Blood bank and Blood Transfusion Medicine (Book questions)
1/852
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
853 Terms
1. Which immunodominant sugar confers A antigen
specificity?
a. D-Galactose
b. L-Fucose
c. N-Acetylgalactosamine
d. Both A and C
c. N-Acetylgalactosamine
(GalNAc) confers type
A specificity. D-Galactose (Gal) confers type
B specificity. L-Fucose (Fuc) confers typeOspecificity.
The type A and type B sugars are built on Fuc.
If a patient has an A2 ABO type, which of the following
statements is true?
a. The patient's red cells will react with anti-A1 lectin
b. The patient's serum will react with A2 cells
c. The patient's red cells will react with anti-A2 lectin
d. The patient's serum will react with A1 cells if
anti-A1 is present
d. the patients serum will react with A1 cells if anti-A1 is present
The A2 subgroup is described as having both qualitative
and quantitative differences when compared
to the A1 subgroup. This means that there
is less A antigen found on the red cells of people
with A2, and their A antigen looks "different"
when compared to that of people with type A1.
Therefore the red cells from those with type A2
will not react with anti-A1 lectin. Approximately
20% of those with type A have the A2 phenotype,
and between 1% and 8% of those individuals
make anti-A1. There is no anti-A2 reagent, and
people with the A2 phenotype would not react
with A2 cells, because that would imply an autoantibody
is present.
Which genotype confers the Bombay blood type?
a. Hh
b. hh
c. Sese
d. Lele
b. hh
People with the Bombay phenotype do not
express the H antigen. An individual with the
hh genotype would not express H antigen.
Which genes encode for Rh antigens?
a. RHDCE
b. RHD
c. RHCE
d. Both b and c
d. both b and c
The RHD gene encodes for the D antigen.
The RHCE gene determines C, c, E, and e specificities.
Therefore the correct answer must include
both genes.
Testing for the D antigen was conducted at the IAT
phase. A control was included in the testing. Both
the patient's red cells and the control tube reacted
at 4+. How would you interpret this test?
a. The test is invalid because the control tube was
positive
b. The patient is D positive
c. The patient is D negative
d. The test should be repeated and the control tube
omitted
a. The test is invalid because the control tube was positive
In indirect antiglobulin test (IAT) phase, a control
tube is included to show that agglutination
detected in the patient test tube is appropriate.
In weak D testing, the control tube uses saline
rather than anti-human globulin (AHG) reagent.
Agglutination in the control tube suggests that
the patient cells are already sensitized with immunoglobulin,
so a positive reaction in the patient
test tube should be invalidated and investigated.
Of the red cells listed, which has the most D antigen
present?
a. Rh null
b. D positive
c. dce/dce
d. D--
d. D—
Individuals with the D phenotype may possess
more D antigen because they have inherited a nonfunctioning
RHCE gene. Basically, the RHD gene
ofDindividualshasnocompetitionwhenbuilding
D antigen, so they end up with more. Rh-null
individuals do not express any Rh antigens. Dpositive
individuals possess theDantigen, butwithout
knowing the genotype, theamount ofDantigen
cannot be estimated. A person with the dce/dce
genotype would be considered Rh-negative.
Which is true of the Duffy blood group system?
a. Antigens are resistant to enzyme treatment
b. Antibodies never show dosage
c. Fya and Fyb are codominant alleles
d. The majority of whites are Fy(a-b-)
c. Fya and Fyb are codominant alleles
The Duffy blood group system contains two
codominant alleles, Fya and Fyb, as well as Fy3,
Fy5, and Fy6. The Fya, Fyb , and Fy6 antigens
are sensitive to ficin, and antibodies made against
the Duffy antigens can show dosage. Approximately
68% of the black population is Fy(ab).
Which antibody is typically considered to be an autoantibody
if found in the serum of an adult?
a. Anti-K
b. Anti-I
c. Anti-D
d. Anti-Fya
b. Anti-I
The I antigen is a precursor to the H antigen, so
individuals who express the H antigen are presumed
to have the I antigen. Therefore, if an individual
expresses anti-I, it is typically considered
to be an autoantibody. Anti-I typically presents
as a cold-reacting, clinically insignificant IgM
autoantibody.
Which reagent destroys all of the Kell blood group
system antigens?
a. DTT
b. Chloroquine diphosphate
c. AHG
d. LISS
a. DTT
Dithiothreitol (DTT) disrupts the tertiary structure
of proteins, and denatures the Kell system antigens
on red cells. Chloroquine diphosphate (CDP) can
be used to dissociate antibodies from red cells.
Anti-human globulin (AHG) reagent is used in
the indirect antiglobulin test (IAT). Low ionic
strength solution (LISS) is used as a potentiator.
Which is true of antibodies to Kidd blood group system
antigens?
a. They are enhanced by enzymes
b. Titers can quickly drop in patients
c. Both A and B
d. None of the above
c. Both A and B
The Kidd blood group system contains three antigens,
Jka, Jkb, and Jk3. Antibodies made against
this blood group system are typically IgG, are best
detected by indirect antiglobulin test (IAT), are
enhanced by treating reagent red cells with
enzymes, and can show dosage. Antibody titers
have also been found to increase and then quickly
decrease in patients.
Which of the following is true of the Lewis system?
a. Lewis antigens are found on type II precursor cells
b. Lewis antigens are well developed at birth
c. Antibodies to Lewis antigens always cause HTRs
d. Antibodies to Lewis antigens rarely cross the
placenta
d. Antibodies to Lewis antigens rarely cross the placenta
The Le gene adds fucose to either a type I precursor
chain to make the Lea antigen or adds fucose
to the H structure to make Leb. Type II chains
never express Lewis antigen activity. Newborns
express the Le(ab) phenotype. Antibodies
against the Lewis antigens are typically roomtemperature
(RT) reactive, IgM class, and not clinically
significant. Because they are typically IgM
class, they cannot cross the placenta.
Which of the following is true of antibodies to MNS
blood group system antigens?
a. Anti-U is directed at a high-incidence antigen
b. Anti-N is commonly found
c. Anti-M is always clinically significant
d. Anti-S is reactive with enzyme-treated cells
a. Anti-U is directed at a high incidence antigen
The U antigen is located near the red membrane on
glycophorin B (GYB), so is always present when S
or s is inherited. The amino acid structure on GYB
is the same as the first 26 amino acid sequence on
glycophorin A (GYA), so the only individuals who
can make anti-N are those who lack GYB. Anti-M
is typically an IgM class antibody, usually considered
to be clinically insignificant. The effect of
enzymes on the S antigen is variable.
Which of the following antibodies is classified as
"biphasic" and an autoantibody?
a. Anti-B
b. Anti-P
c. Anti-H
d. Anti-Lea
b. Anti-P
Allo-anti-P is a rare antibody made by individuals
with the P2
k phenotype, somost examples of anti-P
seen in the blood bank are actually autoanti-P.
Autoanti-P is associated with paroxysmal cold
hemoglobinuria. This antibody is an IgG antibody, also called the Donath-Landsteiner antibody. It is a
biphasic hemolysin that attaches to P-positive red
cells at lower temperatures. Complement is
attached, and when the red cells are warmed to
37 C, hemolysis occurs. The other antibodies
listed are typically RT reactive antibodies.
You have performed an antibody screen using the
tube method. All three screening cells tested negative.
The Coombs check cells in all three tubes are also
nonreactive. What should you do?
a. Respin the tubes and reread them
b. Report the antibody screen as negative
c. Repeat the antibody screen
d. Perform an antibody identification panel
c. Repeat the antibody screen
Coombs check cells are used to verify that antihuman
globulin (AHG) has been added to reagent
tubes and that it is active. When the check cells do
not agglutinate, either AHG was not added or it
was somehow inactivated. This usually occurs
because of inadequate washing. If the check cells
do not work, the entire test should be repeated.
