Prescribing in Respiratory Medicine
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
113 Terms
What is asthma?
inflammation and narrowing of small airways
usually intermittent and reversible
causes cough, wheeze, chest tightness and SOB
can affect in children or adults
What is COPD?
chronic airflow obstruction
causes air trapping, SOB, cough, wheeze, sputum production
usually as result of smoking or environmental exposure
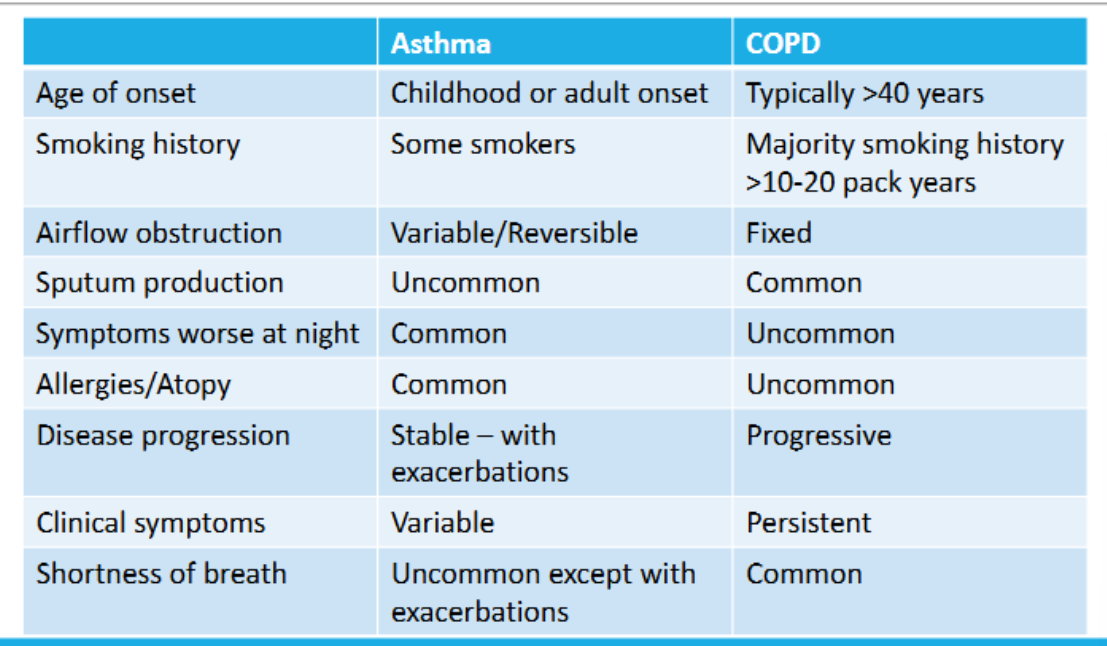
Compare asthma and COPD?
What type of white blood cell is primarily involved in asthma-related inflammation?
eosinophils
What triggers eosinophilic inflammation in asthma?
allergens such as pet dander
What type of white blood cell is primarily involved in COPD-related inflammation?
neutrophils
What triggers neutrophilic inflammation in COPD?
Inhalation of toxins, especially cigarette smoke.
What is a key feature of eosinophils in asthma?
pro-inflammatory and associated with persistent inflammation
What is a key consequence of neutrophil activation in COPD?
tissue destruction and airway inflammation
What is the most cost effective COPD intervention according to QALY?
flu vaccination
What are group A COPD patients and what is the inital treatment?
few symptoms and low risk of exacerbations
bronchodilator
What defines group E patients in COPD and what is the treatment?
≥2 moderate exacerbations or ≥1 hospitalization.
What defines group B patients in COPD and what is the treatment?
mMRC ≥ 2 or CAT ≥ 10. - low risk and more symptoms
mMRC - Modified medical research council dyspnea questionnaire
CAT - COPD assessment test
LABA + LAMA.
What should be considered before adjusting asthma medication?
Alternative diagnoses
comorbidities
inhaler technique
smoking
psychosocial and environmental factors.
What is the first-line treatment for newly diagnosed asthma in patients aged ≥12?
low-dose ICS/formoterol combination inhaler as needed (AIR therapy).
When should moderate-dose MART be considered?
If asthma remains uncontrolled on low-dose MART.
What should be checked if asthma is uncontrolled despite good adherence to moderate-dose MART?
FeNO level and blood eosinophil count.
What add-on therapies are trialed if eosinophils or FeNO are raised?
LTRA or LAMA for 8–12 weeks.
What is the next step if asthma is uncontrolled on high-dose ICS?
Refer to a specialist in asthma care.
