OD 621 Ocular Anatomy Final
1/494
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
495 Terms
vitreous body
Clear gel in the posterior compartment of the eye.
-largest single struture of the eye
-occupies ~80% of the eyeball's volume
Where does the vitreous body lie in the eye?
Between the lens and the retina.
vitreous body function
Light transmission medium from the lens to retina.
Shock absorber with viscoelastic properties.
UV light filter, especially between 300–350 nm.
Storage and transport of metabolites for lens and retina.
vitreous body boundaries
Anterior: Posterior lens surface Canal of Petit (retro-zonular region)
Peripheral & Posterior: Pars plana, retina, optic nerve
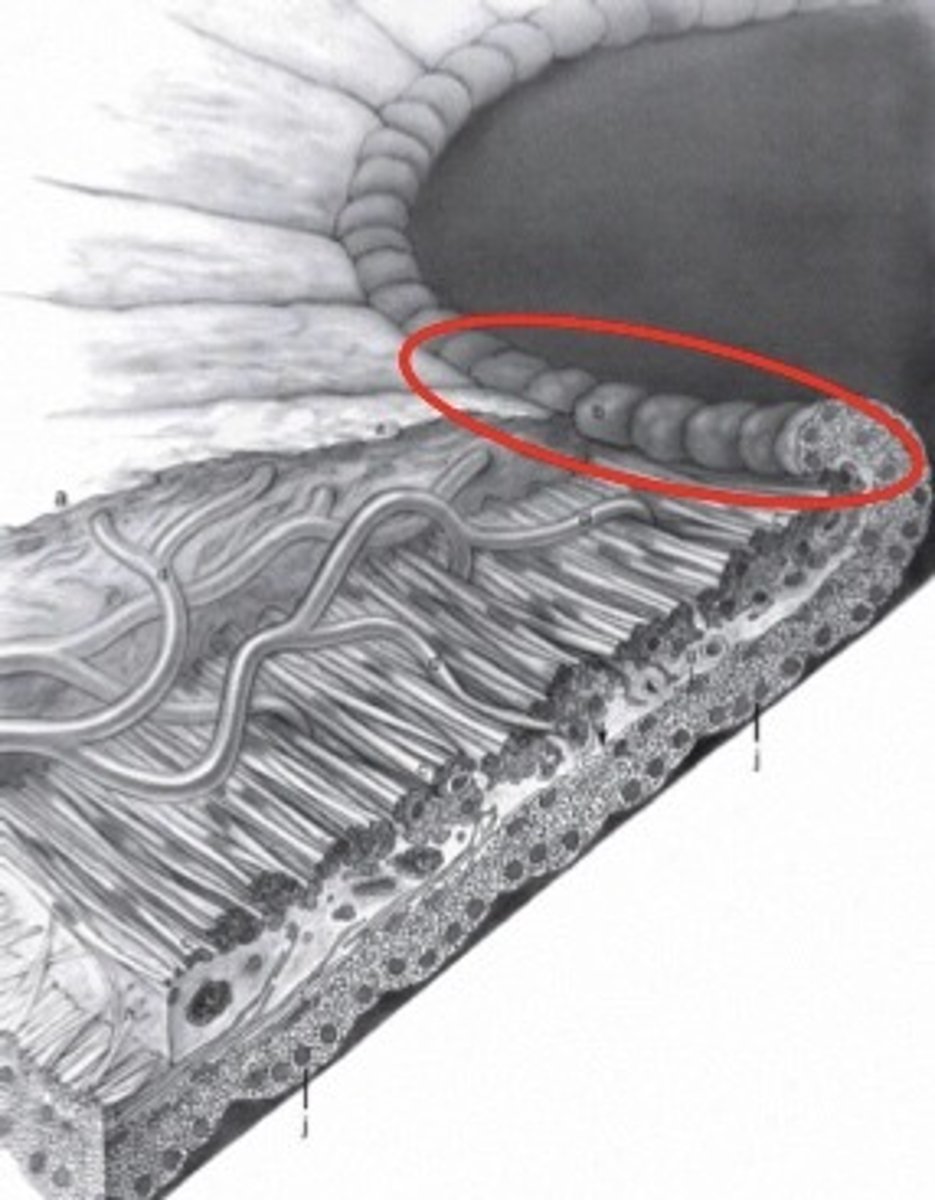
Vitreous Base
strongest vitreous body attachment
-At Ora Serrata
-Attached to ciliary body epithelium & peripheral retina ILM
-Collagen oriented orthogonally
-Does not weaken with age
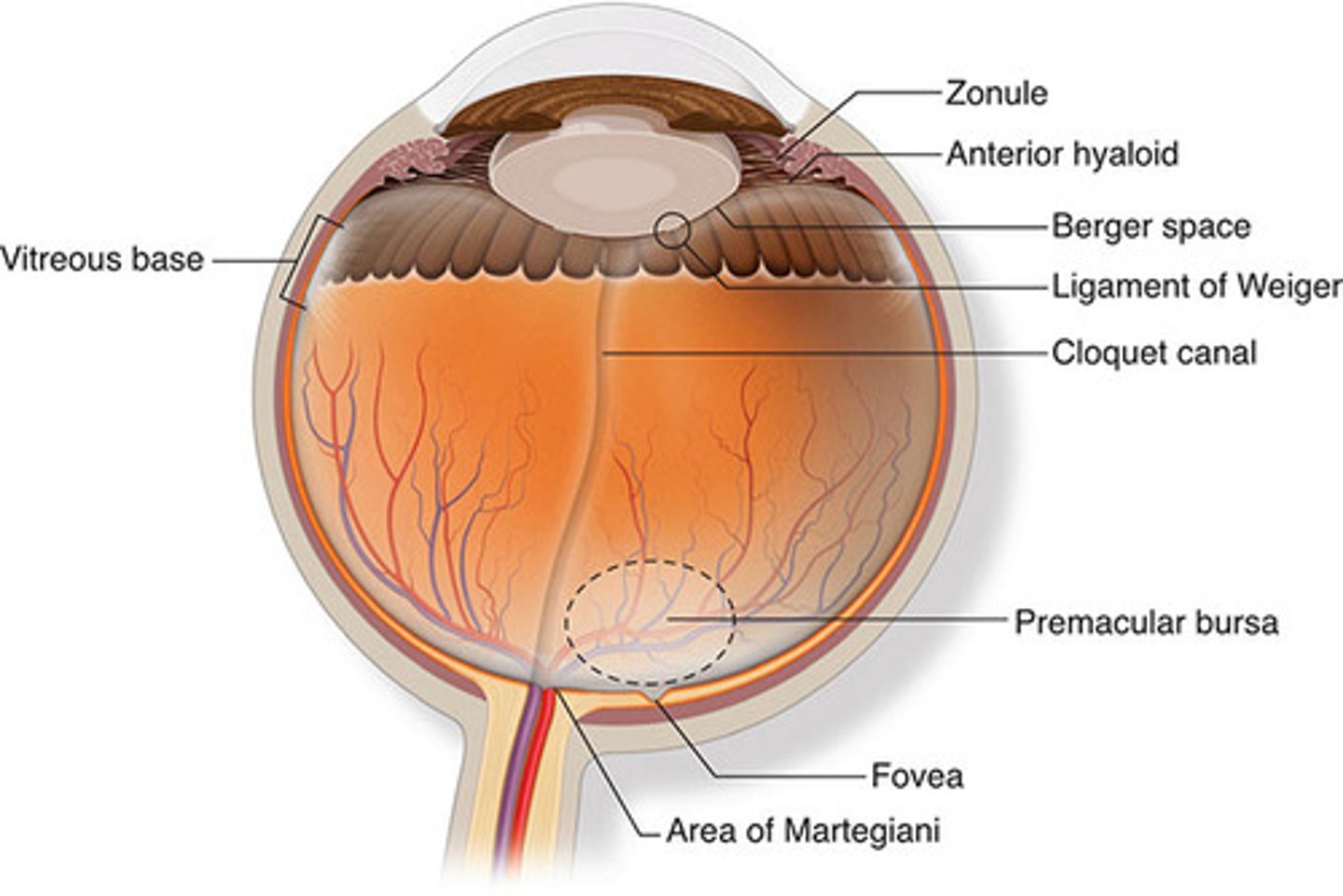
Weiger's Ligament
retrolental vitreous attachment
-Between posterior lens capsule & anterior vitreous cortex