An antibody panel has six 2+ reactive cells at AHG
phase. Panel testing using enzyme-treated cells
showed no reactivity. Which is the most likely antibody
that is present?
a. Anti-Fya
b. Anti-e
c. Anti-k
d. Anti-Lua
a. Anti-Fya
Because enzyme treatment removed the reactivity
noted in the original panel, we can infer that the
unexpected antibody is directed to an antigen that
is sensitive to enzymes. Of the antigens given in the
list, only the Fya antigen is sensitive to enzymes.
A patient has a currently nonreactive antibody screen
but has a history of anti-Jka in the patient file. Which
type of crossmatch must be performed on this patient?
a. Immediate spin crossmatch
b. IAT crossmatch
c. Electronic crossmatch
d. Both a and c
b. IAT crossmatch
Whenever an unexpected antibody is currently
reactive or noted in a patient's history file, an indirect
antiglobulin test (IAT) crossmatch must be
performed. An immediate spin or electronic crossmatch
is performed only on patients with no evidence
of clinically significant antibodies,
currently and historically.
A recently transfused patient has a 3+ reactive DAT
with anti-IgG. Which procedure should be used to
identify the specificity of the IgG antibody attached
to the red cells?
a. Adsorption
b. Neutralization
c. Titration
d. Elution
d. Elution
A positive direct antiglobulin test (DAT) implies
that the patient has an IgG antibody attached to
the red cells. An elution procedure would dissociate
the antibody from the red cells and collect it so
the specificity can be determined. An adsorption
removes red cell antibodies from plasma by
adsorbing antibody onto red cells. Neutralization
is performed to inactivate an antibody present in
plasma. A titration is performed to determine
how much antibody is present in plasma.
An O-negative mother gave birth to an O-positive
baby. Her rosette test was positive. Which of the following
is true?
a. The test is invalid because of the mother's
ABO type
b. A Kleihauer-Betke test should be performed to
quantify the fetal maternal hemorrhage
c. The mother should be given a 300-mg dose
of RhIG
d. A weak D test should be performed on the baby
b. A Kleihauer-Bette test should be performed to quantify the fetal maternal hemorrhage
A positive rosette test is a qualitative indicator that
a fetal bleed has occurred. This is important to
detect in Rh-negative mothers who have an Rhpositive
baby. To provide the correct dosage of
Rh immunoglobulin, a quantitative test must be
performed to quantify the amount of bleed that
occurred. The Kleihauer-Betke test looks for fetal
hemoglobin in a sample collected fromthe mother.
In which of the following settings are platelet transfusions
not indicated?
a. Thrombotic thrombocytopenic purpura
b. Immune thrombocytopenic purpura with severe
intracranial hemorrhage
c. Massive transfusion
d. Vascular catheter placement, platelet count
24,000/mL
e. Brain biopsy, platelet count 62,000/mL
a. Thrombotic thrombocytopenic purpura (TTP)
is characterized by thrombocytopenia, microangiopathic
hemolytic anemia, renal dysfunction, and
central nervous system involvement. Basically,
giving platelets to a patient with TTP provides
fuel that would exacerbate the condition. The
other conditions listed are all appropriate indicators
for platelet transfusion.
An obstetric patient presents to the hospital with
marked vaginal bleeding and severe lower abdominal
pain. During placement of an intravenous catheter,
she was noted to have marked oozing. She is diagnosed
with disseminated intravascular coagulation
as a complication of her primary problem. She is
given cryoprecipitate and fresh frozen plasma before
going to the operating room. What element of cryoprecipitate
is important in treating this patient?
a. Factor I
b. Factor II
c. Factor VIII:c
d. Factor VIII:vWF
e. Factor XIII
a. Factor I
In disseminated intravascular coagulation, platelets
and fibrinogen are inappropriately consumed,
and so transfusion therapy should be targeted
toward replacing those elements. Cryoprecipitate
contains in a concentrated form most of the coagulation
factors found in fresh frozen plasma.
These include von Willebrand factor, fibrinogen
(I), factor VIII, fibronectin, and factor XIII. Cryoprecipitate
is primarily used clinically for patients
with deficiencies of factor XIII and fibrinogen.
A patient's ABO blood type is determined by which
of the following?
a. Genetic inheritance and environmental factors
b. Genetic inheritance
c. Environmental factors
d. Immune function
e. Maternal blood type
b. Genetic inheritance
The best answer to this question is genetic inheritance,
which includes but is not limited to the
mother's blood type. Inheritance of the ABO antigens
are driven by the ABO, H, and Se genes.
Genetic inheritance, environmental factors, and
immune function would influence the presence
of antibodies against certain ABO antigens.
A trauma patient with type AB is seen at a rural hospital.
The hospital only has 3 units of type AB RBCs.
What blood type of RBCs can the patient receive as
an alternative?
a. Type O
b. Type B
c. Type A
d. None of the above
e. All of the above
e. All of the above
The patient can receive all of the blood types listed,
but good blood management would dictate the
order in which they were transfused. Generally,
the best course of action would be to transfuse type
A first because it is usually more plentiful than type
B. Patients with O type can receive only type O
blood, so it is best to conserve type O when possible.
If type A is not plentiful, type B can be given.
Once either type A or type B is given, types should
not be mixed, to help avoid potential reactions. If
type A or B is exhausted, it is then appropriate to
move to type O.
A genetic state in which no detectable trait exists is
called:
a. Recessive
b. Dominant
c. Incomplete dominance
d. Amorph
d. Amorph
An amorph, or silent, gene does produce a detectable
antigen product. Examples of amorph, or
null, phenotypes include Rhnull, O, and Lu
(ab).
Most blood group antigens are expressed as a result
of which of the following?
which of the following?
a. Autosomal recessive inheritance
b. X-linked dominant inheritance
c. Y-linked recessive inheritance
d. Autosomal codominant inheritance
d. Autosomal codominant inheritance
Most blood group systems genes exhibit codominant
expression, or equal expression of both
traits. In an autosomal recessive inheritance pattern,
a trait is observable only when not paired
with a dominant allele. X-linked and Y-linked
inheritance patterns are complex and not typically
seen in most blood group systems.
What blood type is not possible for the offspring of
AO and BO parents?
a. AB
b. A or B
c. O
d. All are possible
d. All are possible
This answer is best explained through the use of a
Punnett square
How many molecules of IgM are needed to fix
complement?
a. 1
b. 2
c. 3
d. 4
a. 1
IgM is classified as having a large pentamer structure.
Thus only one IgM is required to initiate the
classical pathway in the complement system. In
comparison, it takes two IgG molecules to activate
complement.
For lysis of red blood cells to occur after antigen-
antibody reaction, which compound is required?
a. Albumin
b. Glucose-6-phosphate dehydrogenase (G6PD)
c. Complement
d. Antihuman globulin (AHG)
c. Complement
In vitro, complement is detected through the use
of anti-C3b or anti-C3d reagents. When detected,
this indicates complement proteins have been
attached to the red cell surface as a result of the
activation of complement's classical pathway.
In vivo, complement activation may proceed to
intravascular hemolysis if conditions are right,
which would result in the lysis of red blood cells.
An end-point of tube testing other than agglutination
that must also be considered a positive reaction is
called:
a. Clumping
b. Mixed field
c. Hemolysis
d. Microscopic
c. Hemolysis
Hemolysis as a reaction end-point indicates the
presence of a complement-activating antibody.
