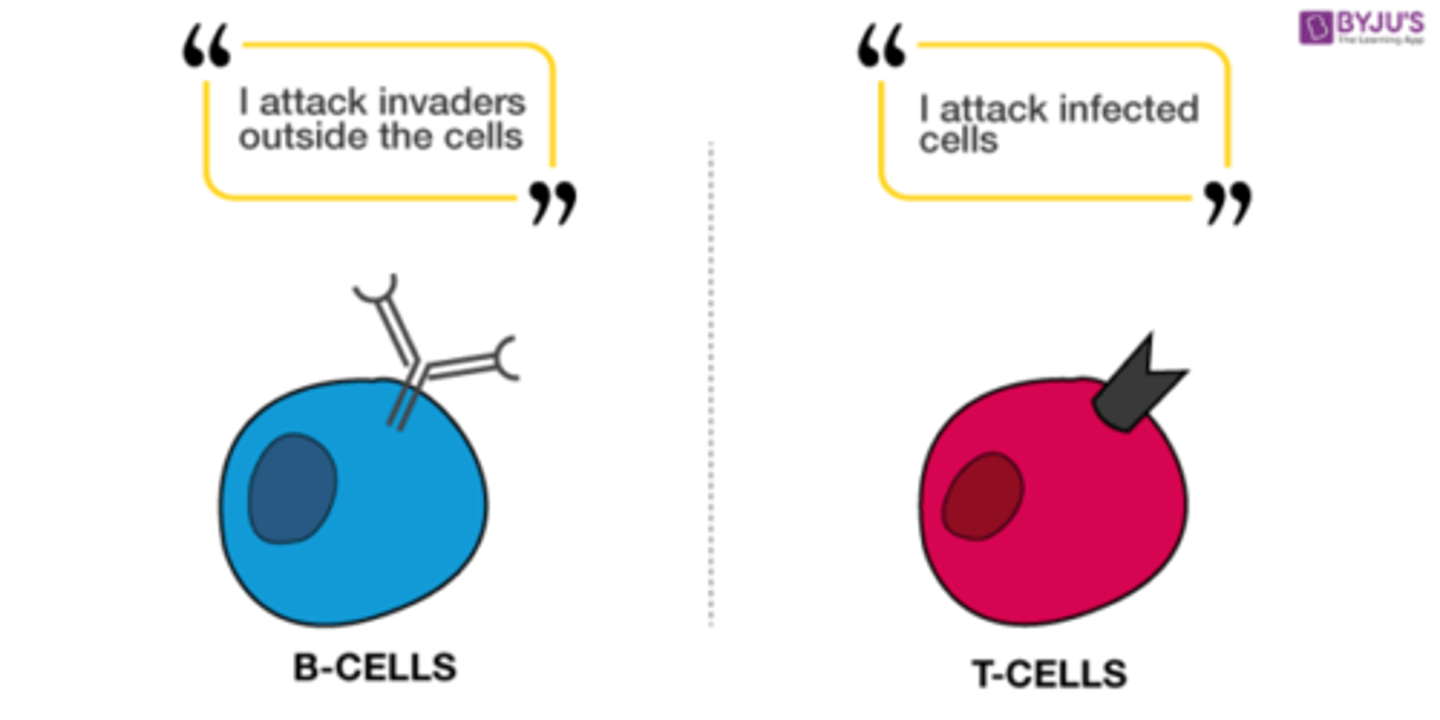
Humoral Immunity
Sends out antibodies
Antibodies
Patrol through blood & lymph
Combat viruses & bacteria moving around the space between cells
(Body has to be able to detect pathogens like bacteria, viruses, and fungi to be able to defend against them)
Antigens
Large molecules not normally found in body
B-Lymphocyte
Originates & matures in bone marrow
As it matures, it develops the ability to identify pathogens clearly
Also learns how to bind to a specific antigen
Develops self-tolerance (ability to not attack body's own cells)
What happens when a B-cell detects an antigen it has antibodies for?
