advanced nursing exam 3
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
Prerenal Causes of Renal Failure:
o Factors that reduce systemic circulation leading to a reduction in renal blood flow and decreased glomerular perfusion; prolonged leads to intrarenal AKI
o Common causes-
- decreased cardiac output (cardiogenic shock, dysrhythmias, heart failure, MI)
- Decreased peripheral vascular resistance (anaphylaxis, neurologic injury, septic shock)
- Decreased renovascular blood flow (embolism, renal artery thrombosis)
- Hypovolemia (burns, dehydration, GI losses, hemorrhage)
Intrarenal Causes of Renal Failure:
o Conditions that cause direct damage to the kidney tissue, resulting in impaired nephron function
o Common causes-
- #1 in hospitalized patients is atubular necrosis – ischemia, nephrotoxins, sepsis
- Interstitial nephritis (allergies, antibiotics, NSAIDS, infections)
- Nephrotoxic injury (chemical exposure, contrast media, hemolytic blood transfusion reaction)
Postrenal Causes of Renal Failure:
o Post renal: involves mechanical obstruction to the outflow of urine. When flow is obstructed urine refluxes into the renal pelvis.
o Common causes-
BPH, Bladder cancer, Renal calculi, Prostate cancer, Trauma
Phases of Renal Failure: Oliguric
· Urinary changes—*oliguria – output < 400 mL/day
· Occurs within 1 to 7 days after injury
· Lasts 10 to 14 days
· Urinalysis shows casts, RBCs, WBCs, protein
· Specific gravity 1.010
· 50% patients non-oliguric; greater than 400 mL urine/day
Phases of Renal Failure: Diuretic
· Daily urine output is 1 to 3 L; up to 5 L
· Osmotic diuresis from high urea and inability of tubules to concentrate urine
· Monitor for hypovolemia, hypotension, hyponatremia, hypokalemia, and dehydration
Phases of Renal Failure: Recovery
· Increased GFR, decreased BUN and creatinine (return to normal)
· Influenced by the severity of injury and complications
Lab values with acute renal failure:
o Lab Values: increase creatinine, increase BUN, decrease GFR, decreased specific gravity, azotemia (nitrogen in blood), hypokalemia/hyperkalemia, hyponatremia
o Monitor potassium closely
Symptoms of Renal Failure:
o Fluid retention - edema, weight gain, crackles in the lungs
o Metabolic acidosis - tachycardia, HA, diarrhea, vomiting, Kussmaul breathing
o Normal or decreased serum Na+ - nausea, HA, weakness, seizures, coma
o Hyperkalemia - fatigue, weakness, dysrhythmias
Solutions to Hyperkalemia:
o 1. calcium gluconate IV – increases threshold for cellular excitation so potassium moves back into cells (can cause arrhythmias, so give over 10 minutes in ICU)
o 2. Regular insulin IV – GIVE WITH DEXTROSE; given to drive potassium back into the cell
o 3. Sodium bicarbonate – exchanged hydrogen ions for potassium to neutralize pH
o 4. Kayexalate – excreted through the GI tract
o 5. Loop Diuretics – excretes through the urinary tract
o 6. Hemodialysis
Continuous Renal Replacement Therapy (CRRT):
o Toxins and fluids are removed while acid-base status and electrolytes are adjusted slowly
o Used in hemodynamically unstable patients
o Patient is 1:1
o do not use AV fistulas for CRRT! use CVDC
Common Complications of CRRT:
o #1: clotting
o Others: infection, bleeding, hypotension, electrolyte imbalance
Sustained Low-Efficiency Daily Dialysis (SLEDD):
o Hybrid between intermittent HD and CRRT
o Managed strictly by an RN
o uses a CVDC
o Runs for 6-12hrs/day
o Patient does not have to be 1:1
What is Hemodialysis?
o Rapid fluid removal, effective in potassium removal, temp access can be placed at bedside
o Restrictive, vascular access, expensive
o uses fistula
o if patient is hypotension (SEE THIS PATIENT FIRST)
Dialysis access sites:
o Venous access sites: common include subclavian & femoral
o Red: pulls patient blood
o Blue: pushes filtered blood back to the patient
RN Responsibilities for Dialysis:
o Monitor flowsheets hourly
o Q8HRS labs
o Maintain line patency
Chronic Kidney Disease (CKD):
o Defined as GFR < 60 for 3 months+
o S/S: fluid retention, peeing at night, insomnia
o Most die due to CVD (manage HTN)
o Do not be concerned if a patient with CKD comes in with a creatinine of 3 or a slightly low Hbg or RBC (this is normal for them) - high potassium and HTN are still a concern
Management of CKD:
o Correct fluid volume issues, RRT, lower potassium
o Give calcium supplements, antihypertensives, erythropoietin, lipid-lowering drugs
End Stage Renal Disease (ESRD):
o GFR < 15
o Symptoms usually begin here
o Dialysis or renal transplant is required for survival
What education would you give a patient on peritoneal dialysis?
o Less complicated, portable system, less cardiovascular stress
o High infection risk, catheter migration
o Peritonitis is main concern with PD due to the catheter in abdomen – use strict aseptic technique
o PD patients have dialysis daily so missing an appointment is a concern
Main differences between patient populations on hemodialysis vs peritoneal vs CRRT:
o Hemodialysis: usually 3 appointments per week, can be done through a catheter or fistula
o Peritoneal: belly filled with fluid where peritoneum is used as a natural filter, fewer restrictions, patients often need to be healthier
o CRRT: critically ill patients who are hemodynamically unstable
Care for AV fistulas:
o Most CKD patients have a fistula
o Limb alert on that side; feel the thrill, listen for bruit (both are good)
o Post-Op: do not lift heavily
Contraindications for kidney transplantation:
Advanced cancers, untreated heart disease, chronic respiratory failure, extensive vascular disease, chronic infection, unresolved psych issues
Renal transplants and the use of immunosuppressive drugs cause increased mortality primarily due to what?
o Immunosuppressive drugs are required for life after transplant
o Increased mortality due to infection and cancer risk
Are NSAIDs used for CKD patients?
No, because of the increased risk for renal damage and GI bleeding
What is the Romberg test?
o Test of proprioception
o Have patient stand with feet together and close eyes
o (+) if sways or falls with eyes closed
o Indicates vestibulocochlear dysfunction or spinal cord disease
o Risk for falls
Nerve regeneration in PNS vs CNS:
o PNS is more likely to regenerate than SNS
o PNS nerve fibers regenerate within the myelin sheath
o If the axon of the nerve is damaged, the cell will attempt to repair itself by growing back to its original destination through branches at the damaged end
What does GABA do? What does that mean?
o GABA is the main inhibitory neurotransmitter, like serotonin and dopamine
o Block chemical messages to prevent their actions
Function & assessment of the 1st cranial nerve:
o Olfactory nerve (smell) - purse sensory nerve
o Occlude one nostril and as the patient to identify specific smells
Function & assessment of the 2nd cranial nerve:
o Optic nerve - pure sensory nerve
o Snellen assessment, one eye at a time
o Confrontation of visual fields
Function & assessment of the 3rd cranial nerve:
o Oculomotor nerve - pure motor nerve
o Innervation of pupil and lens, upper eyelid, and visual tracking muscles
Function & assessment of the 4th cranial nerve:
o Trochlear nerve - pure motor nerve
o Innervation of muscle used to move eye down and shift from side to side
Function & assessment of the 5th cranial nerve:
o Trigeminal nerve - mixed nerve
o Facial sensation test
Function & assessment of the 6th cranial nerve:
o Abducens nerve - pure motor nerve
o Innervates the muscle used to abduct the eye
Function & assessment of the 7th cranial nerve:
o Facial nerve - mixed nerve
o Check for symmetrical movements of the face
Function & assessment of the 8th cranial nerve:
o Auditory nerve - pure sensory nerve
o Hearing test & vestibular function tests (watch for nystagmus)
Function & assessment of the 9th cranial nerve:
o Glossopharyngeal nerve - mixed nerve
o Stimulate the gag reflex
Function & assessment of the 10th cranial nerve:
o Vagus nerve - mixed nerve
o Have patient say "ah" and inspect for symmetry of the palate
Function & assessment of the 11th cranial nerve:
o Spinal accessory nerve - pure motor nerve
o Have patient turn head against resistance and elevate shoulders against resistance
Function & assessment of the 12th cranial nerve:
o Hypoglossal nerve - pure motor nerve
o Have patient stick out their tongue and look for deviation
How to perform a somatic sensory exam for pain, temperature, and touch:
o Touch with eyes closed
o Sharp dull, symmetrical, etc.
