HISTEM W8 Oral Mucosa and Tongue
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
Describe the Oral mucosa. What are the 3 main types?
Stratified squamous epithelium on top of lamina propria (CT proper/dermis layer)
May be a deeper layer of submucosa present (hypodermis)
3 types:
Masticatory mucosa – keratinized; gingiva & hard palate
Lining mucosa – non-keratinized; cheeks, lips, floor of mouth, soft palate
Specialized mucosa – on tongue; contains taste buds
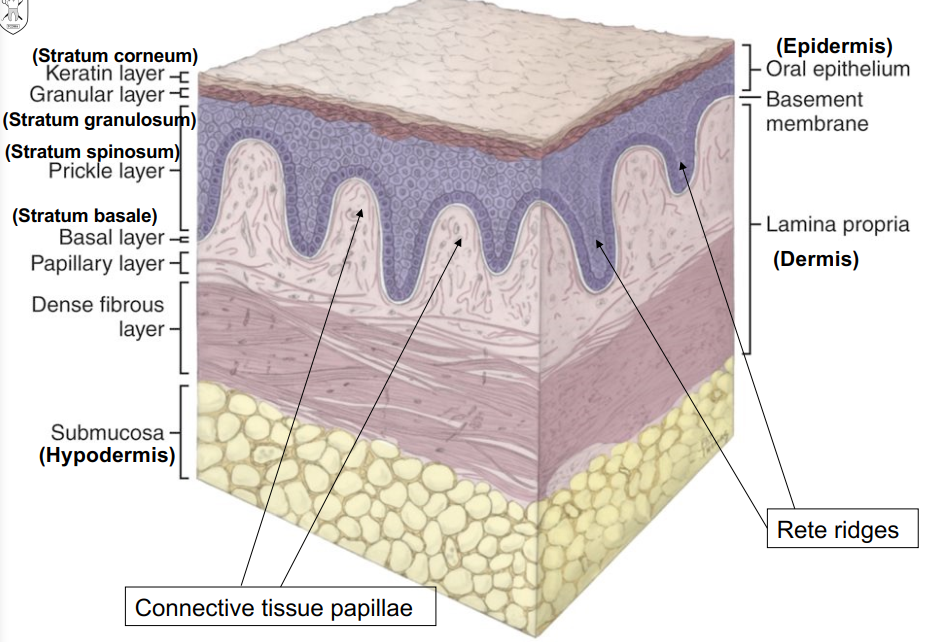
What lies between the epithelium and lamina propria in the oral mucosa?
basement membrane → lamina lucida, lamina densa, reticular lamina
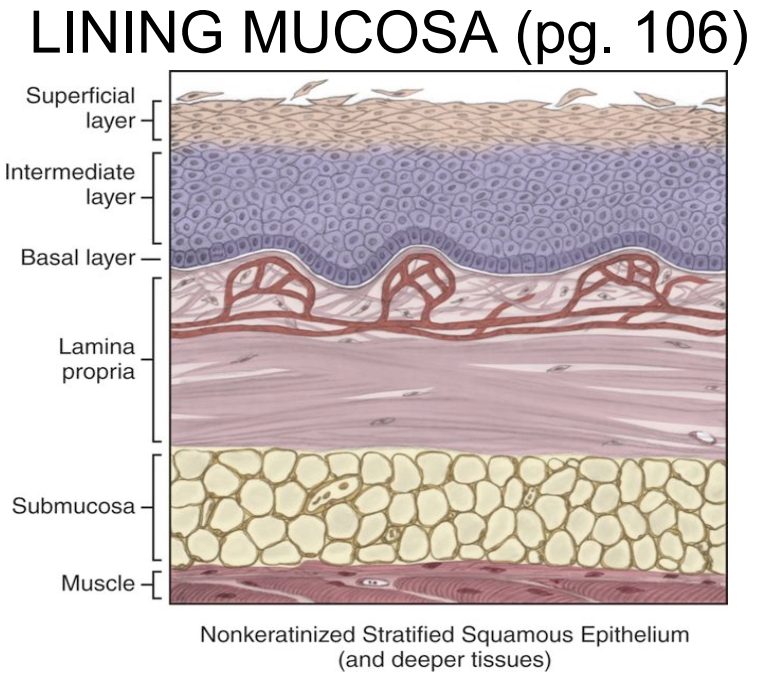
Describe Lining mucosa.
