Alveolar Hemorrhage and Pulmonary Vasculitis
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
19 Terms
What is Alveolar Hemorrhage?
Alveolar Hemorrhage is bleeding into the alveolar space
→ caused by a disruption of the alveolar capillary basement membrane or by inflammation of the arterioles, venules or alveolar septal capillaries
What are the three kinds of Alveolar Hemorrhage?
Pulmonary Capillaritis
Bland Hemorrhage
Diffuse Alveolar Damage
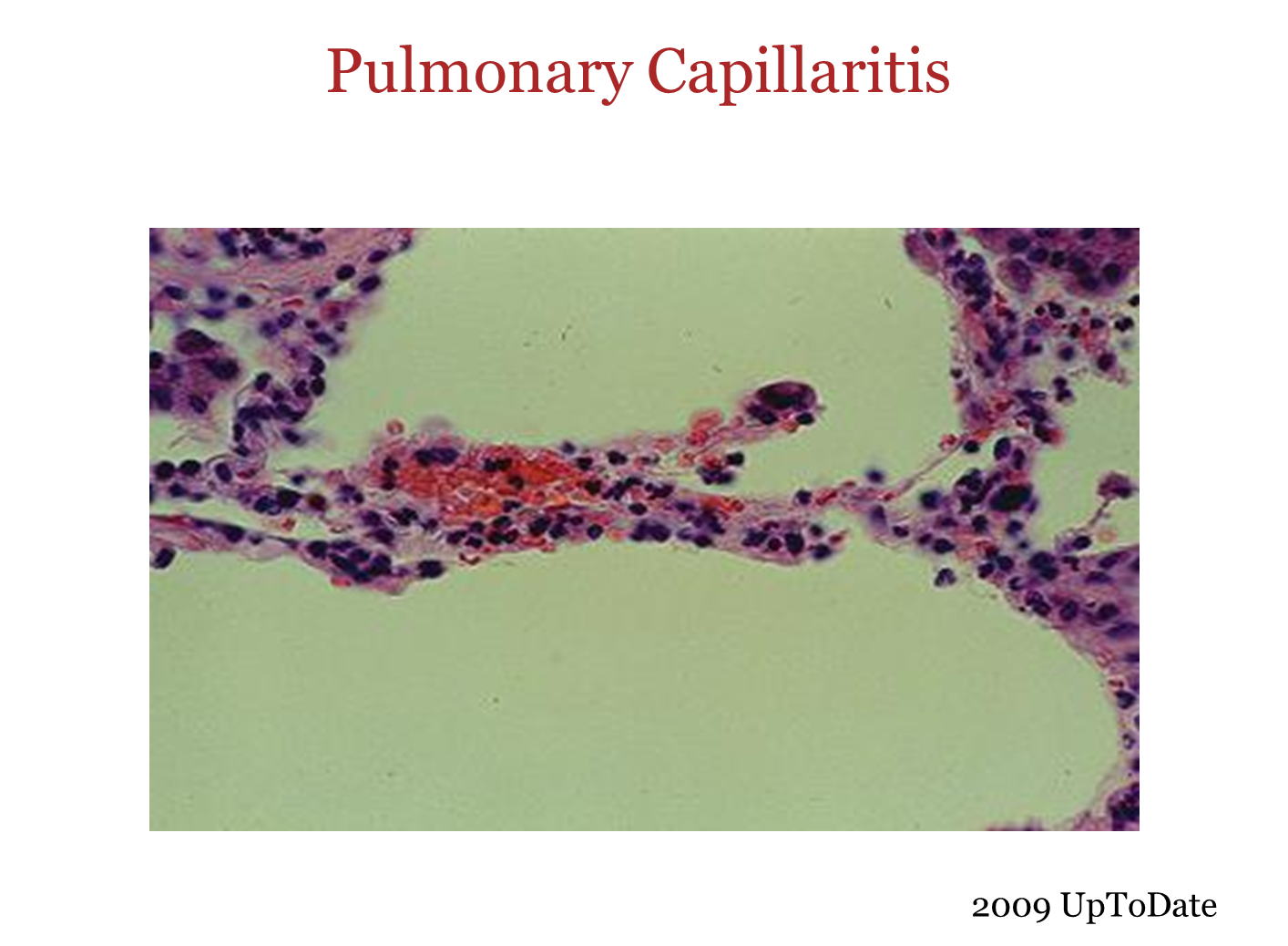
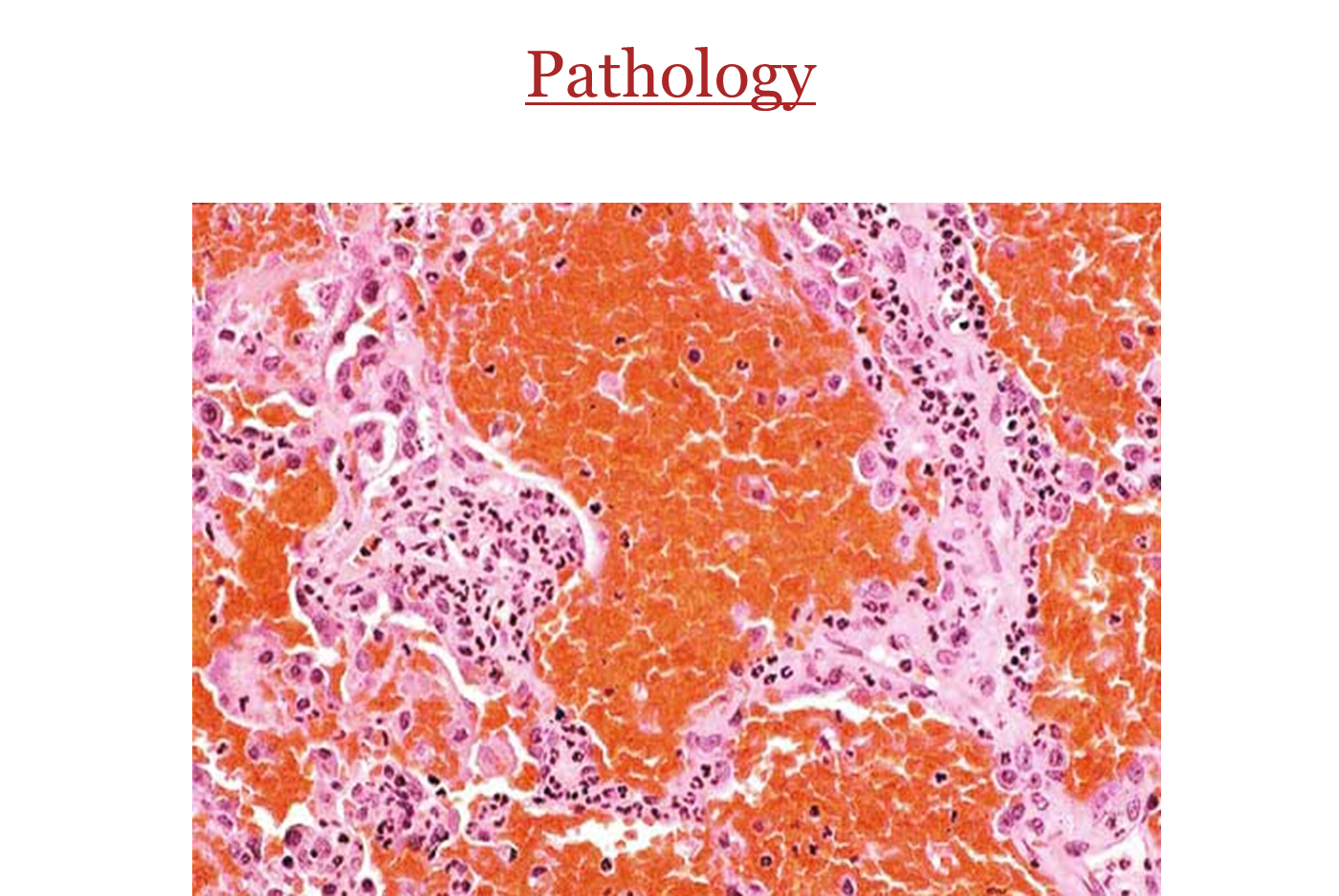
What is Pulmonary Capillaritis
A form of alveolar hemorrhage where there is neutrophilic inflammation which will destroy the capillaries as they become inflammed leading to blood leaking into the alveolar spaces
→ the abundance of blue dots below show the high level of neutrophils and inflammatory cells in the alveoli
What is Bland Pulmonary Hemorrhage
Type of alveolar hemorrhage
→ hemorrhage into alveolar space without inflammation or destruction of alveolar structures
→ caused by a defect in the capillary basement membrane causing blood to leak out into the alveolar space
How do Alveolar Hemorrhage present typically? (symptoms, physical exam, PFT, Labs)
Alveolar hemorrhage will typically present abruptly with a rapid onset
→ patients will cough and may have hemoptysis (but not necessary)
→ patients with systemic issues causing alveolar hemorrhage may have fever
Patients may have some for of systemic disease sign on physical exam. If they do, it may be a sign of an autoimmune disorder
→ Uveitis, Arthritis, Skin Rashes, etc
On PFT
→ may see obstructive or restriction depending on the disease
→ will always see an elevated DLCO even though the patient is hypoxemic
Labs
→ decreased hemoglobin
Why is DLCO elevated during alveolar hemorrhage?
