2- Contractility
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
33 Terms
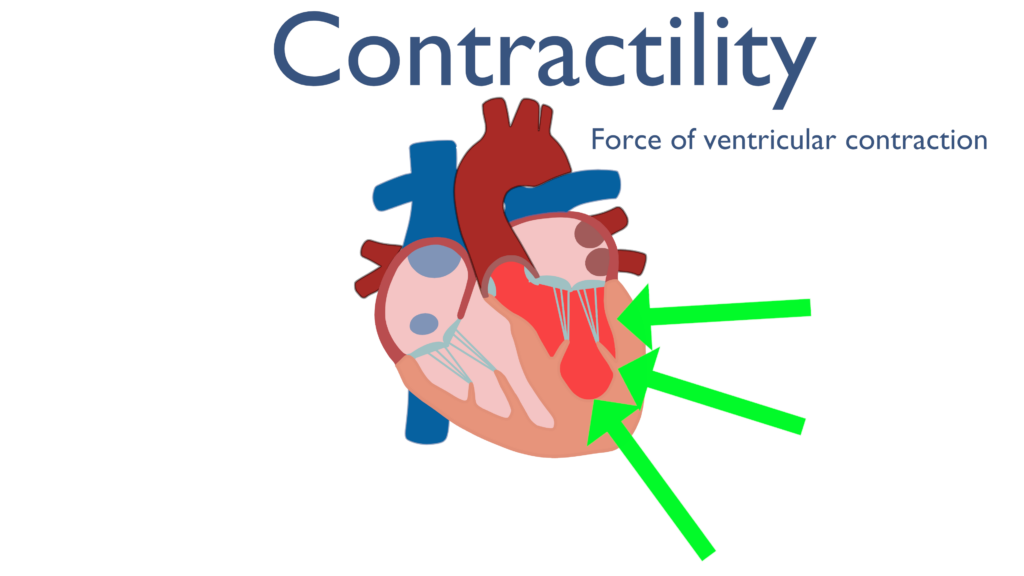
What is contractility?
The cardiac muscle's ability to contract. The factors that affect contractility are called inotropic factors.
What are the two types of cardiac muscle fibers?
Contractile fibers (99%): They form the atrial and ventricular walls and are responsible for pumping blood.
Autorhythmic fibers (1%): They form the heart's conducting system and are specialized for initiating and conducting impulses.
Why is the cardiac muscle considered a "functional syncytium"?
Because the muscle fibers are connected by gap junctions that allow for the rapid spread of excitation waves, making the heart behave as a single unit. It also obeys the all-or-none law.
What is the mechanism of cardiac muscle contraction?
An action potential spreads along the T-tubules.
Activation of DHP receptors causes an influx of extracellular calcium (
Ca++).
This small influx stimulates the release of a larger amount of
Ca++ from the sarcoplasmic reticulum (SR) through ryanodine receptors, a process known as Calcium-Induced Calcium Release (CICR).
Ca++ binds to troponin C, which causes a conformational change in the troponin-tropomyosin complex, uncovering the myosin-binding sites on actin.
Cross-bridges form, causing the actin filaments to slide over the myosin filaments ( systole).
The force of contraction is directly proportional to the amount of cytosolic Ca++.
How does cardiac muscle relaxation occur?
Ca++ is pumped back into the SR by a calcium pump.
Ca++ is also extruded from the cell by a membrane calcium pump and a sodium-calcium exchanger.
Ca++ is released from troponin C.
Tropomyosin moves back to cover the active sites on actin.
The interaction between actin and myosin ceases ( diastole).