Lining mucosa:
soft, pilable, moist, stretchable, cushioned
NON-KERATINIZED stratified squamous epithelium
Lamina propria is smoother (less rete ridges/CT papillae
contains elastic fibers and submucosa
Where is Lining mucosa located in the oral cavity? (3)
floor of the mouth
buccal, labia, alveolar mucosa, ventral surface of the tongue
soft palate
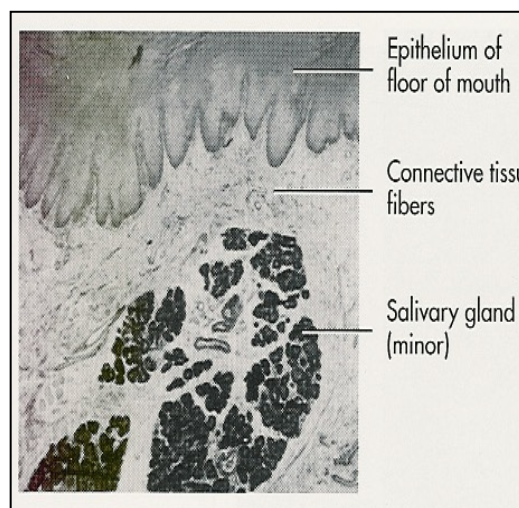
Describe the lining mucosa in the Floor of the Mouth.
non-keratinized, thin
Lamina propria → highly vascularized, not very many rete ridges/CT papillae
Submucosa → loosely attached to bone/muscles; submand. and sublingual salivary glands found here
Describe the lining mucosa in the Cheeks
Non-keratinized
Lamina propria → highly vascular
Submucosa → contains adipose tissue and minor salivary glands
May have Fordyce granules, melanin pigmentation
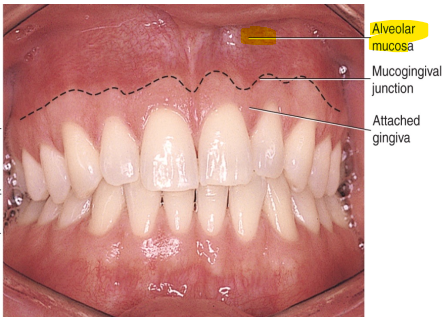
Describe the lining mucosa of Alveolar Mucosa.
Non keratinized
Extremely mobile, lines vestibules the spaces between the lips/cheeks and the teeth/gums.) of the oral cavity