During a DLCO test we provide a patient with a small amount of carbon monoxide, and we monitor how much carbon monoxide the patient breathes back out
→ if the patient breathes less back out, it means they have a higher level of diffusion
→ bleeding into the alveolar space will cause the carbon monoxide to bind to the blood in the alveoli, making it seem like diffusion is higher when it actually is not
What would you see for a patient with alveolar hemorrhage using a broncho-alveolar lavage
Broncho-alveolar lavage will confirm a diagnosis of alveolar hemorrhage
→ bronchoscope will enter into the bronchial and inject saline and aspirate it back a few times - you would see the aspirate become steadily more clear to pink to red
→ You would see progressively bloody aliquots on serial effluents
What is the c-ANCA and p-ANCA lab test?
When you have a patient that has alveolar hemorrhage you need to confirm whether the issue is immune mediated or not. so we check for two types of antibodies (anti neutrophil cytoplasmic antibodies)
1) c-ANCA
→ auto antibodies directed against serine proteinase 3
→ means the hemorrhage is caused by granulomatosis with polyangiitis
2) p-ANCA
→ auto antibodies directed against myeloperoxidase
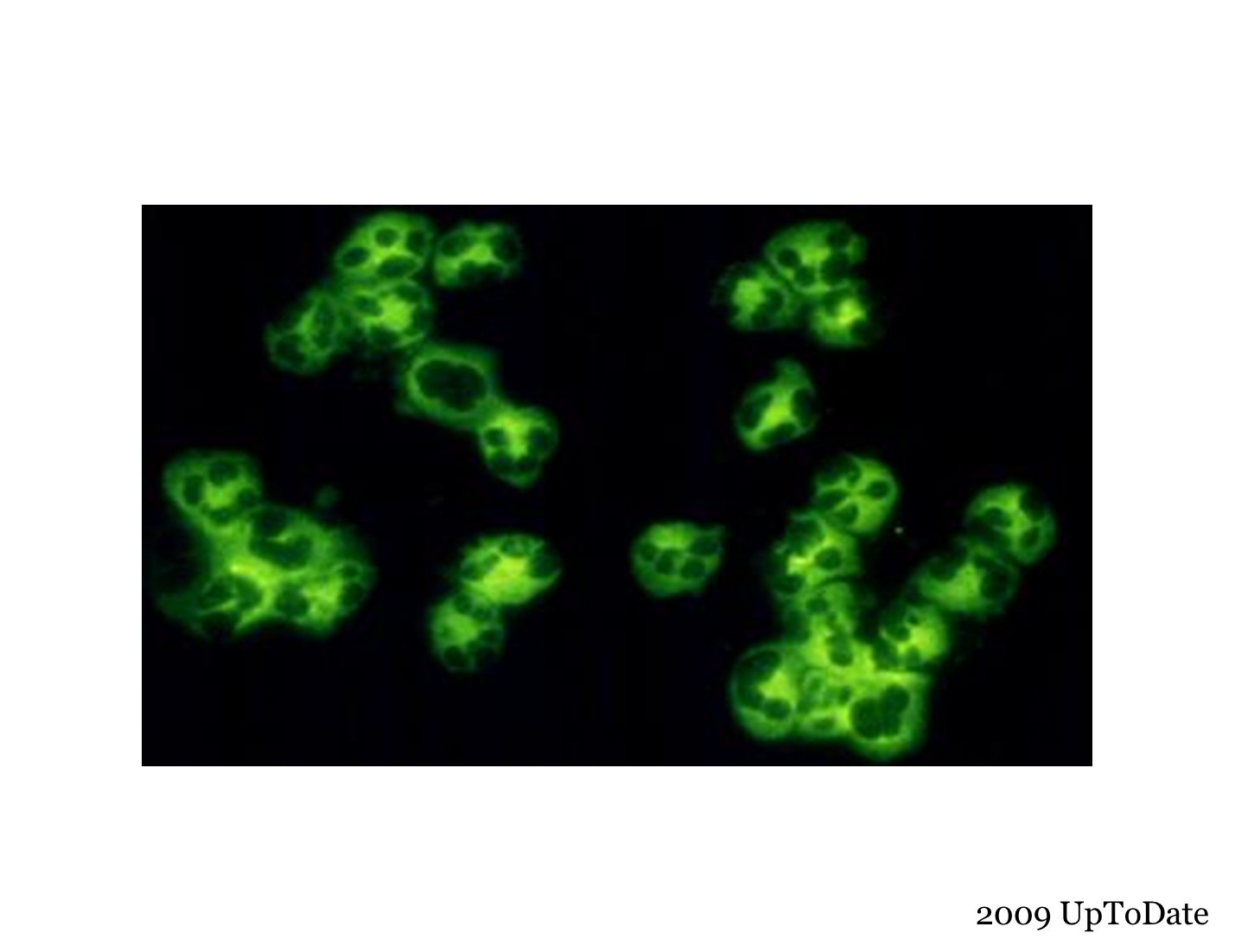
Which pattern is this?
