final exam blueprint
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
adverse effects of captopril
Cough, unpleasant Gi distress and pancytopenia
Digoxin hold parameter
pulse less than 60 adult 70 kid 90 infant
arrhythmias
adverse effects of milrinone
Ventricular arrhythmias hypotension
and thrombocytopenia.
Quinidine most common adverse effects
•Dizziness, drowsiness, slurred speech
•n/v, changes in taste
•New arrhythmias
•Respiratory depression
quinidine contradinications
Bradycardia, heart block (minus pacemaker) HF hypotension shock and electrolyte disturbances
Patient teachings for nitroglycerin
Teach pt to lay or sit down prior to admin (risk of low bp)
Sublingual dose every 5 minutes if relief isn’t felt total of three times. If pain persistent the pt should go to the ER
nursing monitoring considerations for atorvastatin
Monitor serum cholesterol and LDL levels before and periodically during therapy to evaluate the effectiveness of this drug.
Monitor liver function tests before and periodically during therapy to monitor for liver damage; consult with the prescriber to discontinue the drug if the aspartate aminotransferase (AST) or alanine aminotransferase (ALT) level increases to three times higher than normal.
Cholestyramine drug-drug interaction
•Malabsorption of fat-soluble vitamins
•Delayed absorption of thiazide diuretics, digoxin, warfarin, thyroid hormones, hormonal contraceptives, corticosteroids
•Separate by taking these drugs 1 hour before or 4-6 hours after bile acid sequestrants
Nursing assessment for drugs affecting coagulation
screen for hemorrhagic disorders recent traumas spinal puncture gi ulcers recent surgery intrauterine device placement TB indwelling cath threatened abortion
asses baseline status before beginning therapy: body temp, skin color lesions and temp; affect orientation and reflexes; pulse blood pressure perfusion respiration and adventitious sounds, clotting studies renal and hepatic function test CBC stool guaiac ECG
evaluate for therapeutic effects of warfarin INR 2-3 sxs of blood loss
iron deficiency anemia
▪See this in blood loss, GI bleeding
▪Menstruating people
▪Pregnant/lactating people (demands increased)
▪Rapidly growing adolescents
▪c/o being tired d/t insufficient O2 delivery to the tissues.
▪Usually treated with iron replacement therapy
Megaloblastic anemia
▪Insufficient folic acid or vitamin B12 which leads to slowing of nuclear DNA synthesis that results in larger, immature cells
▪They become crowded in the bone marrow and fewer RBCs are produced which leads to increased immature cells in circulation
▪Folic acid: leafy green veggies, milk, eggs, liver; treat with folic acid or folate
▪Vitamin B12: meats, seafood, eggs, and cheese; treat with vit B12
▪Pernicious anemia
hemolytic anemia
▪Can be inherited (sickle cell and thalassemia) or acquired
▪Sickle cell: abnormal Hgb, Hemoglobin S, gives RBCs a sickle-shaped appearance. Sickled RBCs can become lodged in tiny blood vessels causing occlusions and anoxia/infarction of tissue in that area= SEVERE pain
▪Thalassemia causes decreased synthesis of alpha- or bet—Hgb chains of hemoglobin. Ineffective maturation of the RBC leads to early lysis.