o Used to assess cranial nerve 5
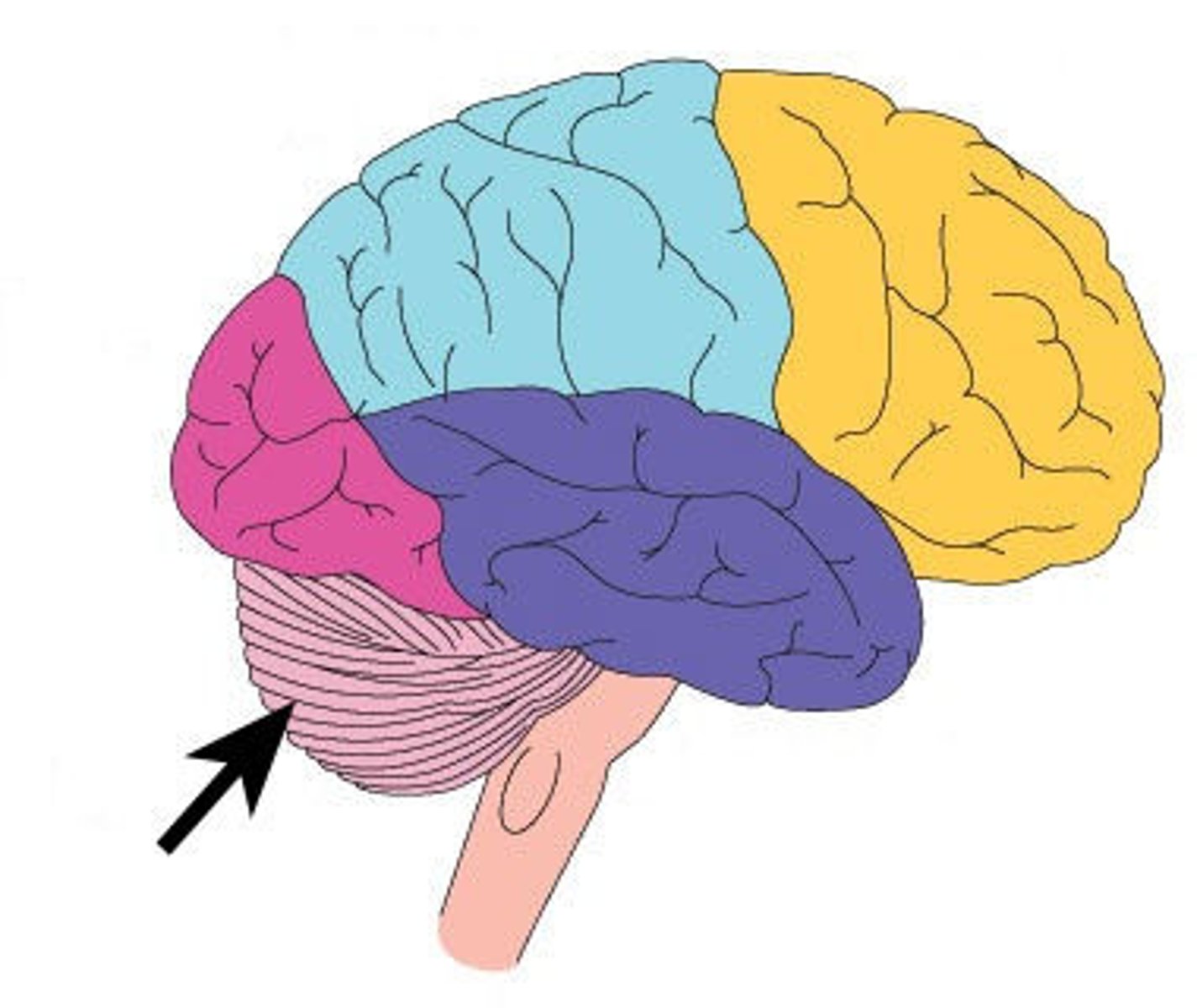
What role does the cerebellum play?
o Controls voluntary movement and stability
o If a patient has damage to the cerebellum, they are a high fall risk
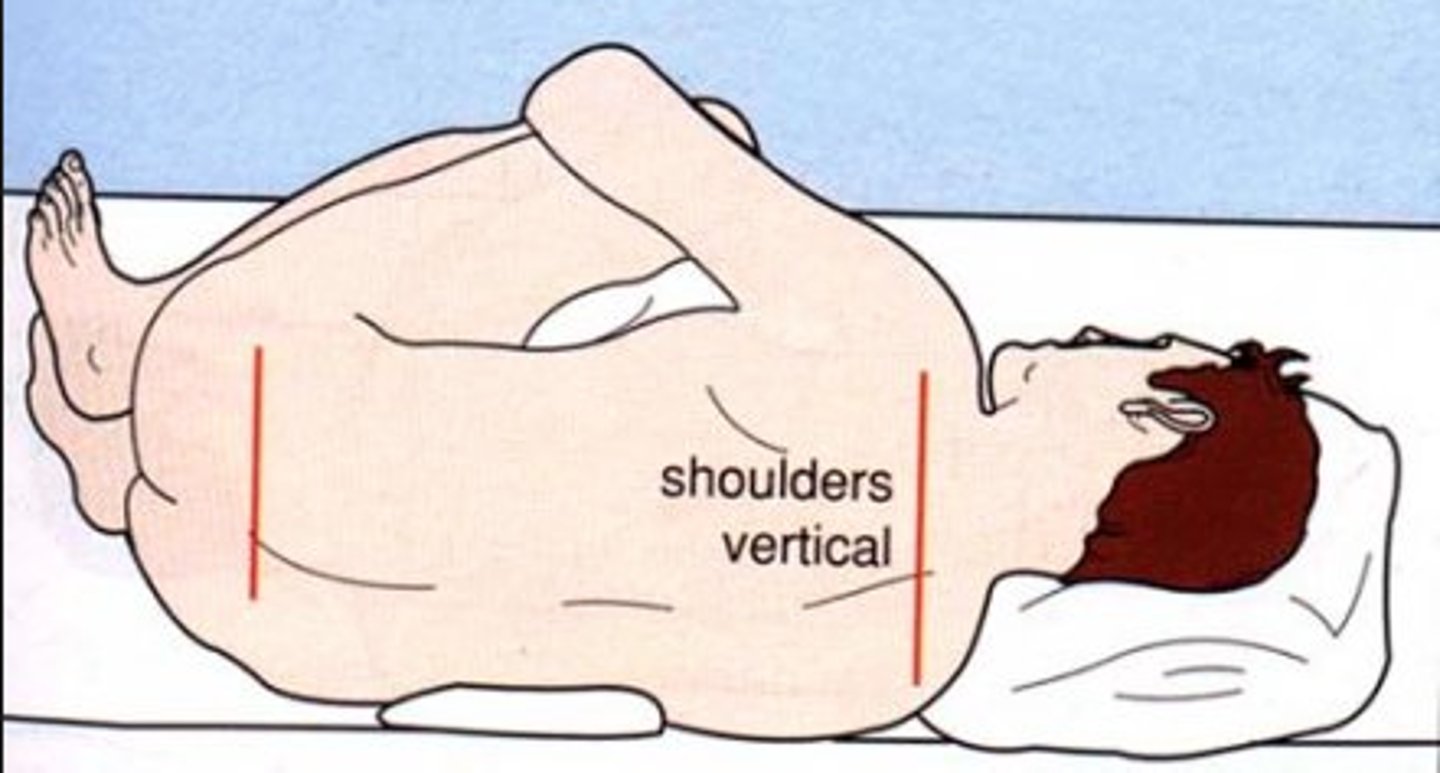
Lumbar Puncture:
- halo sign - indicates clear fluid is CSF
- Contraindications: suspected increased ICP, trauma, infection at site
- Pre: have patient void, assess for pain, explain procedure
- During: lateral recumbent position
- Post: monitor neuro status and VS, HA, nuchal rigidity
Tests for the nervous system: CT, CT angiography
o CT Scan: provides rapid images of the brain with or without contrast
- Ask about allergies to shellfish, iodine, or contrast dye before
o CT angiography: noninvasive image of the vascular system in the brain
Tests for the nervous system: cerebral angiography
- catheter inserted into femoral artery into aortic arch into carotid, contrast inserted, radiographic images are taken as contrast flows through vessels
- Assess for stroke risk before procedure due to risk of thrombi dislodgement
- After, monitor every 15-30 min for first 2 hours, every hour for next 6 hours, and every 2 hours for next 24 hours. Maintain bedrest for 6 hours.