This reaction is especially important to recognize
because it is an indicator of an antigen-antibody
reaction. When hemolysis occurs, the red cell button
is often smaller than buttons in other tubes
and the supernatant may appear to be pinkish
or reddish.
Mixed-field (mf) agglutination can be observed
in the:
a. DAT on a person undergoing delayed hemolytic
transfusion reaction
b. IAT result of a patient who has anti-Lea
c. DAT on a patient on high doses of penicillin
d. Typing result with anti-A of a patient who is A2
subgroup
a. DAT on a person undergoing delayed hemolytic transfusion reaction
Mixed-field (mf) agglutination indicates the presence
of two red cell populations when noted: one
that is agglutinating, and one that is not. Of the scenarios
presented, a person undergoing a delayed
hemolytic transfusion reaction is most likely to
have two cell populations in circulation—his/her
own red cells and those from the transfusion. In
a delayed transfusion reaction, an antibody has
been stimulated against the transfused cells. A positive
direct antiglobulin test (DAT) in this scenario
indicates the antibody has attached to the transfused
cells but not to the patient's own cells; therefore
mixed-field reactivity is noted.
In which situation(s) may the ABO serum grouping
not be valid?
a. The patient has hypogammaglobulinemia
b. IgM antibodies are present
c. Cold autoantibodies are present
d. All of the above
d. All of the above
Patient's with hypogammaglobulinemia have an
overall reduction of g-globulins and may not be
able to reverse grouping antibodies at levels detectable
by ABO typing tests. IgM antibodies, other
than those normally detected in reverse grouping
tests, or cold autoantibodies may interfere with
reverse grouping tests, making the results invalid.
One example of an IgM antibody that may interfere
with reverse grouping is anti-M.
If you knew the DAT is positive, what would you
expect the Rh control to be when doing a weak D test
through AHG?
a. Negative
b. Positive
c. Mixed field
d. Hemolysis at 37 C would be seen
b. Positive
Cells that are direct antiglobulin test (DAT)-
positive or already have IgG attached would give
a false-positive reaction when tested by the indirect
antiglobulin test (IAT). The IAT is used to
detect antibody bound to red cells in vitro. IAT
is a two-stage procedure. In the first stage, antibodies
are encouraged to combine with their corresponding
antigen during an incubation step. If
DAT-positive red cells (cells that have antibody
already attached) are used in an IAT test, the first
step, in effect, has already occurred. The attached
IgG molecules will be detected in the second IAT
step, the agglutination step, and give a falsepositive
reaction.
How can IgG antibodies be removed from red cells?
a. Elution
b. Adsorption
c. Prewarming
d. Neutralization
a. Elution
An elution is a process that dissociates antigen-
antibody complexes on red cells. An adsorption
is a process that uses red cells to remove red cell
antibodies from a solution. Prewarming is a technique
in which all reagents and patient samples
used in a test procedure are incubated to reach
37 C (or the preferred testing temperature)
before the test is conducted. Neutralization combines
a soluble antigen with antibody in vitro and
is used as an antibody identification technique.
Therefore the best answer is elution.
Testing needs to be done with an antiserum that is
rarely used. The appropriate steps to take in using this antiserum include following the manufacturer's
procedure and:
a. Performing a cell panel to be sure that the antiserum
is performing correctly
b. Performing the testing on screen cells
c. Testing in duplicate to ensure the repeatability of
the results
d. Testing a cell that is negative for the antigen and
one that is heterozygous for the antigen
d. Testing a cell that is negative for the antigen and one that is heterozygous for the antigen
Before a reagent is used, it should be assessed to
determine if it meets preset acceptable performance
criteria. For a red cell antiserum, an example
of acceptable performance criteria might
include reactivity with antigen-positive cells and
no reactivity with antigen-negative cells. When
testing antigen-positive cells, cells with heterozygous
inheritance are generally recommended for
use because this would detect the weakest expression
of antigen (single-dose).
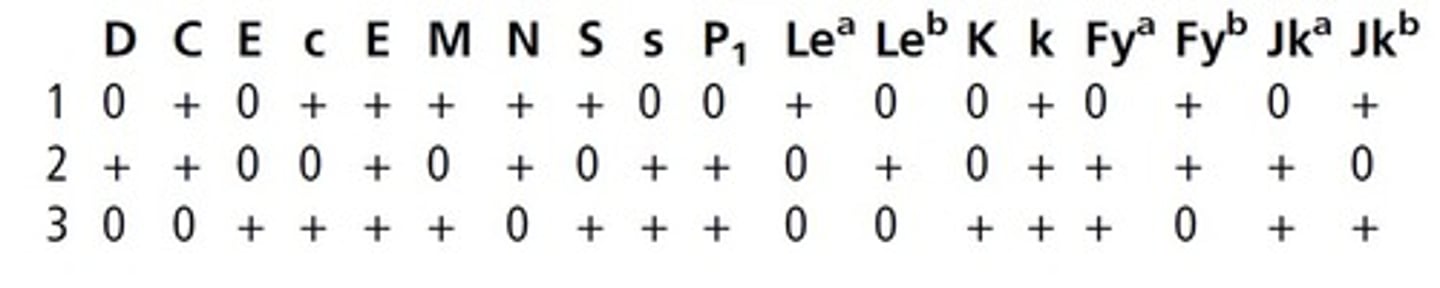
(see pic) Based on the following antigram, which cell is heterozygous
for M?
a. Cell 1
b. Cell 2
c. Cell 3
d. None of the above
a. Cell 1
M and N are antithetical alleles in the MNS system.
A cell with heterozygous expression of the
M antigen would therefore need to also express
the N antigen. In other words, it would need to
beM+N+. Cells that express onlyMor N antigen
(M+N or MN+) would be presumed to be
homozygous for either the M or N antigen,
respectively.
Which antibody can be neutralized with a specific
reagent?
a. Anti-D
b. Anti-Jka
c. Anti-M
d. Anti-Lea
d. Anti-Lea
Neutralization combines a soluble antigen with
antibody in vitro and is used as an antibody identification
technique. Commercially prepared Lewis
substance is available for purchase, so of the list
provided, only anti-Lea could be neutralized.
Group O red blood cells are used as a source of commercial
screening cells because:
a. Anti-A is detected using group O cells
b. Anti-D reacts with most group O cells
c. Weak subgroups of A react with group O cells
d. ABO antibodies do not react with group O cells
d. ABO antibodies do not react with group O cells
O red blood cells possess only the H antigen,
andOred cells used for reagent purposes typically
also lack D antigen. O-negative reagent red
cells do not react with anti-D or any ABO
antibodies.
The use of EDTA samples for the direct antiglobulin
test prevents activation of the classical complement
pathway by:
a. Causing rapid decay of complement proteins
b. Chelating Mg2+ ions, preventing assembly of C6
c. Chelating Ca2+ ions, preventing assembly of C1
d. Preventing chemotaxis
c. Chelating Ca2+ ions, preventing assembly of C1
Ethylenediaminetetraacetic acid (EDTA) chelates
calcium ions to form a soluble complex; therefore
it prevents the assembly of C1.
Check (Coombs control) cells are:
a. Added to every negative antiglobulin test
b. Added to negative direct antiglobulin tests only
c. Used to confirm a positive Coombs' reaction
d. Coated with both IgM and C3d
a. Added to every negative antiglobulin test
IgG-sensitized red cells (check cells or Coombs
control cells) are commercially prepared with
IgG antibodies attached. Proper control of antihuman
globulin (AHG) tests systems (indirect
antiglobulin test [IAT] or direct antiglobulin test
[DAT]) require check cells to be added to negative
tubes to ensure that AHG reagent was added and
is active.