Lamina propria → highly vascularized; lots of elastic fibers
Submucosa → loosely attached for mobility
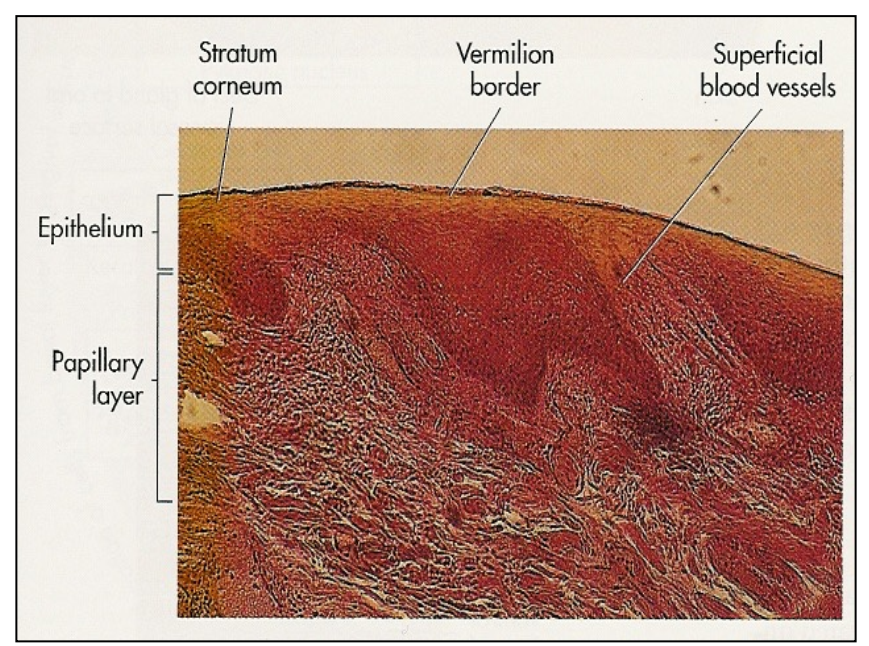
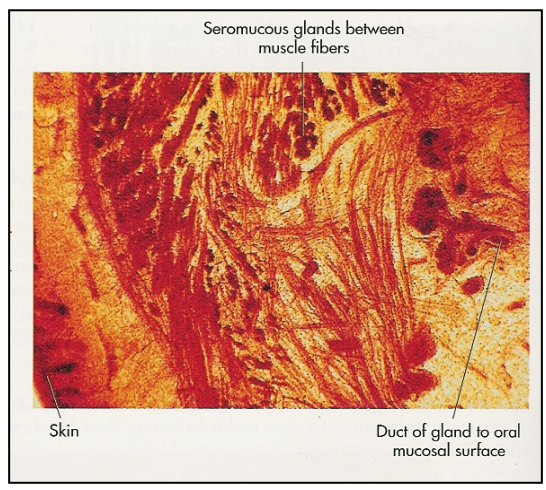
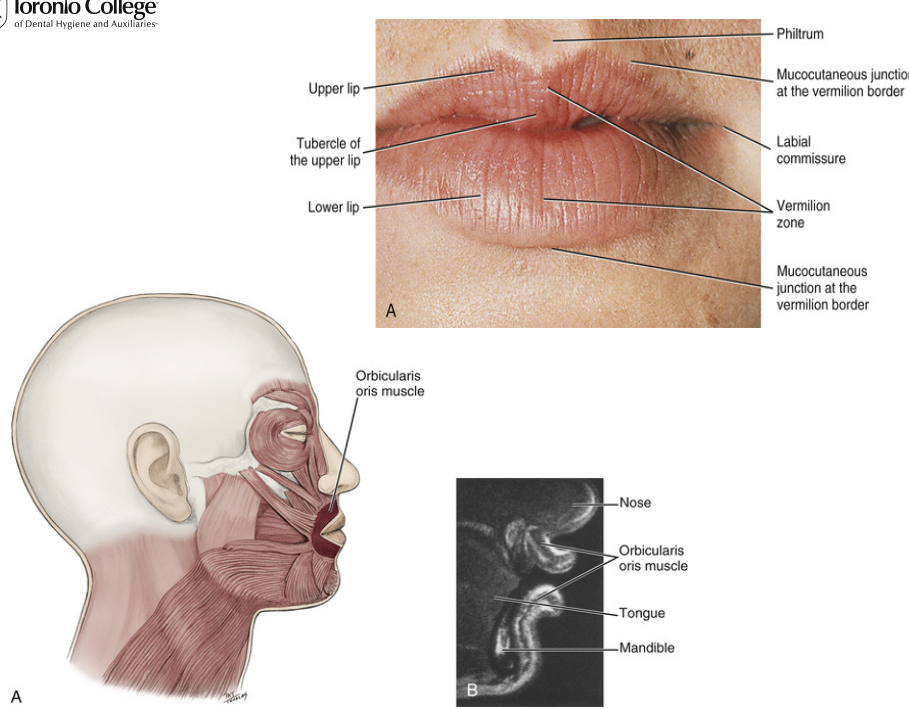
Describe the lining mucosa of the Lips
Non keratinized squamous epithelium (iinner lips)
Lamina propria → contains minor seromucous salivary glands
Submucosa → contains orbicularis oris muscle
muscle encircles the lips → “kissing muscle”
Contains eleidin (clear, semi fluid, intracellular protein)
transparent = blood vessels in papillary layer can show through giving lips their colour
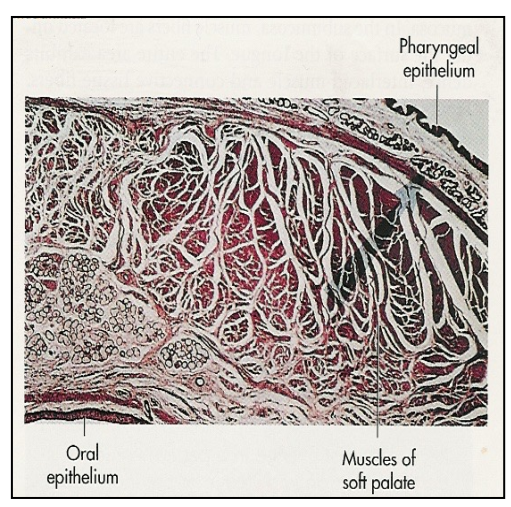
Describe the lining mucosa of the Soft Palate
Non-keratinized stratified squamous epithelium
Lamina propria → highly vascularized
Submucosa → contains muscles of the soft palate and mucous glands (minor salivary glands)
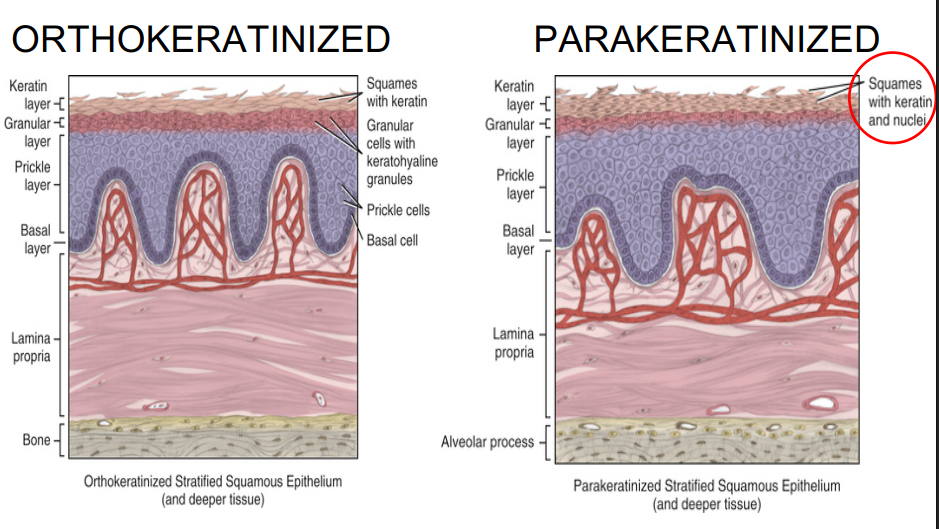
Describe Masticatory Mucosa
Parakeratinized or Orthokeratinized stratified squamous epthelium
Thicker, rubbery surface texture, more resilience, firm base