It recognizes it and binds to it
Memory Cells
Cells that remember the antigen and stay in your immune system so that, if that specific antigen invades your body again, it can quickly identify it and fight it
Neutralization
Antibodies block binding sites on viruses/bacterial toxins, inhibiting them to attach to tissues
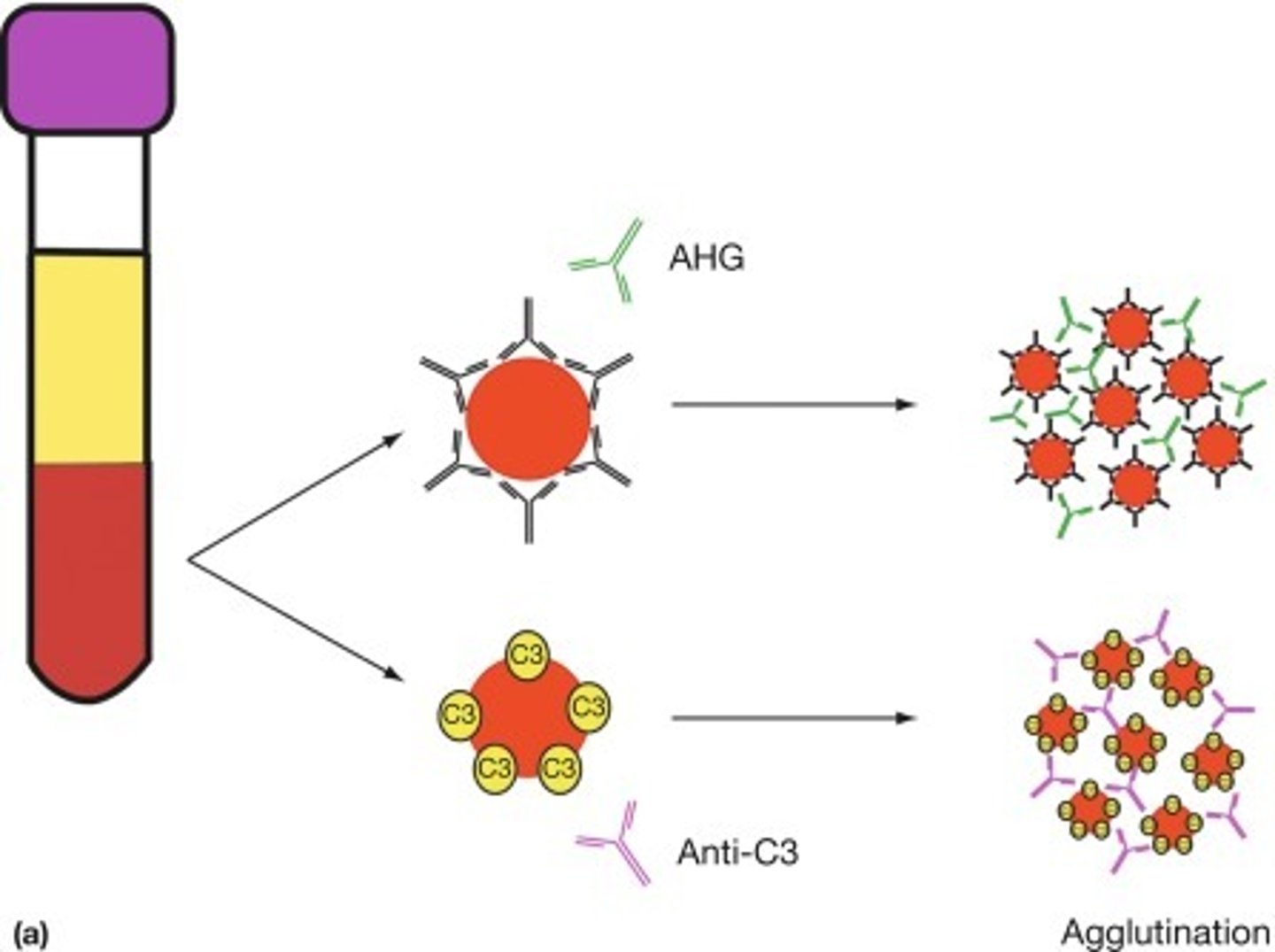
Agglutination
Antibodies binding to multiple antigens
Inhibits movement of antigen (helps macrophages)
What does Humoral response do?
Humoral response helps the body achieve immunity
Can occur naturally or artificially (vaccination)
Babies' passive humoral immunity
Babies obtain passive humoral immunity while in the womb
However, baby's own system won't remember an antigen if it gets infected again
T-Lymphocyte
Goes after infected body cells
Causes inflammation, activates macrophages, increase response of other T-cells, regulate much of immune response
MHC protein
Presents short chains of amino acids based on endogenous proteins
(proteins synthesized in cell)
Several different kinds
(Only need to know about Helper Ts & Cytotoxic Cells)
Helper T-Cells
Can help activate cells that kill invaders
"Calls the shots" in the immune system
Cytotoxic Cells
Kills infected cells
How do Helper T-cells work?