C-ANCA Pattern
→ because the auto-antibodies are directed against the serine-proteinase-3, you would see the fluorescence pattern outside or around the neutrophils, distal to the cytoplasm
→ associated with Granulomatosis with polyangiitis
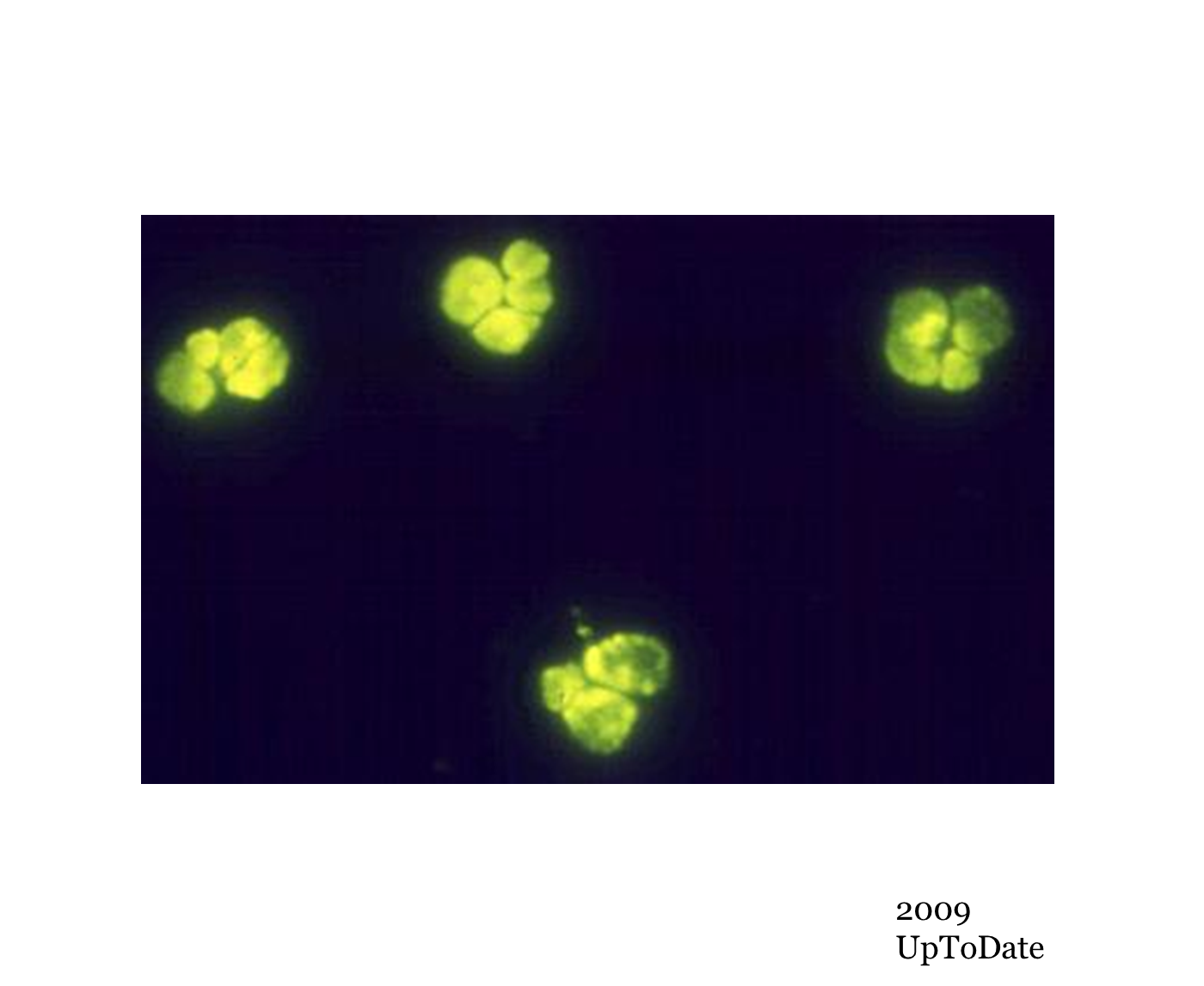
Which pattern is this?
