***async lecture: Top-Down Approach to Evaluation and Devising Goals in the School System
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
school-based vs medical based therapy
school based therapy targets
function- primary concern (we want to facilitate participation in a while, as it related to school-based tasks (e.g., tying shoe-laces, socializing in class)
—> then, look at social limitations (role performance-student role)
medical or clinical based therapy targets
pathology- primary condition
—> then, look at impairments
—> —> lasly, how is function impacted
conceptual framework for school based evaluations
***top-down evaluation
top-down approach
highlights the significance of occupational performance and participation
occupation-centered and begins with understanding the “child’s overall pattern of occupational engagement in relation to a particular context of importance”
begins at the level of participation and performance areas (occupations!)
begins with gathering information about what the child needs and wants to do across a variety of occupational performance areas and settings, often using occupational profile information given by the child, their parents, or some other provider (e.g., teacher) who knows the child
—> focus on the critical occupations that were identified through the occupational profile and the environments in which these occupations take place; it is very important to attend to the environment in this early step of evaluation, as certain environments (e.g,. the school, daycare center, local park) may inherently be connected to expectations for performance
e.g., may be expected that a child eats in his highchair at daycare, but the child may be allowed to eat while standing or walking at home
—>—> and if limitations are identified, then progresses to the level of performance skills such as sensorimotor, cognitive, psychosocial and environmental factors are identified
OT identifies which aspects of occupational performance most inhibit participation; OT may do this using a standardized assessment tool
e.g., using the School Function Assessment, the Assessment of Motor and Process Skills, or observation using the performance skills outlined in the OTPF
OT may identify a pattern of limitations that suggests an underlying performance skill deficit that could be the result of 1 or more causes, such as sensory processing differences, reduced strength, reduced coordination, or delayed development
new trends in evaluation OTPF (4th ed.)
more attention is being given to environment and contextual factors
i.e., barriers in the environment and context
ecological perspective considers the person and environment as 1 unit
i.e., how is the person influenced by its environment?
in order to assess function, 1 must look at the context in which it occurs, for instance, home vs school
physical, temporal, and sociocultural features of the environment are considered
occupation-centered assessment looks at the future needs of the child
i.e., how is this skill going to carry the child through life?
factors that influence ***evaluation
client needs and role
e.g., role as a student in the classroom
reason for referral
reason for referral may also impact which assessment tool you use and which clinical reasoning you reference (e.g., if a child is referred bc of sensory issues, you will use a sensory assessment)
press of eligibility for service
skill level of the clinician
may also affect which evaluations and assessment tools we use (i.e., do we feel confident enough doing life-skill assessments on older kids, like high-schoolers?)
***evaluation purposes
the proces of evaluation *allows the therapist to collaborate with the client and family to establish whether there is a need for OT, and if so, to **establish goals, and **determine intervention methods; in addition, ***data from evaluation can serve as a ***foundation for clinical decision making at each stage of the therapeutic process
*establish eligibility
**provide a focus for intervention planning
***provide a baseline to evaluate progress, so you can continue to monitor progress towards goals
in clinical situations, OTs conduct evaluations for the purposes of:
*screening
determine if a child would benefit from a more comprehensive OT evaluation, with data being derived from…
standardized tools,
locally developed checklists,
communication with the child, parents, teachers, or other providers,
and observations
*determining the scope and frequency of OT services