Abundant and pronounced rete ridges (prickle cell layer) = firm base
Thin or absent submucosa
Where can you find Masticatory mucosa in the oral cavity?
Attached gingiva
Dorsal surface of tongue
Hard palate
What is the difference between Parakeratinized and Orthokeratinized
Presence (parakeratinized) or absence (orthokeratinized) of nuclei in the keratinized layer.
Parakeratinized has a thinner keratin layer than orthokeratinized
Draw and label the Gingiva and the junctions between each “zone”
Gingiva = Free gingiva, attached gingiva, interdental gingiva/papilla
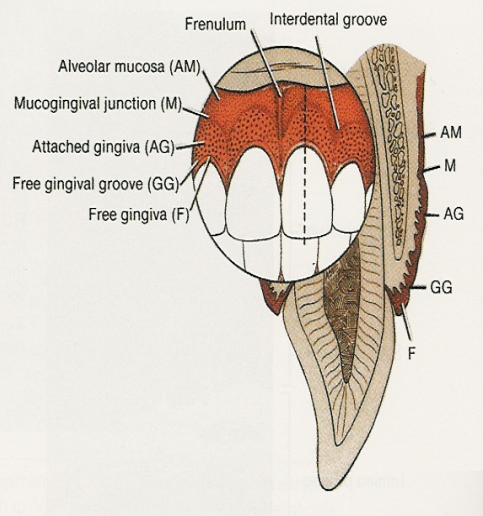
What is keratinized and smooth, has its inner margin at the gingival sulcus and outer margin as the oral cavity?
Free Gingiva
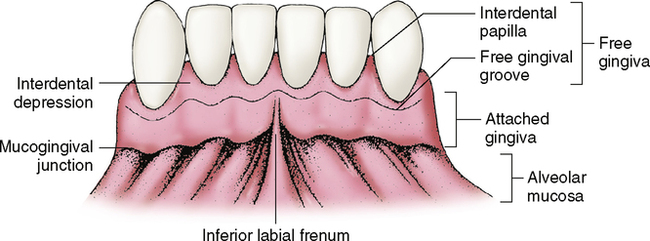
What is between the free gingival groove and mucogingival junction? What is its appearance?
Attached gingiva → keratinized and stippled appearance
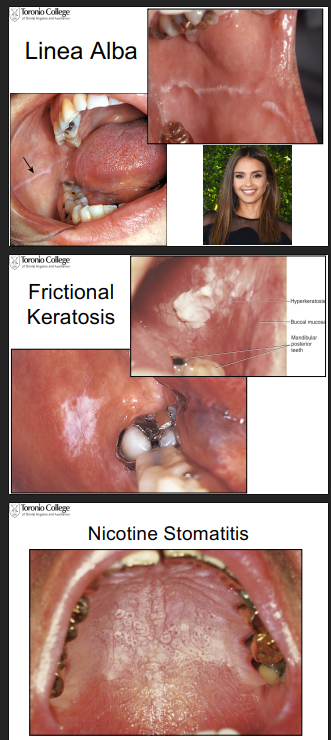
Why does hyperkeratinisation occur in the oral cavity?