What type(s) of red cells is(are) acceptable to transfuse
to an AB-negative patient?
a. A negative, B negative, AB negative, O negative
b. O negative only
c. AB negative only
d. AB negative, A negative, B negative only
a. A negative, B negative, AB negative, O negative
People with the AB blood type are considered to
be universal recipients because they possess all
possible ABO antigens; therefore they do not
make any antibodies to ABO antigens. People
with AB who are also negative for the D antigen
may receive any type of blood as long as they have
not made an antibody against the D antigen.
A nonbleeding adult of average height and weight
with chronic anemia is transfused with 2 units of
red blood cells. The pretransfusion Hgb is 7.0 g/dL.
What is the expected posttransfusion Hgb?
a. 8 g/dL
b. 9 g/dL
c. 10 g/dL
d. 11 g/dL
b. 9 g/dL
Transfusing 1 unit of red cells usually increases
the hemoglobin (Hgb) by approximately 1 g/dL.
Therefore transfusing 2 units of red cells to a
patient not actively bleeding should increase the
pretransfusion Hgb by 2 g/dL.
An IgA-deficient patient with clinically significant
anti-IgA requires which of the following?
a. Leukocyte-reduced fresh frozen plasma
b. CMV-seronegative RBCs
c. Irradiated RBCs and platelets
d. Washed RBCs
d. Washed RBCs
A patient with IgA deficiency and clinically significant
anti-IgA requires washed red blood cells if a
transfusion is necessary, because washing
removes plasma proteins. It should be noted that
washing is associated with a loss of about 10% to
20% of the original unit.
Anti-H will react weakest with blood from a person
with _____________.
a. Group O
b. Group A1
c. Group A2
d. Group A2B
b. Group A1
Of the types listed, the enzyme that converts
H antigen to A1 antigen is the most active. Therefore
group A1 has very little unconverted H antigen.
The order of blood types possessing the most
H antigens to the fewest H antigens is O>A2>
B>A2B>A1>A1B.
Which of the following antibodies do not match the
others in terms of optimal reactive temperature?
a. Anti-Fya
b. Anti-M
c. Anti-K
d. Anti-S
b. Anti-M
Anti-Fya, anti-K, and anti-S all preferentially react
at the anti-human globulin (AHG) phase. Although
anti-M also can be found to react at the AHG
phase, many examples react only at room temperature
(RT) phase.
What antibody can an R1r patient make if transfused
with R2R2 blood?
a. Anti-D
b. Anti-C
c. Anti-E
d. Anti-c
e. Anti-e
c. Anti-E
A patient with R1r possesses D, C, c, and e antigens.
R2R2 blood possesses D, c, and E antigens.
To determine what antibodies could be made on
exposure, determine what is different between
the two, or what foreign antigen could be introduced
to the patient. In this case, the E antigen
would be foreign and could potentially stimulate
antibody production.
What is the probability of finding blood negative for
the Jka and Fya antigens (23% of population is Jk
[a] and 34% of population is Fy[a])?
a. 5.1%
b. 51%
c. 7.8%
d. 78%
c. 7.8%
To determine the combined phenotype for blood
negative for the Jka and Fya antigens, multiply the
percentages of person negative for each antigen.
0:23 x 0:34 = 0.0782 or 7.8%
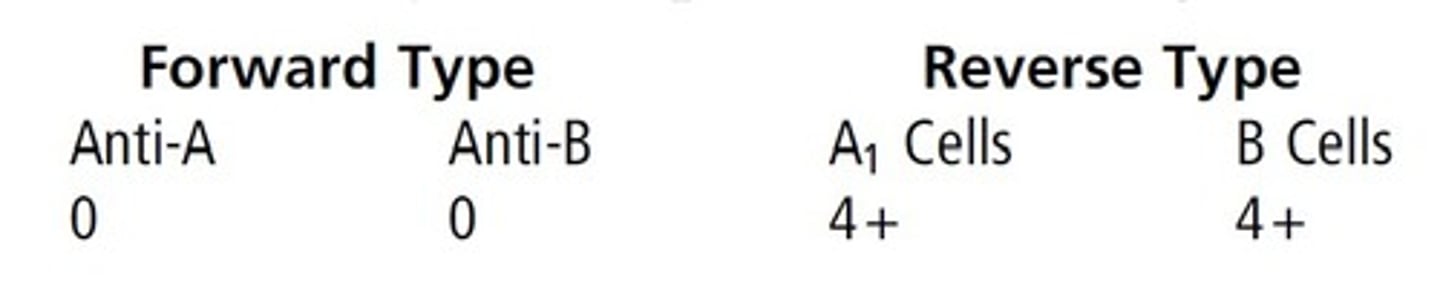
(see pic) If the following patient's RBCs were tested against
anti-H lectin and did not react, this person would
be identified as a(an):
a. Acquired B
b. Secretor
c. Oh phenotype
d. Subgroup of A
c. Oh phenotype
Persons of the Oh phenotype (Bombay) type as
group O, but also possess potent anti-H. This
anti-H is usually detected in tests using group O
cells (antibody screen or crossmatch), but may
be noted in ABO grouping, because the reverse
cells could be hemolyzed instead of just
agglutinated.
If a person has the genetic makeup Hh, AO, LeLe,
sese, what substance will be found in the secretions?
a. A substance
b. H Substance
c. Lea substance
d. Leb substance
c. Lea substance
• Hgene: Produces Hantigen on type II chains in
secretions and H antigen on red cells
• A gene: Encodes for a glycosyltransferase that
produces A antigen
• O gene: Silent gene
• Le gene: Encodes for a fucosyltransferase that
produces Lea antigen
• se gene: Amorph allele; inheriting two se genes
means that the person is a nonsecretor
Le and secretor gene interaction: If Le is inherited
without Se, only Lea will be found on red
cells and in saliva. Because this person is a nonsecretor,
only Lea antigen will be present in the
secretions.
Before A and B antigens can be expressed, the precursor
substance must have the terminal sugar
_______________.
a. d-Galactose
b. N-Acetylgalactosamine
c. Glucose
d. L-Fucose
d. L-Fucose
N-Acetylgalactosamine (GalNAc) confers type A
specificity. D-Galactose (Gal) confers type B
specificity. L-Fucose (Fuc) confers type O specificity.
The type A and type B sugars are built
on Fuc.
A white female's RBCs gave the following
reactions: D+, C+, E-, c+, e+. The most probable
Rh genotype is:
a. DCe/Dce
b. DCe/dce
c. DCe/DcE
d. Dce/dCe
b. DCe/dce
The DCe/dce (R1r) phenotype is found in approximately
35% of whites and 15% of blacks.
Although DCe/Dce (R1Ro) and DCe/dCe (R1r0)
are also possibilities, they are statistically less
probable than DCe/dce. It is not possible for this
person to be DCe/DcE, because she tested negative
for the E antigen.
If a D-positive person makes anti-D, this person is
most likely:
a. Partial D
b. D negative
c. Weak D as position effect
d. Weak D because of transmissible genes
a. Partial D
Individuals who inherit the D antigen with weakened
or missing epitopes are described as having
partial D antigen and often present with weakened
expression of the D antigen. Because the partial
D antigen is essentially incomplete, if an
individual with partial D antigen is exposed to
complete D antigen, the person would theoretically
be able to make an alloantibody against
the parts of the antigen that were foreign.
A serum containing anti-k is not frequently encountered
because of which of the following?
a. People who lack the k antigen are rare
b. People who possess the k antigen are rare
c. The k antigen is not a good immunogen
d. Kell-null people are rare
a. People who lack the k antigen are rare
The k antigen is present in 98.8%of white individuals
and 100% of black individuals, so it would be
very rare to encounter someone who lacked the k
antigen.