to determine the scope and frequency of intervention, OTs conduct a comprehensive evaluation and collect data from numerous sources (e.g., child, parent, teacher) and with multiple methods (e.g., parent interview, observation of the child in various environments, standardized assessment tools)
how the data is collected and through which mechanisms is often determined, in part, by the practice setting (e.g., OT providing services in an outpatient pediatric clinic may focus evaluation heavily on sensory integration and how these factors influence a child’s occupational performance)
frequency and duration are often determined by the therapist’s experience working with children with similar presentations and developmental trajectories, funding and legal parameters, or other factors associated with the setting (e.g., an OT working in a school setting may typically see a child for an academic year)
**setting goals and developing intervention plans
***documenting progress toward therapy goals
establish a baseline and post-intervention measures associated with the progress made during OT intervention
in many cases, the OT will encourage the child to engage in occupations or perform skills associated with a standardized assessment tool to mark progress
in other cases, parents, teachers, and providers may complete rating checklists or provide other forms of input to share their perspectives related to the child’s progress or how their own stress and quality of life have (or have not) benefited as a result of intervention
comprehensive ***evaluations
eligibility: to establish eligibility for service, should use a standardized and norm-referenced tool to ensure reliable and valid measures; should include in-depth observation of child in natural environment
parent or teacher interview
to understand whether this is typical performance of a child, or whether they are having an off day
best choice: norm-referenced used in combination with criterion-referenced or curriculum-based assessments
norm-reference/standardized test:
compare child to typical age peers
criterion-referenced test:
compare child’s performance as it relates to the setting where you are evaluating them; child is compared to themselves on a certain criteria that is already established by an assessment tool
***evaluation process
referral
gather preliminary data or background info
formulate assessment plan
administer assessment tool
document results
develop meaningful recommendations
examination: body function deficits limiting school function
this includes all the tests and measures taken on a child
e.g., might look at fine motor testing, gross motor testing, sensory profile visual perceptual (TVPS) and visual motor tests (VMI), ROM, MMS
==> all meant to look at the body function deficits a child may have (as it limits to their participation in school)
organized by headings
assessment
interpretation of results
determine the significance of body function limitations
i.e., is this just a mild body function limitation that can be compensated for? or is it severely affecting ADLs?
link body function limitations to functional limitations
e.g., how does a child’s limited ROM —> affect function and the child’s ability to put on a coat?
use of clinical reasoning skills to place value on the data gathered and reported above (impairments)
determine how extensive those performance skills and body function limitations are affecting the child’s overall performance
development of recommendations and ***goals
client factors:
functional limitations
parent/caregiver/teacher priorities
e.g., what concerns them the most?
service delivery model:
direct (1-on-1)
, consult or monitor (giving the teacher or parent some strategies in which they can try out; re-monitor progress)
choosing goals that target occupation based function vs body function limitations
why address functional limitations and social role limitations?
though we assume that pathology and impairments lead to dysfunction and social role limitations, it is important to realize that function can be improved, and roles can be fulfilled without addressing all impairments and despite underlying pathology
occupation-based performance is often complex, and a number of body function limitations can contribute to a limitation in activity performance
goals that are based on body function limitations are too narrow and do not consider the context in which function occurs
devising educationally relevant ***goals
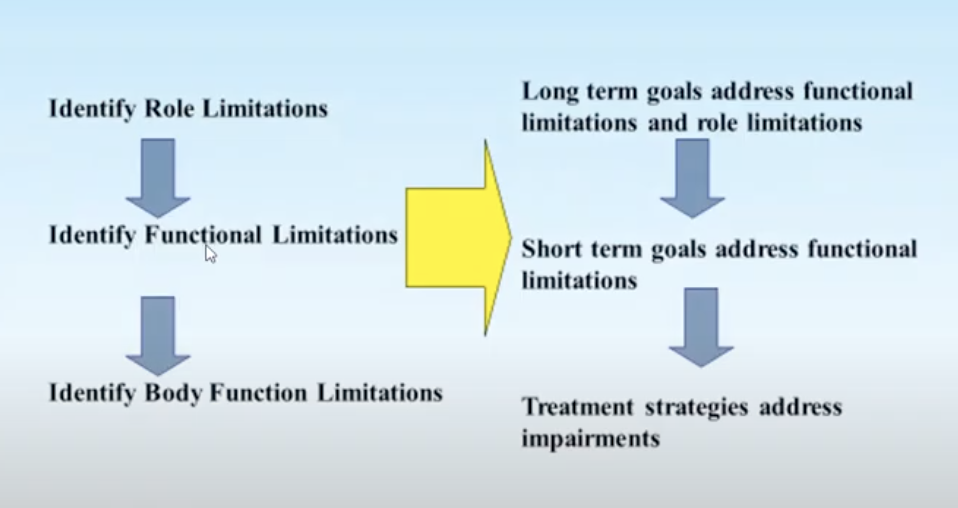
***top-down approach
utilize a top-down approach to goal writing
identify role limitation (occupational lens)
—> identify functional limitations
—> —> identify body function limitations
