8, 10 Peds Endocrinology (and lots of diabetes review, plus a tiny bit of neonate/breastfeeding stuff)
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
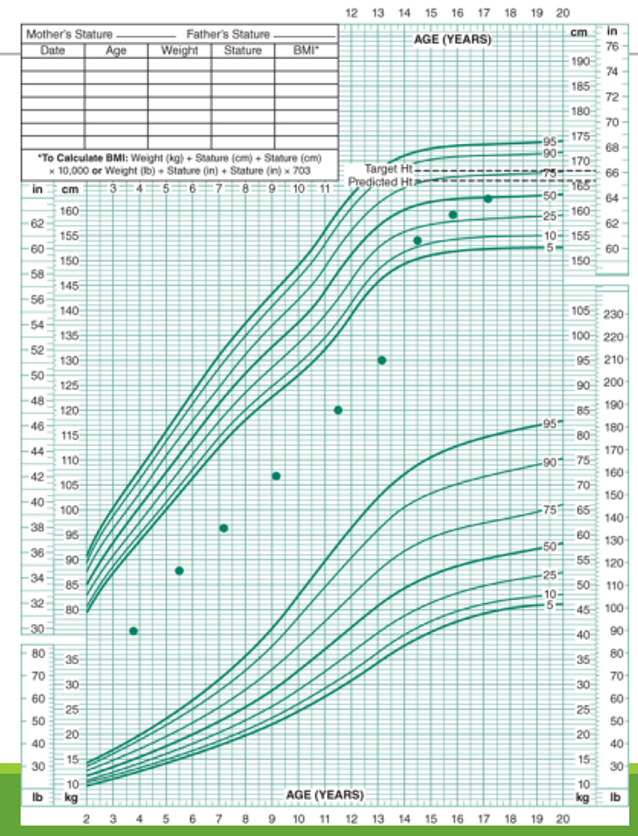
What type of growth condition do you suspect for this growth curve?
Constitutional Growth Delay (Late Bloomer)
What lab do we use as a proxy to estimate growth hormone secretion? Why?
Insulin-like Growth Factor-1 (IGF-1) is a good estimate, as GH stimulates its release; random samples of GH are of no benefit because secretion of GH is pulsatile
What is the difference between somatotropin and somatostatin? What are they (or their analogues) used to treat, respectively?
somatotropin is recombinant GH, and somatostatin BLOCKS GH release
somatropin - used to treat growth hormone deficiency
somatostatin analogue, octreotide - used to treat acromegaly and gigantism
What is octreotide?
somatoSTATin analogue, used to treat GH excess (follwing surgical removal of pituitary adenoma)
What usually causes GH excess?
pituitary adenoma secreting excess GH; treatment of GH excess includes excision followed by treatment with octreotide (somatostatin analogue)
BMI ___-____% = overweight
BMI ___ % = obese
- BMI 85-95% percentile for age and gender assigned at birth --- overweight
- BMI > 95% --- obese
How would you expect C-peptide levels in Type 2 Diabetes to be different from C-peptide levels in Type 1 Diabetes?
C peptide in T2DM - high or normal (beta cells are overworking themselves; making too much insulin to make up for insulin resistance; too much glucose in blood. although chronic T2DM can lead to beta cell burnout, causing low C peptide; you would probably see this in T2DM patients who require insulin)
C peptide in T1DM - low (beta cell burnout/death; beta cells quit, they’re done with this shit)
What age is the peak onset for type 1 diabetes?
10-12 yo; most common in people less than 20 yo
True or False: 80% of Diabetes 1 cases occur in people with a FH of DM type 1.
False; Actually, 80% of cases occur in persons WITHOUT a FH of DM
Name three diagnostic criteria for diabetes diagnosis.
hyperglycemia symptoms and random venous plasma glucose > 200 mg/dL
fasting plasma glucose > 126 mg/dL
A1C > 6.5%
What is the A1C goal for children with diabetes?