Nursing considerations for lorazepam
maintain pt who have received parental benzodiazepines in bed for at least 3 hours after admin
taper dose gradually (seizures in epileptic pts and withdrawal symptoms)
give IV slow (bc agent is associated with bradycardia hypotension and cardiac arrest
Contraindications of benzodiazepines
•Smaller doses in pts with liver disease
•Crosses placenta and breast milk; known to cause birth defects
•Glaucoma or alcohol intoxication heightened
•Black box: if combined with opioids, profound sedation, resp depression can lead to coma, death
•15-20% of African-Americans have delayed metabolism of benzos
•Caution with elderly – unpredictable reactions
Adverse effects of MAOI
•Dizziness, excitement, mania, tremors, agitation
•Liver toxicity
•n/v/d
•Fatal hypertensive crisis –occipital headache, palpitations, neck stiffness, nausea, vomiting, sweating, dilated pupils, tachycardia, chest pain – leads to intracranial bleed/ fatal stroke
Adverse effects of TCA
•Drowsiness, sedation, sleep disturbances, fatigue, hallucinations, visual disturbances, difficulty concentrating, weakness, ataxia
•Dry mouth, constipation
•Hypo or hypertension
•Arrhythmias
•Withdrawal syndrome if stopped abruptly
•VERY lethal if taken in an OD
Therapeutic action of MAOI
•Reserved for pts not responding to other medications
•Inhibits MAO – an enzyme which breaks down norepinephrine, dopamine, and serotonin
•Strict dietary regimen to prevent toxicity
Therapeutic action of TCA
•Inhibits reuptake of norepinephrine and serotonin – leading to increased concentrations in brain
•Anti-cholinergic effects
•Sedative effects – most effective for depressed pts with anxiety and sleep disturbances
•Clomipramine also used for OCD
•Treatment of enuresis
Nursing considerations and teaching needs for clozapine
warn about the risk of tardive dyskinesia and ither extrapyramidal side effects with continued use
asses temp skin color lesions CNS orientation affect reflexes bilateral grip strength bowel sounds and reported output pulse ascultation and blood pressure RR and adventitious sounds urinary output obtain liver and renal test BG levels thyroid function EKG CBC
Nursing considerations and teaching needs for lithium
frequent serum lithium lvl (specifically in renal cv disease dehydration debilitation and those taking diuretics monitor for toxic levels and arrange appropriate dose)
adequate intake of salt and water, risk of dehydration in hot weather
nurse monitoring and teaching needs for phenytoin
nurse monitoring and teaching needs for hydantoins
Dopaminergic agents
•Effective at increasing dopamine levels as long as dopamine receptors remain in the substantia nigra to respond
•Restores balance of inhibitory and stimulating neurons
•Relieves signs of Parkinson disease
•Apomorphine SQ
•Carbidopa added to increase effect
pediatric considerations for muscle rexlantants
safety not established
Metaxalone has established ped dose
other agents, dose, age and weight
Baclofen is indicated for muscle spasticity with cerebral palsy
Methocarbamol-treated tetanus
dantrolene upper motor neuron spasticity
centrally acting muscle relaxants indication
•Baclofen used for neuromuscular diseases
•Methocarbamol used for tetanus
•Other meds: use with other measures such as rest, ice/heat, NSAIDs
teaching points and nursing assessments for opiods
performing baseline and periodically pain assessment