Helper T-cells will have specific receptors that'll only bind to a specific combination of a class 2 MHC & a specific antigen
If combination is met, Helper T-Cell bonds to MHC antigen and gets activated
Replicates & makes memory T-cells
Releases cytokines
Boosts signal that something is wrong in body
Tube Dilution
sample added/ total sample
Final Dilution
(current tube dilution) times (previous final dilution)
Concentration
(previous concentration)times (previous tube dilution)
Single Gene
Caused by changes(mutational) in a DNA sequence. This leads to a denatured
Cystic Fibrosis(Recessive - aa)
Mutation in the CFTR gene
Causes Lung Issues/Infertility
Huntington’s(Dominant - AA)
CAG mutation
Cognitive Problems
Muscle Dystrophy(Sex Linked - XaXb)
a group of diseases that cause progressive weakness and loss of muscle mass
Multifactorial
Caused by both environmental(causes genes to malfunction) and mutations in your genes. This affects multiple genes
Breast Cancer
Heart Disease
Alzheimer’s Disease
Caused by environmental factors and mutations
Cognitive decline and behavioral changes
Life expectancy decreases
Chromosomal Mutation
Either missing or having extra copies of a gene. It could also be a damage to a chromosome
Deletions or breaks or rejoining of a chromosome
Either adding 1 or deleting 1 chromosome
Down Syndrome
Trisomy(3 copies) of the #21 chromosome
Comes with intellectual disabilities and face features are deformed
Huntington’s Disease
A single #4 chromosome
Uncontrollable movements and muscle mass loss
Mitochondrial
Mutations in chromosomal DNA(in the mitochondria)
Passed from the mother gene
Optic Neuropathy
Is caused by mitochondria DNA mutations
Causes vision loss which is permanent
Leber Hereditary optic neuropathy
A genetic condition that leads to vision loss due to the degeneration of the optic nerve, often caused by mutations in mitochondrial DNA.
Difference between Diagnostic and Screening Test
Screening tests are used to detect potential health issues or diseases in asymptomatic individuals, aiming for early identification and prevention. These tests are typically applied to large populations, prioritizing sensitivity to catch as many potential cases as possible, even at the risk of false positives. Examples include mammograms, cholesterol checks, and newborn screenings. In contrast, diagnostic tests are used to confirm or rule out a disease or condition in individuals who are symptomatic or who have tested positive in a screening. These tests are more specific and accurate, minimizing false results to ensure a definitive diagnosis, which then informs treatment decisions. Screening tests often lead to follow-up diagnostic testing if abnormalities are detected.
What is Quad Screening
a prenatal blood test done during the second trimester of pregnancy (around 15-22 weeks) to assess the risk of certain birth defects in the fetus
4 things tested..
HCG
AFP
Estriol
Inhibin A
Blood drawn → goes to lab
Look for these proteins/hormones
If levels too high/low → risk of abnormalities
Can also check for risk of neural defects
First Trimester Screening
Occurs between weeks 10-15
Screen for a protein and a hormone : HCG Hormone or PAPP-A protein
Done by a blood draw → will be sent to lab, where they measure range of hormone/range (check if levels are too high/low) → if yes, then risk for potential abnormalities
Done simultaneously with the NT ultrasound (done at same time)
85% accurate – 5% false positive
Early on in pregnancy – making educated guesses to help parents make choices regarding their pregnancies, but it is not 100%
Cell-free fetal (CFF) DNA Analysis(Non-invasive Prenatal Screening)
Week 10 onwards (can get done anytime later in the future)
Mom will get blood drawn → sent to lab
CFF DNA isolated away from mom’s blood sample → testing just the fetus
Help determine risk of baby having abnormalities,
For pregnancies, separates baby and mother’s blood ( ensures mom doesn’t get rid of
Don’t have full picture / all DNA, not a full diagnosi
Chrionic Villus Sampling
Weeks 10-13
Diagnose baby with chromosomal abnormalities
Invasive test → mom comes in , needle put through her transcervical cervix, cut into placenta, CVS is anchor of placenta, where mom/baby info talks to each other, can aspirate (vacuum) up cells that belong to baby, can now pull apart, extract DNA, and analyze baby’s health
Transabdominal, needle inserted through abdomen instead
Next thing that can be determined is paternity (who is the father)
Risk of miscarriage
Risk of development issues
Amniocentesis
What is it, and what does it tell us?