Its the tissue’s response to frictional or chemical trauma (chronic trauma)
Examples:
linea alba = a line where max and mand teeth occlude
frictional keratosis = tissue response to teeth grinding or cheek biting (looks white, thickened, textured)
gingival fibrosis = toughing of the gums
nicotine stomatitis = damage to tissues from heat of smoking
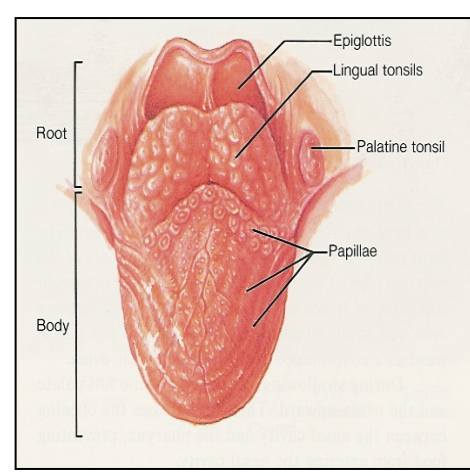
The anterior 2/3rds of the tongue is composed of what kind of muscle? What about the posterior 1/3rds? What are the names of these regions of the tongue?
Anterior aka body of tongue = skeletal muscle
Posterior aka root of tongue = skeletal muscle + anchored to the hyoid bone and covered with lingual tonsils.
What is the condition that is a short lingual frenum?
Ankyloglossia (tongue-tied)
