WCU PHYS 261 Final
1/102
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
103 Terms
internal respiration and external respiration
What are the 2 types of respiration?
from a high area to a low area
In which direction does air flow due to pressure differences?
Gas exchange that occurs between the aleveoli and RBCs, and between the RBCs and tissue
What is internal respiration?
air movement between the lungs and the atmosphere
What is external respiration?
when air moves from the atmosphere into the lungs
What is inhalation?
when air moves from the lungs into the atmosphere
What is exhalation?
that pressure and volume are inversely proportional
What is Boyle's Law?
760 mmHg
What is the atmospheric pressure at sea level?
pressure inside the lungs
What is intrapulmonary pressure?
volume inside the lungs
What is intrapulmonary volume?
760mmHg
What is the atmospheric pressure and intrapulmonary pressure when you are at rest?(neither inhaling or exhaling)
400ml air
What is the lung volume during rest?
lower
For inspiration, is the intrapulmonary pressure higher or lower than the atmospheric pressure?
-blood O2 levels are low, while CO2 is high
-chemoreceptors get stimulated
-chemoreceptors stimulate medulla(respiratory center)
-medulla stimulates the phrenic nerve
-phrenic nerve stimulates the diaphragm and respiratory muscles
-diaphragm and muscles move down and outward
-negative pressure created inside the lungs
-thoracic veins drain blood into the lungs
-increase in intrapulmonary volume
-decrease in intrapulmonary pressure by 4mmHg= 756mmHg
-air enters lungs
What are the steps of inspiration?
Central receptors
-located near the medulla
-detect hydrogen concentration in CSF and by detecting hydrogen, it can tell if CO2 has increased
Peripheral receptors
-found in carotid artery and aortic bodies
-detects a decrease in O2 levels, and if decreased, it stimulates the medulla
What are the 2 types of chemoreceptors and their functions?
-inhalation caused the lungs to be filled with air
-stimulates stretch receptors within the medulla
-medulla inhibits the phrenic nerve
-diaphragm and respiratory muscles no longer stimulated by phrenic nerve
-diaphragm and muscles relax
-diaphragm moves up and muscles move inward
-lungs recoil properly
-blood is pushed out of the lungs