What defines uncontrolled asthma?
Exacerbations needing oral steroids, reliever use ≥3 days/week, or night waking ≥1/week.
What is poor asthma control?
need to use reliver inhaler >3x per week
night time symptoms
chest tightness
cough
SOB
wheeze
exercise symptoms
reduced peak flow
moderate – 50-75% best/pred. PEF
severe – 33-50% best/pred. PEF
life-threatening - <33% best/pred.PEF
What is poor asthma control?
wheeze
cough
SOB
sputum changes
fatigue
grogginess or headache
What type of preventer inhaler is used in asthma?
ICS, with LABA or LAMA added if needed
What are the preventer inhaler options in COPD?
LABA or LAMA; LABA/LAMA; LABA/LAMA + ICS if indicated.
What is the reliever inhaler used in both asthma and COPD?
SABA (short-acting beta agonist).
Which condition may use a MART regimen?
asthma
Should patients with asthma or COPD have a written clinical management plan?
yes for both conditions
What physical activity intervention is recommended for COPD?
pulmonary rehabilitation
How is weight managed differently in COPD?
reduce if high
increase if low
What vaccination is recommended for both asthma and COPD?
flu vaccination
What is the prednisolone dose for asthma exacerbations?
40mg for 5 days
What is the prednisolone dose for COPD exacerbations?
30mg for 5-7 days
if first episode of exacerbation - 5 days
if patient prone to exacerbation - 7 days
When are antibiotics indicated in asthma or COPD exacerbations?
if signs of infection
What type of nebuliser is used in asthma exacerbations?
Oxygen-driven nebuliser with salbutamol 2.5 mg and ipratropium 500 mcg
What type of nebuliser is used in COPD exacerbations?
Air-driven nebuliser with salbutamol 2.5 mg and ipratropium 500 mcg.
What is the oxygen saturation target in asthma exacerbations?
>94%
What is the oxygen saturation target in COPD exacerbations?
>94%
If CO2 retention = 88-92%
Is peak flow monitoring useful in asthma exacerbations?
yes
monitor QDS and aim for PEF >75% of best before discharge.
How do SABAs work in the airway and give 2 examples?
They bind to beta-2 receptors in airway muscles, causing relaxation.
salbutamol and terbutaline
How long do LABAs typically last?
around 12 hrs
Indacaterol lasts 24hrs
Examples of LABAs?
formoterol
salmeterol
indacaterol
How do SAMAs work and give example?
work on the parasympathetic nervous system
cholinergic nerves cause airways to tighten, by blocking these nerves they cause dilation
ipratropium bromide
How long does it take for LAMAs to work and give examples?
slow release over 12-24 hrs
Tiotropium, Aclidinium bromide (Eklira), Glycopyrronium bromide (Seebri), Umeclidinum (Ellipta).
What are inhaled corticosteroid inhalers and give examples?
works by binding to common glucocorticoid receptor and suppress chronic inflammation
Beclometasone, Budesonide, Fluticasone, Mometasone, Ciclesonide
Side effects of ICS?
Oral thrush – ensure patients rinse their mouth after taking these
Dry throat/mouth
Hoarse voice
Increased risk of pneumonia in COPD
What is the recommended eosinophil threshold for ICS use in COPD?
only use ICS if eosinophils >0.3.
What is the minimum inspiratory flow needed for nebuliser aerosol to reach the lungs?
6-8L/min
What percentage of a nebulised drug dose is typically deposited in the lungs?
about 10%
Why is drug loss high with nebulisers?
Medication is retained in dead-space or lost in room air during expiration
Which is more effective: nebuliser or spacer with SABA?
Spacer with SABA is more effective than a nebuliser
What is the usual dose of salbutamol used in nebulisers?
2.5mg
Which inhaled antibiotic is sometimes used via nebuliser?
colistimethate sodium (Colomycin)
When can nebulised medication be considered appropriate?
If the patient has distressing breathlessness despite maximal inhaler therapy.
What are the benefits of nebulised therapy in select COPD patients?
Reduces symptoms, improves ADLs, increases exercise capacity, and improves lung function.
What is the primary pathological feature of community acquired pneumonia?
Infection causing consolidation of the lung parenchyma.
What types of pathogens commonly cause CAP?
bacteria and viruses
Name two typical bacterial causes of CAP.
streptococcus pneumonia and haemophilus influenzae
Name one atypical bacterial cause of CAP?
mycoplasma
Name four viral causes of CAP?
respiratory syncytial virus
adenovirus
influenza
COVID
List common symptoms of CAP?
pleuritic chest pain
cough
fever
SOB
malaise
confusion
irritability
What does CURB-65 stand for?
confusion
urea >7mmol/L
respiratory rate >30
low blood pressure
age ≥65
What CURB-65 score indicates mild pneumonia?