This is an active process that requires energy
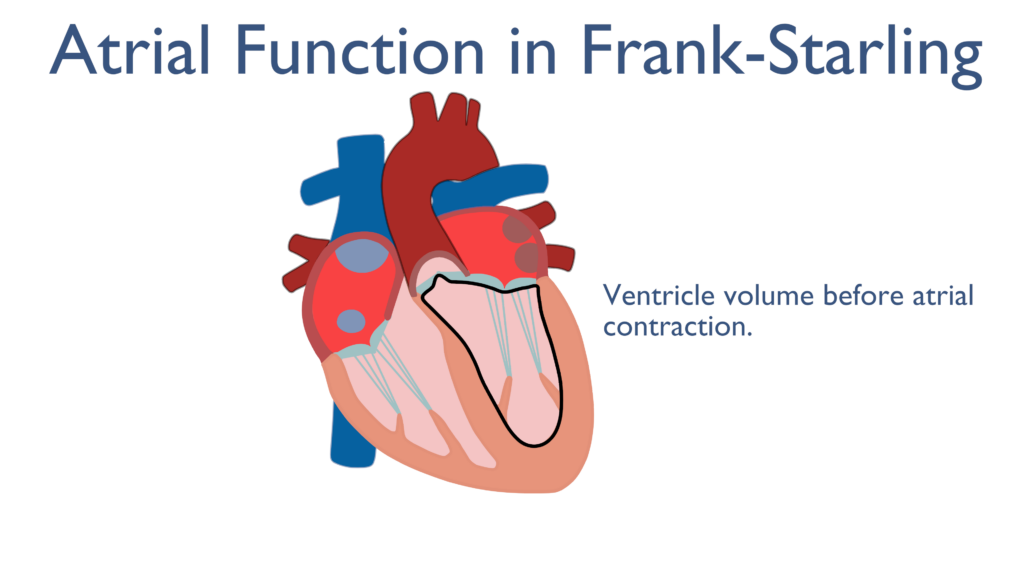
What is the Frank-Starling Law?
Within physiological limits, the force of myocardial contraction is directly proportional to the initial length of the cardiac muscle fibers (preload or End-Diastolic Volume, EDV).
What are the main factors that affect contractility?
Mechanical Factors: Preload (direct relationship) , Afterload (inverse relationship).
Cardiac (Intrinsic) Factors: Myocardial mass and Heart rate.
Extracardiac (Extrinsic) Factors: Nervous factors (e.g., sympathetic stimulation) , Physical factors (e.g., temperature) , and Chemical factors (e.g., hormones, blood gases, ions, drugs).
Inotropic factors
are substances that affect contractility. Positive inotropic factors increase it, while negative inotropic factors decrease it.
How are cardiac muscle fibers structured?
They form a branching network. Each fiber is a distinct unit enclosed by a sarcolemma (cell membrane), meaning there is no protoplasmic continuity between them.
What are intercalated discs?
These are specialized cell junctions that connect individual cardiac muscle cells.
They contain two types of junctions?
Tight junctions: Provide a strong mechanical connection, allowing the pull of one fiber to be transmitted to the next. This creates a mechanical syncytium.
Gap junctions: These are permeable channels that allow ions to diffuse freely between cells. This provides low-resistance bridges for electrical signals, creating an electrical syncytium.
Is the heart a true syncytium?
No, because individual fibers are separated by distinct membranes and lack protoplasmic continuity.
Yes, it acts as a functional syncytium because the presence of gap junctions allows it to function as a single unit, obeying the all-or-none law. The atria and ventricles each form a separate functional syncytium.
What's the key difference between cardiac and skeletal muscle contraction?
Skeletal muscle contraction relies almost entirely on Ca++ released from its extensive sarcoplasmic reticulum.
Cardiac muscle contraction is highly dependent on both extracellular Ca++ influx (via DHP receptors) and the subsequent release of Ca++ from the sarcoplasmic reticulum (via CICR). The force of cardiac contraction is directly proportional to the amount of intracellular Ca++.
What mechanical factors affect contractility?
Preload: The load on the muscle before it contracts. In the heart, this is the End-Diastolic Volume (EDV) or pressure (EDP). A greater preload leads to a stronger contraction. This is the basis of the Frank-Starling Law.
Afterload: The load the muscle must overcome to contract. In the heart, this is the aortic pressure and blood viscosity. An increased afterload decreases the velocity and force of contraction.