-Forms Patellar Fossa
-Forms a ring enclosing Space of Berger (potential space)
-Weakens with age
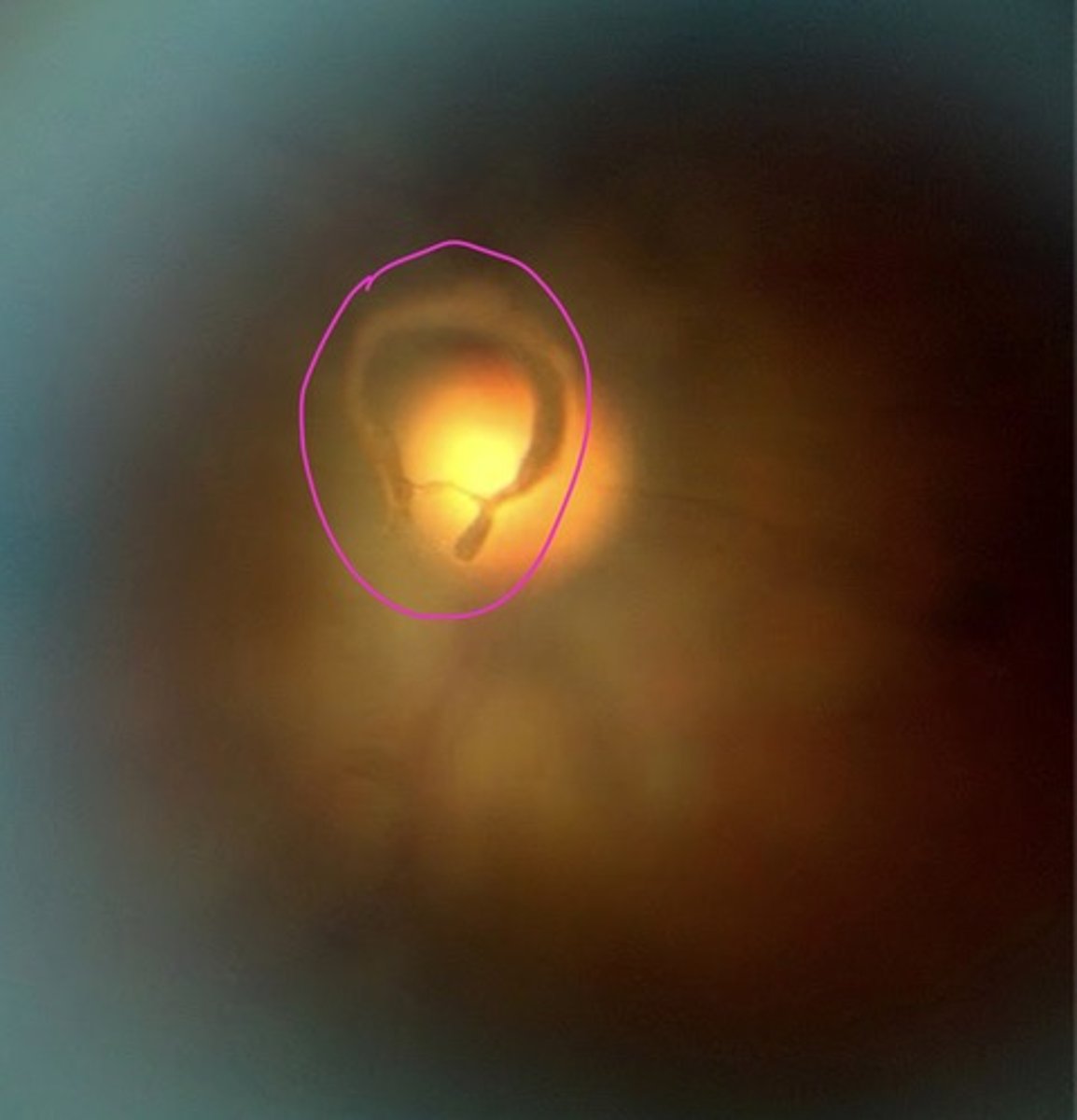
Cloquet's Canal
-Remnant of embryonic hyaloid artery
-1–2 mm wide central channel
-Surrounded by secondary vitreous
-Ends at Area of Martegiani near optic nerve
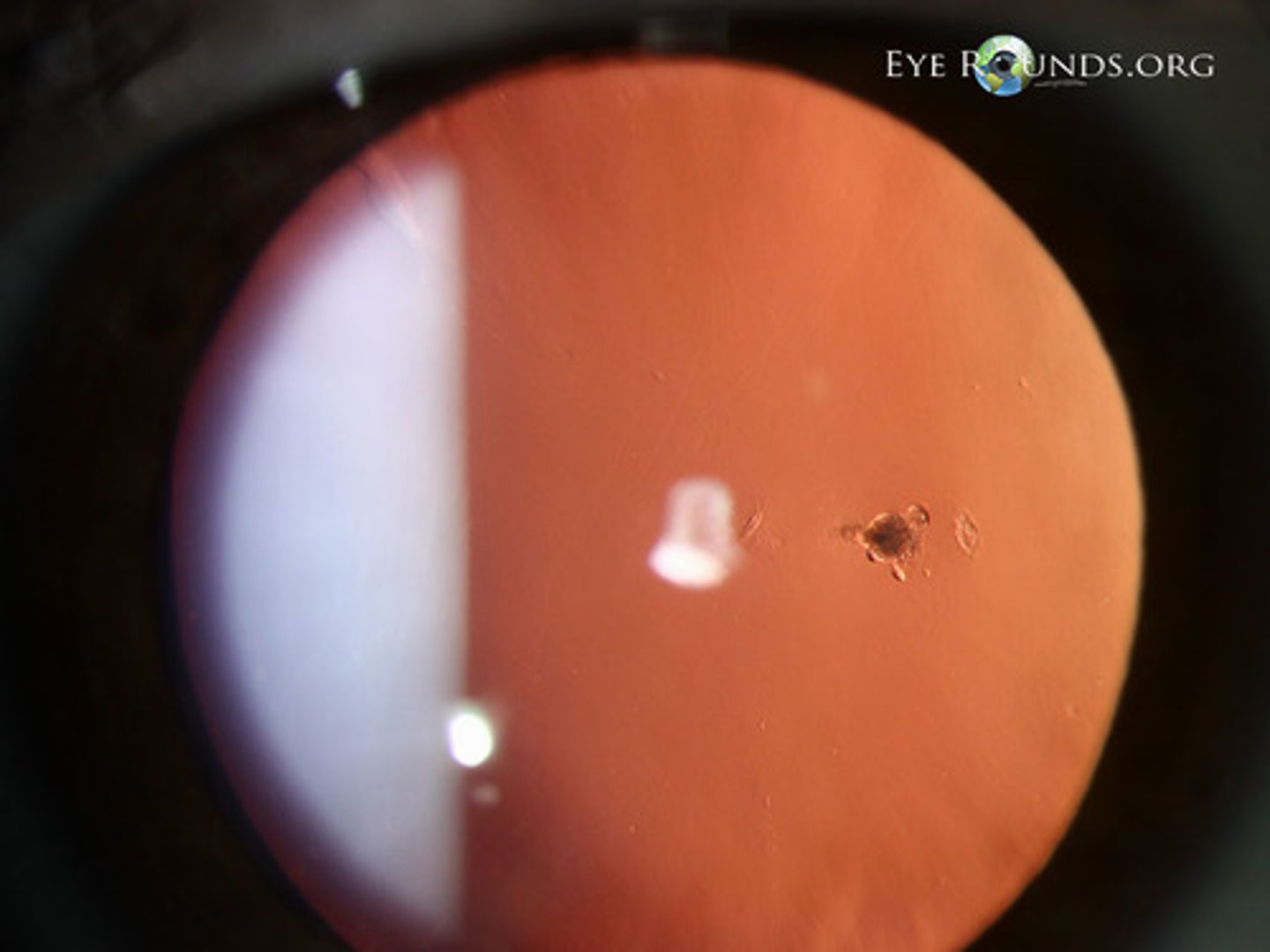
Mittendorf's Dot
small circular opacity on posterior capsule of lens (anterior attachment)
Bergmeister's Papilla
small tuft of fibrous tissue that remains at the optic disc (posterior attachment)