-decrease in intrapulmonary volume
-increase in intrapulmonary pressure by 8mmHg= 764mmHg
-air leaves lungs
What are the steps of expiration?
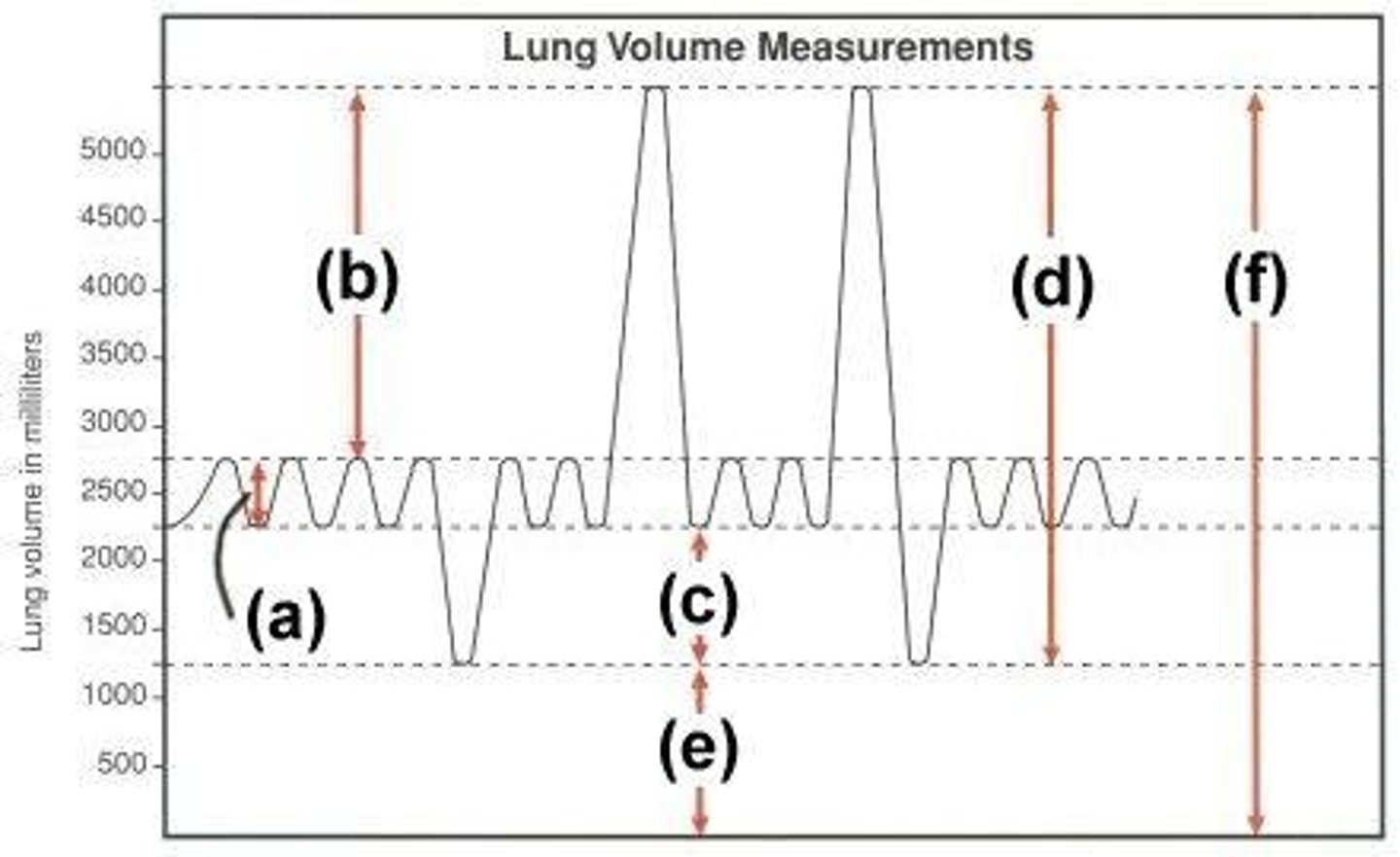
a- tidal volume(TV): a normal breath
b- inspiratory reserve volume(IRV): the amount of air your can forcefully inhale after a normal inhale
c- expiratory reserve volume(ERV): the amount of air you can forcefully exhale after a normal exhale
d- vital capacity(VC): the amount of air that can be manipulated
e- residual volume(RV): the amount of air always left in the lungs
f-total lung capacity(TLC): the total amount of air your lungs can hold
What are the parts of components capacity and their meaning?
-the concentration of free hydrogen ions in a solution
-0-14
-acidic: 0-7, neutral: 7-8, basic: 8-14
What is pH, its range, and the categories within its range?
-pH is acidic
-metabolic: imbalance between acid and base due to excess acid in the body or not enough base in the body
-respiratory: imbalance between acid and base due to excess CO2 in the body
What is acidosis, the 2 types of acid-base disturbances, and their meanings?
-pH is alkaline(basic)
-metabolic: imbalance between acid and base due to excess base in body or not enough acid in body
respiratory: imbalance between acid and base due to not enough CO2 in body
What is alkalosis, the 2 types of acid-base disturbances, and their meanings?
metabolic(compensation done by the respiratory system): hyperventilation- releasing CO2 because CO2 is an acid, and releasing it will increase the pH
respiratory(compensation done by the metabolic system): kidney will increase reabsorption of HCO3-, and because HCO3- is basic, it increases the pH
What are the 2 compensations for the 2 types of acidosis?
metabolic(compensation done by the respiratory system): hypoventilation- retaining CO2 because CO2 is an acid, and retaining it will decrease the pH
respiratory(compensation done by the metabolic system): kidneys will increase secretion of HCO3-, and because HCO3- is basic, it decreases the pH
What are the 2 compensations for the 2 types of alkalosis?
-transportation of nutrients and hormones
-regulation of water and pH
-defense against infections and blood loss
What are the functions of blood?
fluid plasma and blood cells(RBCs, WBCs, and platelets)
What is blood composed of?