==> long-term goals address functional limitations and role limitations
—> short-term goals address functional limitations
—> —> treatment strategies address impairments
e.g., functional limitation= child’s inability to grasp a spoon
long-term goal= bob will be able to grasp and bring 10/10 spoonfuls of lunch to his mouth/eat, in order to participate in lunchtime w/ his peers
short-term goal=
bob will be able to grasp his spoon using a cylindrical grasp (positioning)
bob will be able to grasp his spoon using an adapted handle (compensatory)
essential components of a ***goal
***goal writing
there are many acronyms designed to help students and therapists recall what needs to be placed in a goal, i.e., ABCDE, SMART
it is less important to remember the acronym and more important to remember what constitutes a good goal
goal writing
intervention goals should be…
observable
occupation-based
measurable
meaningful to the client constellation
when working with children, intervention goals may be focused on the child’s individual occupational performance and/or their participation during co-occupations
in addition, OT goals should be based on the progress trajectory that the OT predicts, based on knowledge of the child and family, the context or environment, and previous professional experience
OT should also encourage the family to share their priorities; OT then frames these priorities into measurable goals
when child-centered and family-centered goals are ideal, OTs may need to consider other factors, depending on their practice setting, when developing intervention goals
e.g., OTs working in the school setting may be required to align their OT goals with educational standards
goals will be assessed to determine how much progress the child has made in a certain timeframe
OTs may write long-term goals and short-term objectives or benchmarks
specific dates to review progress toward short-term objectives and long-term goals should be established prior to the beginning of the intervention
oftentimes, the goal review period is determined based on the OT’s best guess regarding the rate that which the child will make progress
goal writing’s 3 components:
the person
goals will never be written for actions or target behaviors that the OT will perform (e.g., “the OT will evaluate the need for assistive equipment”); rather, the goals should be written so that the focus is on the person receiving the intervention and the person’s demonstration of certain target behaviors
usually, is the child
in some cases, may focus on enhancing the parent’s skill development, in which the person named in the goal would be the parent
the daily occupation or routine
target behavior is often presented as a verb (e.g., dress, play with, pick up, wash)
target behavior might be based on different performance skills, completing certain tasks associated with an occupation, completing a certain occupation, or completing (or participating in) a daily routine
is the occupation or routine that will be enhanced as a result of OT; specifically, the goal should include language associated with the level of participation or independence that is expected and the quality of the person’s performance
depending on the child’s needs and presentations, goals to improve performance may not be appropriate; it may be more realistic to write goals that are focused on maintaining performance or participation and/or to reduce the speed of functional decline
specific context
ideal content for OT intervention is in the child’s natural contexts and environments (e.g., if OT is writing a goal associated with eating during family mealtimes, the appropriate environment to measure the target behavior is in the family’s home)
when certain skills will be performed
where they will be performed
who will be present when the skill will be performed
e.g.,
presenting concerns
difficulty with handwriting due to delayed visual-motor integration (i.e, inconsistent letter formation)
assessment tool
Beery Test of Visual-Motor Integration
goal areas
improve handwriting and visual-motor integration skills for education
intervention focus
copying shapes and letters with consistency (activities may include: drawing pictures with multiple shapes, making greeting cards, writing thank you notes)
discharge qualifications
improved handwriting (i.e., consistent letter formation)
devising functional ***goals
ABCDE
SMART
A: audience- who
typically, child
e.g., Susie
B: behavior- what
written as a specific action verb
e.g., Susie will grasp a spoon
C: condition- how
making an intervention realistic for the child (make it simple!)