Peripapillary Adhesions
-around the edge of the optic disc
-medium attachment
-weakens with age
Macular and peripheral retinal attachment
-weak attachment
-some individuals have attachment 3-5 mm below vitreous base that attach to retinal blood vessels
Vitreous body structural zones
Cortical Zone (~2%) Peripheral, metabolic activity, contains hyalocytes
Medullary Zone (~98%) Central, cell-free, mostly collagen & HA
Vitreous Cortex
-Anterior Cortex: Near lens, ciliary body
-Posterior Cortex: Near retina (ILM)
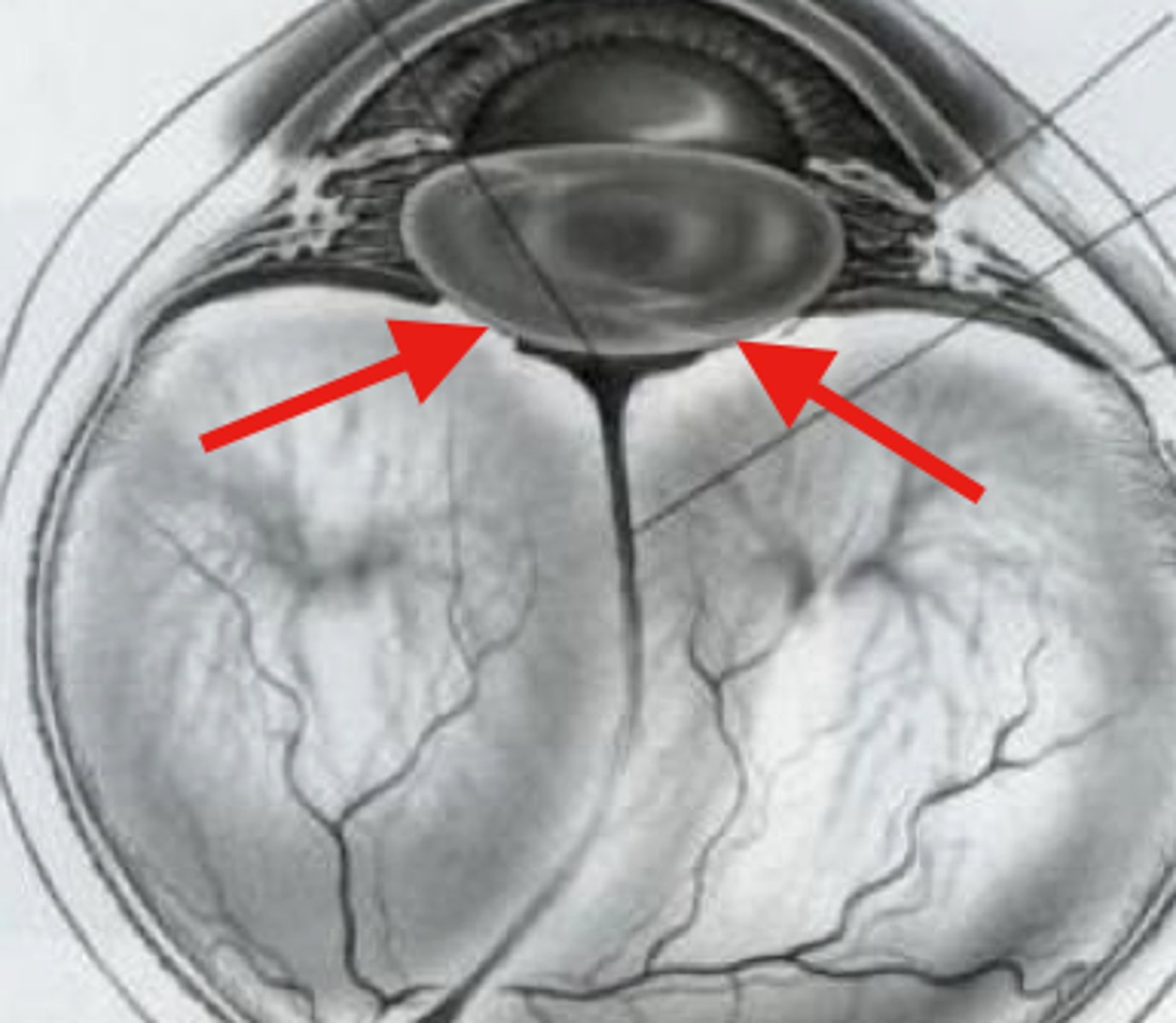
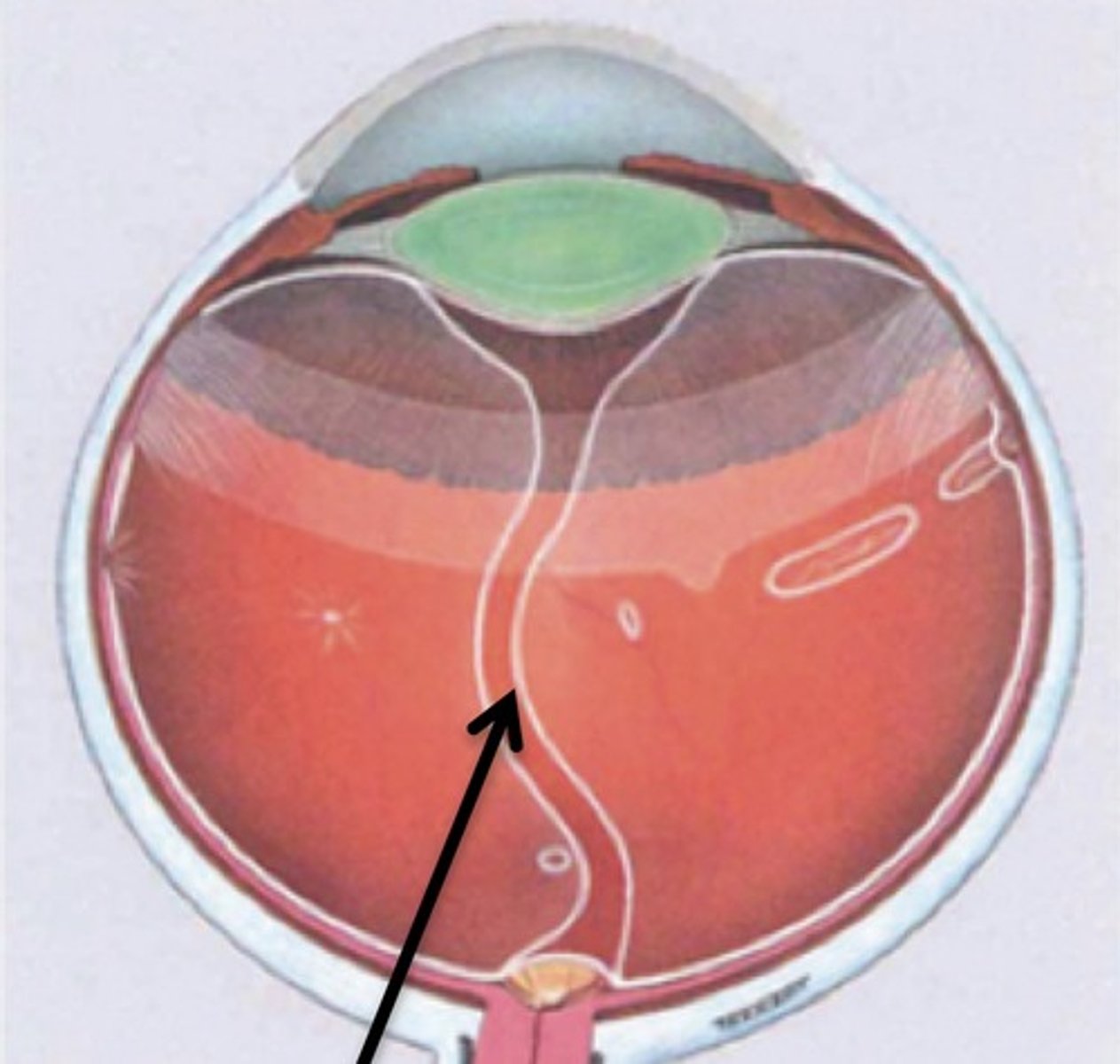
Posterior Vitreous Detachment
Separation of vitreous gel from retina
-Caused by syneresis (liquefaction of gel)
-May lead to:
--Retinal detachment
--Vitreous hemorrhage
--Macular hole
--Epiretinal membrane
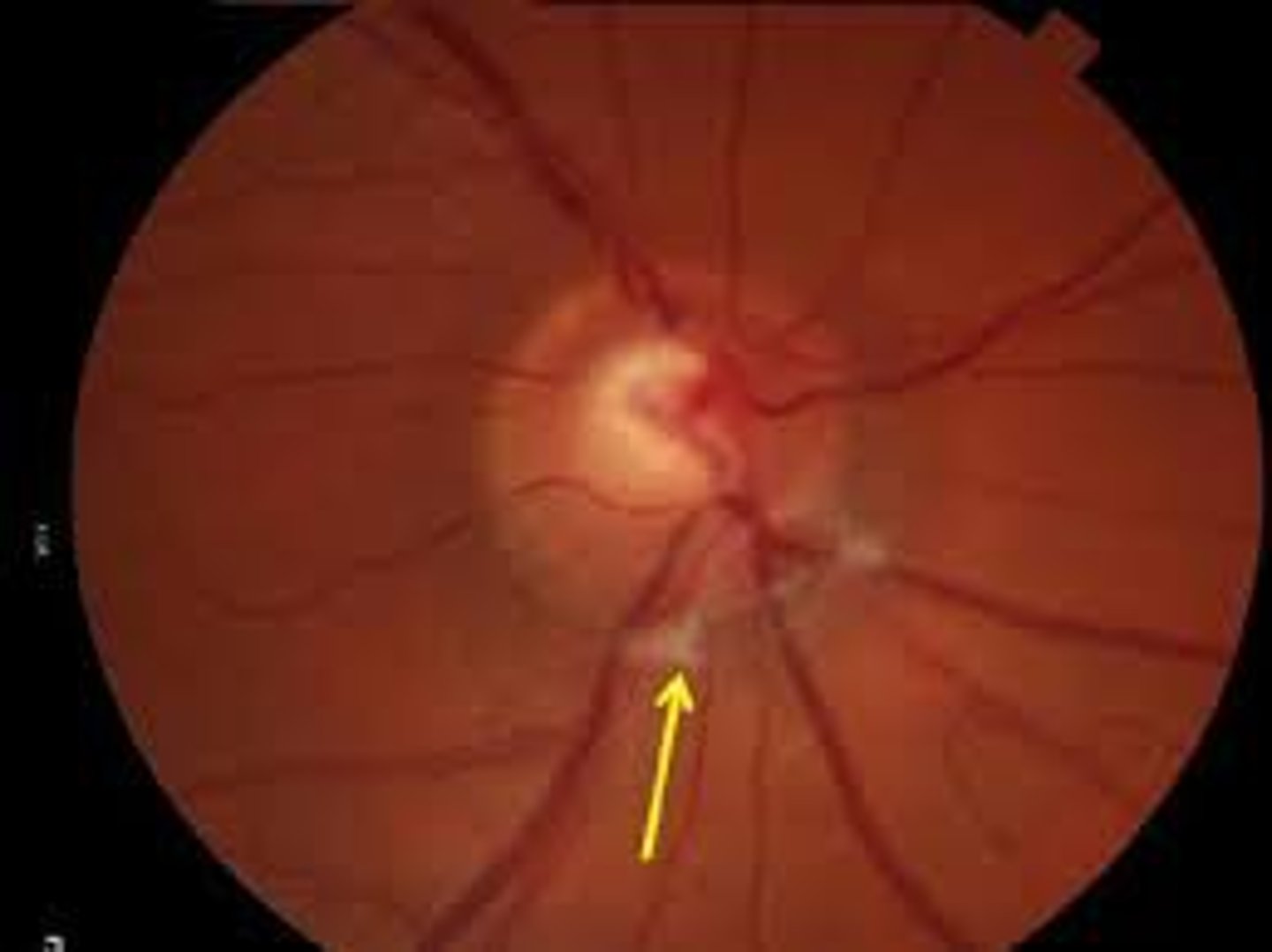
Weiss ring
sign of PVD
-where PVD pulls away from around the optic disc
Vitreous Body water content
98.5-99.7% water
What is the main collagen type in the vitreous body?