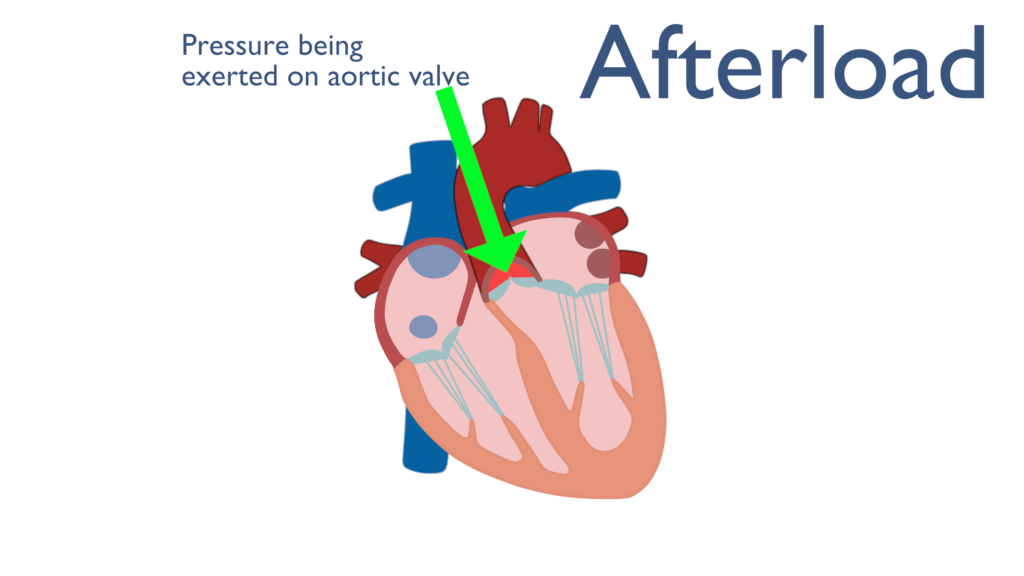
Afterload:
The load the muscle must overcome to contract. In the heart, this is the aortic pressure and blood viscosity. An increased afterload decreases the velocity and force of contraction.
Preload:
The load on the muscle before it contracts. In the heart, this is the End-Diastolic Volume (EDV) or pressure (EDP). A greater preload leads to a stronger contraction. This is the basis of the Frank-Starling Law.
What intrinsic (cardiac) factors affect contractility?
Myocardial mass: Loss of muscle tissue (e.g., from ischemia) decreases the force of contraction.
Heart rate: An increase in heart rate (tachycardia) can increase contractility due to an accumulation of intracellular calcium.
Inotropic state: Determined by the amount of calcium available to the contractile proteins.
Myocardial mass:
Loss of muscle tissue (e.g., from ischemia) decreases the force of contraction.
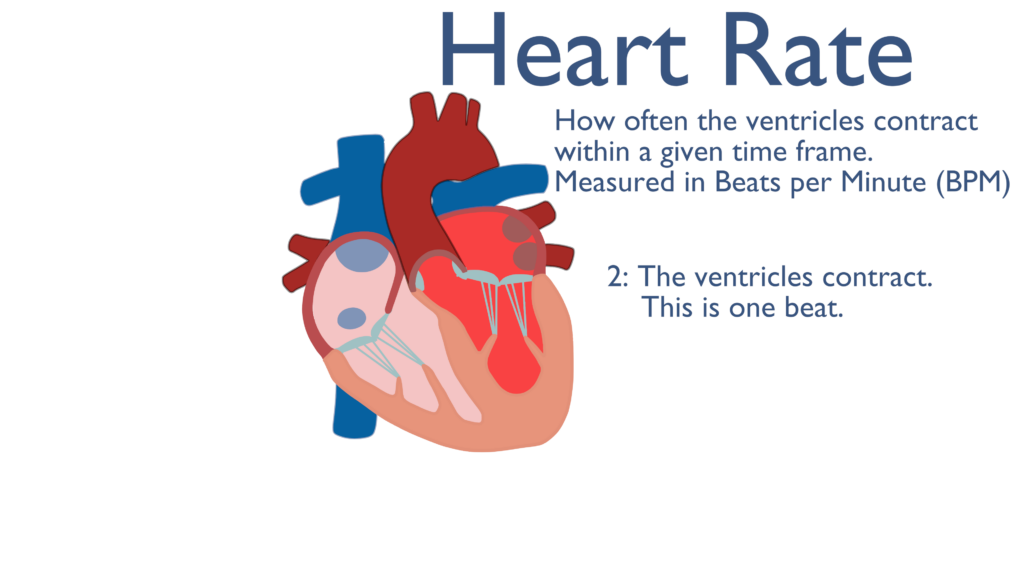
Heart rate:
An increase in heart rate (tachycardia) can increase contractility due to an accumulation of intracellular calcium.