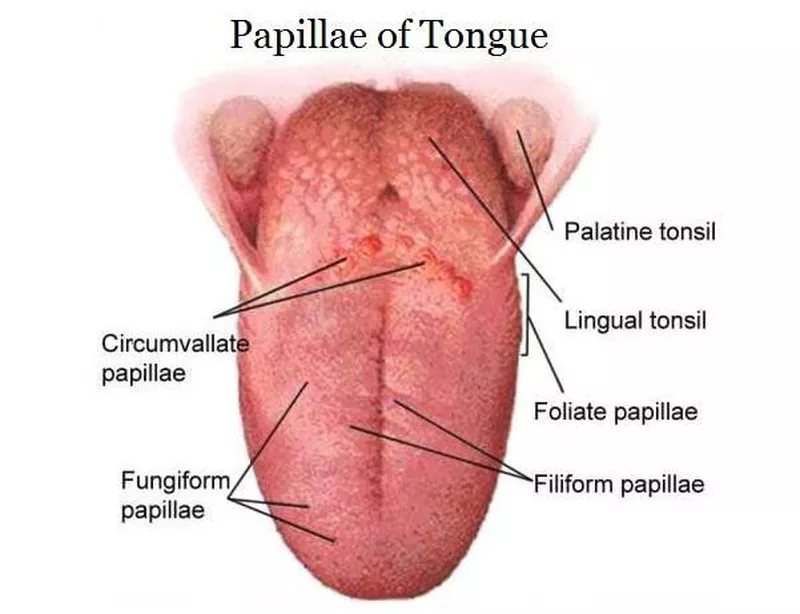
What is the function of the lingual papillae
provide friction for handling food and contains taste buds
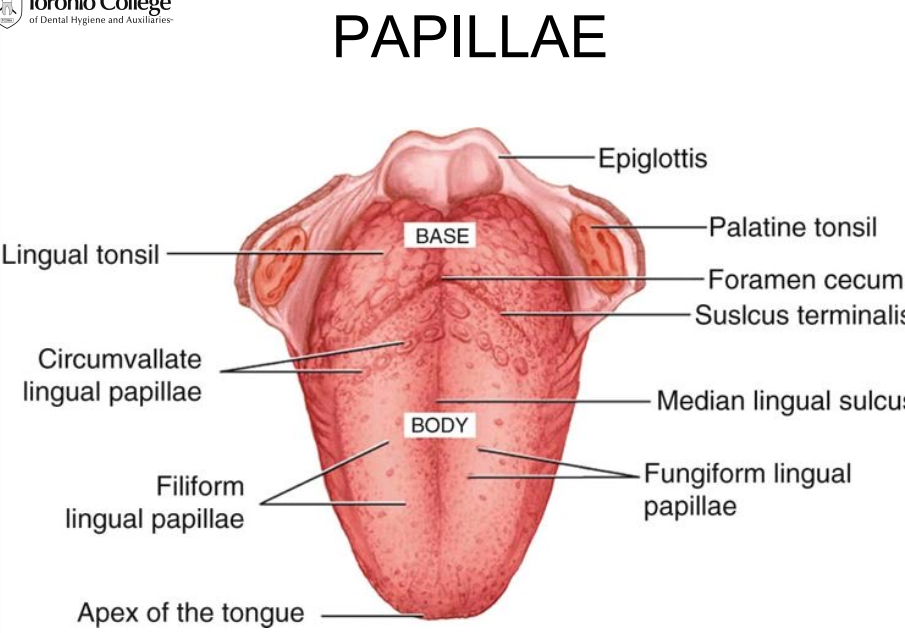
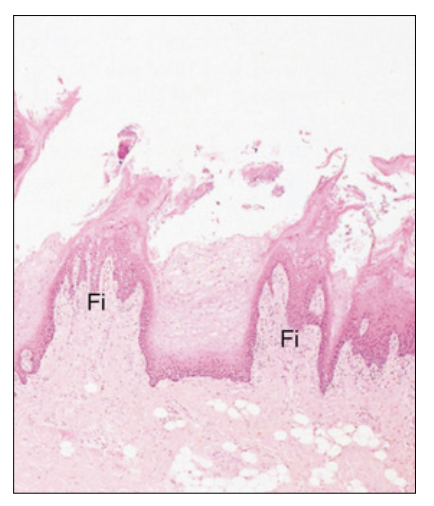
Describe Filiform Papillae and its function
most common, make up majority of the dorsal surface of tongue
fine pointed cones, tips pointing towards the throat
slender and threadlike
lined with a THICK layer of ortho/parakeratinized epithelium overlying core of lamina propria
no taste buds
Fx: is to provide mechanical grip for food manipulation
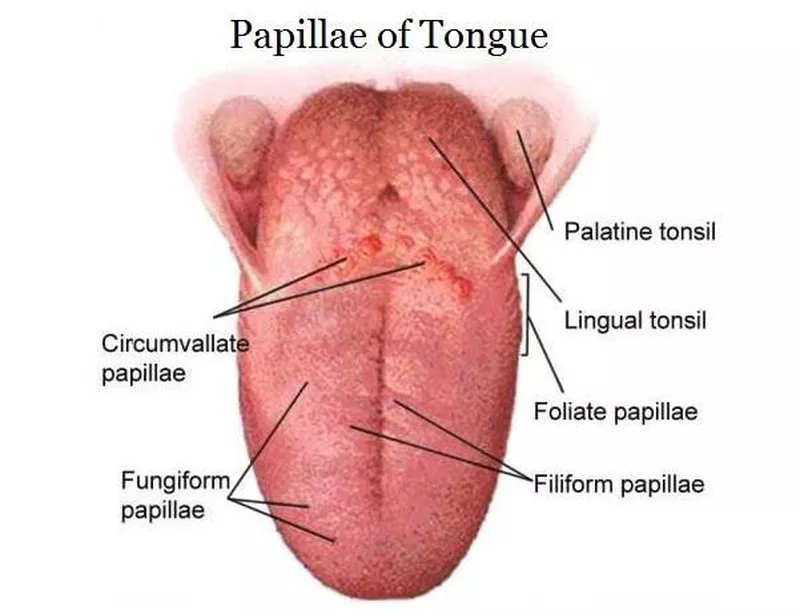
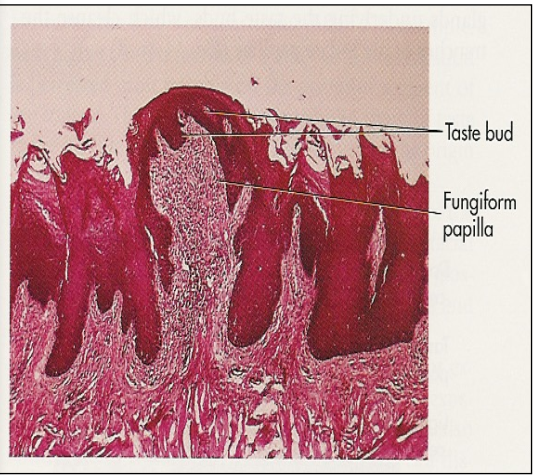
Describe Fungiform papillae
reddish dots on the tongue
mushroom shaped