e.g., Susie will grasp a spoon, using a cylindrical grasp
D: degree- how
a type of measure, i.e., within a time, w/ a quantity
e.g., Susie will grasp a spoon, using a cylindrical grasp, 10/10 times
E: explanation- why
why is this goal important? why is it justified?
e.g., Susie will grasp a spoon, using a cylindrical grasp, 10/10 times, to improve participation with peers
S: the significant part/behavior/activity
M: measurement
A: it is achievable (__)
R: relates to __
T: time limit is __
e.g., Sydney is a 5-year-old girl who receives occupational therapy services! due to fine-motor deficits and limited participation in fine-motor activities in the classroom!
goal: Sydney will *cut out basic shapes with scissors **within ¼” of the line consistently ***by the end of the school year
*S: scissors skills are significant at that age
**M: within 1/4" of the line
A: it is achievable (PDMS-2 and HELP)!
R: it relates to her participation in classroom activities!
***T: by the end of the school year
devising measurable ***goals
task completion- number of steps, number of opportunities to perform the task across the school day or week
hard to measure progress without steps outlined
time to complete- absolute or relative
absolute
e.g., a child will do push-ups 5 times in 10 minutes
relative: more related to the context and what is expected of the child in the classroom, or expected when compared to other children w/ similar conditions
e.g., (at school) a child will write 3 ten-word sentences in 10 minutes
this would be required b/c the teacher gives 10 minutes to complete the warm-up assignment
accuracy- deviation from target line
e.g., a child will cut w/ scissors, deviating no more than a quarter inch from the target line
standardized score
***goal writing:
long term objective
john will manage his clothing independently within the classroom environment in order to participate more fully in the student role
who= john
what= manage clothing
how= independently
why= context of school environment and to enhance student role
*we don’t have time/quantity measurements for long-term goals, only short-term ones!
***goal writing:
short-term objective
purpose of short-term objectives is to provide a logical breakdown of long-term goals and to serve as guideposts for measuring progress; are often focused on a collection of different target behaviors or discrete skills leading up to a more functional outcome (e.g., child may have a long-term goal to complete a daily journal activity with the same quality as his peers; the OT may develop a series of short-term goals leading up to successful completion of the journal activity,
e.g.,
(1) select a topic to read about
(2) initiate the writing process without additional teacher prompts
(3) legibly form all letters
(4) check work for quality using a checklist)
(A) *John will **put on his coat ***independently when preparing to go outside or leave school at the end of the day ****5/5 afternoons per week
*A: audience- who = john
**B: behavior- what = put on his coat
***C: condition- how = independently
****D: degree- how = 5/5 afternoons per week
E: explanation- why
(B) *John will **fasten the button on his pants ***after toileting consistently ****in 3/3 opportunities
*A: audience- who = john
**B: behavior- what = fasten the buttons on his pants
***C: condition- how = after toileting
****D: degree- how = in 3/3 opportunities
E: explanation- why
short term ***goal:
body function limitations and strategies
decreased bilateral hand coordination
—> activities to promote coordinated use of 2 hands
decreased pinch strength
—> activities to enhance pinch strength
decreased stereognosis
—> activities that require discrimination of objects between fingertips
impaired sequencing
—> activities that have number steps that need to be completed in sequence
***discharge planning
goal achievement (i.e., a measure of when the child has achieved their goals); Goal Attainment Scale
re-assessment of functional gains
summarize the changes in client’s ability to engage in occupations between the initial evaluation and discontinuation of services and make recommendations as applicable
e.g.,
identify in a summary what you think the child and family will need for their next level of OT services based on the child and family’s needs or the needs of the child in the school and or clinic setting
constraint-induced movement therapy to increase the functioning of his neglected side
what would you recommend for community resources?
adaptive physical/sports community groups (with sports working on upper extremity range of motion and strength, e.g., swimming, wheelchair basketball, wheelchair baseball, etc.)
