3.1 blood borne pathogens
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
What are the three blood borne viruses?
HIV (human immunodeficiency virus)
HBV (hep b virus)
HCV (hep c virus)
How many people have died of global HIV as of 2023?
~42.3 million people but 6 have been cured (stem-cell transplantation)
A +RNA, enveloped, retrovirus (viral retrotranscriptase RNA → DNA ) that infects CD4+; also macrophages, dendritic cells
HIV
What are the important HIV proteins?
Gp160 (Env)
Proteases
Reverse transcriptase (RT)
Integrate
These are all antiviral targets!
This envelope protein of virus binds CD4 receptor and CXCR4 and CCR5 co-receptors of the host cell to fuse the viral envelope w the cell membrane
Mechanism of gp160 (Env)
Mechanism of protease
Cleaves viral poly proteins into functional proteins
Generates DNA from viral RNA template
Reverse transcriptase (RT)
Integrates viral DNA into the the host genome
Integrate
Transmitted in blood, genital secretions, breast milk
Needle stick accidents, open wound or mucous membranes
HIV encounter
Enters body through blood or mucosa
Infects dendritic cells, then CD4+ lymphocytes
Progeny virus is shed into the bloodstream (viremia)
Spread to brain, spleen, GI
HIV entry and spread
Acute a stage includes “mononucleosis-like” symptoms that can last 1-4 weeks, incubation is 2-6 weeks
HIV
4th generation immunoassays: combine (blank) antigen and (blank) antibodies
Earliest positive 15-20 days
Test for viral RNA if symptomatic and <15 days of exposure
First to peak after infection is viral RNA → p24 antigen → antibody
HIV testing
What is the HIV window?
Time between getting HIV and when it will show on tests:
Nucleic acid test: 10-33 days
Antigen/antibody lab test: 18-45
Rapid antigen/antibody test: 18-90 days
Antibody test: 23-90 days
This latency stage is:
Asymptomatic
Viral load is at a low level
Continuous viral repli leads to CD4 destruction
HIV: low levels of HIV RNA and declining CD4 counts
CD4 cell count <200 so cell mediated immunity is lost
Weight loss, wasting
Opportunistic infections: bacteria, viruses, fungi, Protozoa (those usually non-pathogenic become pathogenic
Tumors
Neurological diseases
AIDS: high levels of RNA low CD4
HAART/ART
Highly active anti-retroviral therapy: cocktail of inhibitors that target different stages in repli (see HIV proteins: 4)
“Chronic manageable disease”: CD4 levels recover and viral plasma RNA undetectable but still lifetime of drugs
Occupational exposures:
Per cutaneous injury (needle stick)
Mucous membranes or non-intact skin
Non-infectious unless visible blood: “external” body fluid
More blood = more risk of infection
PEP vs PrEP
PEP: post exposure prophylaxis (preventative)
ART regimen, short-term that decreases likelihood of HIV infection from exposure
Start asap w/in 72 hours of exposure for 28 days, rested 4-6wks, 12, 24; secondary transmission to others rare but modify behavior first 6-12 weeks after exposure
PrEP: Pre Exposure Prophylaxis
liver disease mostly cased by viruses but could also be caused by toxins in alcohol or mushrooms
hepatitis
three hepatitis viruses that result in acute or chronic disease and transmission is blood and bodily fluids:
Hep B: chronic is 5%
Hep C: chronic is 80%
Hep D, needs Hep B to be viral and repli
which hep virus is transmitted by fecal/oral route and causes acute disease?