assess CNS effects monitor resp rate sculate lungs for adventitious sounds to evaluate ae
monitor pulse bp and CO
institute comfort and safety measures
teach to avoid driving assistance with ambulation and avoid making important decisions
adult lifespan considerations for antimigraine and opioids
Migraine meds contraindicated in pregnancy, barrier contraceptive, no breastfeeding
opioids: used cautiously in pregnancy, neonatal opioid withdrawal
pt teaching for oral contraceptives
steps to take if a dose is misses/ lost
smoking cessation
indication of hydroxyprogesterone
Reduction of risk of preterm birth in patients with a single-fetus pregnancy who have a history of singleton spontaneous preterm birth
indications and therapeutic actions of androgens
•Growth and development of male sex organs and maintenance of secondary sex characteristics
•Increase retention of sodium, potassium, nitrogen, phosphorus, and decrease urinary excretion of calcium
•Increases protein anabolism, reduces protein catabolism
•Increase production of RBC
•Danazol – used for endometriosis and fibrocystic breast disease in females
phenylephrine contraindications and most common adverse effects
contraindication
hypertension and glaucoma
•Caution is pts with history of heart disease
•Alpha2 drugs should not be used if hypotensive or bradycardia
adverse effects
•Anxiety, restlessness, strange dreams
•Arrhythmias
•n/v, difficulty urinating
dose specific considerations for adrenergic antagonist
peds dose calculated by age and weight second check does with 2nd nurse
Anticholinergic agents therapeutic action
•Blocks Ach receptors
•Decreases secretions before anesthesia, treat Parkinsonism, restore heart rate & blood pressure after vagal stimulation, relieve motion sickness/vomiting, relaxes bladder muscles/tightens sphincters, inhaled agents for bronchospasms and relieving hay fever rhinitis
Important teaching points for anticholinergic
Avoid driving and operating heavy machinery
stay hydrated
Monitor heat exposure
Avoid OTC meds
follow up
important teaching points: lifespan
doxycycline antibiotics lifespan
can cause pitting enamel and calcium deposits in growing bones
barrier contraceptive
Adverse Reactions: Vancomycin
•n/v/d, taste alterations
•C. diff
•Nephrotoxicity
•Red man syndrome
Important teaching for Zidovudine
important teaching points for topical antifungals
correct method of admin
length of time necessary to treat infection
clean dry socks
keep infected area clean, mild soap and pat dry keep dry
avoid scratching, use cool coompress
avoid occlusive dressings and applying to open skin b/c risk of systemic aborbption
report local irritation, burning oer worsening of infection
drug drug interactions of Amphotericin B
nephrotoxic meds
Drug drug interactions Dextromethorphan
MAOIs
Patient education drugs acting on the Upper respiratory tract
drug drug interactions of Theophylline
caffeine
cig
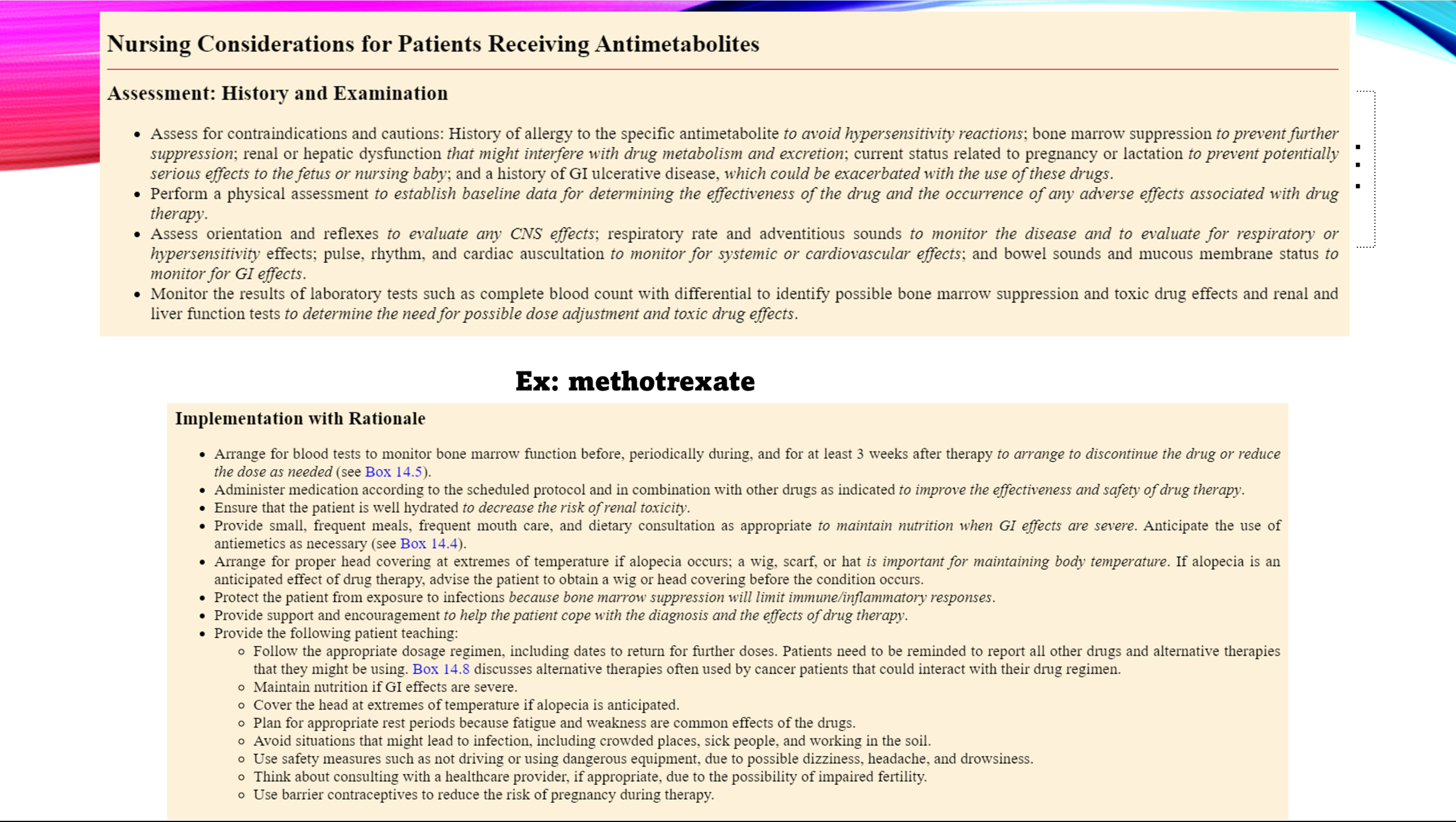
patient teachings and nursing intervention of Methotrexate
Adverse effects: Salicylates
dyspepsia
bleeding
salicylism- tinitus, dizziness n/v/d
salicylate toxicity → cardiac and respiratory collapse
Therapeutic Action: Acetaminophen
•Acts directly on thermoregulatory cells in hypothalamus to cause sweating and vasodilation
Indications: NSAIDs
•Start with these for rheumatoid arthritis (ibuprofen)
Nursing interventions: Immune Suppressant |
