StemUp: OCR A A level Biology 3.1.2 Transport in animals
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
Why do multicellular organisms need a circulatory system? (2)
- Multicellular organisms have a low surface area to volume ratio, high metabolic rate, and are often very active
- They need a constant, rapid supply of oxygen and glucose, which is provided by the circulatory system using blood
What are the two different types of circulatory systems? (2)
- Open circulatory system (e.g., insects)
- Closed circulatory system (e.g., fish and mammals)
Describe open circulatory systems (5)
- Blood flows freely through the body cavity
- The heart pumps blood into a main artery
- Which opens into the body cavity
- Where it flows around organs and re-enters the heart through valves
- Does not transport oxygen (tracheal system does this)
Describe closed circulatory systems (3)
- Blood is always confined to blood vessels
- Heart pumps blood into arteries, which branch into capillaries
- Oxygen and nutrients diffuse into cells, and veins return blood to the heart
What is the difference between a single and a double circulatory system? (2)
- Single circulatory system (e.g. fish) = Blood passes through the heart once per circuit
- Double circulatory system (e.g. mammals) = Blood passes through the heart twice per circuit (pulmonary and systemic systems)
What is the advantage of double circulatory systems? (2)
- Heart gives the blood an extra push between the lungs and the rest of the body
- Making O2 delivery faster
Describe the function and structure of arteries (4)
- Arteries carry blood away from the heart under high pressure
- Most carry oxygenated blood (except pulmonary arteries)
- Thick-walled with elastic tissue for stretch and recoil, and smooth muscle to vary blood flow
- Lined with smooth endothelium to reduce friction
What are arterioles? (2)
- Arterioles branch from arteries and transport blood into capillaries
- They have thinner walls, less elastic tissue, and smooth muscle to control blood flow to tissues
What are capillaries and what is their role? (2)
- Capillaries are the smallest blood vessels, with permeable walls that are one cell thick
- They are the site of metabolic exchange between blood and cells
What are venules? (2)
- Blood vessels that connect capillaries to veins
- They have thin walls containing muscle cells
What are veins? (4)
- Carry blood back to the heart under low pressure
- Most carry deoxygenated blood (except pulmonary veins)
- They have a wide lumen, thin walls, and valves to prevent backflow
- Blood flow is aided by surrounding muscle contraction
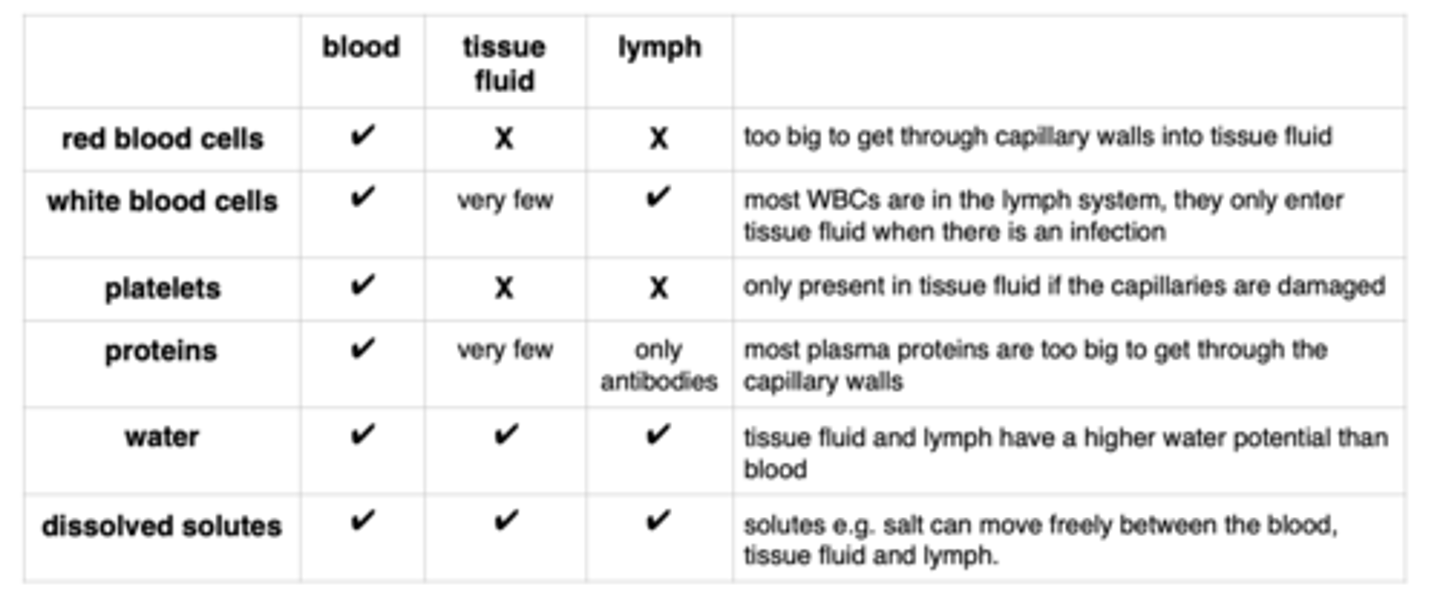
What is tissue fluid? (2)
- Surrounds cells and allows the exchange of oxygen, nutrients, and waste