Hep A and E
efficient vaccine is available for this hepatitis virus
major blood-borne pathogen
liver disease and cancer
around for a long time and ~257 million people worldwide aer chronically infected
HBV
HBV encounter, entry, and spread
blood or genital; needle sticks also sharing razors or toothbrushes, vertical
spreads to liver
long incubation: 4-26 weeks
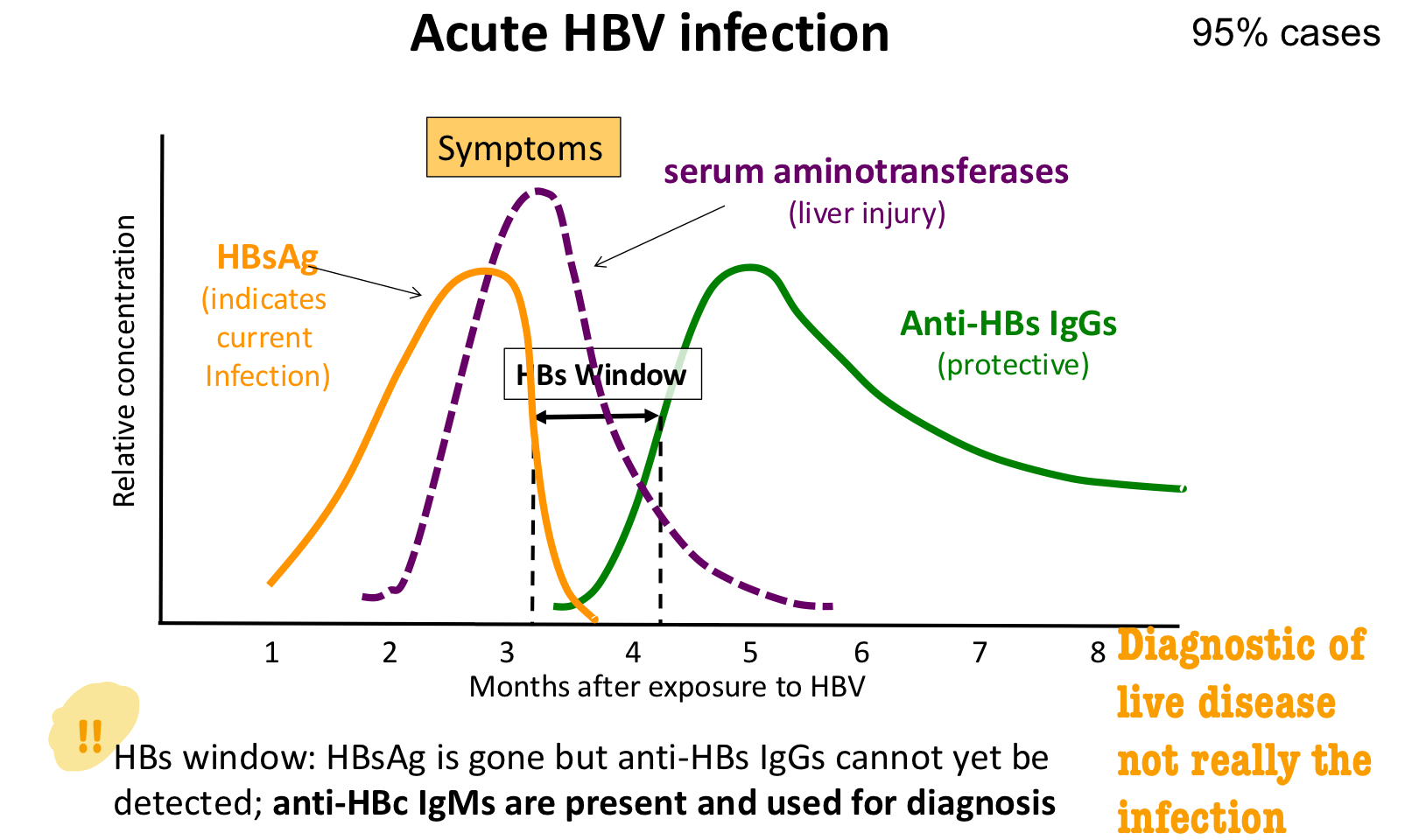
labs that show
increased levels of aminotransferases
absence of Abs to HAV, HBV. HCV
HBsAg detected
acute HBV infection
what is HBsAg?
hep B surface antigens
binds host receptors
key serological marker of HBV infection
elicits protective Abs
subunit vax
increased levels of aminotransferases marker of
liver injury
HBsAg marker of
active infection
anti-HBs antibodies marker of
immunity
how many HBV diseases end in acute, asymptomatic infection?