Tests for the nervous system: electroencephalography, electromyography, electromyography, evoked potentials
o Electroencephalography: electrical activity in the brain is recorded via scalp electrodes
o Electromyography: electrical activity associated with innervation of skeletal muscle determined via needle electrodes
o Electroneurography: measures conduction velocity of peripheral nerves
o Evoked potentials: recordings of electrical activity of nerve conduction after a stimulus via electrodes placed on the scalp
Definition of nystagmus:
o Eyes make repetitive, uncontrolled movements resulting in reduced vision and impaired coordination
o Monitor for in testing the 3rd cranial nerve
Definition of normal tracking:
o Patient should look at and follow a target with their eyes as the tester moves horizontally, vertically, and rotates
o Track should be smooth and brisk
Definition of convergence:
o Eye moves towards the midline of the face
o Tested through holding an object away from the face and bringing it towards the nose
Definition of accommodation:
Adjustment of the optics (lens & pupil) of the eye to keep an object in focus at different distances from the eye
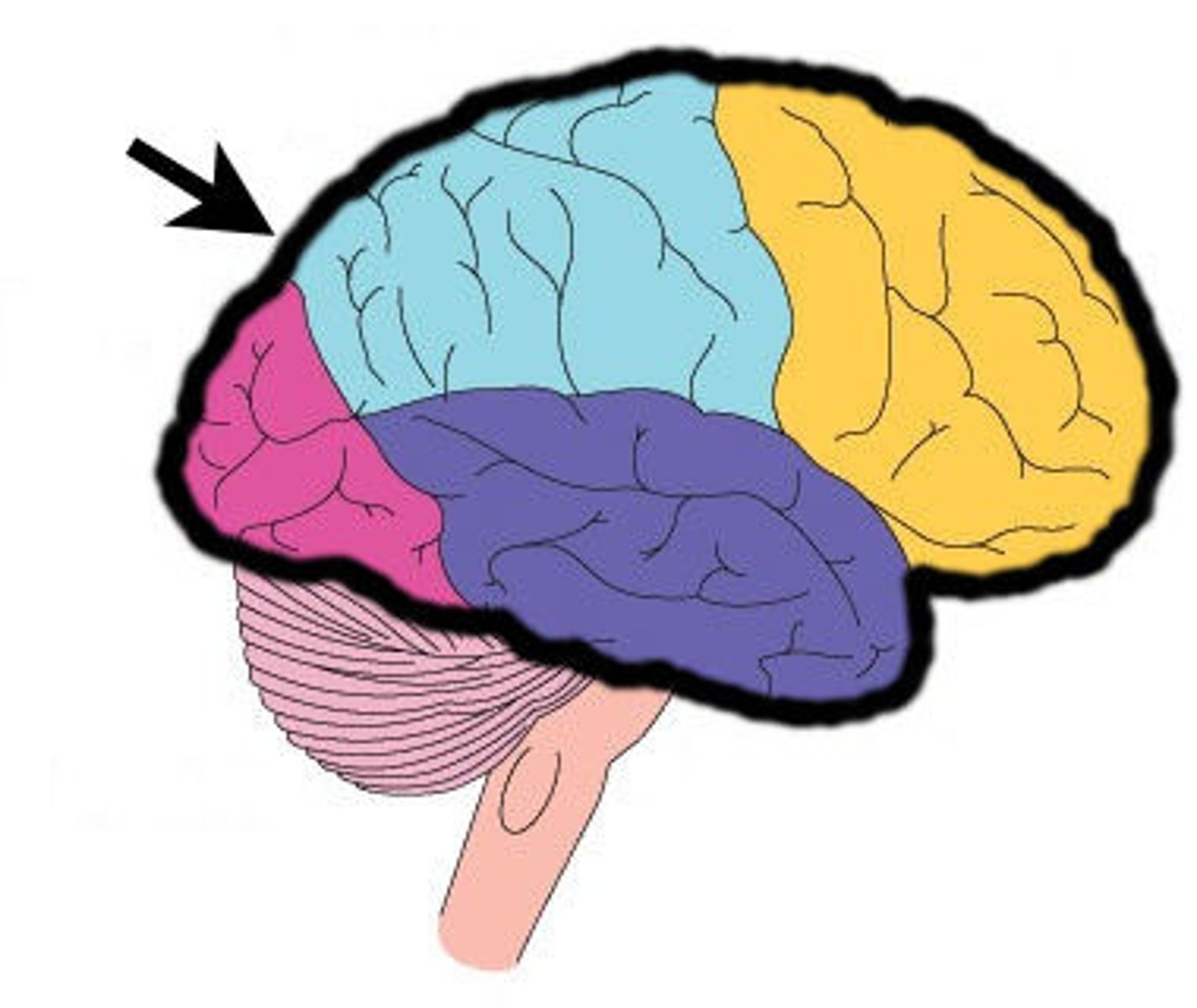
What is the cerebrum?
o Frontal lobe - cognitive, behavior, memory, movement
o Temporal lobe - language
o Parietal lobe - special information, sensory
o Occipital lobe - vision
What factors influence cerebral blood flow?