Type 2 collagen
-structural scaffold
Vitreous body key molecules
-Hyaluronic Acid (HA): Gel stabilizer, fills gaps between collagen
-Glucose: 30-70 mg/100mL
-Vitamin C: high concentration (antioxidant)
Vitreous body gel properties
-Formed by collagen-HA interaction
-Viscoelasticity arises from their synergy—not from either alone
-Forms channels of liquid vitreous between collagen bundles
Cells of the vitreous body
-Hyalocytes: Make HA & glycoproteins
-Fibroblasts: Make collagen
-Macrophages: Immune surveillance
Syneresis
central liquefaction due to reduced collagen
-leads to PVD and other age-related changes
Iris diamter
~12mm
Iris Circumference ~37-38mm
iris thickness
-Thinnest at iris root (insertion into ciliary body) → ~0.5 mm, prone to tearing
-Thickest at collarette
Iris coloration
depends on melanin concentration, distribution, and type in melanocytes
-Melanin absorption effect:
--Absorbs long wavelengths → reflects short → blue-green appearance
--Absorbs short wavelengths → reflects long → brown appearance
Two melanin subtypes: Eumelanin Pheomelanin
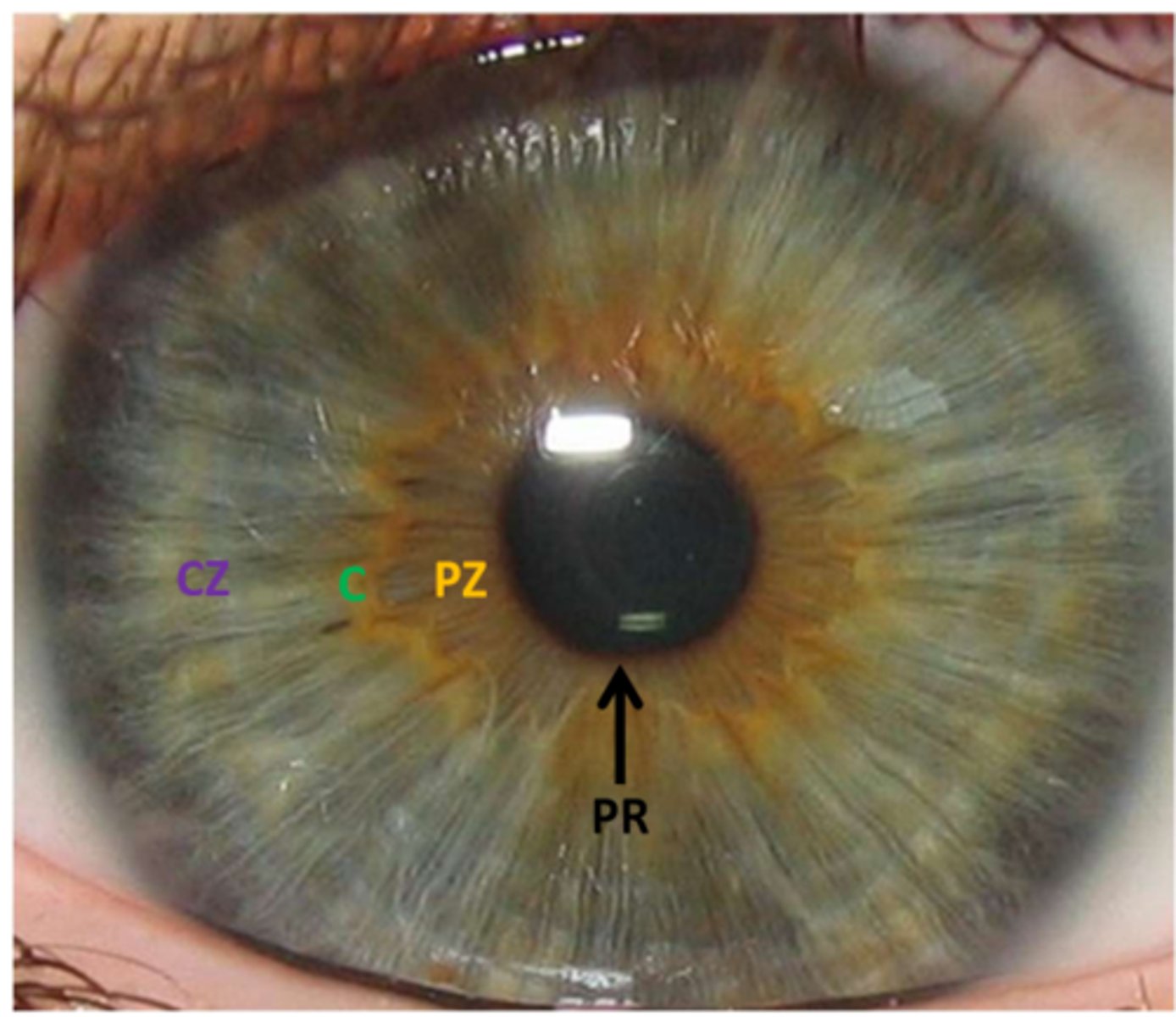
Pupillary Aperture (Pupil)
-Central opening of iris
-Slightly inferior & nasal
-Diameter: 1–8 mm, constantly fluctuates (hippus)
-Controls light entry via miosis (bright light) and mydriasis (dim light)
-Allows unidirectional aqueous humor flow (posterior → anterior chamber)
Pupillary Ruff
Crenated border due to contraction folds of Schwalbe
-Anterior extension of iris pigmented epithelium
Iris collarette
Thickest iris region
-Remnant of embryonic pupillary membrane
-Divides iris into: Pupillary Zone (PZ) → collarette to pupil Ciliary Zone (CZ) → collarette to iris root
Iris root
Thinnest portion (~0.5 mm), peripheral insertion into ciliary body
-most prone to tearing
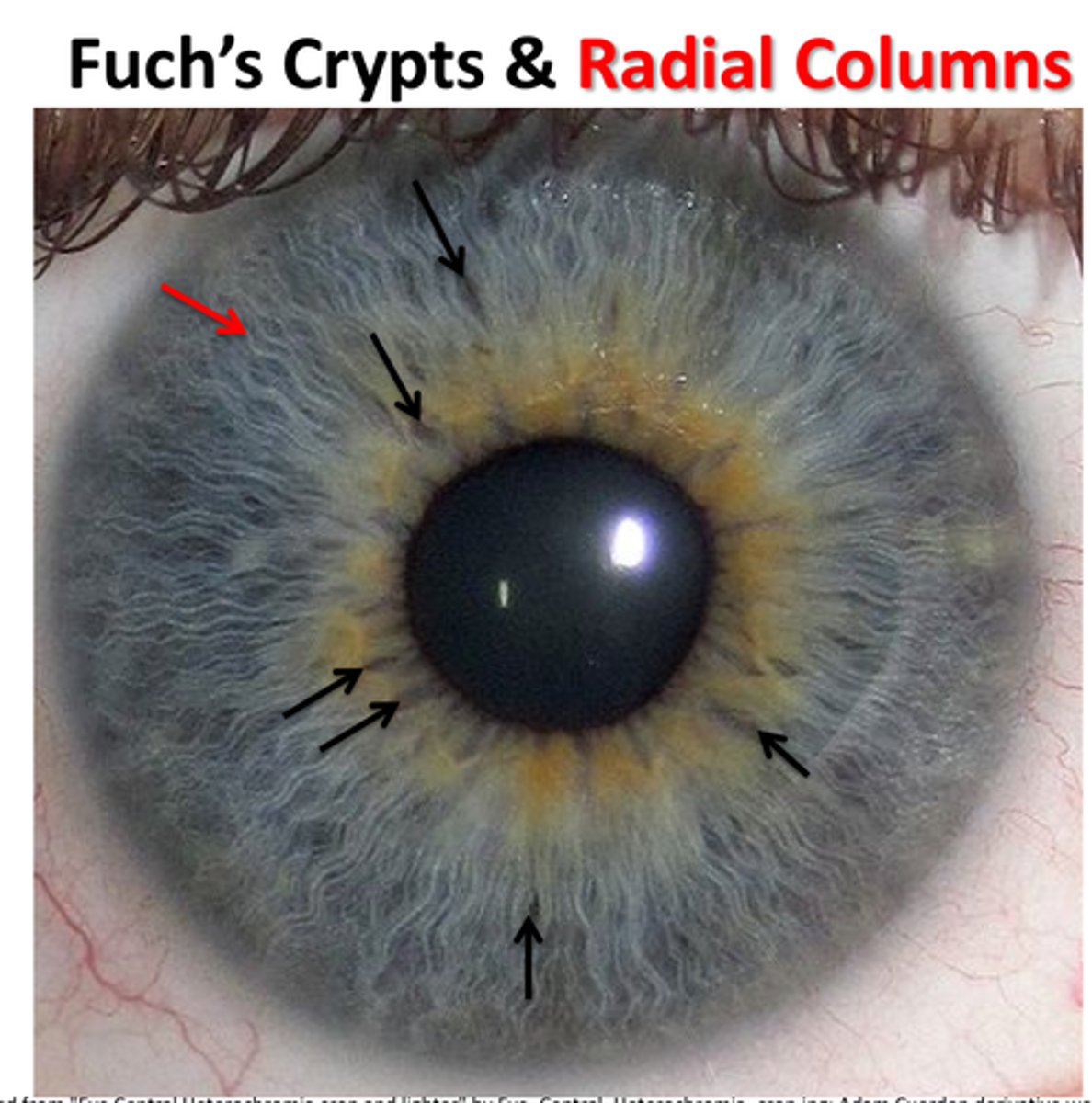
Crypts of Fuch's
Irregular openings near collarette in the anterior border layer of the iris near the collarette
Radial Columns
radial blood vessels encased within collagen in ciliary zone from major arterial circle → minor arterial circle
Collagen prevents kinking during dilation