Inotropic state:
Determined by the amount of calcium available to the contractile proteins.
What extrinsic (extra-cardiac) factors affect contractility?
Nervous factors:
Sympathetic stimulation: Increases contractility (positive inotropic effect) by increasing calcium influx.
Vagal stimulation: Decreases contractility (negative inotropic effect), primarily in the atria.
Physical factors:
Moderate temperature increase: Increases contractility.
Excessive temperature increase (fever): Decreases contractility due to metabolic substrate exhaustion.
Chemical factors:
Hormones: Catecholamines (adrenaline, noradrenaline) and thyroid hormones have a positive inotropic effect.
Blood gases: Moderate hypoxia and hypercapnia can increase contractility, while severe hypoxia has a negative effect.
Inorganic ions:
Low Na+ and low K+ increase contractility.
High K+ decreases contractility and can stop the heart in diastole.
High Ca++ increases contractility and can stop the heart in systole (Ca++ rigor).
pH: Acidosis (high H+) decreases contractility; alkalosis (low H+) increases it.
Drugs:
Positive inotropic drugs: Cardiac glycosides (e.g., digitalis).
Negative inotropic drugs: Quinidine, barbiturates, calcium channel blockers.
Toxins: Snake venoms & toxins of diphtheria → -ve (direct).
Nervous factors:
Sympathetic stimulation: Increases contractility (positive inotropic effect) by increasing calcium influx.
Vagal stimulation: Decreases contractility (negative inotropic effect), primarily in the atria.
Physical factors:
Moderate temperature increase: Increases contractility.
Excessive temperature increase (fever): Decreases contractility due to metabolic substrate exhaustion.
Chemical factors:
Hormones: Catecholamines (adrenaline, noradrenaline) and thyroid hormones have a positive inotropic effect.
Blood gases: Moderate hypoxia and hypercapnia can increase contractility, while severe hypoxia has a negative effect.
Inorganic ions:
Low Na+ and low K+ increase contractility.
High K+ decreases contractility and can stop the heart in diastole.
High Ca++ increases contractility and can stop the heart in systole (Ca++ rigor).
pH:
Acidosis (high H+) decreases contractility; alkalosis (low H+) increases it.
Drugs:
Positive inotropic drugs: Cardiac glycosides (e.g., digitalis).
Negative inotropic drugs: Quinidine, barbiturates, calcium channel blockers.
Toxins:
Snake venoms & toxins of diphtheria → -ve (direct).
-Afterload (inverse relashionship)
It is the load that the muscle fibers faces when it begins to contract. Afterload= aortic pressure,arterial wall rigidity, blood viscosity. Change in the afterload → affects mainly the velocity of shortening of cardiac (inversely).
Significance:
It is an intrinsic mechanism that allows heterometric (change in length) autoregulation of myocardial contractility,
in:
1-Normal heart: Match the ventricular output to changes in the VR
2-Increase aortic pressure: → SV of LV → EDV of next beat → forceful contraction.
3-In Denervated hearts (transplanted hearts): main mechanism that adjusts the pumping capacity of the heart.
4-Failing heart: weak ventricularcontraction→ EDV → myocardial contractility.
EDV= 130 ml
(volume of blood in ventricle at end of diastole.
ESV= 55 ml
(volume of blood in ventricle at end ofsystole).
SV= 75 ml
= EDV – nextESV