o Autoregulated via adjustment in diameter of cerebral blood vessels
o Factors include CO2, O2, and blood pH
Head injury assessment:
o LOC
o Glasgow Coma Scale (< 8 is very concerning)
o Cranial nerve testing
o Motor strength - push/pull, pronator drift (insert picture)
o Vital signs
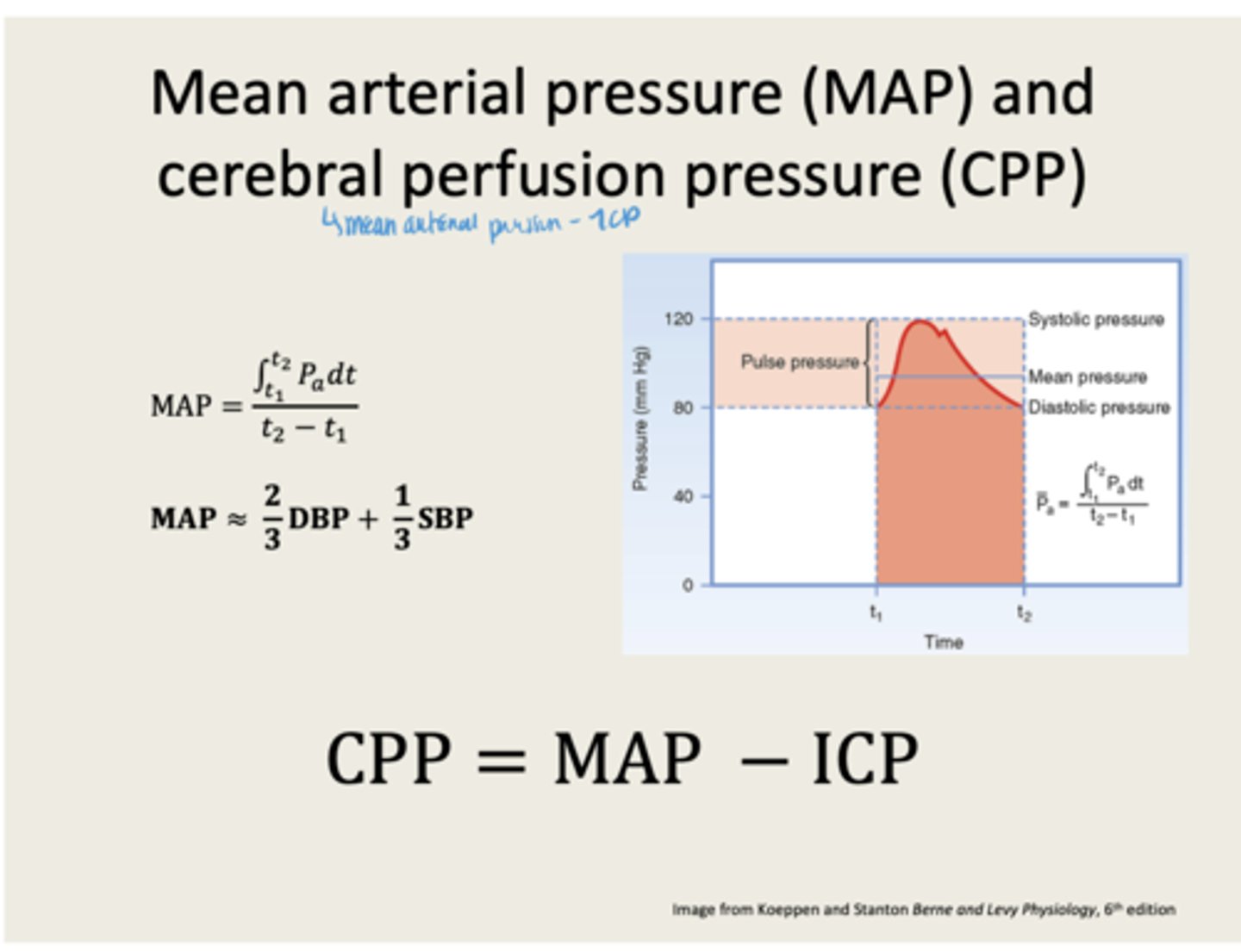
How to measure CPP:
o Cerebral perfusion pressure (CPP) = MAP - ICP
o Normal is 60-100
o If CPP is low, blood flow is low
How to measure ICP:
o Normal ICP is 5-15 (elevated is > 20 sustained)
o Measured as a mean pressure via catheter and transducer (must be level)
o Can drain intermittently or continuously; ventricular can be controlled by nurse
o Immediately report ICP elevation
o Inaccurate readings caused by leaks, obstructions, unlevel system, air in system

What are signs of increased intracranial pressure?
o change in LOC
o change in VS – Cushing’s triad
o compression of CNII – ipsilateral pupil dilation, sluggish pupils, eyelid ptosis
o decrease in motor function – hemiplegia, posturing
o headache that is worse in the morning
o projectile vomiting not preceded by nausea
o Will eventually lead to herniation, death of the brainstem, and loss of respiratory function
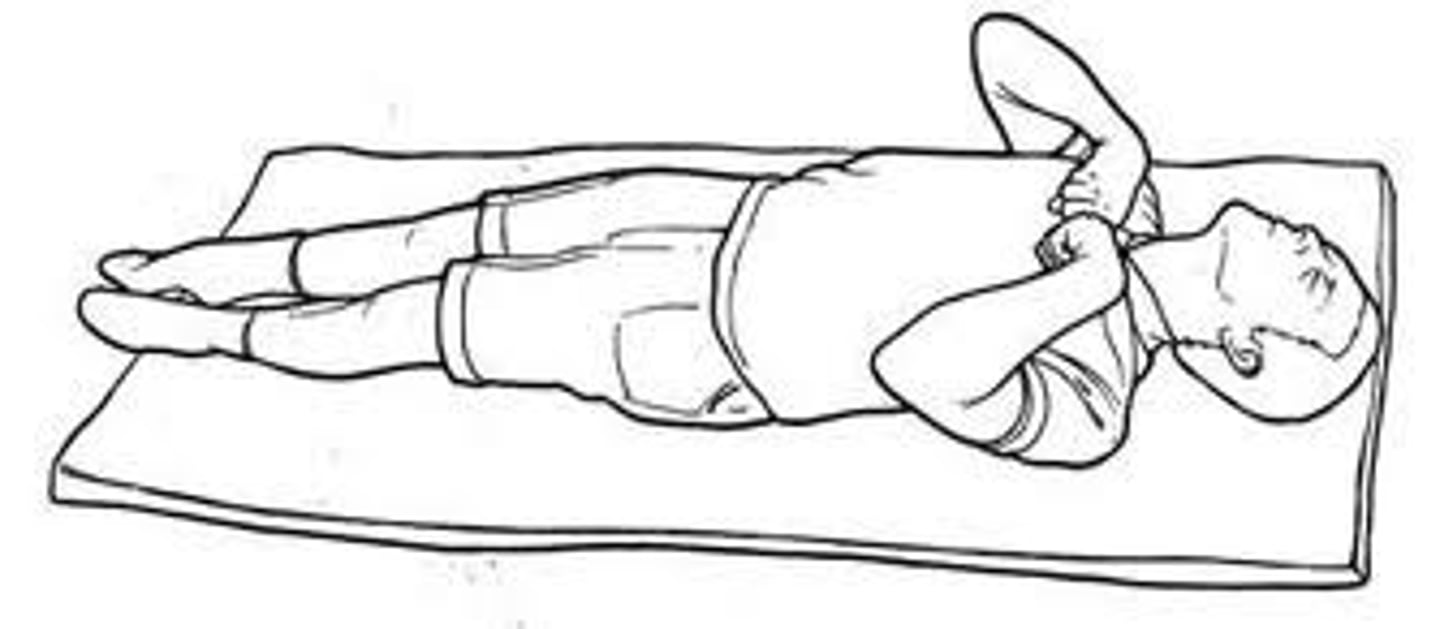
Decorticate Posturing:
o "coming to the core"
o Flexion of arms, wrists, and fingers with adduction in upper extremities. Extension, internal rotation, and plantar flexion in lower extremities
o Interruption of the voluntary motor tracts in the cerebral cortex
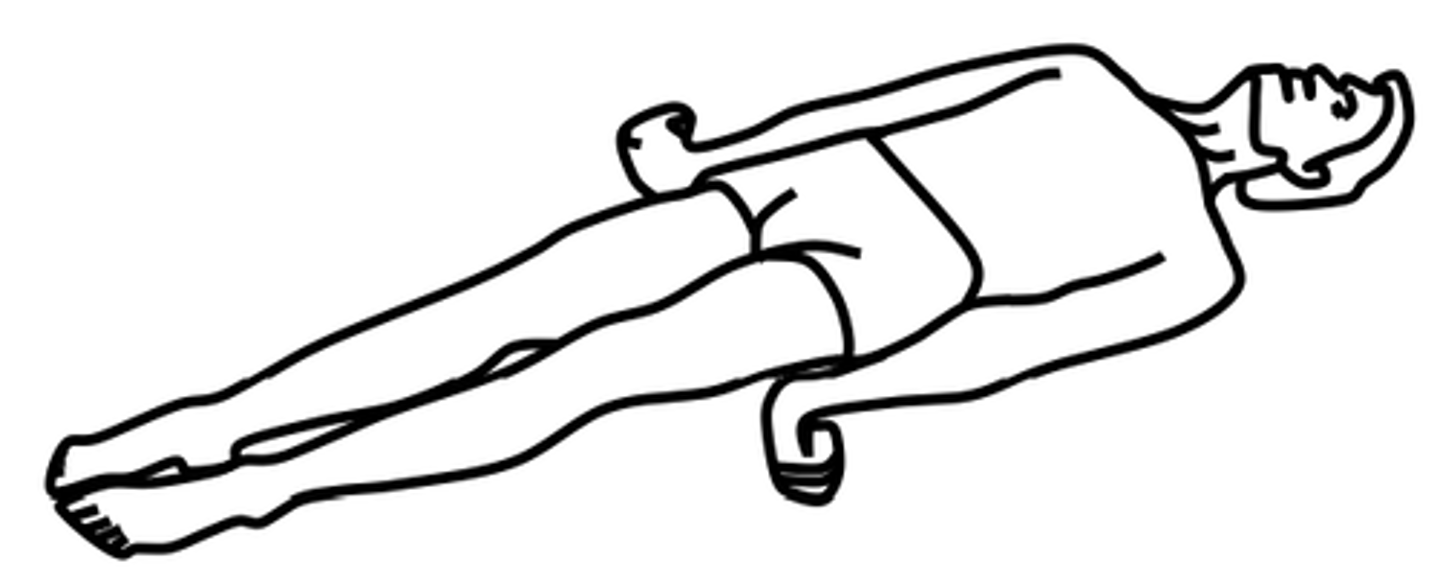
Decerebrate Posturing:
o Worse to see
o All 4 extremities in rigid extension, with hyperpronation of forearms and plantar flexion of feet
o Interruption of the motor fibers in the midbrain and brainstem
Stages of increased ICP:
o Stage 1: total compensation
o Stage 2: decreased compensation, risk for increased ICP
o Stage 3: failing compensation, cushing's traid
o Stage 4: herniation & imminent death
What is Cushing's Triad?