A characteristic of the Xga antigen is that the Xga
antigen:
a. Has a higher frequency in women than in men
b. Has a higher frequency in men than in women
c. Is enhanced by enzymes
d. Is usually a saline reacting antibody
a. Has a higher frequency in women than in men
Expression of the Xga antigen is controlled by an
X-linked gene, and prevalence of the antigen is
higher in females than in males. Anti-Xga is usually
IgG and the Xga antigen is sensitive to ficin.
Which of the following is a characteristic of the Kidd
system antibodies?
a. The antibodies are usually IgM
b. The corresponding antigens are destroyed by
enzymes
c. The antibodies are usually strong and stable during
storage
d. The antibodies are often implicated in delayed
hemolytic transfusion reactions
d. The antibodies are often implicated in delayed hemolytic transfusion reactions
Kidd system antibodies are usually IgG, are
enhanced by enzymes, and do not store well.
The titer of Kidd system antibodies in individual
patients can rise and fall quickly, meaning that
they might not be detected in an antibody screen
if the titer is below the detection point of the test
system.
Anti-E will react with which of the following cells?
a. RoRo
b. R1R1
c. R2R2
d. rr
c. R2R2
• RoRo=Dce/Dce
• R1R1=DCe/DCe
• R2R2=DcE/DcE
• Rr=dce/dce
Therefore anti-E will react only with R2R2 cells
because they are the only ones in this list that possess
the corresponding E antigen.
Which statement is not true concerning anti-Fya and
anti-Fyb?
a. Are clinically significant
b. React well with enzyme-treated panel cells
c. Cause hemolytic transfusion reactions
d. Cause a generally mild hemolytic disease of the
newborn
b. React well with enzyme-treated panel cells
Antibodies to Duffy system antigens are clinically
significant (associated with hemolytic transfusion
reactions) and have typically been shown to
cause mild hemolytic disease of the fetus and
newborn (HDFN). Because the Fya and Fyb antigens
are sensitive to enzymes, anti-Fya and
anti-Fyb would not react with enzyme-treated
panel cells.
Which of the following antibodies can be neutralized
with pooled human plasma?
a. Anti-Hy and anti-Ge:1
b. Anti-Cha and anti-Rga
c. Anti-Coa and anti-Cob
d. Anti-Doa and anti-Jsb
b. Anti-Cha and anti-Rga
Anti-Ch and anti-Rg are usually IgG and react
weakly. Neutralization of these two antibodies
with pooled plasma is often used as part of antibody
identification when either or both antibodies
are present.
Donors who have received RBC transfusion within
the last 12 months are deferred because:
a. Blood could transmit hepatitis or HIV
b. Donor red cell hemoglobin level may be too low
c. Donor health would prohibit the donation
process
d. There will be two cell populations in this
donor
a. Blood could transmit hepatitis or HIV
Potential donors who have been transfused in
the last 12 months are deferred because of the possibility
of exposure to diseases. Although viral
marker testing has increased the safety of the
blood supply, some diseases have a window in
which markers are below the threshold of
detection.
Autologous presurgical donations are not allowed
for which of the following patients?
a. Weigh less than 100 lb
b. Under the age of 14
c. With hemoglobin of 13 g/dL
d. With bacteremia
d. With bacteremia
For autologous donors who weigh less than
100 lb, the volume of blood collected and the
amount of anticoagulant used should be proportionately
less when compared to a donation
from a person weighing more than 110 lb. There
is no age restriction for autologous donors.
Hgb concentration in a potential autologous
donor should be no less than 11 g/dL. Therefore
the only condition that would preclude donation
is current bacteremia. Blood collected while a
patient is septic could cause harm if
transfused later.
Which of the following viruses resides exclusively in
leukocytes?
a. HCV
b. HBV
c. CMV
c. CMV
Cytomegalovirus (CMV) can be transmitted
through transfusion via intact white cells contained
in cellular blood products. Leukoreduction
of blood products reduces the risk for
CMV transmission because the CMV virus
resides within intact white cells.
Which product is least likely to transmit hepatitis?
a. Cryoprecipitate
b. Plasma protein fraction
c. RBC
d. Platelets
b. Plasma protein fraction
(PPF) is prepared from
large pools of human plasma. Although PPF
can transmit infectious agents, the risk for doing
so is reduced because certain viruses are inactivated
or removed during preparation. Of the components listed, PPF is the only component
treated in this manner.
In preparing platelets from a unit of whole blood, the
correct order of centrifugation is:
a. Hard spin followed by a hard spin
b. Light spin followed by a light spin
c. Light spin followed by a hard spin
d. Hard spin followed by a light spin
c. Light spin followed by a hard spin
To prepare platelets, whole blood is first centrifuged
at a light spin, and platelet-rich plasma is
expressed off the red cells into a satellite bag. The
platelet-rich plasma is then centrifuged at a hard
spin, and plasma is expressed off of the platelets.
Which antibody could cause hemolytic disease of the
fetus and newborn?
a. Anti-I
b. Anti-K
c. Anti-Lea
d. Anti-N
b. Anti-K
Of the antibodies in this list, anti-K is the one
most likely to be IgG and able to cross the placenta.
Anti-I, anti-Lea, and anti-N typically present
as IgM class antibodies when encountered
in patient specimens.
A group A, D-negative obstetric patient with
anti-D (titer 256) is carrying a fetus who needs an
intrauterine transfusion. The blood needed
should be:
a. Group A, D-negative RBC
b. Group A, D-negative whole blood
c. Group O, D-negative RBC
d. Group O, D-negative whole blood
c. Group O, D-negative RBC
Group O red cells are most generally used for
intrauterine and neonatal transfusions. Rhnegative
blood is used for fetuses and neonates
when the blood type is unknown or Rh-negative.
In this case, because the mother has anti-D, Rhnegative
blood must be used for the intrauterine
transfusion.
Which of the following mothers should receive
RhIG?
a. A-negative mother; O-negative baby; no prenatal
care, anti-D in mother
b. AB-negative mother; B-positive baby; anti-D
in mother
c. O-negative mother; A-positive baby; no anti-D
in mother
d. A-positive mother; A-positive baby; no anti-D
in mother
c. O-negative mother; A-positive baby; no anti-D in mother
Rh immunoglobulin (RhIG) is given to D-negative
mothers to prevent the formation of anti-D. If a
mother has already formed anti-D, then RhIG will
offer no protection.
How many doses of RhIG are indicated for a
Kleihauer-Betke reading of 0.6%?
a. 1
b. 2
c. 3
d. 4
b. 2
To quantify the amount of fetomaternal hemorrhage
(FMH), the percentage of fetal red cells
counted is multiplied by the mother's blood
volume. The mother's blood volume can be calculated
based on her height and weight, but
often the average of 5000 mL is used for
calculation.
0.6/100 = 5000 mL = 30 mL
What should be done first if a mother types as O and
the baby types as AB?
a. Report the results with no further testing
b. Try to get a sample from the father
c. Recheck all labels, get new samples, if necessary,
and retest
d. Retype using all new reagents
c. Recheck all labels, get new samples, if necessary, and retest
An O mother (genotype OO) would contribute
an O gene to her child, so regardless of the
father's type, an O mother could not have an AB
child. A clerical error has likely occurred and
should be eliminated as a cause of potential
error before further serologic studies are conducted.