This the P-ANCA Pattern
→ all the antibodies are located right around the nucleus, because they are directed against myeloperoxidase
What is the Anti-Glomerular Basement Membrane Antibodies test?
When you have alveolar hemorrhage that you suspect is caused by good pasture syndrome you would test for circulating Ab against antigens in the glomerular basement membrane
→ antibodies are directed against the NC1 domain of the alpha-3 chain of type IV collagen which is only expressed in the lungs and kidney which causes bleeding in both the lung and kidney
What is Anti-Glomerular Basement Disease
Also known as Good-Pasture’s Disease, it is a Type II autoimmune disease
→ caused by circulating anti-glomerular basement membrane antibodies which will cause bleeding in both the lungs and the kidney
→ typically found in young men below the age of 30
What is the clinical presentation of Anti-Glomerular Basement Disease
1) Most commonly associated with glomerulonephritis
→ hematuria
→ RBC casts
→ renal insufficiency
2) Alveolar Hemorrhage will occur in most patients
Importantly the disease will lack systemic symptoms because the auto-antibodies are directed against a protein only found in the lung and kidneys
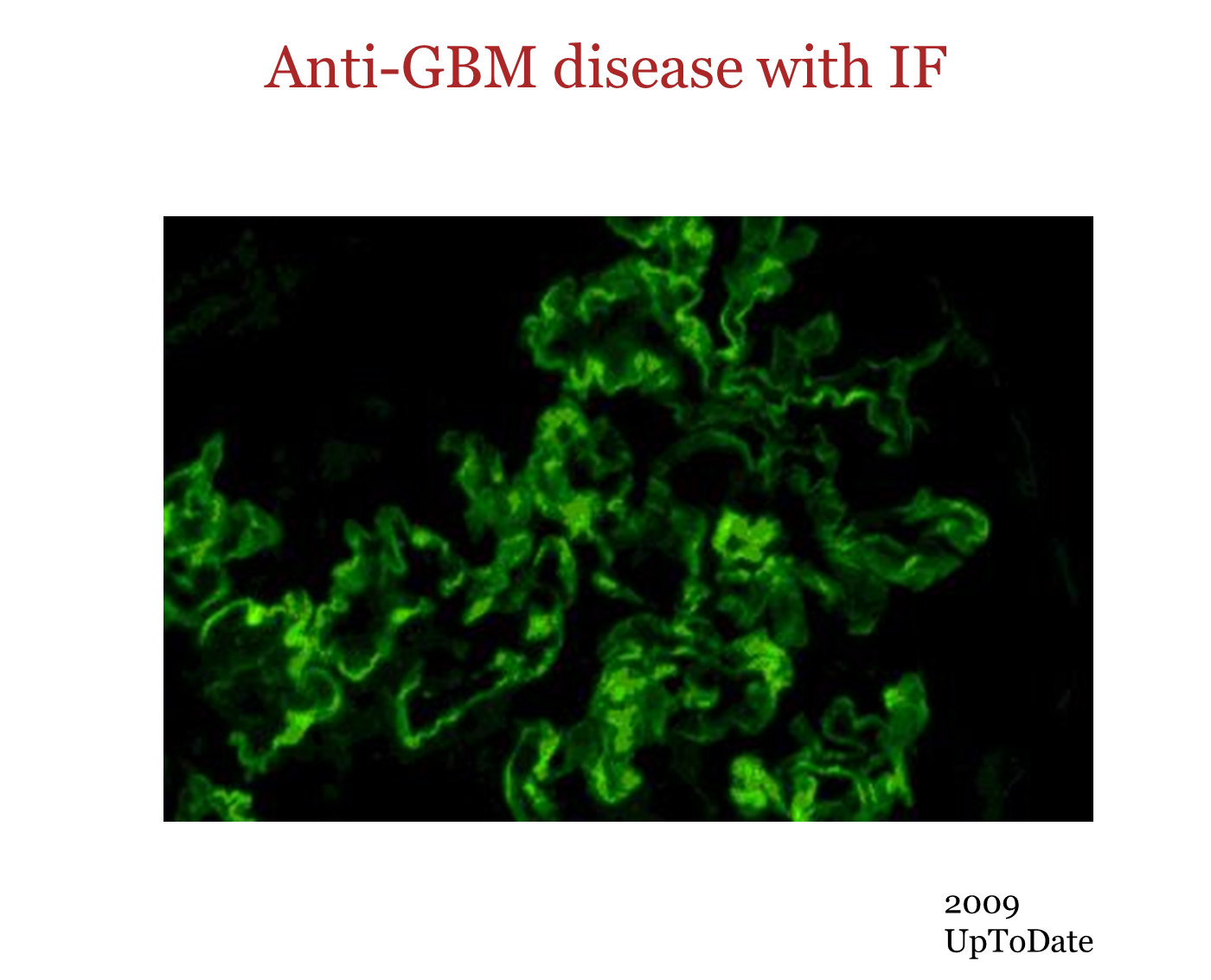
How would you diagnose Anti-Glomerular Basement Disease? What would you see upon renal biopsy
Elevated serum anti-GBM antibodies (greater than 90 percent)
→ 1/3 of patients may also have serum p-ANCA antibodies which makes them more prone to alveolar hemorrhage
→ renal biopsy which will show linear deposition of IgG antibodies along glomerular capillary basement membranes
What is Granulomatosis with Polyangiitis (GPA)
Also known as Wegner’s Granulomatosis, is systemic necrotizing granulomatous vasculitis that involves the upper and lower respiratory tract and kidneys
→ while the disease can present without lower respiratory disease, you need to have upper respiratory disease in order to be classified as GPA
→ most common in young white males
Why is Granulomatosis with Polyangiitis (GPA) systemic
The auto-antibodies that cause Granulomatosis with Polyangiitis will be the C-ANCA Neutrophils of the blood. The disease is systemic, and may cause non-specific issues
1) this means that they will affect a ton of other organs such as…
→ Joint pain - Arthritis
→ Eyes - Uveitis
→ Skin - Rashes
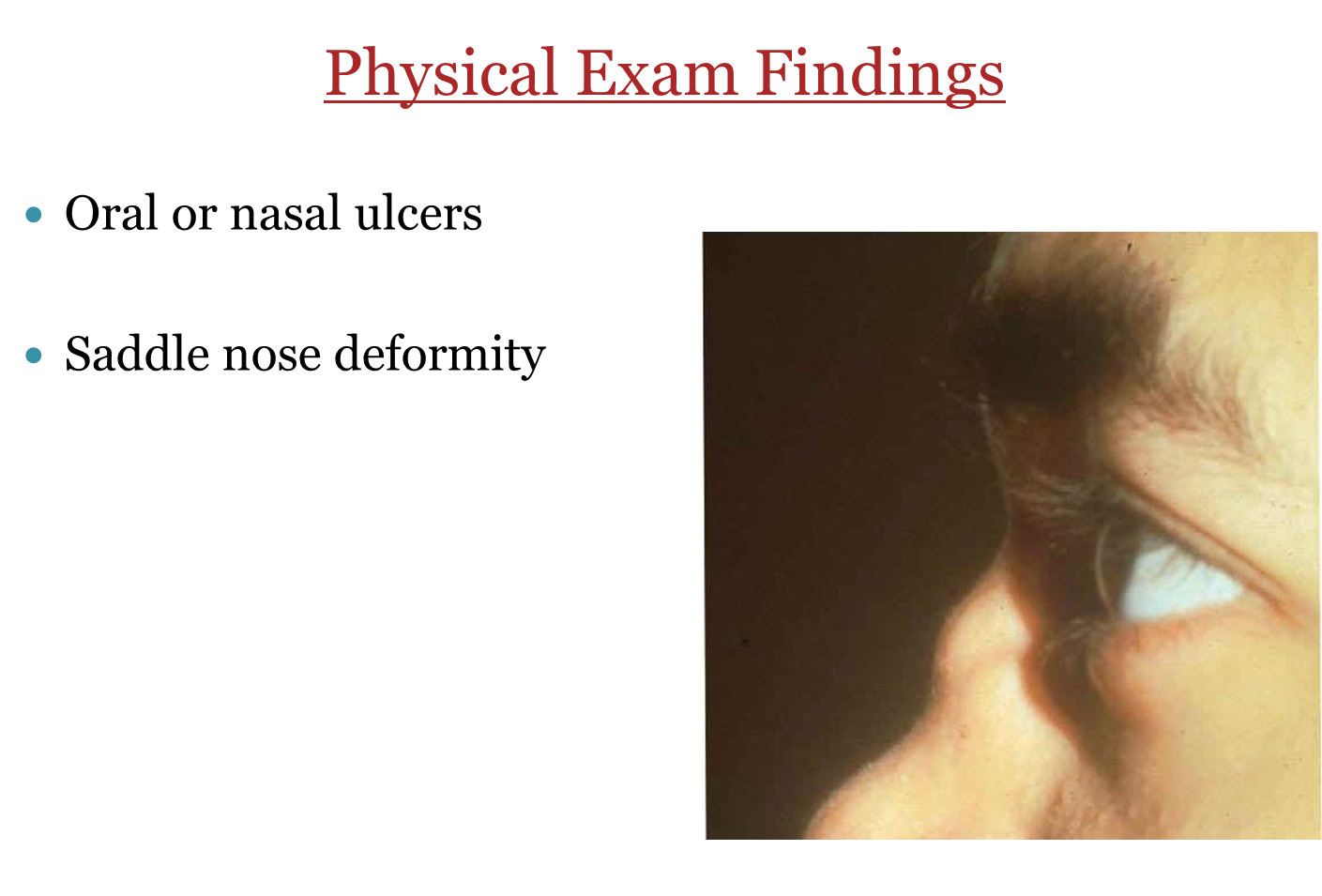
What is the Saddle Nose Deformity?