o Change in VS: systolic HTN w/ widening pulse pressure, bradycardia, irregular respirations
o Ominous sign before moving into stage 4
Nursing considerations for patients with an increased ICP:
o No lumbar punctures! Can cause cerebral herniation
o Maintain PaO2 > 100
o Maintain PaCO2 35-45 (will likely need mechanical ventilation)
o Begin feeding within 3 days of injury due to hypermetabolic state - will need glucose
Mannitol indication and therapeutic response:
o Indicated for cerebral edema or increased ICP
o ICP should decrease as fluid is removed
What does hypertonic saline do for patients with an increased ICP?
o Moves water out of cells and into blood
o Monitor BP and serum sodium levels
What is cerebral herniation? What causes it?
o when brain tissues move from one part of the brain to another adjacent part of the brain
o Inadequate cerebral perfusion -> Cerebral herniation
o Death is imminent
What is the Glasgow Coma Scale and how do you use it?
o Describes the consciousness of patients through assessing eye-opening, motor function, and verbal responses
o Mild/normal = 13-15, moderate = 9-12, severe = 3-8
Considerations for head & spine injuries (times of main concern, hallmark S/S, what should nurses be monitoring):
o Primary prevention is key
o Mortality increased immediately, 2hrs after, and 3 weeks after
o Hallmark S/S: raccoon eyes (periorbital edema), battle's sign (postauricular ecchymosis & otorrhea)
o Nurse should monitor LOC
Acute care of head injuries:
o Maintain HOB > 30*
o Daily weights
o Monitor for DI or SIADH
o keep head midline, avoid neck flexion, avoid hip flexion
o restraints and sedatives to prevent self-injury
o Seizure precautions
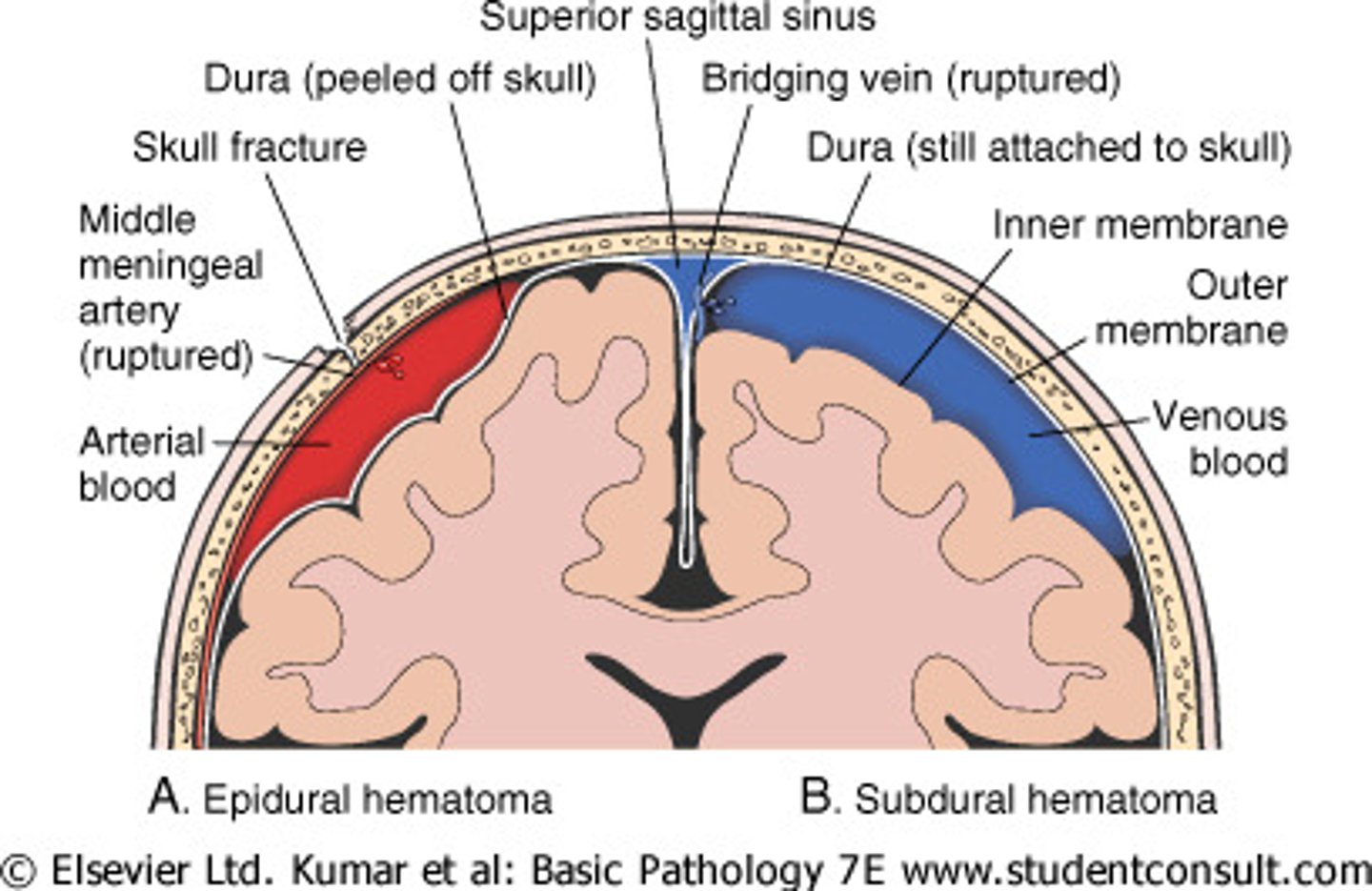
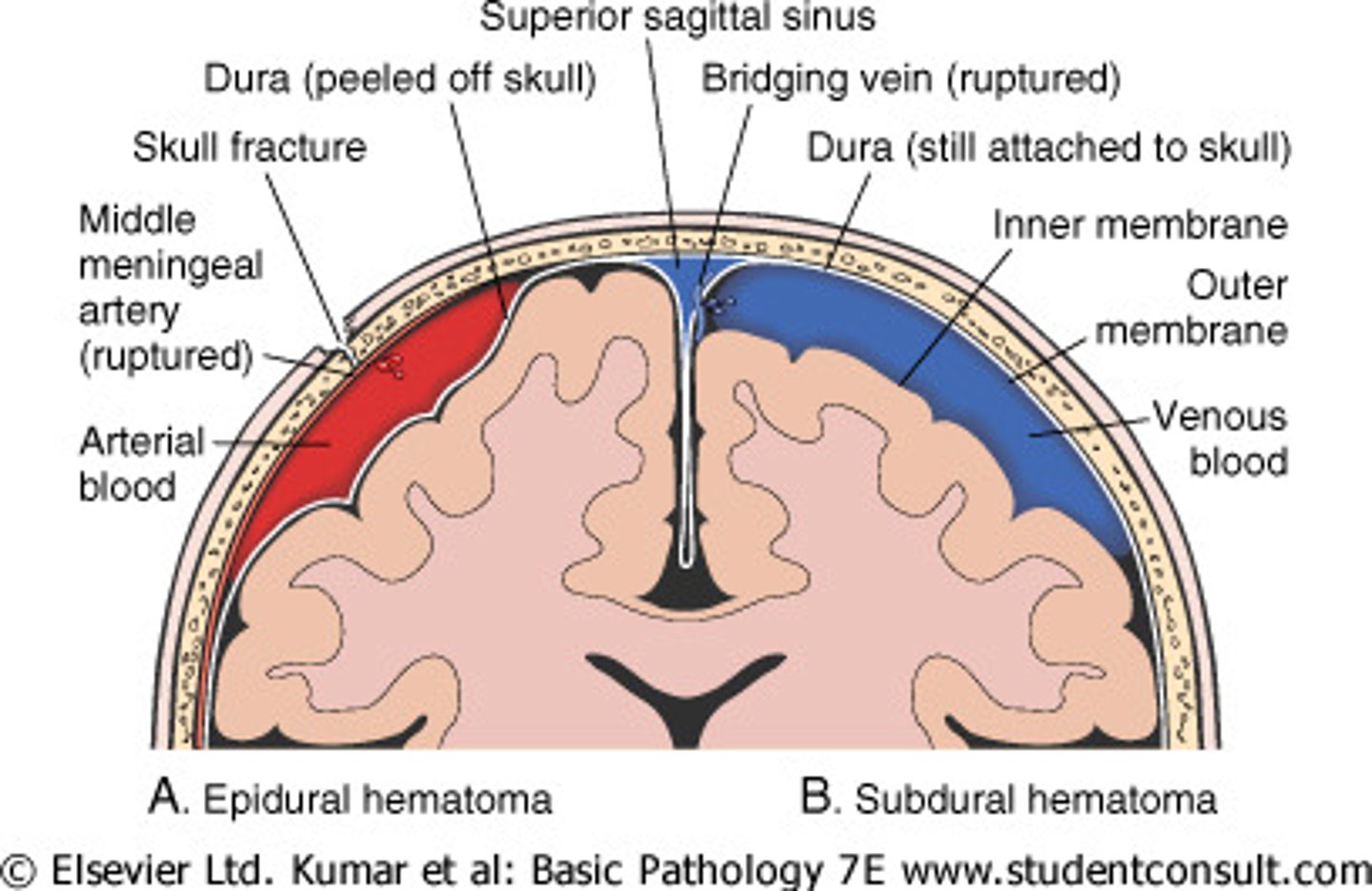
Complication of head injuries - epidural hematoma:
o bleeding between dura and inner surfaces of the brain
o present with unconsciousness, brief period of consciousness, then decreased LOC again w/ nausea and vomiting
o requires immediate surgery
Bacterial meningitis (causative agents, s/s, complications):
o Acute inflammation of the meningeal tissue caused by Streptococcus pneumoniae and Neisseria meningitidis – (NM requires droplet precautions)
o Bacterial is a medical emergency
o S/S: fever, severe HA, n/v, nuchal rigidity, photophobia, decreased LOC, seizures