A diagnostic test that takes a sample of amniotic fluid from the mother and using the cell DNA that is contained to diagnose certain chromosomal or genetic conditions, such as Down’s Syndrome or Cystic Fibrosis
When does it get performed?
Between weeks 14-20 of pregnancy
It isn’t a necessary test, and usually is ordered if a abnormality is detected by an ultrasound. Generally, Amniocentesis is offered if there’s a higher risk that the baby has a genetic condition
This could be from prior screenings, a previous pregnancy with a genetic condition, or a family history of a genetic condition
What happens during Amniocentesis?
First, an ultrasound is established to be able to locate the fetus, and gain an image of the amniotic sac(where the baby is located)
Then, a thin, hollow needle is inserted through the abdomen and uterus into the amniotic sac, but keeping it away from the fetus
The needle then extracts a small amount of the fluid from the sac(called a sample), to be tested for genetic and chromosomal defects
The needle is then removed from the abdomen
This process only takes 30-45 minutes on average, and the part with the needle usually lasts only 2-5 minutes long!
A sample is then sent to the lab for testing, and the results will typically arrive in about two weeks
Risk of miscarriage
Risk of development issues
NT Ultrasound
Nuchal Translucency Ultrasound
Weeks 10-15
Mom lies on back, gel is applied to stomach and wand is used to display images on a screen
Looking at (1) size of nasal bone, and (2) fluid volume of the back of the baby’s neck
Too high/low → indicates risk of chromosomal abnormalities | same if nasal bone not developing properly
Anatomy Ultrasound
Three names: fetal ultrasound, anatomy ultrasound, obstetric ultrasound
Mom lies on back, gel is applied to stomach and wand is used to display images on a screen
Looking at organ formation, size → can determine a baby's age, developing at proper rate, “too small or too big?”, checks heartbeat as well, also to confirm pregnancy
Occurs throughout pregnancies (confirmation of pregnancies, gestational age, continue through second / third trimester to keep track of development
Karyotype vs Pedigree
Karyotype:
A visual representation of an organism's chromosomes, arranged by size and shape.
It shows the number and structure of chromosomes, helping detect abnormalities like extra/missing chromosomes (e.g., Down syndrome).
Read by examining chromosome pairs for size, banding patterns, and the presence of 46 total chromosomes (in humans).
Pedigree:
A chart that tracks the inheritance of traits or genetic disorders through a family.
It shows relationships and whether individuals are affected, carriers, or unaffected.
Read by identifying symbols (circles for females, squares for males), shading (affected individuals), and lines connecting relatives to follow inheritance patterns (e.g., autosomal dominant, recessive, or X-linked traits).
Details on Micropipettes
How to Choose the Right Pipette
Determine the Volume You Need: Select a micropipette that covers the range of your desired volume. For example:
Use a P10 for volumes between 0.5–10 µL.
Use a P20 for volumes between 2–20 µL.
Use a P200 for volumes between 20–200 µL.
Use a P1000 for volumes between 100–1000 µL.
Ensure Precision: Using a pipette close to the middle or upper limit of its range ensures better accuracy than working at its extreme minimum.
Pipette Sizes and Names
P10: Measures 0.5–10 µL. Commonly used for DNA or RNA samples.
P20: Measures 2–20 µL. Ideal for small reagent volumes.
P200: Measures 20–200 µL. Common for general lab solutions.
P1000: Measures 100–1000 µL. Used for larger liquid volumes.
Steps for Using a Micropipette
Set the Desired Volume:
Rotate the dial to adjust the volume displayed in the pipette’s window. Ensure the volume is within the pipette’s range.
Attach the Correct Tip:
Select a tip that fits securely onto the pipette and prevents leakage.
Use small tips (yellow or clear) for P10/P20/P200 and larger tips (blue) for P1000.
Draw Up the Liquid:
Press the plunger to the first stop and insert the tip into the liquid.
Slowly release the plunger to draw the liquid up into the tip.
Dispense the Liquid:
Place the tip into the receiving container and press the plunger to the second stop to fully expel the liquid.
Eject the Tip:
Press the ejector button to discard the tip into a waste container.