A newborn has a positive DAT.What is the best procedure
to determine the antibody causing a positive
DAT in this newborn?
a. An antibody titer on the mother's serum
b. An antibody panel on the mother's serum
c. An antibody panel performed on the eluate of the
mother's cells
d. An antibody panel performed on the eluate of the
baby's cells
b. An antibody panel on the mother's serum
Any antibody attached to a baby's red cells
would have to come from the mother. Sample
from the mother is easily acquired and should
be readily available. Although an eluate could
be performed on the baby's cells, that is a timeconsuming
procedure requiring a large sample.
The best procedure is to perform an antibody
panel on the mother's serum.
Which of the following is(are) an example(s) of a
record-keeping error?
a. Use of correction fluid or tape
b. Using pencil
c. Documentation after the fact
d. All of the above
d. All of the above
Use ofwhiteout obliterates the original results, so is
not allowed. Use of pencil results in a record that
could be changed—that is, the record is not permanent. If it is not recorded, it did not happen,
so documentation after the fact is not allowed.
Which of the antigens below is considered low
incidence?
a. Fya
b. S
c. C
d. Kpa
d. Kpa
is an antigen in the Kell system that is present
in 2% of whites and found only rarely in blacks.
Which of the antigens below is considered high
incidence?
a. Fyb
b. Vel
c. E
d. S
b. Vel
is an antigen of high prevalence. Vel exhibits
variable antigen expression on red cells and is
resistant to treatment with enzymes.
In performing tube testing, you see many mediumsized
agglutinates in a clear background. How would
you grade this reaction?
a. 2+
b. 1+
c. 4+
d. 3+
a. 2+
A 1+ reaction has numerous medium and
small agglutinates with a turbid background. A
2+ reaction has many medium-sized agglutinates
with a clear background. A 3+ reaction has several
large agglutinates and a clear background.
A 4+ reaction has a solid agglutinate with a clear
background.
Of the following, which genotypes would result in
the B phenotype?
a. BB
b. AB
c. BO
d. a and b
e. a and c
e. a and c
A and B genes in the ABO system have codominant
expression, and the O gene is a silent allele,
producing no detectable gene product. For an
individual to have a B phenotype, a B gene needs
to be inherited either in a homozygous fashion or
along with an O gene.
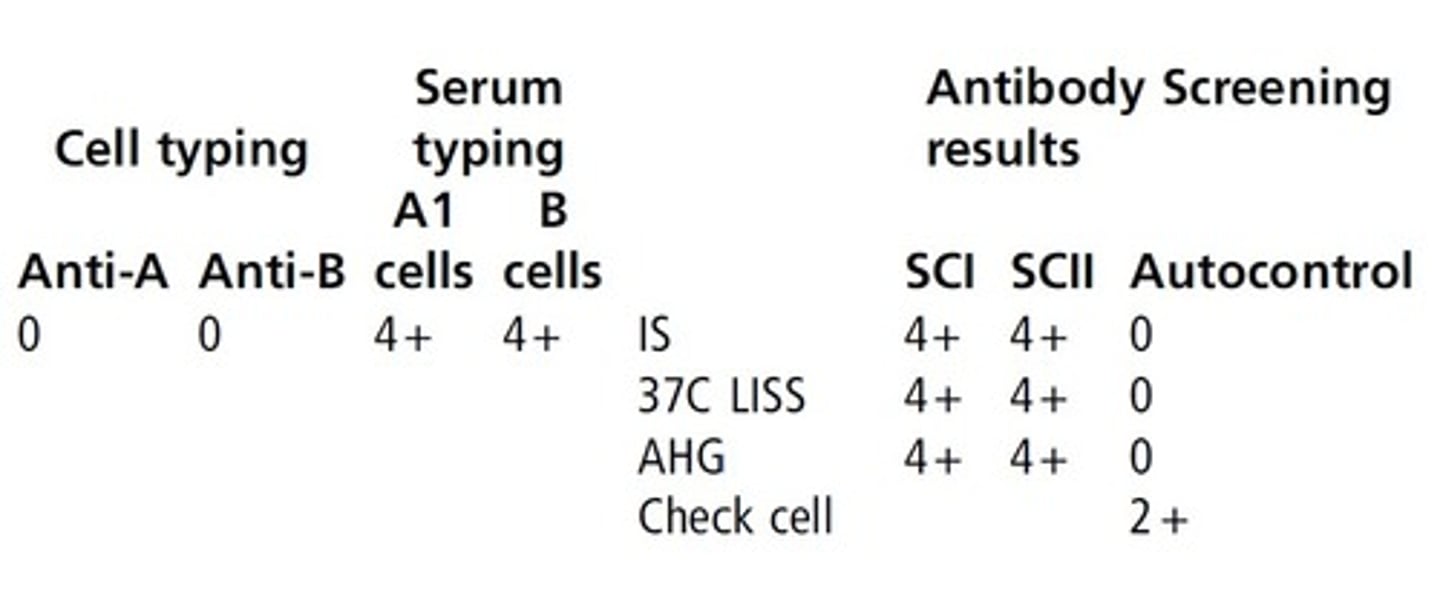
(see pic) How would you interpret the following reactions?
a. Blood type A
b. Blood type O
c. Blood type B
d. Blood type AB
b. Blood type O
The forward type shows no agglutination, meaning
the individual does not possess A or B antigens.
The reverse type shows reactivity with
both A1 and B cells, meaning the individual possess
antibodies to A and B antigens. This is characteristic
of the O blood group.
(see pic) Noting these reactions, if they patient needed blood
now, what type of blood should be transfused?
a. Blood type A
b. Blood type O
c. Blood type A2
d. Blood type A
b. Blood type O
This patient forward types as group A and reverse
types as group O, so an ABO discrepancy is present.
In the event that the patient needs blood
before the discrepancy can be resolved, group O
must be transfused.

Blood group antibodies made by type A and type B
people are predominantly which class?
a. IgE
b. IgA
c. IgG
d. IgM
d. IgM
Group A and B individuals predominantly make
IgM ABO antibodies, but small quantities of
IgG antibody can be seen. Group O individuals
tend to make predominantly IgG ABO antibodies.
This is important to understand why ABO hemolytic
disease of the newborn is more commonly
seen in group O mothers.
(see pic) Based on these reactions, what should be the next step?
a. Test the serum with A2 cells
b. Report the patient as type A
c. Test the cells with anti-A1 lectin
d. Both a and c
e. Request a new specimen
d. Both a and c
This patient forward types as group A and reverse
types as group O, so an ABO discrepancy is present.
You could not report out results until the discrepancy
was explained. The A1 cells are reacting only at 1+ strength, so this points to possible extra
reactivity in the reverse type. Extra reactivity in
the reverse type can be caused by rouleaux,
cold-reactive antibodies (autoantibody or alloantibody),
or passively acquired antibodies. In the
case of a group A individual showing weak reactivity
with A1 cells, this is often seen in group A2
individuals who have made anti-A1. Testing the
cells with anti-A1 lectin would tell us if the patient
possesses A1 antigen, and testing the serum with
A2 cells would tell us if the extra reactivity noted
in the reverse type is likely caused by anti-A1. If
the discrepancy could not be resolved, it would
be advisable to request a new specimen.

A "directed donor" unit of blood is defined as a unit
of blood from a person who gives blood for:
a. Relief of polycythemia or other blood disorder
b. His or her specific use only
c. First-degree blood relative
d. Another person he or she has specified
d. Another person he or she has specified
A directed unit is donated for a specific person
identified by the donor. This is not limited to
blood relatives. A therapeutic phlebotomy is performed
on individuals with polycythemia or other
blood disorders, as ordered by a physician. When
an individual donates blood for his or her own
use, this is called an autologous donation.