A1C <7%
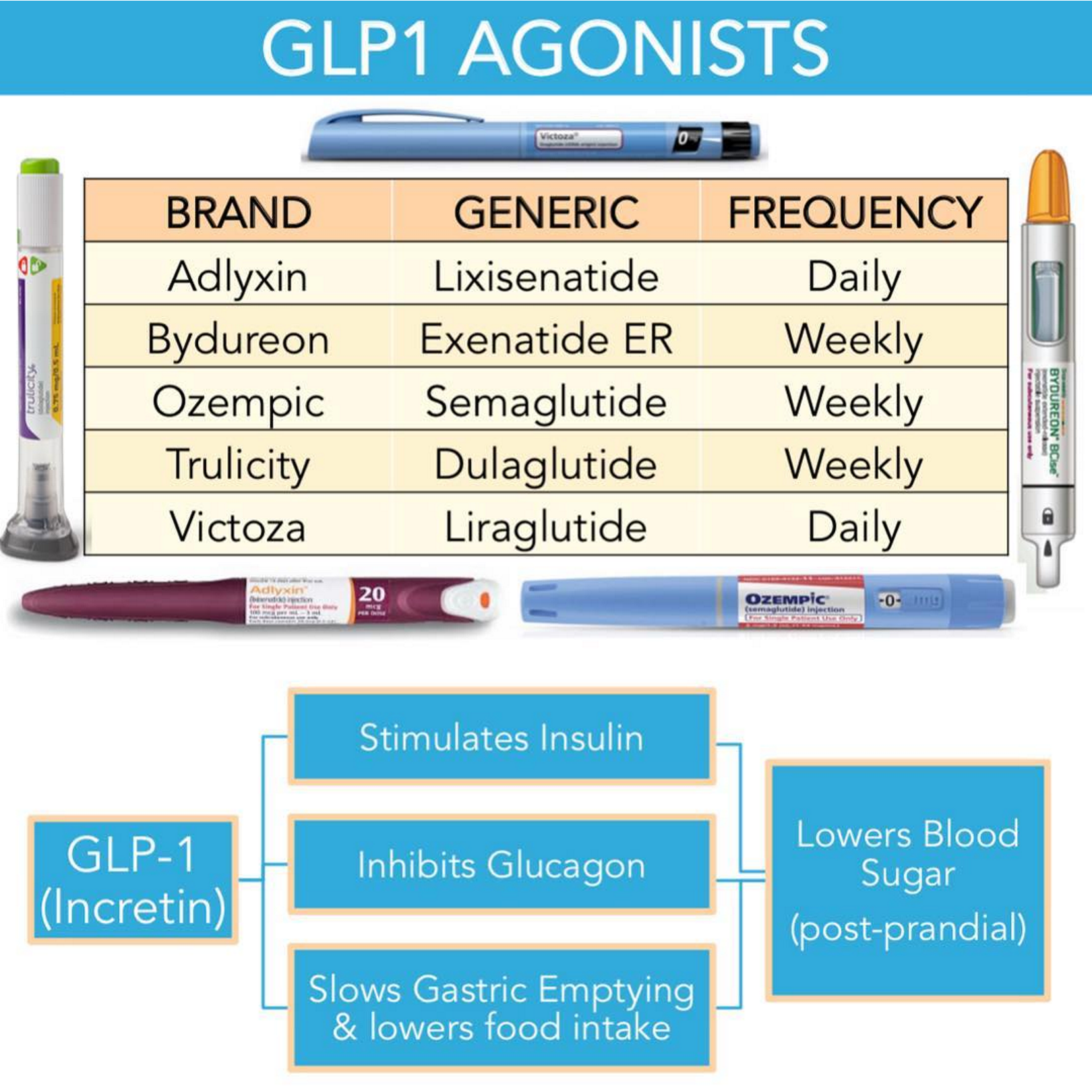
Metformin is the initial pharmacotherapy for DM in children. Name three other pharmacologic treatments for children.
GLP-1 agonists including: Liraglutide (Victoza) SQ daily, extended release Exenatide (Bydureon) SQ weekly, and Dulaglutide (Trulicity) SQ daily
know the three above… the chart isn’t specific to children
insulin therapy indicated when C peptide is low
In Type 2 DM, when should insulin be considered?
When C peptide is low (this is a measure of beta cell function)
True or False - First line treatment for DM in kiddos is metformin
False- although this is the first line pharmacotherapy for DM in kiddos, lifestyle modification should be attempted first
islet cell autoantibodies destroy what types of cells?