o Complications: increased ICP, changes in vision, cerebral edema (seizures, CNII palsy, bradycardia, HTN, death)
Nursing actions for a patient with meningitis:
o Offer cooling blankets for a fever
o Administer sedatives to prevent shivering
o Initiate seizure precautions; have O2 and suction in room
Define subdural hematoma:
o Accumulation of blood on the surface of the brain
o Often after a head injury
Define brain death:
o Function of the cerebral cortex of the brainstem is used to declare brain death as it controls respiratory, vasomotor, and cardiac functions
o If there is no electrical functioning in the brainstem, the patient is considered brain dead
Directions of injury for the spine:
o Flexion – chin to chest
o Hyperextension – head pushed too far back
o Extension-rotation
o Compression – spine is compressed leading to vertebrae being crushed
o Flexion-rotation - most unstable because ligaments that stabilize the spine are torn; most often contributes to severe neurologic deficits
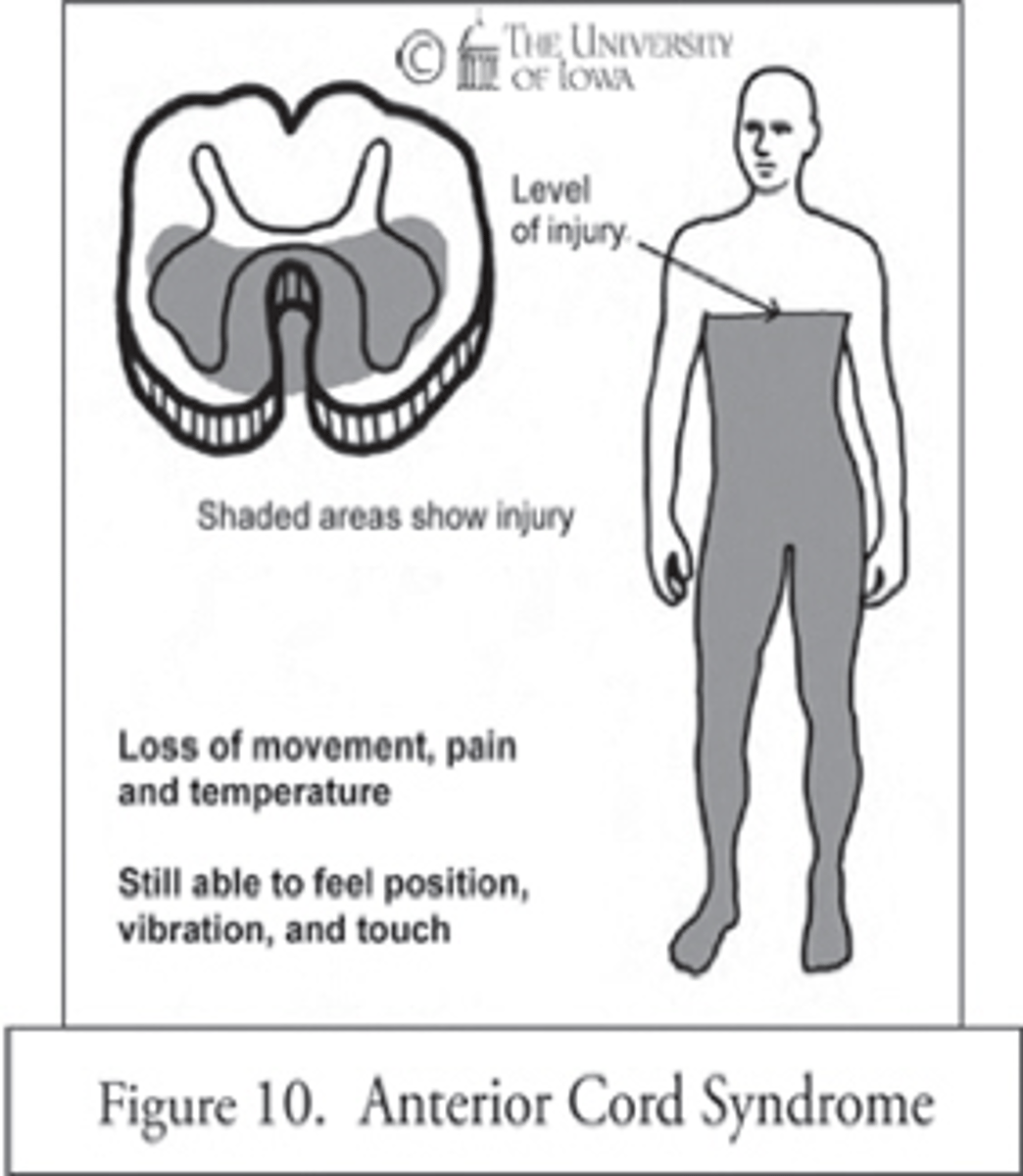
Damage to anterior vs posterior spine:
o Damage to anterior spine - motor deficits
o Damage to posterior spine - sensory deficits
Immediate care of SCI:
o Maintain airway
o Place patient in C-collar
o Permissive HTN: increases SBP is higher intentionally to ensure good blood flow to the cord; maintain SBP >90 and MAP >85
o Watch for increased medication interactions due to altered drug metabolism
o Encourage surgery within 24 hours
Primary injury SCI:
Initial mechanical disruption of axons as a result of stretch or laceration
Secondary injury SCI:
o Ongoing, progressive damage that occurs from inflammation after the initial injury
o Vessels dilate -> increased blood flow to spinal column -> increased pressure -> further damage
o Apoptosis occurs for weeks after the injury and may cause post-injury demyelination leading to scar tissue formation and neuro deficit
Skeletal vs neuro levels of injury:
o Skeletal level of injury is main point at which the most vertebrae have sustained damage - includes cervical, thoracic, lumbar & sacral
- Cervical & lumbar most common
o Neurologic level is the lowest segment of the spinal cord that is fully intact. The level of injury may be cervical, thoracic, lumbar, or sacral.