Before the patient can receive a directed donation
unit, the patient requires which of the following tests
to be completed?
a. Type and screen only
b. Type and screen and compatibility testing
c. Retype of patient and donor unit
d. No additional testing is required
b. Type and screen and compatibility testing
The only difference between a directed donation
and a volunteer donation is that a directed donation
is reserved for a specified individual. Testing
for transfusion of a directed unit is no different
from that conducted on a volunteer unit intended
for transfusion.
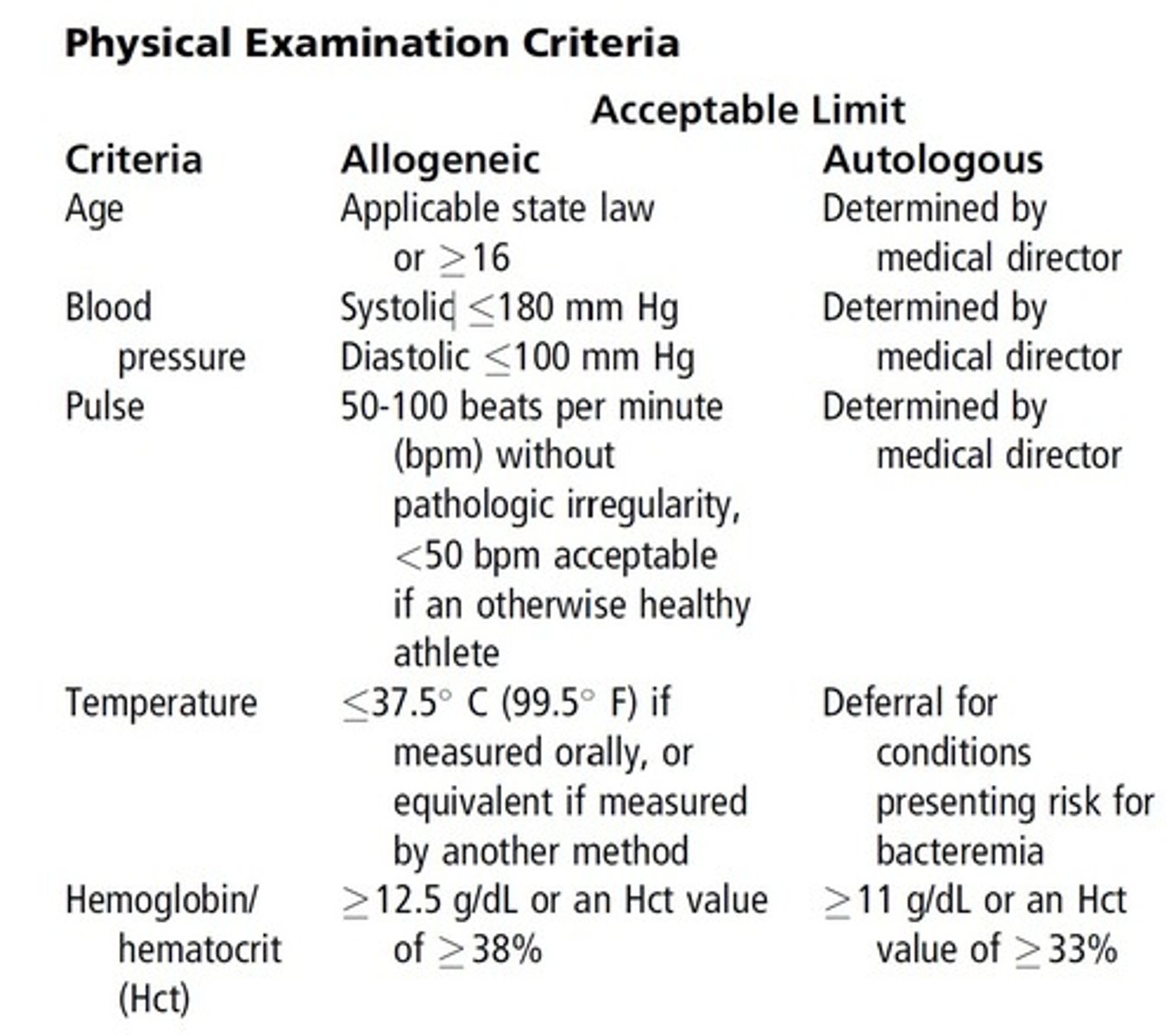
An 18-year-old female with a hematocrit of 38%,
temperature of 37 C, and blood pressure of 175/
90 mm Hg presents for whole blood donation. Based
on this information, would you accept, permanently
defer (PD), or temporarily defer (TD) the donor?
a. Accept
b. TD, blood pressure is too high for a person of
her age
c. TD, temperature is too high
d. PD, for all values listed
a. Accept
Allogeneic donors must meet the following physical
examination criteria before donation: (see pic)
A 63-year-old man with a hemoglobin value of
130 g/dL and pulse of 80 beats/min, who received
human pituitary growth hormone (PGH) when he
was 10 years old, presents for whole blood donation.
Based on this information, would you accept, permanently
defer (PD,) or temporarily defer (TD) the donor?
a. Accept the donor
b. TD, because of the human PGH
c. PD, because of the human PGH
d. PD, because of the high hemoglobin value
c. PD, because of the human PGH
Receipt of human pituitary growth hormone
(PGH) requires indefinite or permanent deferral
because of the theoretical risk for transfusiontransmitted
Creutzfeldt-Jakob disease (CJD).
A 38-year-old female weighing 153 lb, who received
the rubella vaccine 2 months previously, presents to
donate whole blood. She also received 2 units of
packed cells after the delivery of her eighth child
8 weeks ago. Based on this information, would you
accept, permanently defer (PD), or temporarily defer
(TD) the donor?
a. Accept the donor
b. TD because of the packed cells 8 weeks ago
c. PD because of receiving blood products
d. TD because of the rubella vaccine
b. TD because of the packed cells 8 weeks ago
Receipt of the rubella vaccine results in a
temporary deferral of 4 weeks. Because this vaccine
was administered 2 months ago in this individual,
this would not cause a deferral.
Transfusion of blood, components, human tissue,
and/or plasma-derived clotting factor concentrates
results in a temporary deferral of
12 months, so this individual would be temporarily
deferred for 10 months based on the time of
transfusion.
A22-year-old female witha cousinwithAIDSwhohad
taken aspirin the day before and with needle marks on
both arms presents to donate whole blood. Based on
this information,would you accept, permanently defer
(PD), or temporarily defer (TD) the donor?
a. PD, needle marks on both arms
b. TD, needle marks on both arms
c. PD, cousin with AIDS
d. TD, because of the aspirin
a. PD, needle marks on both arms
Use of a needle to administer nonprescription
drugs is a condition for indefinite or permanent
deferral. Casual contact with a person with an
infectious disease generally is not a reason for
deferral. Potential donors who have ingested aspirin
are deferred (48 hours) only if they are donating
apheresis platelets.
Each unit of blood must be tested for all of the following
except:
a. Anti-HIV 1/2
b. HBsAg
c. Anti-HCV
d. Antigen to HCV
d. Antigen to HCV
Required tests for infectious disease screening
include:
• HBsAg
• Anti-HCV
• Anti-HBc
• HCV NAT
• Anti-HIV-1/2
• HIV NAT
• Anti-HTLV-I/II
• Syphilis - RPR or hemagglutination
• West Nile Virus (WNV) NAT
• IgG antibody to Trypanosoma cruzi (Chagas
disease)
The principle of the HBsAg test is to detect which of
the following?
a. Antigen in patient's plasma
b. Antigen on the patient's RBCs
c. Antibody in patient's serum
d. Antigen and antibody in patient's serum
a. Antigen in patient's plasma
The HBsAg test detects the surface antigen of the
hepatitis B virus in the blood. In an infected person,
this antigen can be detected before the antibody
to the core antigen (anti-HBc) is produced.