~2/3
how many of the acute infections recover? turn into chronic infection? fulminant hepatitis?
95% (low chance of reinfection
5% (cirrhosis and hepatocellular carcinoma)
<1% (massive hepatic necrosis and leads to cell death)
which hep virus is oncogenic?
HBV (cancer causing)
T or F: HBV is an enveloped, ds or ssDNA virus
true! with HBsAg and HBcAg
what is HBcAg?
hep B core antigen
forms viral capsid
elicits Abs
what is HBs window?
when HBsAg is gone but anti-HBs IgGs (protective Abs, diagnostic of lover disease not quite HBV infection) undetectable
persistent viremia
HBsAg stay high
no anti-Hs IgGs (instead IgMs then IgGs)
liver cells constantly damaged and regenerated
elevated aminotransferases due to liver injury
leads to cirrhosis, hepatocellular carcinomas; great regen capacity
chronic HBV infection 5% of cases
what Ag is present with acute HBV infection?
HBsAg
what seroconversion occurs with a resolved HBV infection?
HBsAg → anti-HBs IgG
what Ag is present with chronic HBV infection?
HBsAg for >6mo
the three serological for HBV diagnosis and their types of infection
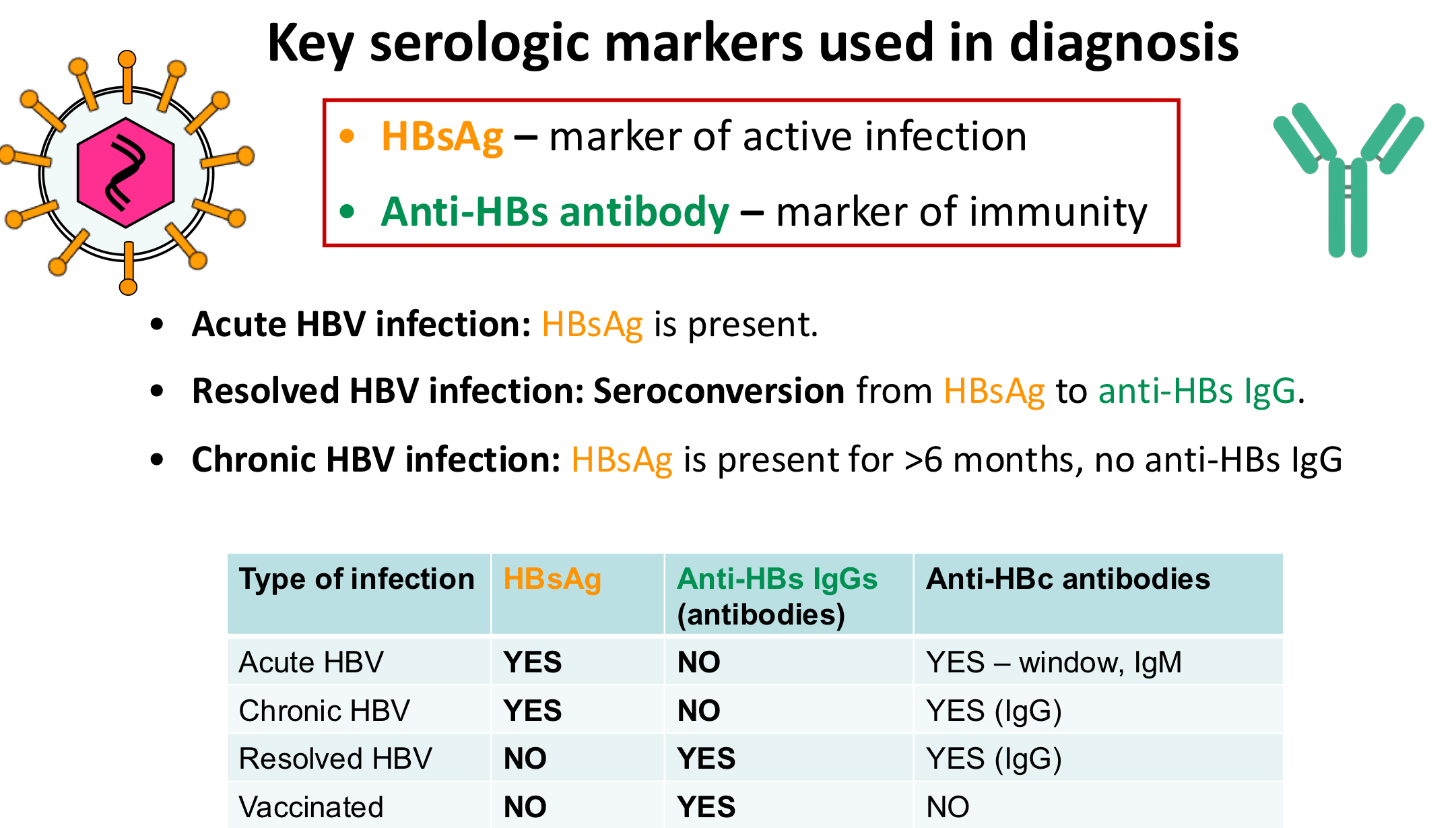
which serological marker is present for vaccination HBV?