Complete vs Incomplete injury:
o Complete: total loss of sensory and motor function below level of injury
o Incomplete: mixed loss of voluntary motor activity and sensation; some tracts intact
Incomplete SCI - Central cord syndrome:
o Commonly seen in cervical region
o Common in older adults
o Leads to motor weakness and sensory loss w/ dysesthesia pain in UEs
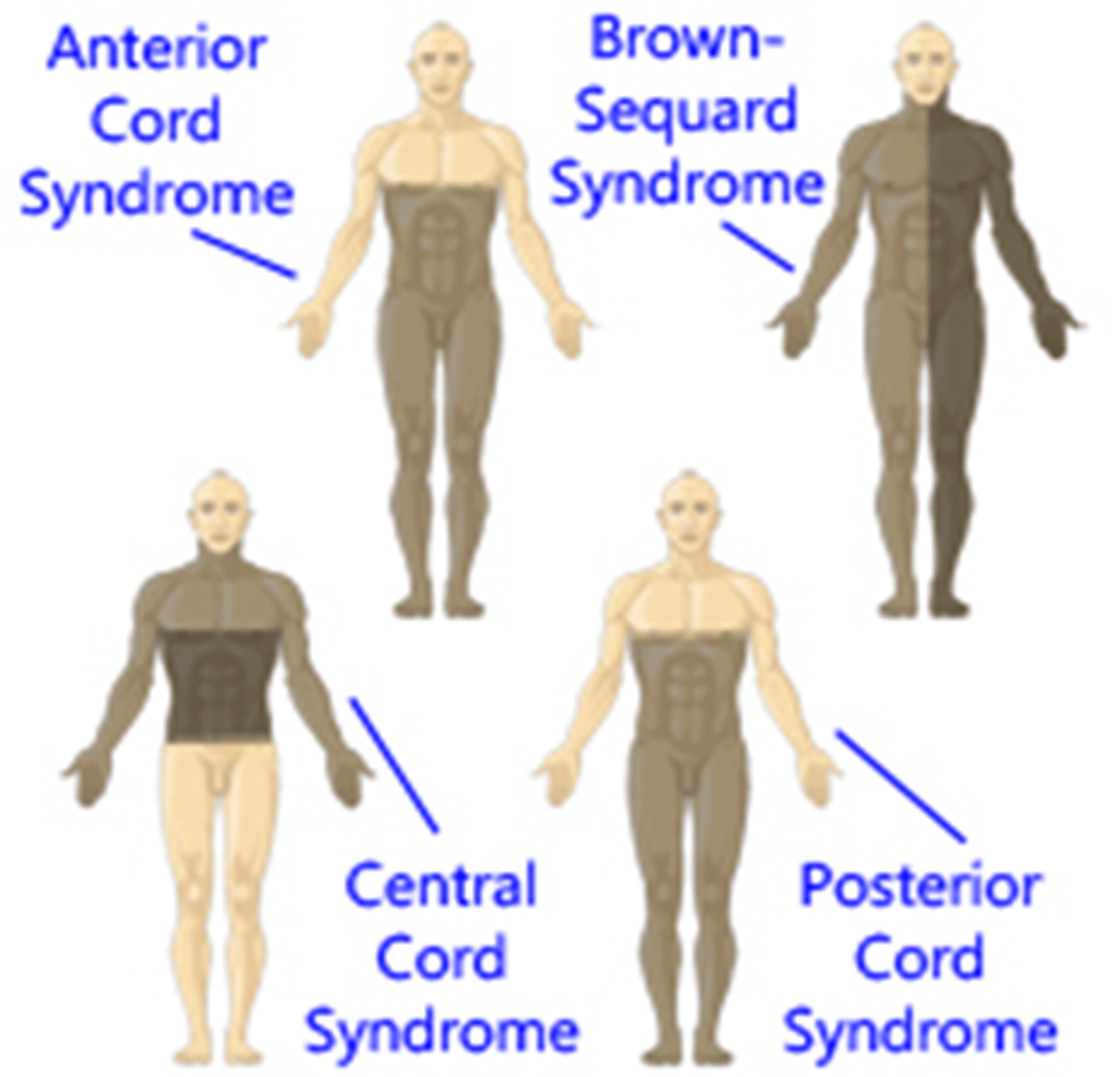
Incomplete SCI - anterior cord syndrome:
o Anterior spinal artery is damaged -> decreased blood flow
o Results from flexion injury
o Leads to motor paralysis and loss of sensation below injury
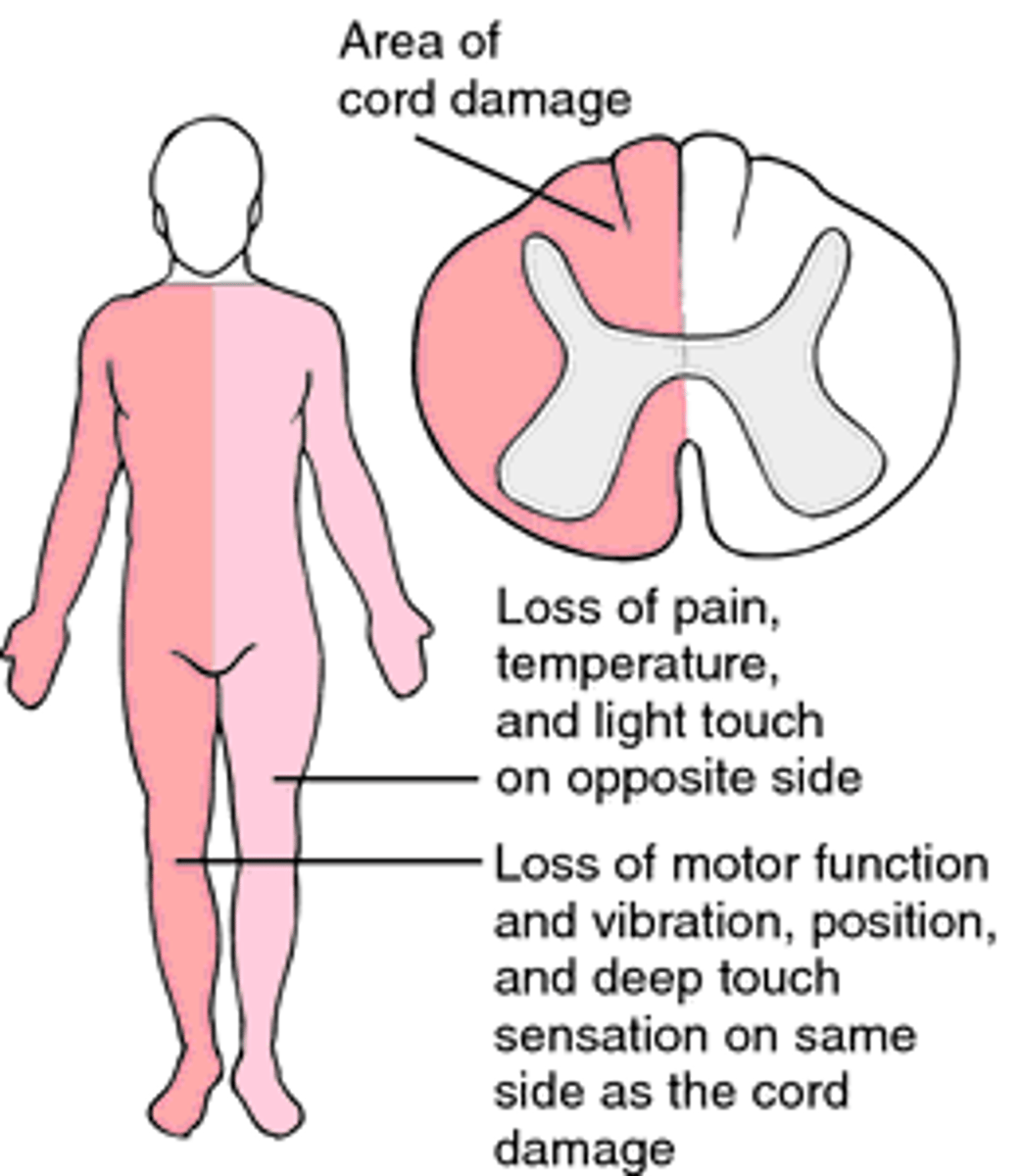
Incomplete SCI - Brown-Séquard Syndrome
o Occurs from penetrating injury
o Ipsilateral loss of motor function from injury
o contralateral loss of pain and temperature sensation from injury
Conus Medullaris Syndrome:
o Damage to lowest portion of the spinal cord
o Motor function can be preserved, weak, or flaccid
o Decrease in sensation and function in the perianal area
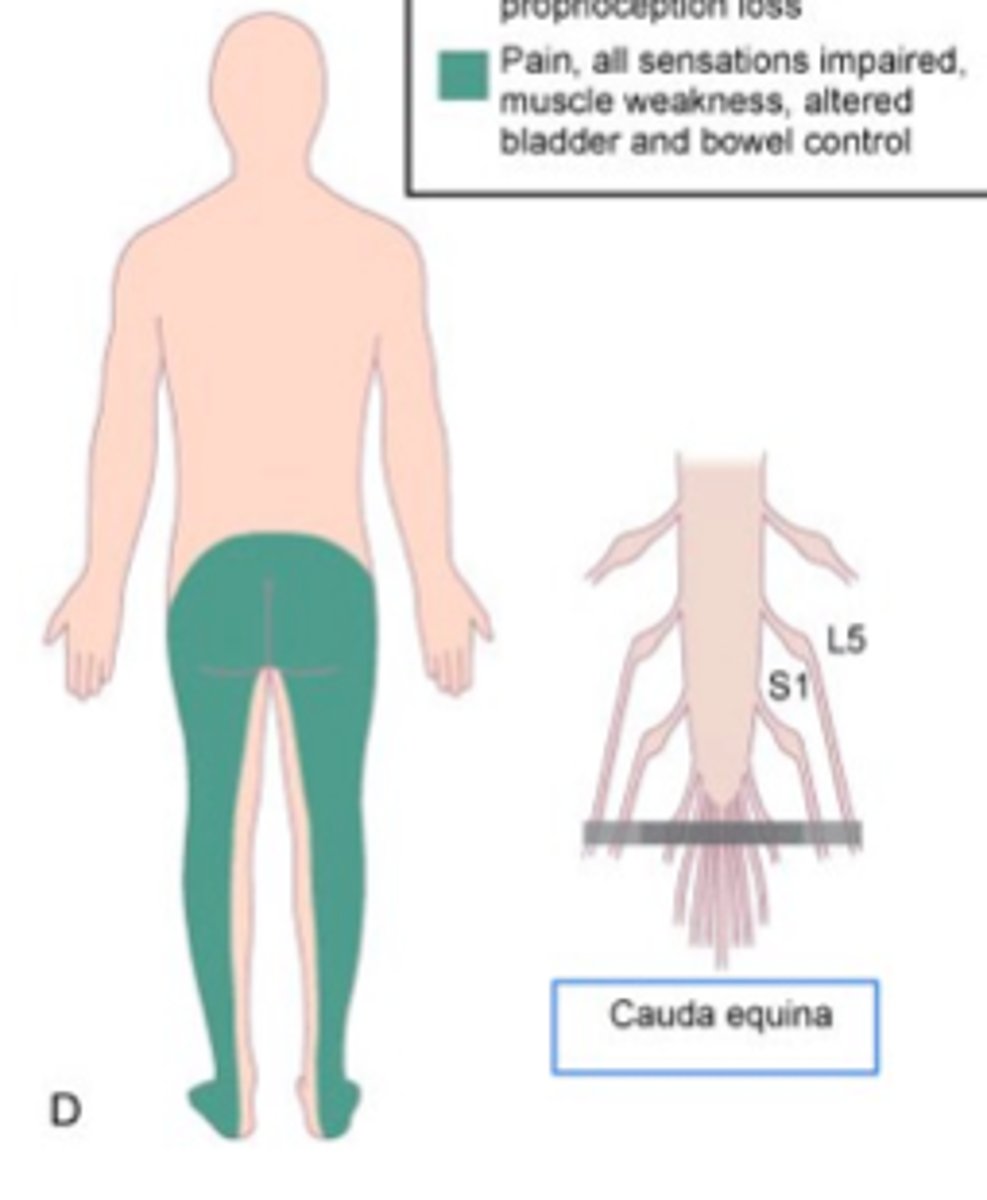
Cauda Equina Syndrome:
o Asymmetrical distal weakness w/ flaccid paralysis of Les
o Loss of sensation in saddle area
o Areflexic bladder and bowel
o Severe pain
Timeline for SCI:
o Within 24 hours, permanent damage may occur because of edema
o Extent of damage and prognosis for recovery most accurately determined 72 hours or more after injury
o Greatest improvement occurs in first 3 to 6 months following injury
Spinal shock:
o s/s: decreased reflex, loss of sensation, absent thermoregulation, flaccid paralysis below level of injury
o lasts days to weeks
o may mask post-injury neuro function
What is neurogenic shock?
o s/s: hypotension, bradycardia, peripheral vasodilation, lowered cardiac output
o generally seen with T6 or higher injuries leading to uninhibited PNS
o treat with norepinephrine to supplement SNS depression
Discuss findings of spinal cord injury at C5 & what functioning the patient will have intact:
o Partial paralysis of the hands and arms as well as the lower body
o Potential quadriplegia
o Bowel and bladder flaccidity
o Diaphragmatic breathing & respiratory insufficiency