Water, hormones, ions, molecules, and proteins
What is plasma composed of?
albumin: 2/3 of the plasma proteins, produced by liver, creates and maintains oncotic pressure
globulins: 3 types- alpha, beta, and gamma, make up immunoglobulins
clotting proteins: 12 different types, produced by liver
What are the plasma proteins and their functions/characteristics?
-the process of RBC production
-produced by bone marrow from stem cells, production is controlled by erythropoietin(released by kidneys)
What is erythropoiesis and its characteristics?
-to transport O2 in blood
-4 chains with 1 heme group each that contains iron that binds oxygen
What are the functions of hemoglobin and its structure?
factors that influence oxygen-hemoglobin binding and release
What is the oxygen-hemoglobin dissociation curve?
-hemoglobin has a low affinity to O2, so oxygen is released to tissues
-pH is down, DPG is up, and temp is up
What are the characteristics of Right Shift in the oxygen-hemoglobin dissociation curve?
-hemoglobin has a high affinity to oxygen, so it doesn't release O2 to the tissues
-pH is up, DPG is down, and temp is down
What are the characteristics of Left Shift in the oxygen-hemoglobin dissociation curve?
-the oxygen carrying capacity of blood
-average male percentage range: 43-49%
-average female percentage range: 37-43%
What is hematocrit and its normal values for males and females?
-iron binds oxygen, and it is transported in hemoglobin in RBCs
-transferrin: transports iron along the body
-ferritin: stores iron along the body
What is the function of iron in blood, the 2 proteins associated with it, and their functions?
-around 120 day lifespan
-shape: biconcave disc
-destroyed in the spleen by macrophages(WBCs)
What are the characteristics of RBCs?
-chains of amino acids, iron, and heme that gets broken down into bilirubin
When RBCs are destroyed in the spleen, what is released?
the process in which our body stops bleeding
What is hemostasis?
-platelet plug(primary): for minor injuries
-clot formation(secondary): for severe injuries, used along with platelet plug
What are the 2 types of hemostasis?
-vessel injury
-vascular spasm: blood vessel constricts to prevent further blood loss
-platelet plug formation: platelets stick together to block the leak
What are the 3 steps in primary hemostasis?
-produced by bone marrow from stem cells
-contains receptors for WWF, TxA2, fibrinogen, collagen, and thrombin
-contains mediators/chemicals such as factors 5 and 8, WWF, TxA2, and fibrinogen
What are the characteristics of platelets?
-arrival of platelets
-binding of platelets to endothelium, and releases collagen and WWF
-recruitment of other platelets(mediators and chemicals)
-platelets cluster
-plug formed
What are the steps for platelet plug formation?
-after the steps of platelet formation occur, fibrin clots wrap around the platelet plug and holds it in place
-after the initial fibrin clot is formed, platelets in the clot contract
-the clot tightens and the 2 damaged vessel ends are pulled together
What are the steps for clot formation?
-intrinsic pathway: blood comes in contact with damaged/exposed endothelium
-extrinsic pathway: the vessel wall is damaged
-common pathway: the result of activating both the intrinsic and extrinsic pathways only because of a severe injury
What are the 3 pathways of coagulation cascade and how are they activated?
intrinsic pathway: 12, 11, 9
extrinsic pathway: 7
common pathway: 10, 2, 13, 1
What factors are part of the intrinsic pathway, extrinsic pathway, and the common pathway?
ABO blood type and Rh blood type
What are the 2 categories of blood types?
-type A
-type B
-type AB
-type O
What are the 4 ABO blood types?
-Rh+
-Rh-
What are the 2 Rh blood types?
antigens and antibodies
What do RBCs have that help differentiate blood types?
type A: A antigens and anti-B antibodies
type B: B antigens and anti-A antibodies
type AB: A and B antigens and no antibodies
type O: no antigens and both anti A and B antibodies
What are the antigens and antibodies for the ABO blood types?