Saddle Nose Deformity is where the nasal bridge collapses causing a saddle-like appearance
→ caused by Granulomatosis with polyangiitis or Wegener’s Disease
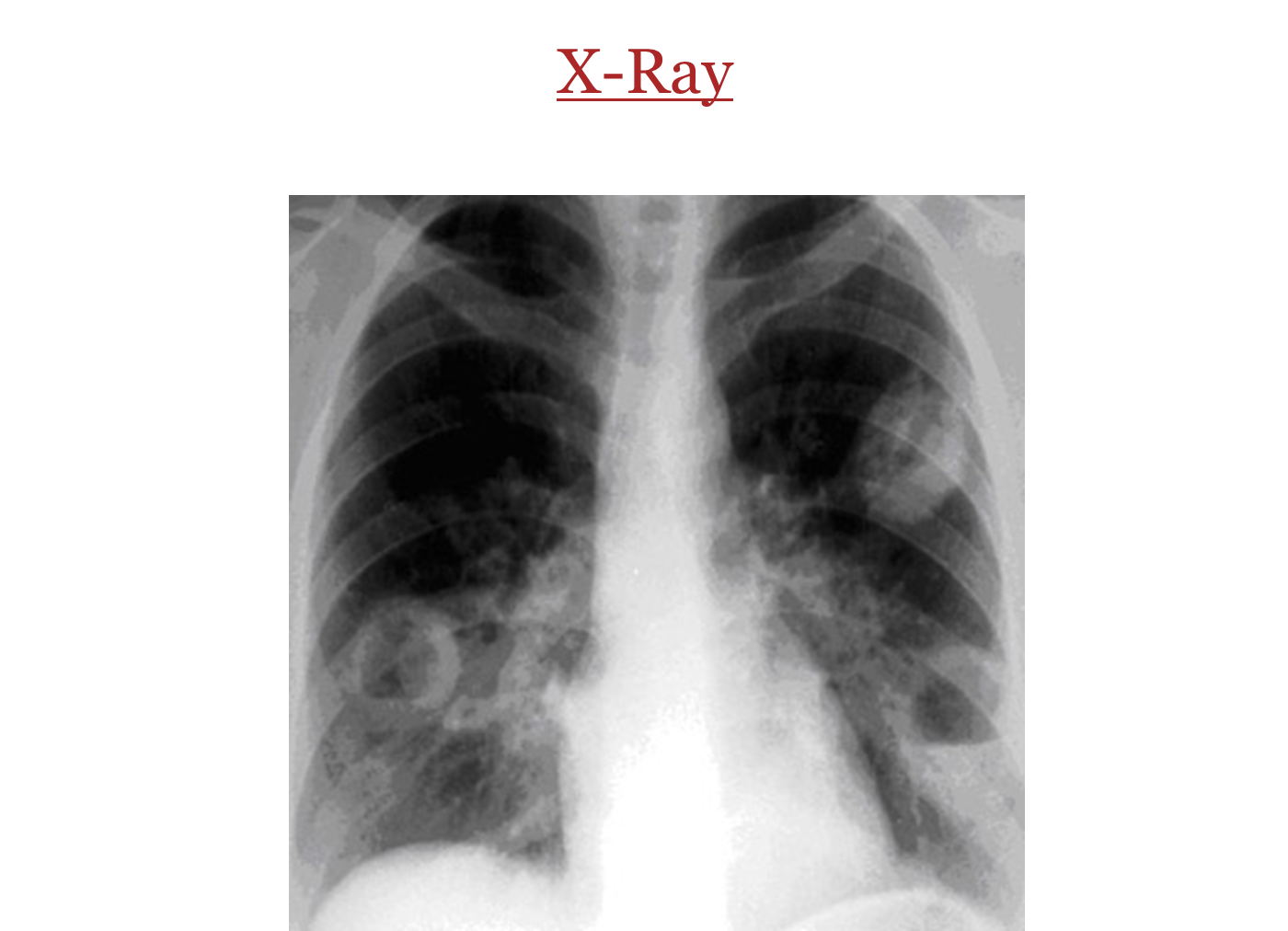
What radiography may be associated with Granulomatosis with polyangiitis
Nodules which may cavitate
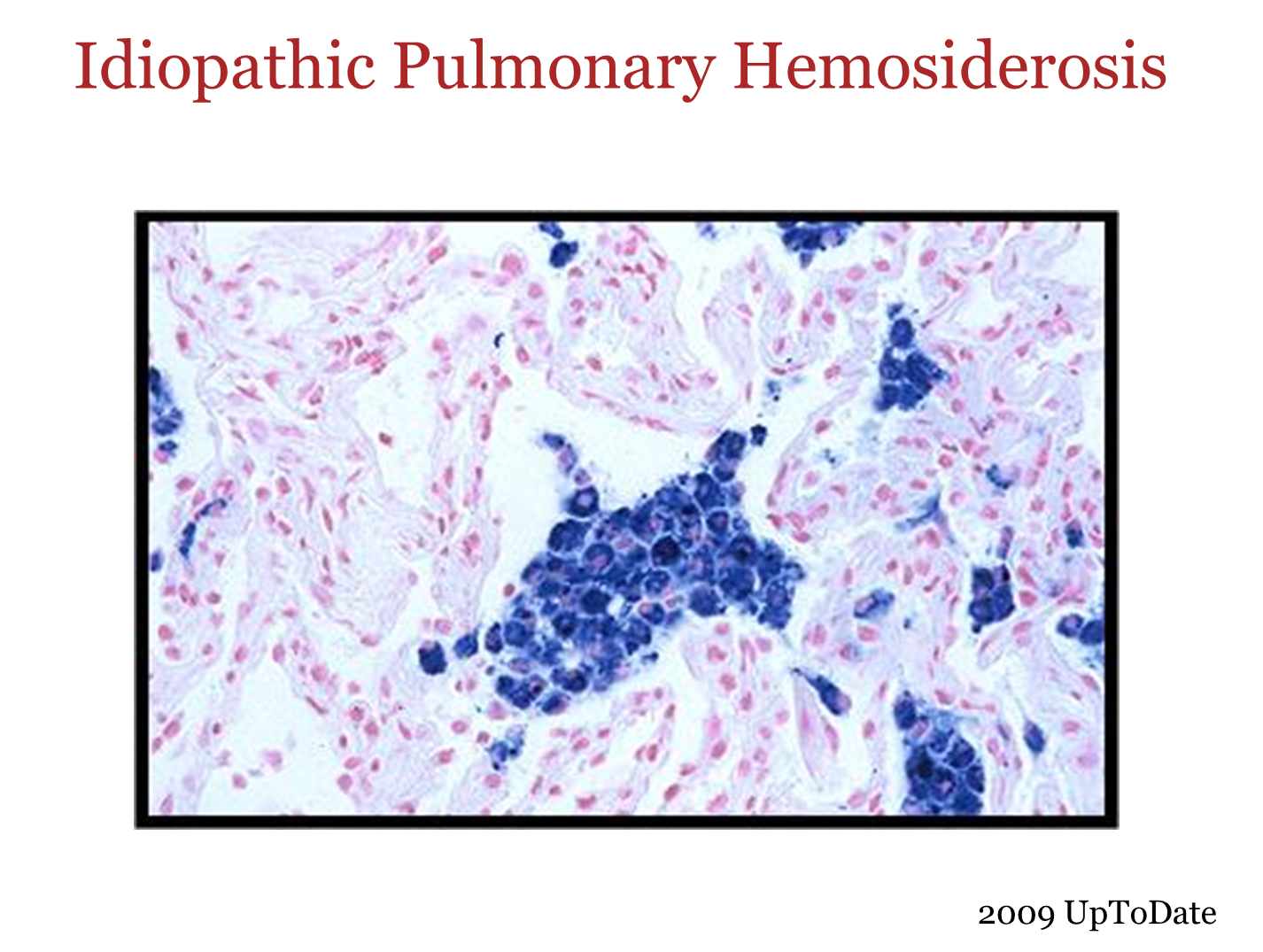
What is Idiopathic Pulmonary Hemosiderosis
Disease of very young children which is a structural defect of the alveolar capillaries basement membranes resulting in bland alveolar hemorrhage
→ you would see recurrent hemorrhage without immune complexes
→ may cause presence of free iron in pulmonary tissue resulting in fibrosis