module 14: acid-fast bacteria
1/19
Earn XP
Description and Tags
genus: mycobacterium
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
acid-fast bacteria
difficult to stain with dyes, but once stained, dye is retain even if treated with acid-alcohol. due to cell wall composition.
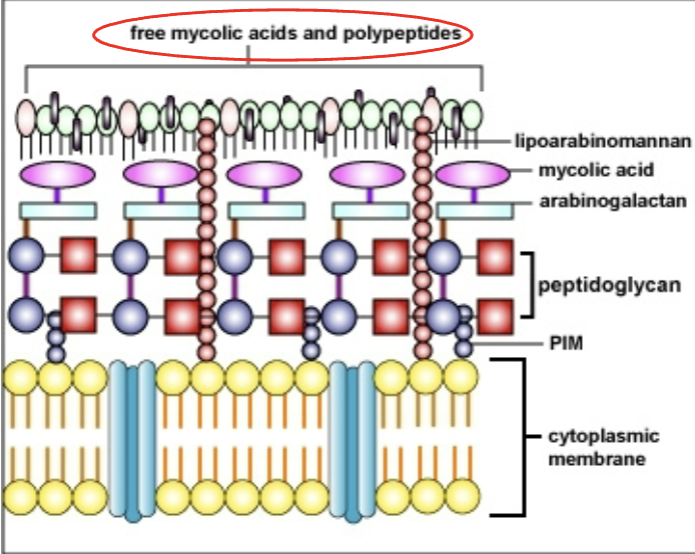
cell wall composition of acid-fast bacteria
unique lipid surface composed of long-chain fatty acids (mycolic acids). TB-specific drugs target mycolic acid synthesis. bind basic dyes, resist staining with many dyes. resistent to acids, alkali, drying. have hydrophobic surface: dyes bound upon use of heat & increase in staining time
acid-fast stain (Ziehl-Neelsen stain)
fix smear with heat, apply carbolfuchsin (primary stain). heat to steaming (or 5 min at room temp). rinse with water. decolorize with acid alcohol, stain with methylene blue (counter-stain). blot slide dry. red = acid-fast bacteria. blue = background.

mycobacterium leprae
causes hansen’s disease: chronic communicable disease that targets skin, mucous membranes, peripheral nerves. source: humans & armadillos. direct contact via inhalation of aerosol droplets. humans have high resistance, disease usually follows prolonged exposure. subclinical infection: no symptoms, + skin test. 2 types
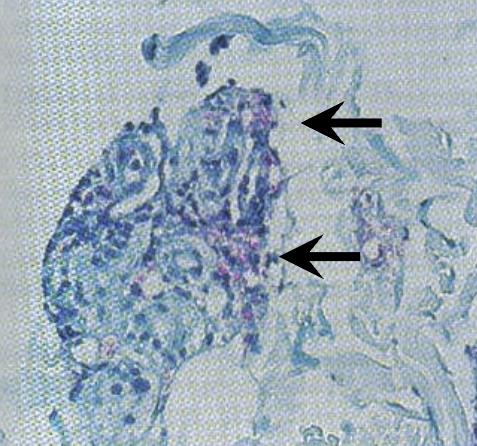
laboratory diagnosis of M. leprae
doesn’t grow on traditional culture media. grows on food pads of armadillos. acid-fast bacteria present inside lepra cells, which are modified mononuclear cells
tuberculoid leprosy
localized mild form of disease. erythematous macules or papules on body. peripheral nerve involvement/damage produce areas of neuropathy: lack of feeling or touch sensations. host response: wall off organism from healthy neighboring tissue (granulomas). lebra cells well-confined within small nodules that don’t spread b/c of strong immune response
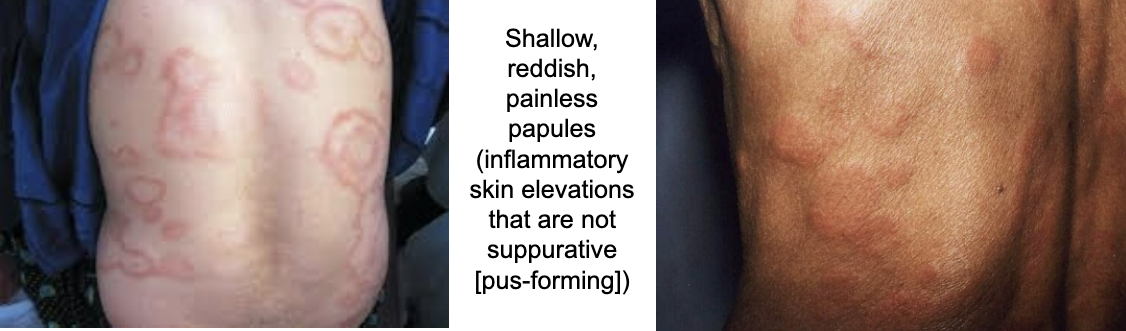
lepromatous leprosy (nodular form)