Rh+: Rh antigens and no anti-Rh antibodies
Rh-: no Rh antigens and anti-Rh antibodies
What are the antigens and antibodies for the Rh blood types?
starts the impulse and spreads it to both the atria and this causes both atria to contract. the impulse then travels to the next segment
What is the function of the SA node?
slows the impulses down, giving the ventricles time to fill with blood. the impulse then travels to the next segment
What is the function of the AV node?
receives impulse from the AV node and gives it to the Purjinke fibers
What is the function of the Bundle of Hiss?
receives impulse and spreads it among the ventricles, causing the ventricles to contract
What is the function of the Purjinke fibers?
SA node, AV node, Bundle of Hiss, Purjinke Fibers
What are the 4 parts of the conduction system of the heart in order?
pacemaker potential: slow depolarization because Na+ channels open and K+ channels close
depolarization: action potential reaches threshold due to the influx of CA2+ through CA2+ channels
repolarization: repolarization due to CA2+ closing and K+ channels opening
What are the steps of SA node action potential?
depolarization: opening of fast voltage-gated sodium channels, sodium enters and membrane becomes positive
early repolarization: opening of voltage-gated potassium channels, potassium leaves and membrane becomes negative
plateau: opening of voltage-gated calcium channels, calcium enters and potassium leaves, membrane is stable(plateaus)
repolarization: voltage-gated potassium channels are open, potassium leaves and membrane becomes negative
What are the steps of Myocardial cell action potential?
P wave: atrial depolarization
QRS complex: ventricular depolarization
T wave: ventricular depolarization
What are the segments of an ECG reading, and what do they represent?

the stretching and recoiling of the arteries
What is pulse?
the force of blood against the walls of the arteries
What is blood pressure?
systole: heart contracting and ejecting blood
diastole: heart relaxed and filling with blood
What are the 2 stages of blood pressure and what do they represent?
-mean arterial pressure, and it is the pressure that propels the blood to the tissues
What is MAP and what does it mean?
DP(diastolic pressure) + PP(pulse pressure)/3
(2 x DP) + SP / 3
What are the 2 equations to find MAP?
the difference between the systolic and diastolic pressures
What is pulse pressure?
low pressure: low blood flow, hypoxia, necrosis
high pressure: damages arteries due to excessive force, then organ damage
high pressure again: increased heart work load due to higher pressure can lead to heart attack
What are the results of low blood pressure and high blood pressure?
baroreceptors that are located in the carotid artery, aortic arch, and kidney
What detects blood pressure and where are they located?
the amount of blood ejected by the heart per minute
What is cardiac output(CO)?
the amount of blood ejected by the heart in a cardiac cycle
What is stroke volume(SV)?
low: all of the 5 parameters will increase and blood pressure will increase
high: all of these 5 parameters will decrease and blood pressure will decrease
What will happen to the 5 blood pressure parameters if blood pressure is low/high?
-heart rate(HR)
-blood volume
-stroke volume(SV)
-peripheral resistance(PR)
-blood viscosity
What are the 5 parameters that regulate/maintain blood pressure?
the amount of work placed on the heart due to incoming blood from the venous end
What is preload?
amount of work placed on the heart due to outgoing blood from the arterial end
What is afterload?
the amount of blood left in the chamber at the end of diastole
What is End Diastolic Volume?
the pressure in the chamber at the end of diastole
What is End Diastolic Pressure?
the amount of blood left in the chamber at the end of systole
What is End Systolic Volume?
the pressure in the chamber at the end of systole
What is End Systolic Pressures?
*BP = CO x PR
*CO = HR x SV
*SV = EDV - ESV
What are the equations for BP, CO, and SV?
arterial damage, bleeding profusely due to arterial damage, blood pressure drops and stimulates baroreceptors, baroreceptors stimulate medulla, medulla stimulates SNS, that brings up the 5 parameters of blood pressure, that in turn brings up blood pressure
What occurs in the body due to sudden hypotension(a man got shot)?
once BP drops, baroreceptors get stimulated, baroreceptors stimulate medulla, medulla stimulated SNS, SNS activates, epinephrine and norepinephrine are released, adrenal medulla stimulated, more epi and norepi is released, SA node is stimulated, and heart rate goes back up
What happens to the heart rate parameter once blood pressure drops?