Islet cells, typically Beta cells (which are responsible for producing insulin); islet cell autoantibodies destroy beta cells leading to T1DM
What point of care test should be done in children presenting with symptoms of appendicitis or gastroenteritis (such as abdominal pain, nausea, vomiting) in order to rule out a serious endocrine problem?
finger stick blood glucose to rule out DKA
other ssx include Kussmaul respirations (SOB) and fruity breath; tachycardia, tachypnea, dry mouth, flushed face, sleepiness
Why is a heavy diaper in a dehydrated child without diarrhea a red flag?
this is concerning for polyuria, a common symptom of DKA
… CHECK BLOOD GLUCOSE
get serum ketones if BG over 200
If blood glucose is > _____, you should check serum ketones to test for DKA
if blood glucose >200
What is the first line treatment for hypertension?
ACEi (-pril)
note: ARBs are -sartans
When should statins be prescribed in children?
When LDL is > ___ mg/dL
Statins and Lifestyle LDL >160mg/dL
True or False - A kiddo with LDL of 140 should be treated with statins.
false
Statins and Lifestyle LDL >160mg/dL
If LDL is 130-159 mg/dL lifestyle only
Goal LDL <100 mg/dL, HDL >35 mg/dL
Goal triglycerides <150 mg/dL
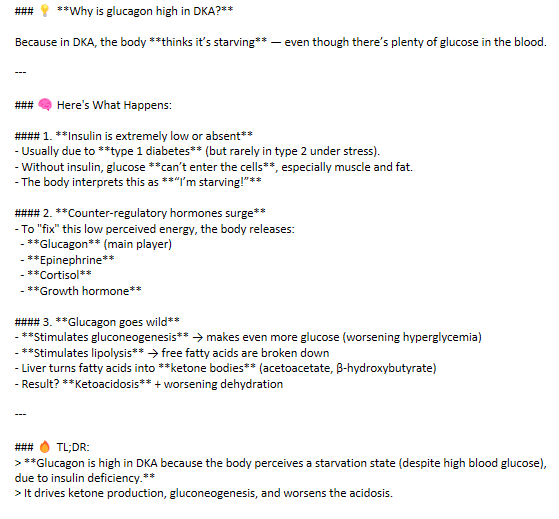
Why do we see excess glucagon, a hormone produced by the pancreas that raises blood sugar levels by triggering the liver to release stored glucose (glycogen) into the bloodstream, in DKA?
🔥 TL;DR:
> Glucagon is high in DKA because the body perceives a starvation state (despite high blood glucose), due to insulin deficiency.
> It drives ketone production, gluconeogenesis, and worsens the acidosis.
more info…
Even though people with DKA have hyperglycemia, the glucose isn’t getting into the cells; this causes a signaling pathways in which glucagon is released in order to break down glycogen stores and produce glucose for the “hungry” cells. In the process, lipolysis occurs and free fatty acids are broken down; the liver turns these into ketone bodies, leading to ketoacidosis and worsening dehydration.
This creates a vicious cycle, worsening the hyperglycemia, without providing a way for the hungry cells to use up the glucose.
This is why patients in DKA need a regular insulin IV drip, to allow the glucose to be used up as fuel. They should be closely monitored, treated with fluids, and they should be monitored for metabolic acidosis. Once acidosis has resolved, BG is controlled, and patient is taking food by mouth, they can be released.