adaptive community cooking classes
CP community groups for socialization with other families with teens who have CP
what would you recommend for equipment needs or accommodation?
more intuitive medication organizers that are color-coded and labeled with the medication name and days to take
button hooks for dressing
adaptive cooking equipment (e.g., handle grips, cooking materials with thicker and longer handles, food timers for reminders)
what would you recommend for home setup or classroom setup?
wheelchair friendly/accessible pathways and equipment in/into the home/school/classrooms (e.g., ramps, handrails, wide door frames, wide hallways, etc.)
wheelchair eye/reach-level shelves (e.g., reorganize furniture or room structure so that Owen can still reach and see everything he needs to while being in his wheelchair)
working elevators in the buildings
what would you recommend for home or classroom programs that would benefit your child and their family/teachers.
increased time for test-taking at school
parent-teacher check-ins to ensure Owen is keeping up academically, and generally feels supported in his learning environment
summarize your recommendations to present to your supervising OTR, the interprofessional team, and to the family/teacher of the child in the Simucase study.
Based on evaluation information, Owen has met all of his identified goals of improved and increased participation in play, completion of household tasks, mobility in community settings, shoulder range of motion, and semi-independent execution of ADLs with minor to moderate cueing (e.g., in meal preparation, medication management, doing laundry, and dressing).
At home, it is recommended that Owen continue to practice these ADLs and any others important to him, with parents grading the activity to either become more complex or to involve less cueing and/or compensation strategies as Owen improves (e.g., have him prepare a meal with more than 5 steps, have Owen engage in overhead throwing tasks, with reminders for optimal positioning and compensation no more than 25% of the time).
In terms of adaptive changes and technologies, Owen can look into medication organizers that are color-coded and labeled for medication management, and adaptive tools for dressing (e.g., button hooks), and cooking (e.g., handle grips, food timers) activities.
However, outside of the home, it is recommended that Owen continue to work on his short-term memory skills and upper extremity range of motion and strengthening through community cooking and adaptive sports activities, in which Owen will have to practice following the rules of the game while also improving shoulder external rotation.
It is recommended that Owen’s home and school environments should also be evaluated for wheelchair accessibility and working elevators.
Teachers and parents should also be proactive in providing Owen support in terms of his learning and socialization, checking in to make sure he is getting appropriate time to complete his assignments, and encouraging him to attend supportive community outings with peers similar to him.
summary
***top down approach to evaluation
***parallel top-down approach to goal writing
***discharge planning
school based vs medical based practice
***top down approach to evaluation
to complete evaluations, OTs work with children and families to…
develop occupational profiles
administer assessment tools
conduct observations
OTs use clinical reasoning to synthesize evaluation data, which serves as a foundation for goal-setting and intervention planning
OTs use observation, standardized assessments, non-standardized assessments, and interviews to gather data to inform the evaluation and intervention planning
OTs use theories, models, and frames of reference to develop hypotheses based on available data collected during the evaluation phase; they use this knowledge to create intervention plans
***parallel top-down approach to goal writing
goals address the priorities and outcomes of OT intervention; they include…
the person
the daily occupation or routine
and the specific context
goals specify an observable and measurable target behavior, which is often presented as a verb (e.g., dress, play with, pick up, wash)
***discharge planning
long-term and short-term ***goals examples
LTG- *Joshua will *engage in developmentally appropriate play *with peers or play partners for at least *5 minutes, 3 times per week, *with minimal assistance, to *support social interaction and play participation.
STG 1- *Joshua will *engage in reciprocal co-play *through pat-a-cake or peek-a-boo *with a new peer or play partner for at least *2 minutes, 3 times per week, to *support participation in social play.
STG 2- *Joshua will *demonstrate a pincer grasp *using his right hand to pick up at least *7 out of 10 small blocks during play, *with supervision and modeling from a caregiver or sibling, during *3 out of 5 weekly sessions to *support fine motor development and appropriate object manipulation