thin layer of orthokeratinized or parakeratinized epithelium over lying the highly vascular lamina propria
has taste buds
Fx: taste
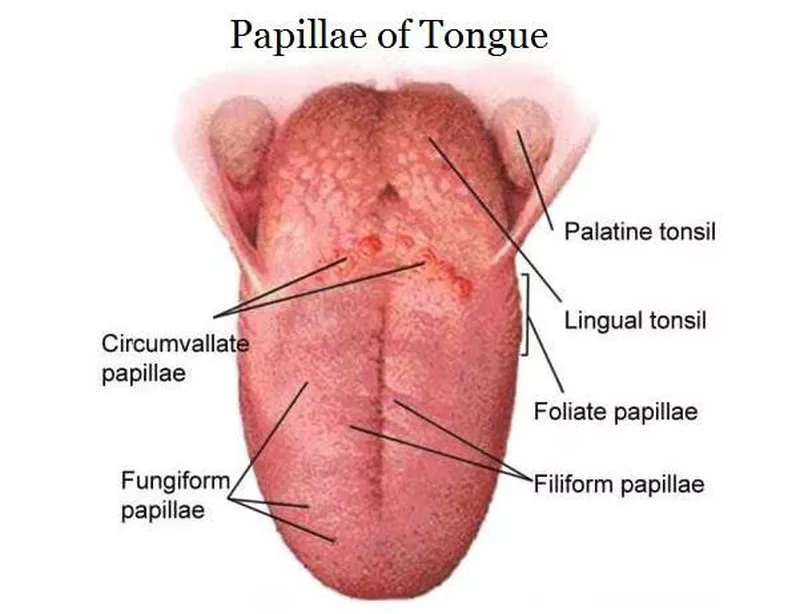
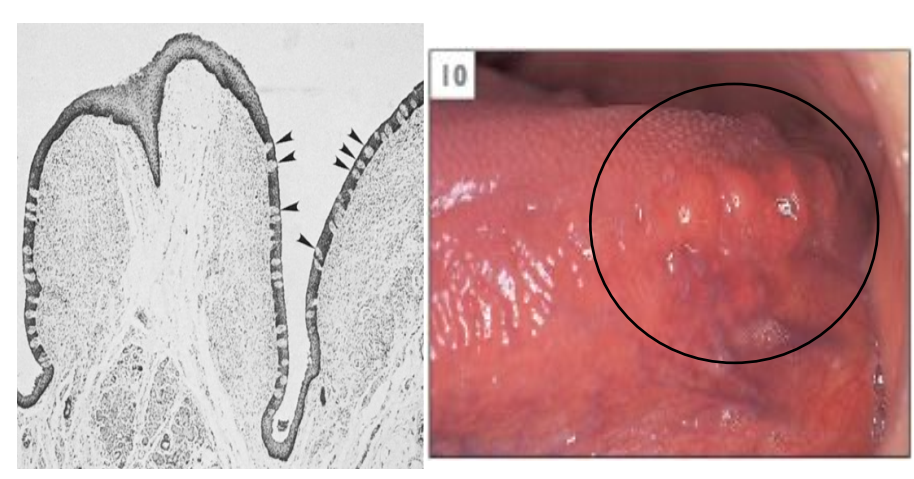
Describe Foliate Papillae
4-11 (amount)
Located on the vertical and parallel ridges on the lateral side of the posterior 1/3rd of tongue
Leaf-shaped
Lined with ortho/parakeratinized epithelium over core of lamina propria
has taste buds
Fx: taste
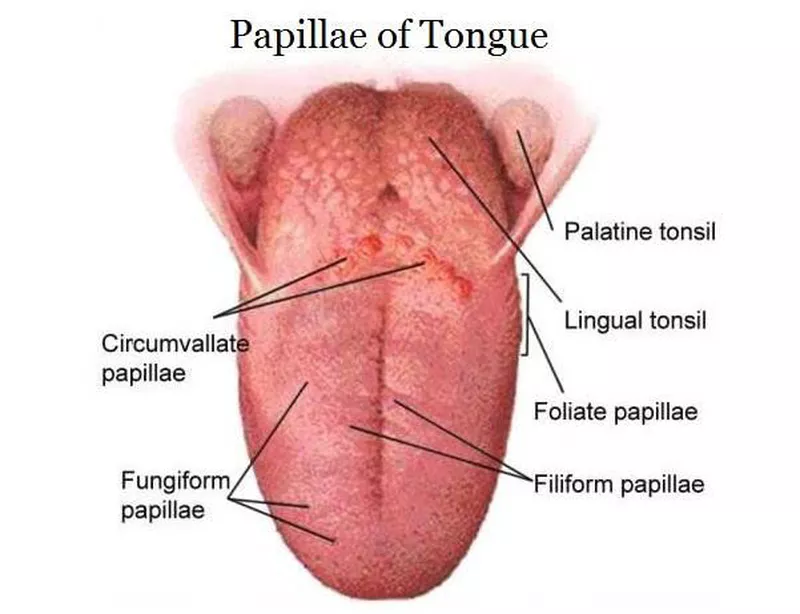
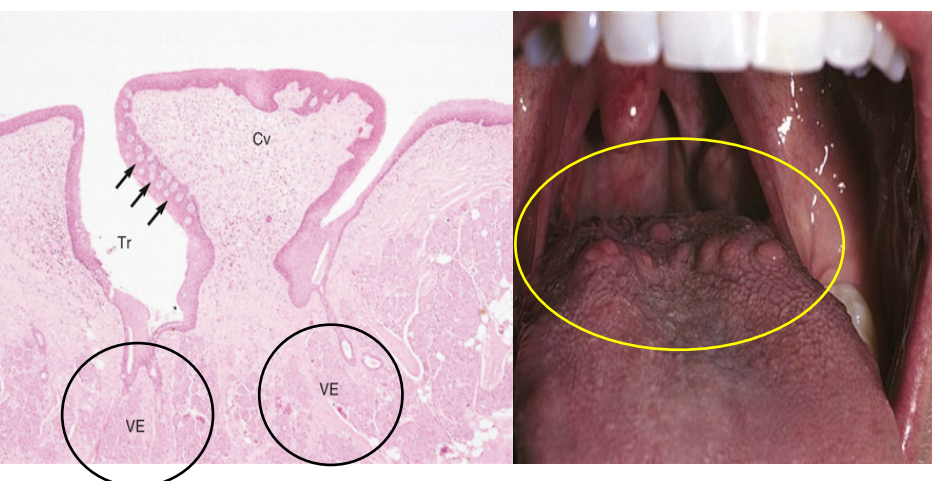
Describe Circumvallate papillae (vallate papillae)
7-15 raised, mushroom shaped papillae
located on the posterior 1/3rd of tongue in a V shape alignment
ortho/parakeratinized epithlium overlying lamina propria
has surrounding groove where von ebner gland is located
Fx: taste