- It does not contain red blood cells or large proteins
How is tissue fluid formed and partially reabsorbed? (6)
1. Hydrostatic pressure forces fluid out of capillaries
2. The fluid forms tissue fluid around the cells
3. Hydrostatic pressure decreases as fluid leaves
4. Oncotic pressure, due to plasma proteins, lowers water potential in the capillaries
5. Water re-enters capillaries via osmosis at the venule end
6. Excess tissue fluid returns to the blood via the lymphatic system
How does the lymphatic system return excess tissue fluid to the blood? (2)
1. Excess tissue fluid enters lymph capillaries, where it becomes lymph
2. Lymph moves through lymph vessels, aided by valves, and is eventually returned to the blood through vessels in the thorax
Draw a label that shows the differences in the composition of blood, tissue fluid and lymph (6)
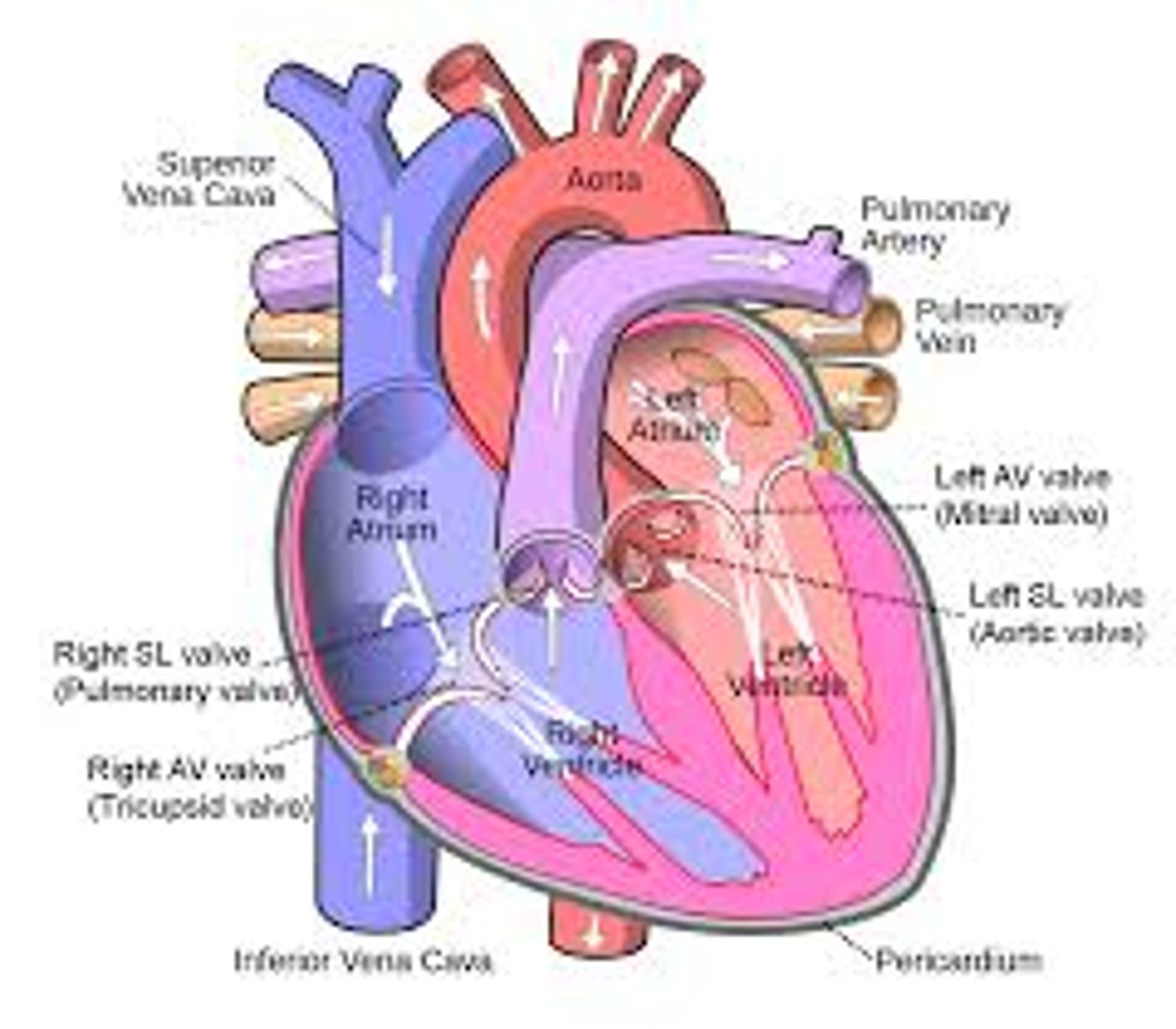
Draw and label a diagram of the internal structure of the heart (13)
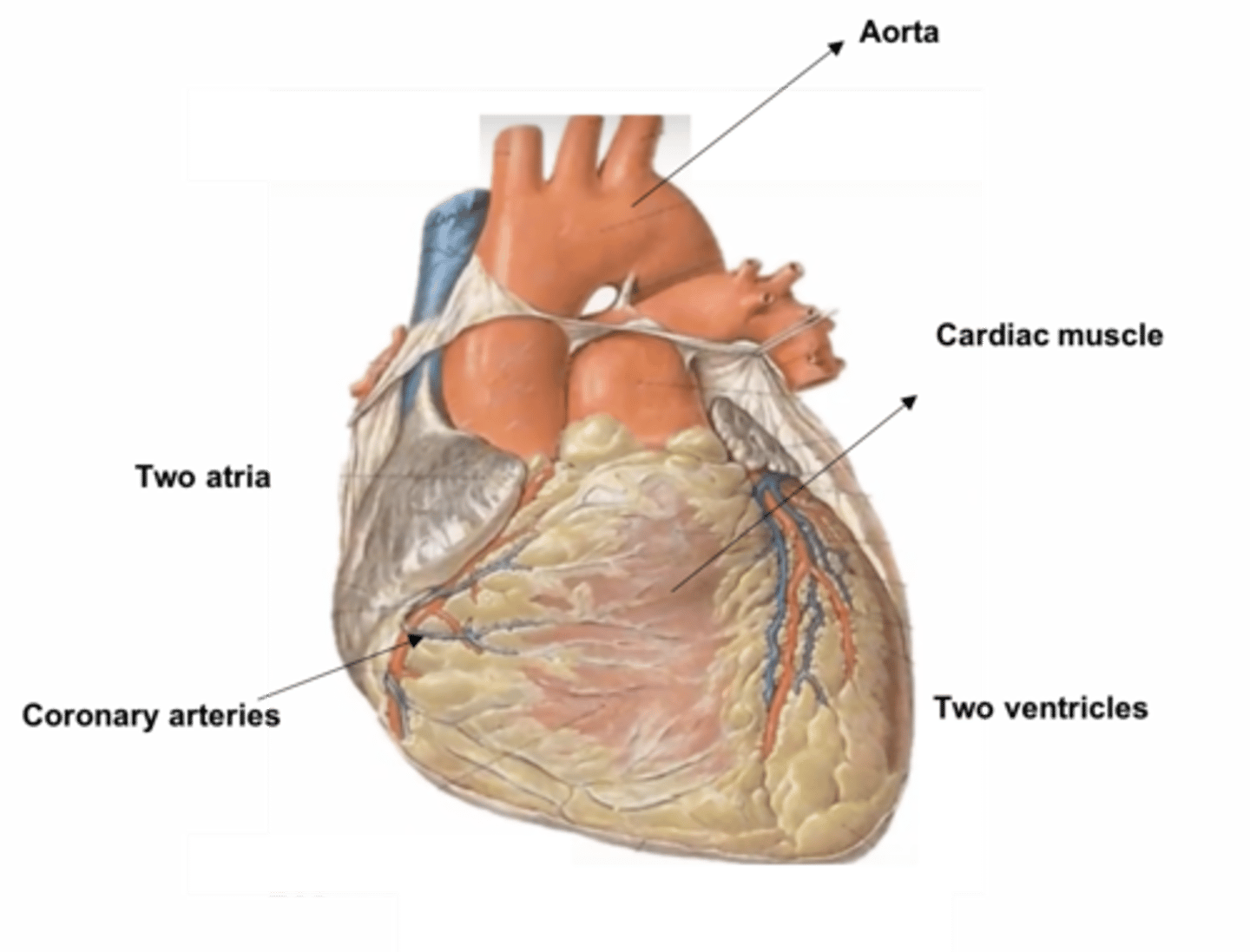
Draw and label a diagram of the external structure of the heart (5)
What are the functions of the right and left sides of the heart? (3)
- Right side = Pumps deoxygenated blood to the lungs
- Left side = Pumps oxygenated blood around the body
- The left ventricle has thicker muscle to generate enough pressure for systemic circulation
How do AV and SL valves prevent backflow of blood? (3)