Cryoprecipitate is prepared by first thawing:
a. Fresh frozen plasma at 1 to 6 C, and then doing
a cold centrifugation to pack the cryoprecipitate
to the bottom so the plasma may be removed
b. Fresh frozen plasma at room temperature, then
placing in the freezer for 2 hours, then centrifuging
and removing the cryoprecipitate
c. Cryoprecipitate at 1 to 6 C, then pooling the
thawed cryoprecipitate in batches of 10 units,
then quickly refreezing
d. Cryoprecipitate at room temperature, then centrifugation
in the cold to concentrate the cryoprecipitate
to the bottom before adding more plasma
to reconstitute
a. Fresh frozen plasma at 1 to 6 C, and then doing a cold centrifugation to pack the cryoprecipitate to the bottom so the plasma may be removed
Cryoprecipitate (CRYO) is defined as the coldinsoluable
portion of FFP thawed at 1-6 C and
is suspended in 10-15 mL of plasma.
Platelets must be kept in constant motion for which
of the following reasons?
a. Maintain the pH so the platelets will be alive
before transfusion
b. Keep the platelets in suspension and prevent
clumping of the platelets
c. Mimic what is going on in the blood vessels
d. Preserve the coagulation factors and platelet
viability
a. Maintain the pH so the platelets will be alive before transfusion
Platelets must be gently agitated during storage by
the use of a rotator to prevent the pH from
decreasing below 6.2.
After thawing and pooling cryoprecipitate for transfusion
to a patient, the product should be stored at:
a. Room temperature
b. 1 to 6 C
c. 37 C
d. 0 C
a. Room temperature
Thawed cryoprecipitate components are stored at
room temperature after thawing.
Fresh frozen plasma must be thawed at which
temperature?
a. 1 to 6 C
b. Room temperature
c. 37 C
d. 40 C or higher
c. 37 C
FFP is thawed at temperatures of 30 C to 37 Cor
in an FDA-approved device.
Frozen red blood cells are prepared for transfusion
by thawing at:
a. Room temperature and then washing with saline
b. 37 C in a water bath and then washing with different
concentrations of saline
c. 37 C control incubator and then mixing well
before transfusion
d. 1 to 6 C for 2 days and then washing with different
concentrations of dextrose
b. 37 C in a water bath and then washing with different concentrations of saline
Frozen red blood cells are prepared for transfusion
by first thawing the unit at 37 C. Next,
the glycerol cyropreservative must be removed
through a stepwise decreasing osmolar solution
of saline.
Which is the most likely reason frozen deglycerolized
red blood cells would be used?
a. A patient with antibodies to a high-frequency
antigen
b. Pregnant women requiring intrauterine
transfusions
c. Emergency transfusion situations
d. Group AB Rh-negative patients
a. A patient with antibodies to a high frequency antigen
As frozen units need to be thawed and deglycerolized
prior to transfusion, use of frozen units in an
emergency transfusion situation is not practical.
Group AB Rh-negative patients can receive O, A,
B, or AB Rh-negative units, so transfusion needs
could likely be handled from available refrigerated
units of blood. There are special considerations that
must be made for pregnant women who requiring
an intrauterine transfusion, but a frozen unit of
red cells would likely only be used in the event of
an antibody to a high frequency antigen. Therefore
the best answer for this question is A. Red cell units
are usually frozen for long-term preservation to
maintain an inventory of rare units.
One indication for transfusion of thawed/pooled
cryoprecipitate would be replacement of which of
the following?
a. Factor X in hemophiliacs
b. Factor VIII in massively transfused patients
c. Fibrinogen
d. Volume
c. Fibrinogen
Indications for transfusion of cryoprecipitate
include von Willebrand's disease, Hemophilia A,
to control bleeding associated with fibrinogen
deficiency, and Factor XIII deficiency.
A contraindication for transfusing red blood cells to
a patient is if the patient:
a. Is massively bleeding
b. Has well-compensated anemia
c. Has bone marrow failure
d. Has decreased red blood cell survival
b. Has well-compensated anemia
Indications for transfusionof redbloodcells include
treatment of anemia in normovolemic patients and
physician decision based on the clinical status of the
patient. Patients that are massively bleeding, have
bone marrow failure, or have decreased red blood
cell survival have clinical situations thatwouldwarrant
transfusionbecauseof the needfor hemoglobin
replacement. In patients with compensated anemia,
the body has adapted to allow for adequate tissue
oxygenation. Transfusion should be withheld in
this case until the patient shows clinical signs of
inadequate tissue oxygenation.
Concerning the component and the required quality
control results, which of the following is a true
statement?
a. FFP must have 80 international units of fibrinogen
in 7 units tested
b. Cryoprecipitate must have 80 international units
of factor VIII
c. Leukocyte-reduced red blood cells must have
fewer than 3.31011 WBCs in each unit
d. Platelets must have no red blood cells
b. Cryoprecipitate must have 80 international units of factor VIII
FFP has no quality control or minimum requirements.
Cryo must have80 IU of Factor VIII
and150 mg of fibrinogen. Leukocyte reduced
red cells must have <5106 residual leukocytes
and 85% of original red cells retained. There
are no quality control or minimum requirements
for the number of red cells in platelets.
Fresh frozen plasma must be stored at:
a. Colder than 18 C for no longer than 1 year
from donation
b. Colder than 38 C for no longer than 1 year
from donation
c. Exactly 18 C for no longer than 1 year from
donation
d. 18 C to 38 C for up to 10 years from
donation
a. Colder than 18 C for no longer than 1 year from donation
FFP is stored at -18 C for 12 months,
or -65 C for 7 years with FDA approval.
The storage temperature for packed red blood cells is
_______________.
a. 1 to 10 C
b. 1 to 4 C
c. 1 to 6 C
d. 20 to 25 F
c. 1 to 6 C
Per AABB guidelines, packed red cells are stored
at 1 C to 6 C.
Platelets made from a single whole blood donation
should contain which of the following?
a. 3x1011 platelets in 90% of samples
b. 3.3x109 platelets in 75% of samples
c. 5.5x1010 platelets in 90% of samples
d. 10x1010 platelets in 75% of samples
c. 5.5X1010 platelets in 90% of samples
Platelets made from a single whole blood donation
(random platelets) should contain 5.5x10^10
platelets in 75% of the units tested.
Frozen red blood cells must be stored at
__________________.
a. 180 C or less
b. 18 C or less
c. 32 C or less
d. 65 C or less
d. 65 C or less
RBCs Frozen with 40% glycerol are stored
at -65 C for 10 years.
The temperature for incubation of the indirect antiglobulin
test (IAT) should be ____________.
a. 24 C
b. 6 C
c. 37 C
d. 37 +/- 10 C
c. 37 C
In the IAT, incubation takes place at 37 C for
a specified amount of time to allow antigenantibody
reactions to occur.
The temperature of a blood refrigerator without a
continuous recording device should be recorded:
a. Daily
b. Every 4 hours
c. Once every 24 hours
d. Every 30 minutes
b. Every 4 hours
Per AABB Standards, if an automated temperature
recording device is not used, then temperatures
of the blood component storage
environment must be measured manually every
4 hours.
When should quality control be performed on routine
blood typing reagents?
a. At the beginning of each shift
b. Once daily
c. Weekly
d. Only when opening a new vial
b. Once daily
As suggested by AABB, red cell reagents, antisera,
and antiglobulin serum should have quality
control performed each day of use.