o May need help managing secretions
o SNS dysfunction - neurogenic shock
o Poikilothermism - inability to sweat or shiver below level of injury (common with high cervical injuries)
Discuss findings of spinal cord injury at C8 & what functioning the patient will have intact:
o Damage to nerves between C7 and T1
o Potential quadriplegia
o Bowel and bladder flaccidity
o More function in hands & arms
o SNS dysfunction - neurogenic shock
Discuss findings of spinal cord injury at T1 & what functioning the patient will have intact:
o Partial or full paralysis of the lower part of the body
o SNS dysfunction - neurogenic shock
Discuss findings of spinal cord injury at T10 & what functioning the patient will have intact:
Partial or full paralysis of the lower part of the body
What is the highest injury that you can expect a patient to have full function of their UEs?
T6
Autonomic dysreflexia:
o Seen in patients with injuries higher than T6
o Massive uncompensated cardiovascular reaction mediated by sympathetic nervous system
o SNS responds to stimulation of sensory receptors - parasympathetic nervous system unable to counteract these responses.
o S/S: HTN, bradycardia, throbbing headache, flushing above point of injury
o MEASURE PAITENT BP WHEN COMPLAINING OF HEADACHE
o Elevate HOB to 45*, notify HCP, assess for & remove stimulus, treat BP
Care of neurogenic bowel:
o Bowel program started during acute care
o Daily rectal stimulant @ regular time or manual evacuation
o NG suctioning (monitor for metabolic alkalosis - monitor sodium & potassium)
Care of the neurogenic bladder:
o Bladder dysfunction due to absent or decreased bladder innervation
o Acute Phase: urinary retention -> insert foley
o Post-Acute Phase: failure to store urine -> straight cath regimen
o Straight Cath regimen:
- 4-6x/day (Q4HRS)
- Keep urine residuals < 500mL
Care of traction pin site:
o Cleansing with ½ strength peroxide and normal saline twice a day
o Applying antibiotic ointment
Leading cause of death to SCI patients:
pulmonary embolism
A patient presents with back pain that worsens with activity. What condition does the nurse connect this symptom to?
spinal cord tumor