- Valves open one way, and the relative pressure in the heart chambers determines whether they open or close
- Open: When the pressure is higher behind the valve
- Closed: When the pressure is higher in front of the valve
What are the key steps in examining the external and internal structure of the mammalian heart? (2)
- External: Identify the four main blood vessels
- Internal: Measure the thickness of the ventricle and atria walls, and locate and examine the AV and SL valves
What happens during atrial systole? (2)
1. Atria contract, increasing pressure and pushing blood into the ventricles through open AV valves
2. Ventricles are relaxed, and the SL valves are closed
What happens during ventricular systole? (3)
1. Ventricles contract,
2. Increasing pressure and causing the AV valves to close ('lub' sound)
3. The pressure forces the SL valves open, and blood is pumped into the pulmonary artery and aorta
What happens during cardiac diastole? (3)
1. Atria and ventricles relax
2. SL valves close ('dub' sound) as the pressure in the pulmonary artery and aorta is higher
3. Blood flows passively into the ventricles from the atria.
How is heart action initiated and coordinated? (6)
1. The heart is myogenic, meaning it can contract without nervous signals
2. The sino-atrial node (SAN) in the right atrium initiates electrical signals
3. Causing both atria to contract
4. Electrical activity is passed to the atrioventricular node (AVN)
5. Then through the bundle of His to the Purkyne fibres
6. Causing the ventricles to contract
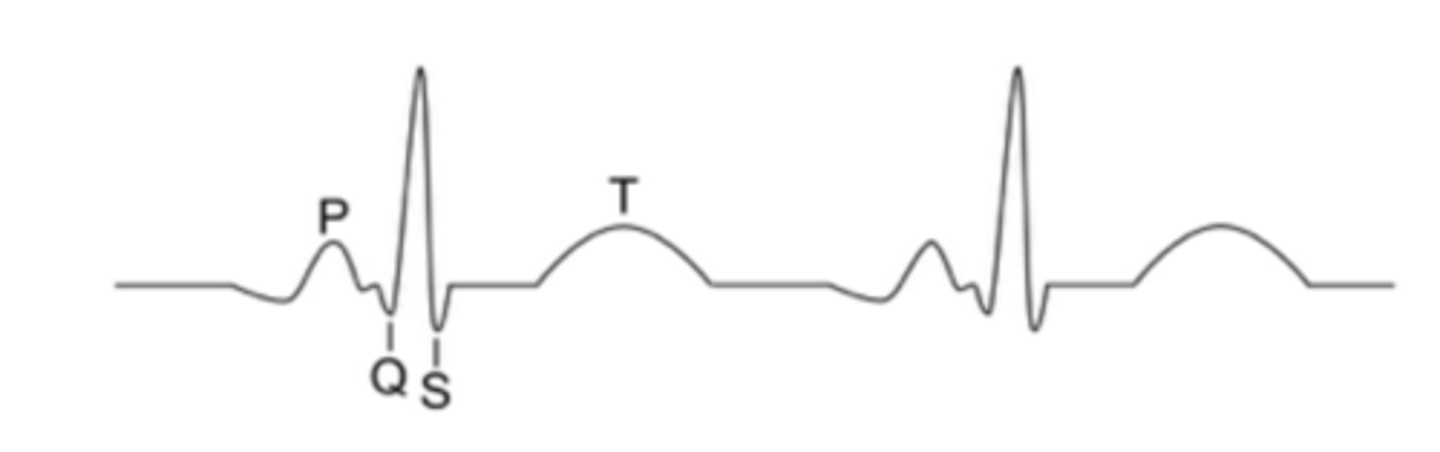
What do the P wave, QRS complex, and T wave represent on an ECG trace? (3)
- P wave: Atrial contraction (depolarisation)
- QRS complex: Ventricular contraction (depolarisation)
- T wave: Ventricular relaxation (repolarisation)
What does the height of the waves on an ECG represent? (2)
- The height corresponds to the amount of electrical activity in the heart
- The bigger the wave, the stronger the contraction
What are some common heart rate abnormalities seen on an ECG? (4)
- Tachycardia: Heartbeat is too fast (at rest)
- Bradycardia: Heartbeat is too slow
- Ectopic heartbeat: An extra heartbeat
- Fibrillation: Irregular heartbeat, with the atria and ventricles losing their rhythm
Draw a diagram of an example ECG trace (5)
What is the structure of haemoglobin? (3)
- Haemoglobin is a water-soluble, globular protein
- It consists of two alpha and two beta polypeptide chains, each with a haem group containing Fe²⁺
- Each haemoglobin molecule can bind up to 4 oxygen molecules
How does oxygen bind to haemoglobin? (2)
- In the lungs, oxygen binds to the iron in haemoglobin to form oxyhaemoglobin
- This is a reversible reaction: Hb + O₂ ⇌ HbO₈
How does partial pressure affect haemoglobin's affinity for oxygen? (2)