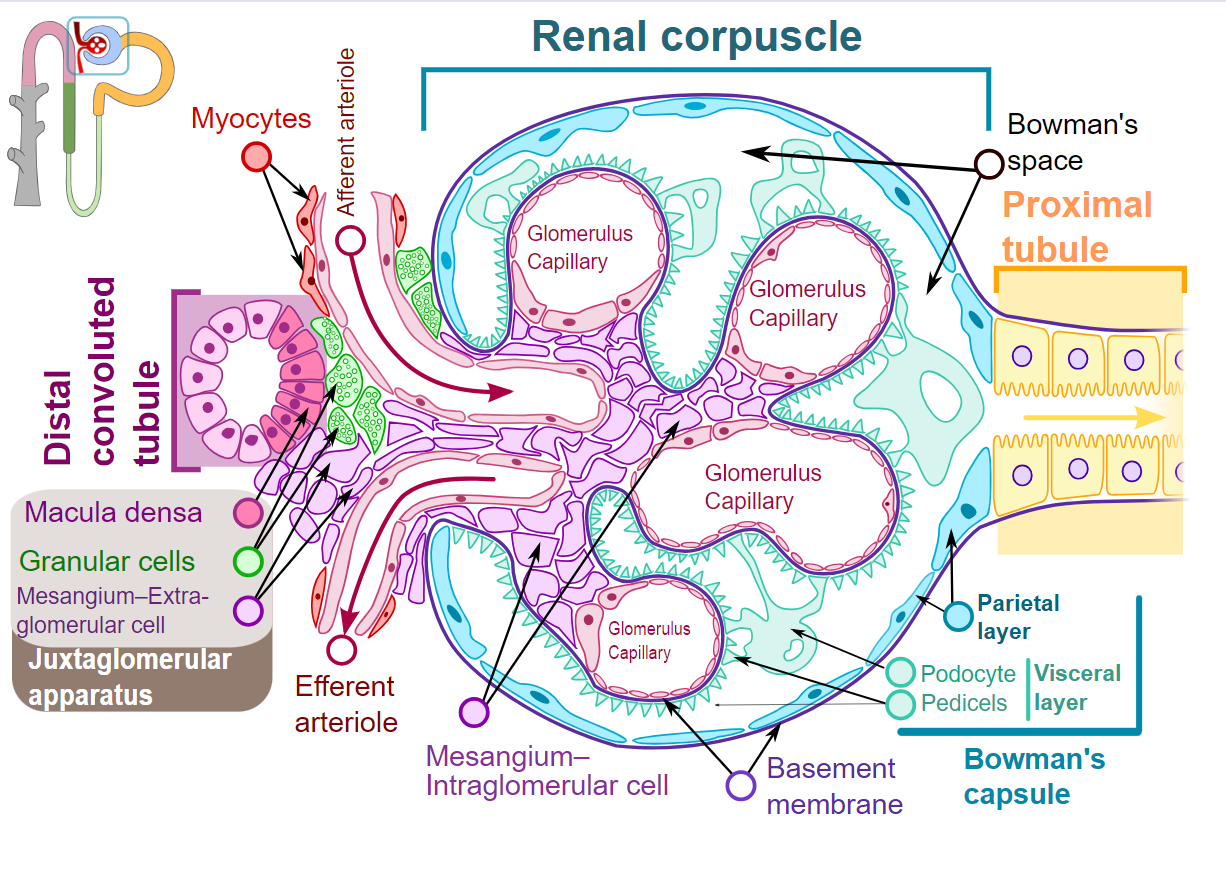
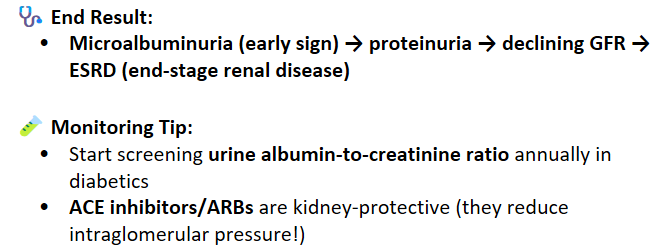
Explain how diabetes can lead to diabetic nephropathy
Hyperglycemia means that more glucose is filtered by the glomerulus
- proximal tubules reabsorb more glucose and sodium, reducing sodium delivery to macula densa (the cells that sense flow); → tricks the macula densa into thinking the filtration is too low → afferent arteriole dilates, increasing glomerular pressure, and leading to hyperfiltrationChronic hyperglycemia → formation of advanced glycation end-products (AGEs) which damage:
mesangial cells, leading to expansion of mesangial cells
glomerular basement membrane, leading to thickening and scarring
end result: leakier glomeruli → albumin leaks out, leading to albuminuria
Podocyte injury - high glucose leads to podocyte apoptosis and detachment, which leads to increased proteinuria, esp albuminuria
Glomerulosclerosis - all of the above lead to progressive scarring and decreased filtration
tubulointerstitial fibrosis - chronic protein leakage + inflammation → damage to tubules and interstitium → loss of nephron function over time
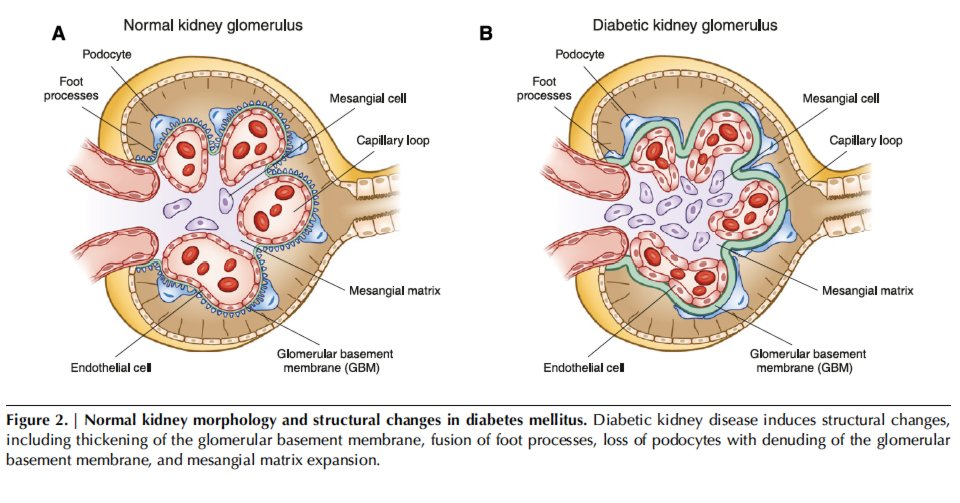
What is the earliest sign of diabetic nephropathy?
microalbuminuria
___-_____ nodules are the hallmark lesions seen in advanced diabetic nephropathy
Kimmelstiel-Wilson nodules
note… this isn’t for Peds I’m just putting this in here as a review :)
What is cretinism? What would you expect labs to look like? What is the treatment?
congenital hypothyroidism
TSH high, T4 low
Levothyroxine (10-15 mcg/kg/day)
Why should you check for Graves antibodies in a pregnant woman who has a history of thyroidectomy (or Radioactive Iodine Ablation)?
Even though she no longer has her thyroid (or an active thyroid), she may still have the TSI (thyroid stimulating immunoglobulins) antibodies from Graves- which can attack the fetus’s thyroid gland and lead to congenital hyperthyroidism in her child (or neonatal thyrotoxicosis)