Contraction folds of Schwalbe
small radial folds in pupillary zone to ruff
-posterior surface
Structual folds of schwalbe
radial folds from ~1.5mm from ruff to Valleys of Kuhnt
-posterior surface
4 layers of the iris
1. Anterior Border Layer
2. Stroma and Sphincter Muscle
3. Anterior Myoepithelium
4. Posterior Pigmented Epithelium
Anterior Border Layer (iris)
-Not epithelium → condensation of underlying stroma
-Contains crypts of Fuch’s (focal defects for aqueous entry into stroma)
-Layers: superficial fibroblasts & deeper melanocytes
-Cell connections: gap junctions, intermediate junctions
-Thickest near pupillary margin
-Firm attachment to iris pigment epithelium
-Usually ends at iris root (may extend as iris processes to Schwalbe’s line)
Iris stroma
connective tissue with melanocytes, clump cells of Koganei (pigment-filled macrophages), fibroblasts, mast cells, lymphocytes, collagen, ground substance, blood vessels, nerves
-Continuous with ciliary body stroma at iris root
Spincter Pupillae Muscle
-0.75–1 mm wide circular smooth muscle in pupillary zone
-Gap junctions connect cells
-Surrounded posteriorly by connective tissue (separates from dilator muscle)
-Fuch’s Spurs: pigmented extensions from dilator muscle to SM
-Function: miosis (parasympathetic, neuroectoderm origin)
Anterior Myoepithelium (iris)
-Origin: inner layer of optic cup (neuroectoderm)
-Two portions in each cell:
--Muscular portion (basal) → forms radial dilator pupillae muscle (dilation, sympathetic, not true smooth muscle)
--Epithelial portion (apical) → pigmented cuboidal cells
-Joined by gap junctions & desmosomes
-Dilator muscle inserts below midpoint of sphincter
Posterior Pigment Epithelium (iris)
-Origin: outer layer of optic cup (neuroectoderm)
-Single layer of cuboidal/columnar pigmented cells
-Intercellular junctions: --Zonula occludens & zonula adherens → tight barrier between aqueous of anterior & posterior chambers (different protein concentrations)
--Gap junctions & desmosomes → between PPE cells and between PPE & AME
Where do radial iris vessels originate?