- As partial pressure of oxygen (ppO₂) increases, haemoglobin's affinity for oxygen increases, and it binds more oxygen tightly
- As ppO₂ decreases, haemoglobin's affinity for oxygen decreases, and it releases oxygen
Where does oxygen loading and unloading occur in the body? (2)
- Loading: In the lungs, where partial pressure of oxygen is high, oxygen binds to haemoglobin
- Unloading: In respiring tissues, where ppO₂ is low, oxygen is released
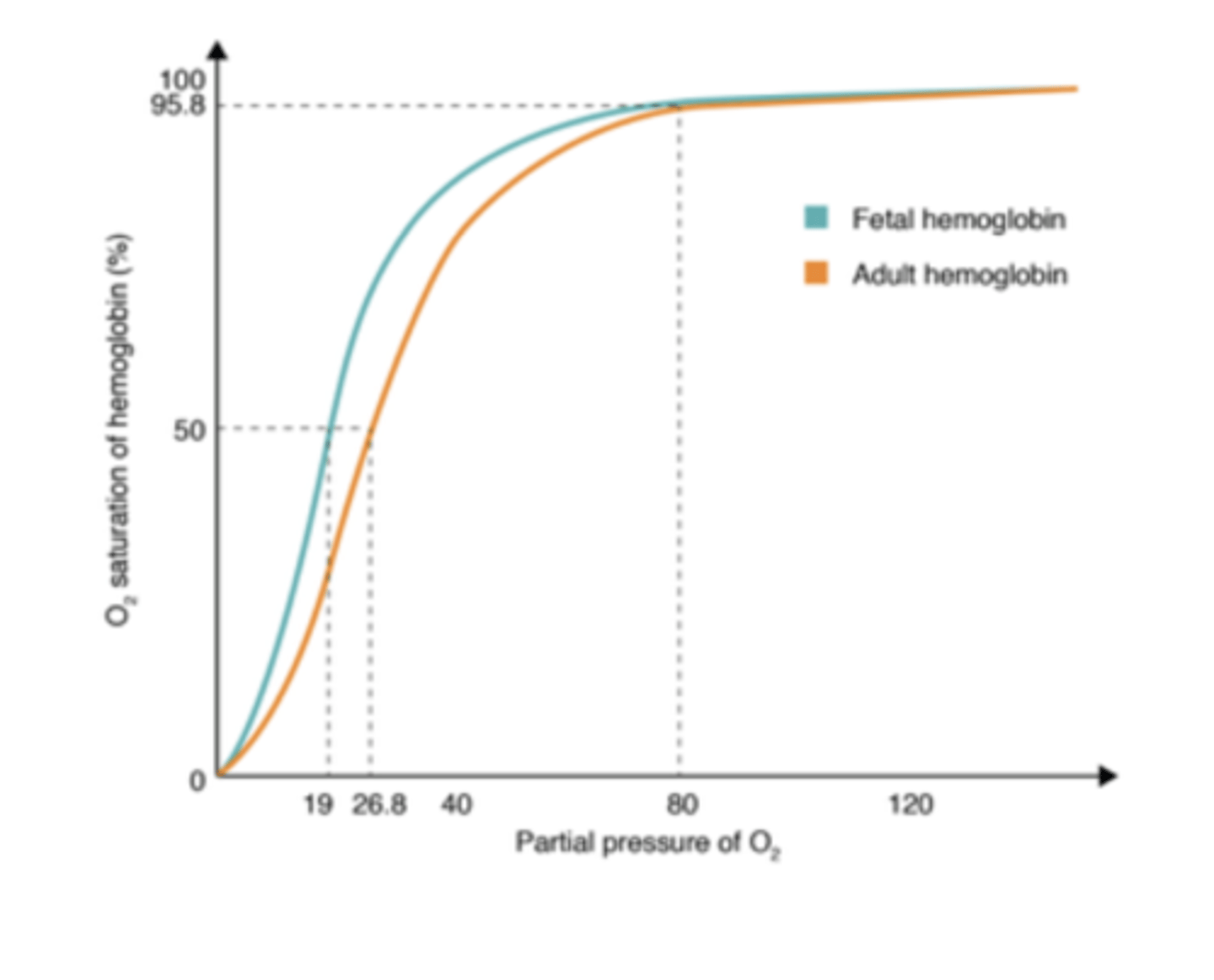
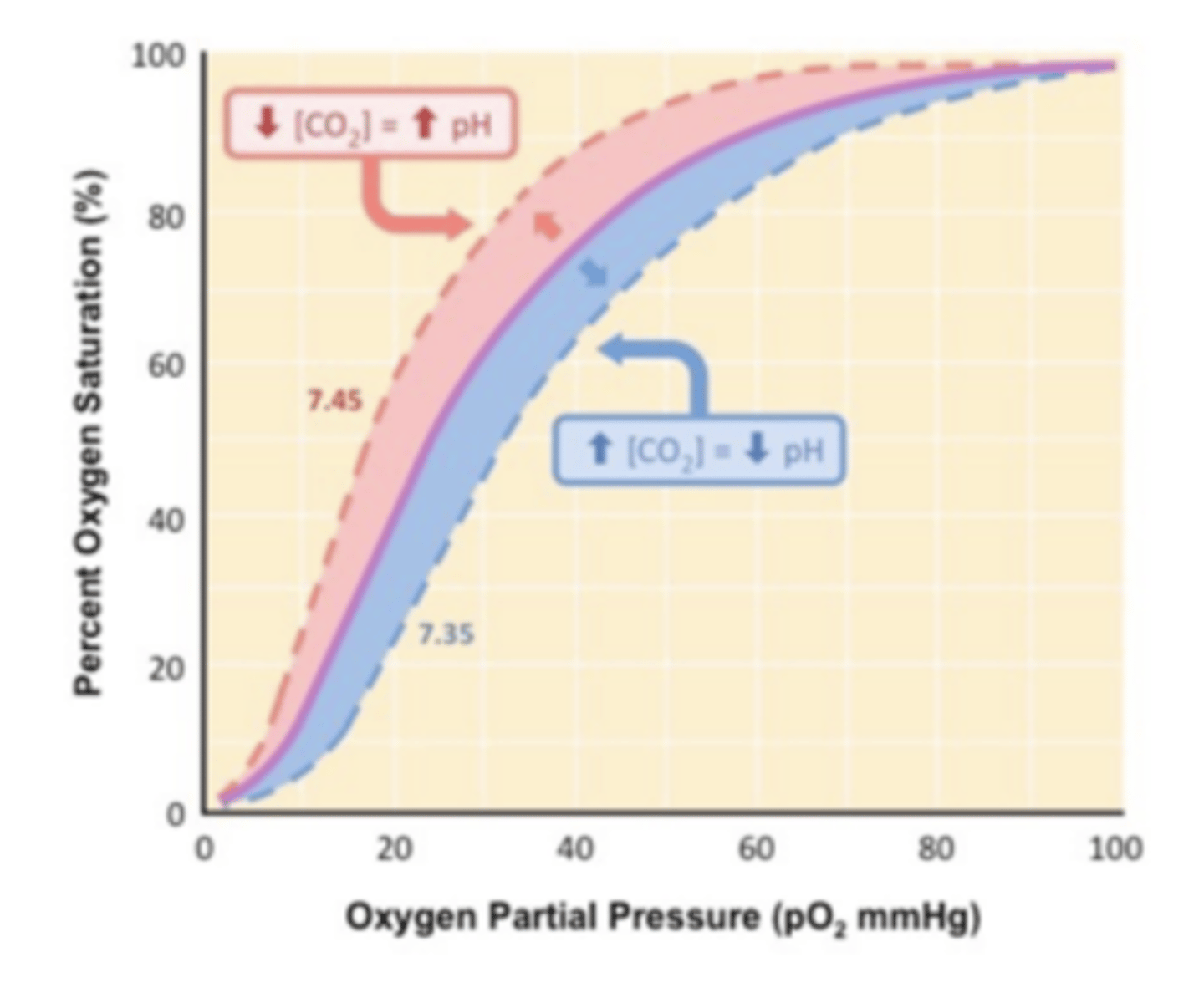
What does the haemoglobin dissociation curve show? (3)
- It shows how haemoglobin saturation changes with partial pressure of oxygen
- At high ppO₂, haemoglobin is highly saturated, and at low ppO₂, it is less saturated
- The curve is S-shaped due to the ease of oxygen binding after the first molecule binds
What is the Bohr effect? (2)
1. When CO₂ levels increase (and pH decreases), the dissociation curve shifts to the right
2. More oxygen is released because haemoglobin has a lower saturation and releases oxygen more readily in respiring tissues
How is carbon dioxide transported in the blood? (2)
1. Most CO₂ diffuses into red blood cells and reacts with water to form carbonic acid, catalysed by carbonic anhydrase
2. Some CO₂ binds directly to haemoglobin and is carried to the lungs
What happens to carbonic acid in red blood cells? (3)