True or False - The MCC of goiter and acquired hypothyroidisim in childhood is Hashimoto’s disease, otherwise known as Chronic Lymphocytic Thyroiditis.
True
What medications are used to treat hyperthyroidism in children?
methimazole (suppresses thyroid function) and beta blockers (atenolol) for nervousness, tachycardia
rarely is radioactive iodine or surgical treatment used in pediatric patients, due to complications (and RAI can increase risk of future thyroid cancer)
True or False - Congenital Hyperthyroidism typically resolves in 3 years as maternal antibodies decline.
False - it typically resolves in only 1-3 months as maternal ab decline
A 7-year-old boy is brought to the clinic by his parents because of fatigue, constipation, and abdominal pain for the past week. His teachers have also noticed that he seems lethargic and is having trouble concentrating in class. On examination, he is mildly dehydrated and has diffuse abdominal tenderness.
Lab studies reveal:
Calcium: 12.5 mg/dL (normal: 8.5–10.5)
Phosphate: 2.2 mg/dL (low)
PTH: 150 pg/mL (normal: 10–65)
Vitamin D: normal
Creatinine: normal
An ultrasound of the neck reveals a solitary hypoechoic mass near the inferior pole of the right thyroid lobe.
Which of the following best explains this patient’s hypercalcemia? As a bonus (not multiple choice), is this PTH-dependent or independent?
A. Excessive intake of calcium and vitamin D
B. Parathyroid adenoma
C. Williams syndrome
D. Malignancy-associated PTHrP production
E. Immobilization
✅Correct Answer: B. Parathyroid adenoma
✨Explanation: 🧪 Recognizing Hypercalcemia:
Symptoms: "Stones, bones, groans, thrones, and psychiatric overtones" → This kid has abdominal pain, constipation, fatigue, and difficulty concentrating.