disseminated form of disease. usually occurs due to deficient cell-mediated immunity. nodules of tumor-like lesions on skin & mucous membranes. lesions open & drain, can lead to secondary infections
treatment & prevention of leprosy
3-drug regimen: rifampin, clofazimine, dapsone. multi-drug therapy (MDT): doesn’t cure, but controls. isolate into leper colonies, vaccines like BCG
mycobacterium tuberculosis (MTB)
causative agent of TB. chronic granulomatous infection. any tissue or organ can be infected, predilection for lungs (pulmonary, extrapulmonary = not in lungs). susceptible are very young, very old, immunocompromised due to low CMI response, IV drug abusers, those in poor living conditions, those with poor nutrition
laboratory diagnosis of MTB
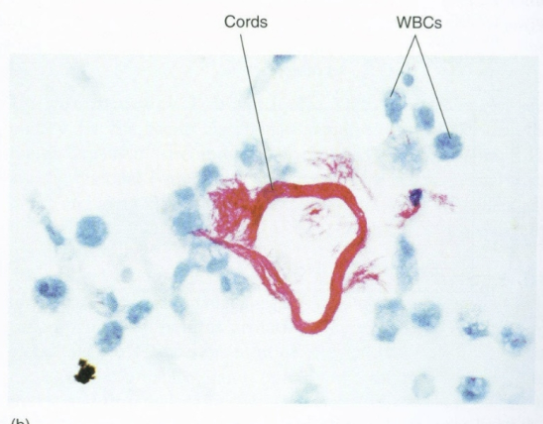
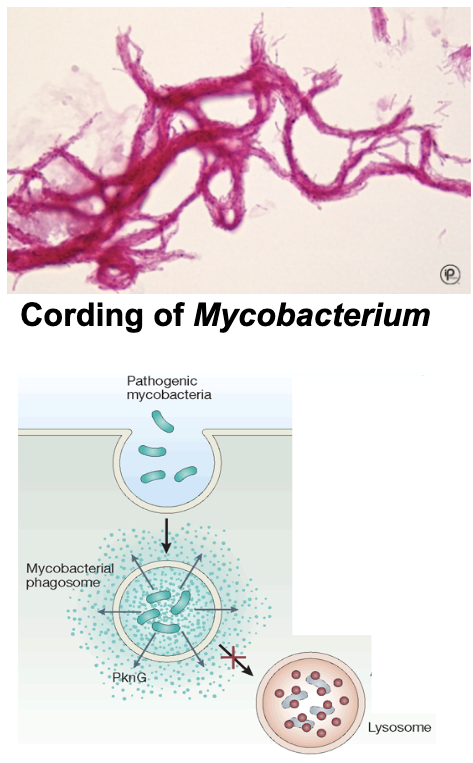
sample digestion, decontamination. sputum sample: mucous & bacteria can contaminate culture. culture: slow growing, aerobic, increased CO2, 35-37C. AFB stain: serpentine cording. cord inhibits phagocytosis, inhibits neutrophil migration, toxic to mammalian cells. niacin accumulation, nitrate reduction, catalase positive
tuberculin
purified protein derivative (PPD) of MTB. used to test if person is exposed to this protein from bacteria, vaccination, or exposure. injected under the skin on forearm, read 2-3 days later to test if they have anti-TB antibodies (Mantoux test)
Mantoux test
positive skin reaction: hard, dense wheal (red, itchy raised welt), indicates propr exposure. negative skin reaction: no hard, dense, raised mass
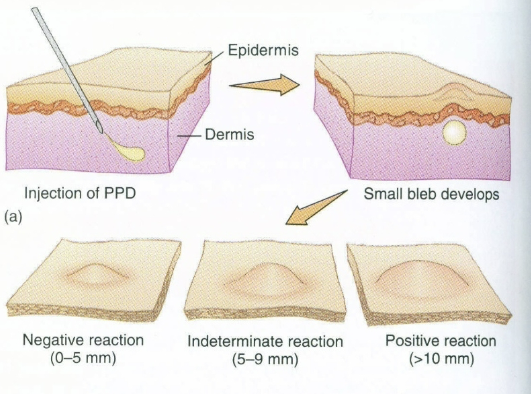
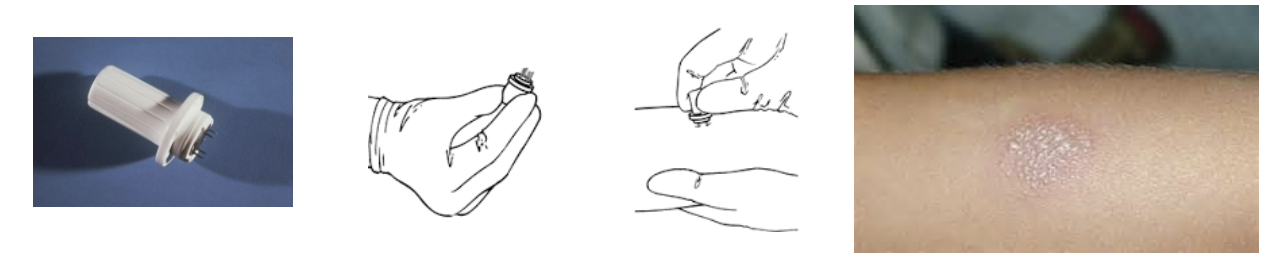
tine test (screening test)
multiple puncture tuberculin skin test. uses small button that has 4-6 short needles coated with tuberculin. pressed into skin, forcing antigens into skin. measure size of palpable induration. negative result: no papules. positive test should be verified using Mantoux test
determinants of MTB pathogenicity