1. Carbonic acid dissociates into hydrogen ions (H⁺) and hydrogencarbonate ions (HCO₃⁻)
2. The H⁺ ions cause oxyhaemoglobin to unload oxygen, and haemoglobin takes up H⁺ ions
3. To form haemoglobinic acid, preventing pH changes
What is the chloride shift? (2)
- To maintain the charge balance when HCO₃⁻ ions leave the red blood cells
- Cl⁻ ions diffuse into the red blood cells
What happens to carbon dioxide when blood reaches the lungs? (2)
- In the lungs, H⁺ and HCO₃⁻ ions recombine to form CO₂ and water
- The CO₂ diffuses into the alveoli and is exhaled
Draw and label a oxygen saturation curve for the Bohr Effect (4)
How is the oxygen dissociation curve for fetal haemoglobin different from adult haemoglobin? (2)
Shifted to the left
How does the fetus receive oxygen from the mother's blood? (1)
Across the placenta
Why does fetal haemoglobin need a higher affinity for oxygen? (4)
- By the time the mother's blood reaches the placenta
- Its oxygen saturation has decreased because her cells have used some oxygen
- Fetal haemoglobin must have a higher affinity for oxygen
- To absorb enough oxygen at the lower partial pressures, ensuring the fetus survives
What would happen if fetal haemoglobin had the same affinity for oxygen as adult haemoglobin? (2)
- The fetus's blood wouldn't be saturated enough with oxygen
- The fetus might not survive
Draw and label a oxygen saturation curve for fetal vs adult haemglobin (2)