anti-HBs IgGs
HBsAg: present
Anti-HBs IgGs: no
Anti-HBc: yes window IgM
acute HBV
HBsAg: present
Anti-HBs IgGs: no
Anti-HBc: IgG
chronic HBV
HBsAg: no
Anti-HBs IgGs: present
Anti-HBc: IgG
resolved HBV
HBsAg: no
Anti-HBs IgGs: present
Anti-HBc: no
vaccination for HBV
treatment for acute vs chronic HBV?
acute: self-resolving
chronic: no cure but use antivirals like ribavirin to reduce viral load or PEGylated interferon (stabilized interferon)
HBV prevention: active vs passive immunization
active: subunit vax is recombinant HBsAg for infants and healthcare workers
passive: anti-HBV IgGs (HBIG) infants of chronic HBV carriers and take w subunit vax
when to take HBV PEP?
exposure to HBV-infected blood, vaccine w/in 12 hours of exposure plus HBIG
*but if you have been vax and have documented anti-HBs IgG, you do not need PEP
enveloped, +RNA virus in family of hepacivirus, discovered 1989 (recently). in the US is the leading cause of liver transplant
HCV
HCV encounter, entry, spread
transmitted blood (some risk w razors and toothbrushes and low risk with sex)
spreads to liver, multiplies then to blood
long incubation: 4-26 weeks
of the ~2/3 acute asymptomatic HCV infections how many recover? how many become chronic?
20%
80%; cirrhosis 20-30% → hepatocellular carcinoma
high prevalence bc HCA is an error prone RNA virus that mutates easy with RdRp low fidelity frequent mistakes with no correction = vast genetic diversity
HCV RNA (genome): yes
aminotransferase levels: high
anti-HCV Ab: no early yes later
acute HCV
HCV RNA (genome): yes
aminotransferase levels: variable
anti-HCV Ab: yes
chronic HCV
HCV RNA (genome): no
aminotransferase levels: normal
anti-HCV Ab: yes
resolved HCV
T or F: positive anti-HCV Ab test distinguishes resolved vs chronic infections
FALSE! need to test for HCV RNA
T or F: to distinguish from acute vs chronic infection you check for HCV RNA then check again in 3mo
true :)
how to treat chronic HCV?
antivirals, pegylated interferon (prolong immune response)
outcome of HCV treatment:
SVR (sustained virologic response): no HCV RNA 6mo after end of treatment (45-90% ppts cured?)
no vaccine or PEP
vaccine: yes
PEP: yes
antiviral: yes
survival on fomite: 1-3 weeks
risk of infection after needle stick: 7-30% (viral load)
HBV
vaccine: no
PEP: no
antiviral: yes
survival on fomite: up to 4 days
risk of infection after needle stick: 2%
HCV
vaccine: no
PEP: yes
antiviral: yes
survival on fomite: few hours
risk of infection after needle stick: 0.3%
risk w bloody dental procedures
HBV: prevent w PPE, safe injection practices, HBV vax
risk w needle stick
HCV HIV