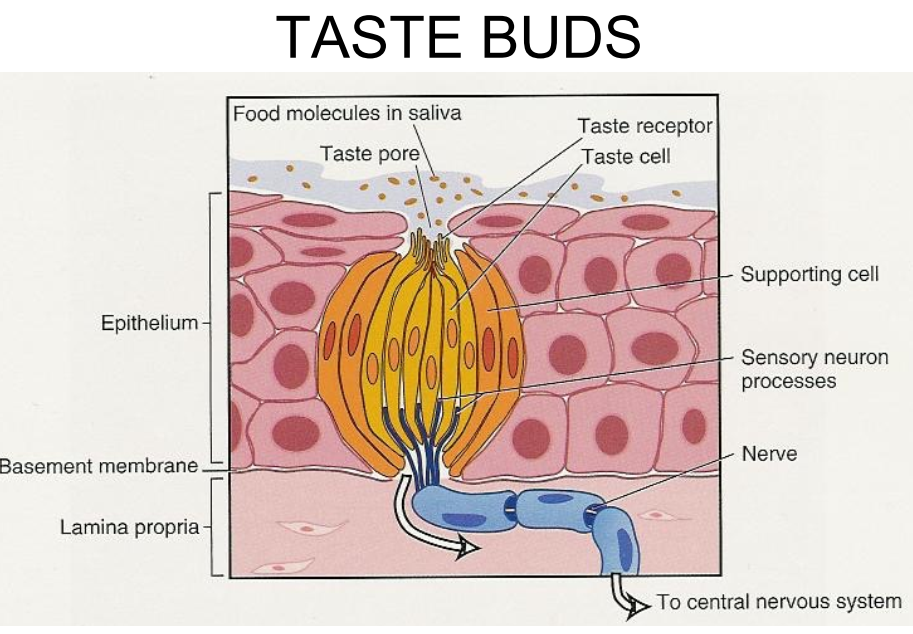
Describe the structure of Taste buds.
Microscopic barrel shaped bodies derived from epithelium and 30-80 spindle shaped cells
What is the turn over rate for taste buds?
~ 10 days
How do we taste/perceive taste?
Dissolved molecules of food touch taste receptors at the taste pore (opening of the taste bud)
Taste cells have a sensory neuron that will send impulses to the CNS (central nervous system) to be identified
4 types of taste sensation = sweet, sour, salty and bitter
Why is turn over time an important piece of information for cells in the oral cavity?
Helps us determine healing rates and recovery times from damage
JE = 4-6 days
Hard palate = 24 days
Lining mucosa faster than masticatory mucosa
Taste buds = ~ 10 days