cord factor: cell wall glycolipid, contributes to virulence, causes granulomatous lesions. survives intracellularly: protected from functional processes of phagocyte due to cell wall lipids. once inside phagocytes, MTB inhibits phagosome-lysosome fusion
clinical infection of MTB
from infected humans. people are susceptible, but have inherent resistance. ingestion when primary lesions in mouth & intestines. contact of broken skin with organism. inhalation of infected droplets, multiplication, primary pulmonary infection. bacteremia may follow with dissemination to multiple organs. tuberculin skin test positive (hypersensitivity response) within 6 weeks.
primary tuberculosis
alveolar macrophages in lungs phagocytose MTB & form granulomatous tubercles. tubercles disintegrate to form cheese mass (caseation) in lungs, which becomes cavity. with adequate CMI, T-lymphocytes become active, lesions heal, injured tissue calcifies. potential for TB reactivation exists
active tuberculosis
lack of localized containment of infection, follows primary with inadequate CMI. liquefication of caseous mass (necrotic process leading to gross appearance of the lungs to be cheesy"). microbe number increases & organisms spread. lesions result. fever, chills, night sweats, weight loss, cough, hemoptysis (bloody sputum)
treatment & prevention of MTB
MDR: INH, PZA, ethambutol. rest, balanced diet, vitamins (esp. C). isoniazid (INH): used when change in skin test result from - to + (suggests infection). BCG vaccine: attenuated bovine TB bacillus. used in some locations, not always effective
mycobacterium bovis
causes TB in cows. highly virulent to man. transmissible to humans via ingestion of milk. niacin negative (distinguish from M. tuberculosis), associated with TB of lungs, bone, viscera, & GI tract
mycobacterium avium-intracellulare complex
mainly from contaminated water via ingestion. similar to TB: cough, fever, weight loss, night sweats. disseminated disease. most common systemic bacterial infection in HIV/AIDS. treatment: multi-drug regimen (not always effective): ethambutol, rifamycin, clofazimine, aminoglycoside