protect pt from expsure to infections and mainain strict aseptic technique
instruct on the use of barrier contraceptive
Contraindications: Vaccines
acute illness
immune deficiency
caution pregnancy
allergies and hypersensitivity
recieved immune globuins/ blood products within 3 mo
adverse effects of Furosemide
hypokalemia
hypocalcemia
hypotension
ototoxicity
alkalosis
adverse effects of Spironolactone
•Hyperkalemia – lethargy, confusion, ataxia, muscle cramps, arrhythmias
•Androgen effects – hirsutism, gynecomastia, deepening of voice, irregular menses
Contraindications of Furosemide
severe renal failure
hepatic coma
caution pregnancy, lupus, peds gout
contraindication of Spironolactone
hyperkalemia severe renal disease caution pregnancy
patient teachings of phenazopyridine
causes reddish orange urine
measures to prevent UTIs
patient teaching of antacids
importance on maintaing fluid and nutritional intake if GI upset occurs
Bowel training to deal with diarrhea/ constipation
Caution with prolonged use and rebound acid
periodic monitoring
Therapeutic Action: H2 Anatagonist
•H2 blockers
•Blocks h2 receptors – reducing 70% of hydrochloric acid release
•Used for short-term treatment of duodenal ulcers, prophylaxis of stress-induced ulcers in critical patients, treatment of erosive GERD, relief of heartburn, acid indigestion, and sour stomach
•Famotidine approved for pediatrics
Therapeutic Actions Chemical stimulant
•Directly stimulates the nerve plexus in intestinal wall to increase movement
•Castor oil – blocks absorption of fats but can lead to constipation due to lack of stimulus
Adverse Effects Chemical stimulant
•Diarrhea, abdominal cramping, nausea (GI upset)
•Dizziness, headache
•Sweating, palpitation, fainting (sympathetic stress reaction to the GI stimulation)
•Cathartic dependence – overuse of laxatives; GI tract becomes dependent, leading to constipation, impaction
Adverse Effects Loperamide
Constipation, N/
fatigue weakness
Therapeutic Actions Loperamide
Slow motility of GI tract
Relieve symptoms of diarrhea reduce output on ileostomies.
reduces cramping
contraindication of Hydroxyzine
nursing assessment for Dronabinol
assess CNS effects, don’t combine with hCNS suppressants
can alt mental status safety precautions.
nursing considerations of Octreotide
assess abd
arrange for baseline ultrasound evaluation of the gallbladder to detect the presence of gallstones before treatment.
desmopressin indication
patient teachings of Prednisone
Protect the patient from exposure to infection
Drug-drug interactions Adrenocortical Agents
glucocorticoids (methylprednisolone, prednisolone, prednisone, budesonide)
•Effects increase when combined with erythromycin, ketoconazole
•Effects decreased when combined with salicylates, barbiturates, phenytoin, rifampin
•With NSAIDs or etoh can increase GI distress/bleeding
•Use with K-depleting agents can cause hypoK
•With vaccines can reduce antibody response
mineralocorticoids
•Effects decreased when combined with salicylates, barbiturates, phenytoin, rifampin
•Decreased effectiveness of antidiabetic meds
indication of radioactive iodine
indications of Glargine
indication of Metformin
•Improves insulin sensitivity of peripheral cells
•Used off label for PCOS
Therapuetic action and indications of epinephrine
dilation of the bronchi increase rate and depth of respirations
drug of choice in acute bronchospasms