Lab: Elevated calcium, low phosphate, high PTH.
🔍 Identifying the Cause:
High calcium + high PTH = PTH-dependent hypercalcemia
The neck mass suggests a parathyroid adenoma, which is the most common cause of primary hyperparathyroidism, even in children (though rare).
💡 PTH Status:
This is a PTH-dependent hypercalcemia.
❌Incorrect Answer Explanations:
A. Excessive intake of calcium and vitamin D → Would suppress PTH (so this would be PTH-independent).
C. Williams syndrome → Can cause hypercalcemia in infants via increased sensitivity to vitamin D, but not with elevated PTH.
D. Malignancy-associated PTHrP → Also PTH-independent, and true PTH would be low.
E. Immobilization → Seen in adolescents with high bone turnover (e.g., cerebral palsy); also PTH-independent.
The following conditions can lead to PTH-______ hypercalcemia:
MEN 1&2
FHH - familial hypocalciuric hypercalcemia
tertiary hyperparathyroidism due to renal failure
Explain why.
The following conditions can lead to PTH-dependent hypercalcemia:
MEN 1&2
FHH - familial hypocalciuric hypercalcemia
tertiary hyperparathyroidism due to renal failure
Primary Hyperparathyroidism:
Most common in adults, but can occur in kids.
Causes: Parathyroid adenoma, hyperplasia.
Syndromic forms:
MEN 1 (pituitary, pancreas, parathyroid)
MEN 2A (medullary thyroid cancer, pheochromocytoma, parathyroid hyperplasia)
Familial Hypocalciuric Hypercalcemia (FHH):
Autosomal dominant.
Mild hypercalcemia, often asymptomatic.
Labs: High PTH, low urinary calcium (low urine Ca/Cr ratio).
Important to differentiate from primary hyperparathyroidism to avoid unnecessary surgery.
Tertiary Hyperparathyroidism (chronic renal failure):
Chronic kidney disease → long-standing secondary hyperparathyroidism.
Eventually, parathyroid glands become autonomous → high PTH even when calcium rises.
How many wet diapers per day is normal in the first week of life?
On the first day after birth, expect only 1–2 wet diapers. On days 2–3 of your baby's life, expect 2–4 wet diapers. By day 4, your baby should have 4–6 wet diapers per day. On day 5 and onward, your baby should have 6 or more wet diapers per day.
How many stools is normal per day?
1-4 days (it can take about 24-48 hours for meconium to pass)
How much weight loss is normal in first week of life?
formula fed 3-5%; breast fed 5-7%; LGA may lose more weight
What are two hormones produced by the pituitary gland that are important for lactation?
prolactin (anterior pituitary gland) and oxytocin (posterior pituitary gland)
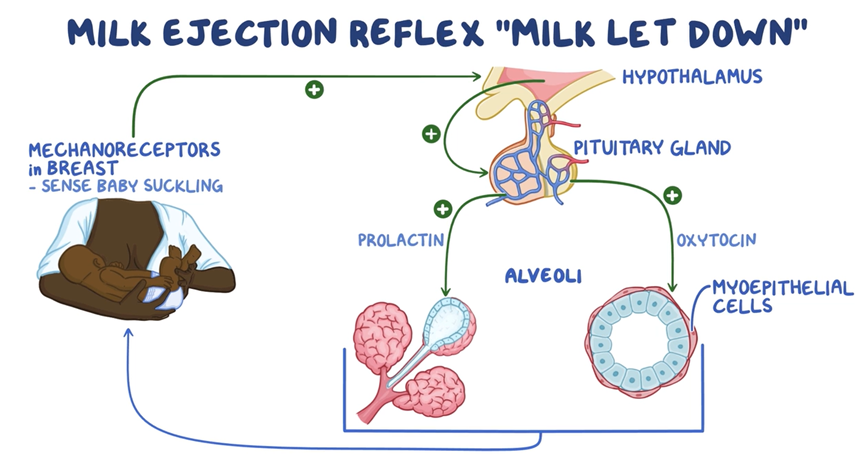
How long does it take for transitional milk to come in?
2-5 days after birth
When should breast feeding begin?
within an hour after birth; don’t delay, this can delay transitional milk from coming in