once BP drops, blood volume is increased by activating the renin-angiotensin-aldosterone system that makes more blood, bringing blood volume back up
What happens to the blood volume parameter once blood pressure drops?
once BP drops, baroreceptors get stimulated, baroreceptors stimulate medulla, medulla activates SNS, epi and norepi released, activates all 3 muscle types(smooth, cardiac, skeletal) to contract, bringing up venous return, bringing up EDV, bringing up SV, bringing up CO, bringing up BP
What happens to the stroke volume parameter once blood pressure drops?
once BP drops, baroreceptors get stimulated, baroreceptors stimulate medulla, medulla activates SNS, [epi and norepi are released, alpha receptors in arterial walls are activated, Ca is released and binds to smooth muscles, leads to vasoconstriction, bringing up peripheral resistance, bringing up BP], or [blood viscosity increases, bringing up PR and BP]
What happens to the peripheral resistance parameter once blood pressure drops?
tropomyosin: long fibrous protein, rope shaped
troponin: spherical protein made up of 3 subunits(Tt- troponin-tropomyosin, Ti- troponin-interaction, Tc- troponin-calcium)
What are tropomyosin and troponin?
2 chains of actin subunits twisted into a helix, plus 2 types of regulatory proteins: tropomyosin(strand) and troponin(ball)
What does a thin filament consist of?
troponin and tropomyosin are bound together as one protein that is found around actin molecules
What is the troponin-tropomyosin complex?
many myosin molecules whose heads protrude at opposite ends of the filament
What does a thick filament consist of?
a tail, 2 heads that form as ATP-binding sites, a flexible hinge region
What does a singular myosin molecule consist of?
ATP: low energy configuration because it is harder for myosin to use
ADP and Pi: high energy configuration because myosin can use it easier
What are the 2 forms of ATP that can be attached to a myosin head of a thick filament?
-skeletal muscle activation by nerve
-activation causes Ca levels to increase
-Ca permits contraction and its absence prevents contraction
-no stimulation by nerve equals relaxation(no Ca)
What are the 4 key things that make a skeletal muscle contract and relax?
neuromuscular junction process: the release of a neurotransmitter and innervation of the muscles
excitation contraction coupling: the release of calcium and cross bridge formation
sliding filament theory: contraction(when actual contraction occurs)
What are the 3 processes involved in skeletal muscle contraction?
-arrival of action potential
-opening of voltage-gated calcium channel
-entry of calcium
-exocytosis of neurotransmitter
-diffusion of the neurotransmitter across the neuromuscular junction
-binding of the neurotransmitter to the receptors on the postsynaptic membrane
What are the steps of a neuromuscular junction/synaptic transmission?
-fights off infection
-protects us against cancers and damaged cells
What are the functions of the immune cells?
it uses antigens, molecules that are specific to that cell, and recognizes that it is part of self
How does the immune system distinguish "self" from "non-self"?
-cytokines: chemicals released by the WBCs
-lymphoid tissue
What is part of the immune system, besides WBCs?
Primary organs: red bone marrow, thymus
-function: production and maturation
Secondary organs: lymph nodes, spleen, tonsils, GALT(gut associated lymphoid tissue)
-function: maintain mature WBCs that are ready to attack
What are the primary and second organs of the immune system and their function?
chemicals released by the WBCs that affect growth and activity of other WBCs
What are cytokines?
to defend us against microbes and diseases due to abnormal cells
What is the function of WBCs?
rare, blue-colored granules that contain histamine and heparin, in charge of allergic reactions and protects against parasites
What are the characteristics of basophils?
blue-colored granules, in charge of allergic reactions and protects against parasites, their chemicals are toxic to other cells
What are the characteristics of eosinophils?
non-stained granules, the most abundant leukocyte, the first to combat infection, protect against bacteria
What are the characteristics of neutrophils?
monocyte: found in blood, and once it enters a tissue, it becomes an "antigen-presenting cell"
macrophage: a phagocyte that ingests foreign pathogens
What are the characteristics of monocytes and macrophages?