Best Practices:
Hold the pipette vertically when drawing liquid to ensure precision.
Avoid blowing air bubbles or over-pipetting.
Always change tips between samples to prevent cross-contamination.
Details on Gel Electrophoresis
What Is It and What Does It Do?
Gel electrophoresis is a laboratory technique used to separate DNA, RNA, or proteins based on their size. It allows visualization of genetic material to analyze the presence, size, or quantity of specific fragments.
How Do You Properly Load a Well?
Prepare the Gel:
Use agarose gel with a buffer (e.g., TAE or TBE) to provide an electrically conductive medium.
Mix Your Sample:
Add a loading dye to your sample to increase its density and make it visible in the gel.
Load the Wells:
Insert the micropipette tip into the well without puncturing it.
Slowly dispense the sample, keeping the liquid steady to avoid overflow or air bubbles.
Run the Gel:
Place the gel in the electrophoresis chamber, ensuring the DNA moves toward the positive electrode (red).
How Does It Work?
DNA is negatively charged due to its phosphate backbone. When an electric current is applied, DNA migrates toward the positive electrode.
Smaller fragments move faster and farther through the gel, while larger fragments move slower, creating bands.
What Do the Bands Represent?
Position: The distance traveled reflects the fragment size; smaller fragments move farther.
Intensity: Brighter bands indicate a higher concentration of DNA.
Applications of Gel Electrophoresis:
Identifying genetic markers.
Analyzing PCR products for specific gene amplification.
Detecting mutations or verifying DNA extraction success.
What is gene therapy?
Gene Therapy seeks to modify one or more genes to alleviate the symptoms caused by a genetic disorder. However, the approach varies.
INSERT: A functional gene is given to a patient, providing their body with the means to make a functional protein. The defective gene is still present but its effects are masked by the functional gene.
DISABLE: A dysfunctional gene is disabled, eliminating the impact of the protein.
REPAIR: A dysfunctional gene is repaired so that it is able to produce a functional protein.
What is CRISPR?
CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats) is a revolutionary genome-editing technology that allows scientists to precisely modify DNA within an organism. It is derived from a natural defense mechanism found in bacteria, where it is used to identify and destroy invading viral DNA
Repeats in CRISPR
Short segments of DNA that are palindromes(read the same left to right)
Has Spacers between each strand of DNA(matches with viral DNA and is unique)
CAS genes
CAS Genes
Makes CAS Proteins
Helicases: Proteins that unwind DNA
Nucleases: Cut DNA
CRISPR Process
When Bacteriophage injects DNA…
DNA hijacks the cell and becomes embedded in the genome
Normally, the cell would kill the internal cell with the bacteria DNA
Through the Help of CRISPR…
CAS transcribes and translates proteins
Transcribes proteins(with the help of spacers) to make CRSIPR RNA(crRNA)
This combination of crRNA+CAS protein allows for the killing of the bacteria DNA
If we don’t have a spacer which can transcribe proteins..
CAS makes a CAS 1 class protein which..
Takes DNA, breaks it down, and copies the DNA into the CRISPR system
CRISPR CAS 9 solves…
Sickle Cell
Cystic Fibrosis
Muscular Dystrophy
HIV
What is IVF?
IVF, also known as in vitro fertilization, is a set of procedures that can lead to pregnancy
Process of IVF
A patient takes fertility drugs(hormone injections) that allow them to create an excess amount of eggs. The donor then undergoes follicular aspiration to remove the eggs.
These eggs are then fertilized with sperm in a laboratory(initial fertilization takes a few hours) and will take 3-5 days overall to complete.
They are then transferred to a patient’s uterus, which will undergo preparation medication for transferring the embryos.
Doctors will transfer multiple embryos through a catheter, in hopes of having one of these embryos developing in the uterus.
Why do we use IVF?
Infertility: Inability for couples to get pregnant naturally
Blocked Fallopian Tubes
IVF finds a way to insert embryos into a mother’s uterus while avoiding fallopian tubes
Surrogacy among LGBTQ members
Prevents risk of abnormalities in offspring
What is the purpose of PGT?
Tests to ensure the embryo selected has the correct amount of chromosomes → reducing chance of failed IVF cycle or miscarriage
Types of PGT
PGT-A: preimplantation genetic testing for aneuploidy (extra/missing chromosomes)
PGT- M: preimplantation genetic testing for monogenic disorder (single-gene defect)
PGT-A(How does testing work?)