0–1, with >1% mortality—suitable for community management and oral antibiotics.
What CURB-65 score indicates moderate pneumonia?
Score of 2, with 1–10% mortality—consider hospital management or close follow-up in the community.
What CURB-65 score indicates severe pneumonia?
≥3, with ≥10% mortality—requires hospital management.
What imaging is used to confirm pneumonia diagnosis?
chest X-ray showing consolidation, ideally within 4 hours of admission
What blood tests support pneumonia diagnosis?
Inflammatory markers and possibly blood cultures
When is a CT scan indicated in pneumonia?
If there’s a poor response to treatment.
What additional test helps identify viral causes of pneumonia?
Viral swabs
What antibiotics are commonly used to treat CAP and how many days is the treatment?
Amoxicillin
Doxycycline
Clarithromycin.
5 days of treatment
Which antibiotics are used for severe CAP or CURB ≥ 3?
Co-amoxiclav
Tazocin
Meropenem.
What is the gaol after initial IV antibiotic therapy and when should effectiveness be reviewed?
switch to oral antibiotics
effectiveness reviewed after 48hrs
Name four supportive treatments for CAP.
Oxygen therapy, fluids, paracetamol, analgesia.
What is bronchiectasis?
condition where the airways in your lungs are damaged and produce a lot of phlegm (mucus)
What structural change defines bronchiectasis?
permanent dialtion and thickening of smaller airway
What tissue components are damaged in bronchiectasis?
Elastin, muscle, and cartilage.
What cellular changes occur in bronchiectasis?
infiltrates in cell walls and enlarged lymph nodes
What is the “vicious cycle hypothesis” in bronchiectasis?
Infection → inflammation → damage → progressive lung disease → repeat
What are the key features seen in a bronchiectatic airway?
Loss of cilia, increased mucus, destruction of airway wall.
What are the types of bronchiectasis airway?
cylindrical
cystic/saccular
varicose
traction
What is the appearance of cylindrical bronchiectasis?
Tram-track’ appearance with straight and regular outlines.

How does cystic/saccular bronchiectasis appear?
Ballooned airways with honeycomb pattern and air-fluid levels

What characterizes varicose bronchiectasis?
dilated segments with areas of constriction.
What causes traction bronchiectasis?
Fibrosis or scarring of the lung parenchyma.
What is the clinical presentation of bronchiectasis?
chronic cough
sputum production
frequent chest infections
colonisation
minor haemoptysis
breathlessness
crackles on auscultation
What are the exacerbation features of bronchiectasis?
Increased SOB
Increase in sputum
Increase in cough
Changes in sputum – colour, consistency
Fatigue and/or fever >38o C
Name two mucolytics used in bronchiectasis?
Carbocisteine and NACSYS.
When is azithromycin used in bronchiectasis?
for patients with ≥3 exacerbations per year, initiated by a respiratory specialist.
Name three inhaled therapies used in bronchiectasis?
β₂ agonists (SABA, LABA), LAMA, colomycin
What is the role of hypertonic saline in bronchiectasis?
to improve mucus clearance, under specialist supervision.
How often should respiratory physiotherapy be performed in stable bronchiectasis?
Twice daily.
What are the benefits of regular respiratory physiotherapy?
Improves sputum expectoration, cough-related health, quality of life, and exercise capacity.
When should prednisolone doses be weaned and what is the regimen?
if 2 or more short courses are used within 12 months.
reduce by 5mg every 3 days
What are the benefits of prednisolone?
reduced inflammation by:
supressess movement of leukocytes
reduce capillary permeability
reduce immune system response
Side effects of prednisolone?
adrenal suppression
cushing syndrome
increase appetite/weight gain
impaired diabetic control
increased risk of infection
osteoporosis
sleep disorders
What is the function of mucolytics?
break down of chemical structure of mucus to aid clearance
What is the daily dose, CI and side effect of carbocisteine?
2.25 g daily in divided doses (3 × 750 mg); reduce to 1.5 g after 6 months if tolerated.
CI - active peptic ulcer
Side effect - GI upset
What is the dose, form, side effects of NACSYS and what precaution is needed?
600mg OD as an effervescent tablet
use in caution in asthma
side effects - GI upset and headaches
When should NACSYS therapy be initiated?
secondary care
What drug class is montelukast?
leukotriene receptor antagonist
blocks leukotriene receptors to inhibit bronchoconstriction
What is the adult dose of montelukast?
10mg once daily in evening