- Evaluates embryos chromosomes
- Screens for presence of any missing/extra chromosome material
- Cells removed from trophectoderm – (cells that will become placenta )
- Embryo biopsy of blastocysts
PGT-M(How does testing work?)
- Available when there is a known genetic condition in a person/family
- Targets specific gene
- Cells removed from trophectoderm
- Embryo biopsy of blastocysts
Risks/Advantages of PGT-A
Risks:
Possible misdiagnosis
Costly
Embryo damage (cells removed)
Advantages:
Improves ability to choose healthier embryos in cohort →success rate↑for single embryo transfer
Sex selection
Reduce stressful decisions
What is PGT-M
Purpose: To test embryos for specific inherited genetic diseases caused by single gene mutations (monogenic disorders).
What it detects: Diseases like: Cystic fibrosis Tay-Sachs disease Huntington’s disease Sickle cell anemia BRCA1/2 mutations (in some cases)
Who it's for: Couples who are known carriers or affected by a specific genetic disease Often requires prior genetic testing of the parents and affected family members
Cost of PGT-A and PGT-M
PGT-A;
$4,000-$10,000 ($1,500 for embryo biopsy, $150 for each embryo tested) |
PGT-M:
$7,000-$12,000 per IVF cycle |
Plasmid
Cell Specificity
Capabilities/Limitations
None
Capabilities
Can carry genes of any size
Unlikely to cause an immune response
Limitations
Doesn’t uptake a plasmid
Less levels of therapeutic protein production due to the fact that it can’t enter the cell easy
Liposome
Cell Specificity
Capabilities/Limitations
None
Capabilities
Can carry gene of any size
Unlikely to cause immune response
Limitations
Less levels of therapeutic protein production due to the fact that it can’t enter the cell easy
Does not integrate into cell genome, so the affects are temporary
Herpes Virus
Cell Specificity
Capabilities/Limitations
Nervous Cells
Capabilities
Can carry a large amount of base pairs
Carries DNA
Limitations
Will only effect cells of the nervous system
Will not retain in the host cells genome, and will be prevalent for long periods of time
Less levels of therapeutic protein production due to the fact that it can’t enter the cell easy
Adreno-associated- virus
Cell Specificity
Capabilities/Limitations
Dividing and Non-Dividing Variety
Capabilities
Carries a large amount of base pairs
Can enter a variety of cells, making it versatile
Unlikely to cause immune response
Will not retain in the host cells genome, and will be prevalent for long periods of time
Less levels of therapeutic protein production due to the fact that it can’t enter the cell easy
Limitations
Needs a helper virus to replicate
Adenovirus
Cell Specificity
Capabilities/Limitations
Dividing and Nondividing Variety
Capabilities
Carries large amount of base pairs
Is efficient at entering cells which causes high levels of therapeutic proteins
Can enter both dividing and non-dividing
Limitations
Doesn’t integrate into a cells genome
Can cause an immune response(deleting the virus)
Retrovirus
Cell Specificity
Capabilities/Limitations
RNA Dividing Cells
Capabilities
Carries large amounts of bp
Carries RNA
Integrates into host cells genomre
Limiations:
Only infects dividing cells
Integrates into host cells randomly, which can potentially cause cancer
Causes an immune response
Lentivirus
Cell Specificity
Capabilities/Limitations
Dividing and Non-Dividing Cells
Capabilities
Carries large amount of bp
Can enter both dividing and non dividing
Enters cells which allow for release of therapeutic proteins
Will integrate into host cell genome making it long lasting
Doesn’t cause immune response
Limitations
Integrates into host cells randomly, which can cause cancer
PCR Materials
DNA Polymerase
Templete DNA
Buffer
DNA Primer
DNA Nucleotides
Thermal Cycler: Amplifies target DNA into millions of copies using PCR
Denaturation
Happens at 95 Degrees Celsius
Template DNA is first separated apart into two strands after exposure to 95 degrees Celsius
This temp causes the hydrogen bonds in the strand to break
Is done in 30 seconds the first time around, 10 seconds for any other strands
Annealing
Happens at 55-60 Degrees Celsius
Primers will first target a region to be amplified
Primers will find a place on opposite ends of a split strand of DNA
Primers are 20 base pairs long
Primers will anneal(settle) to the denatured strand as the temperature reduces drastically
Hydrogen bonds start to form