From the major arterial circle of the iris in the ciliary body stroma.
What is the function of collagen in radial iris vessels?
It prevents kinking during miosis and mydriasis.
What do radial iris vessels appear as?
Radial columns.
What do radial iris vessels anastomose to form?
The minor arterial circle at the iris collarette.
What type of junctions do endothelial cells of radial iris vessels have?
Zonula occludens (tight junctions).
What barrier do the tight junctions in radial iris vessels contribute to?
The blood-aqueous barrier.
What is the venous drainage system for radial iris vessels?
Vortex veins in the choroid.
What surrounds the tunica adventitia of iris vessels?
A collagen sleeve.
What is the purpose of the collagen sleeve around iris vessels?
It prevents kinking during movement.
What type of capillaries are found in the iris?
Non-fenestrated capillaries.
What do tight junctions between endothelial cells in iris capillaries prevent?
Protein leakage into the aqueous humor.
What does the structure of iris capillaries help maintain?
The blood-aqueous barrier.
Ciliary Body
choroid
the posterior part of the uveal tract, between the RPE and sclera
-Rich in blood vessels and melanocytes (which absorb stray light).
-Provides nutrients to photoreceptors and removes metabolic waste from the retina and retinal pigment epithelium
-Accounts for about 85% of the blood flowing through the eye at any given time.
-0.1 to 0.3 mm thick in the region of the central retina and about 0.1 mm in the periphery
Bruch's Membrane
-Devoid of cells
-Extends from the optic disc (thickest) to the ora serrata (thinnest)
-5 layers: Basement Membrane of the Retinal Pigment Epithelium, Inner Collagenous Layer, Elastic Layer, Outer Collagenous Layer, and Basement Membrane of the Choriocapillaris (BMRPE, ICL, EL, OCL, BMC)
-Regulates fluid passage between retina and choriocapillaris
Choriocapillaris
-Fenestrated capillaries
-The basement membrane of the endothelial cell is located on its external surface.
-No tight junctions → allows exchange of nutrients
-Receives blood form medium and large vessels located in the vessel layers of the choroid.
-Distributes blood through a network of hexagonal lobules
-Each lobule forms its own functional vascular unit and consists of a central feeder arteriole, capillaries, and accompanying peripheral venules.
-Arteriolar and venular systems anastomose with each lobule. Anastomoses do not occur between adjacent lobules.
-If one lobule is damaged or destroyed the other lobules will remain intact
Sattler's Layer
Medium vessels that feed the choriocapillaris
Haller's Layer
-Large vessels that feed Sattler’s Layer
-Posterior to the equator → supplied by short posterior ciliary arteries
-Anterior to the equator → supplied by long posterior ciliary arteries and recurrent vessels from the anterior ciliary arteries
Suprachoroid Lamina
-Pigmented sheets of connective tissue originate from the outermost layer of the choroid and span the suprachoroidal space
-Merges with the lamina fusca of the sclera
-Contains muscle stars (epichoroidal stars) which represent the posterior termination of the longitudinal bundle of the ciliary muscle. Located in the anterior suprachoroid lamina
Suprachoroidal Space
potential space, located between the choroid and sclera, for nerve and arteries to travel
-continuous anteriorly with the supraciliary space
-terminates posteriorly at the optic nerve
Choroidal stroma
composed of loose vascular connective tissue interspersed with numerous melanocytes, fibrocytes, macrophages, plasma cells, lymphocytes, and mast cells. Encompasses Sattler's layer, Haller's layer, and the suprachoroid lamina.
What is the arterial supply to the posterior choroid?
From the ophthalmic artery, short posterior ciliary arteries (10-20) enter the suprachoroidal space to supply the posterior choroid.
What is the arterial supply to the anterior choroid?
Long posterior ciliary arteries pierce the sclera just lateral to the short posterior ciliary arteries and travel anterior within the suprachoroidal space to supply the anterior choroid.
How is the vasculature of the choroid regulated?
The vasculature of the choroid is neuroregulated by input from the autonomic nervous system.
How does venous drainage from the choroid differ from arterial drainage?
Venous drainage from the choroid is atypical in that venous blood vessels do not parallel arterial vessels.
Where are venous blood vessels primarily located in the choroid?
Venous blood vessels are found mainly in the large vessel layer.
What are vortex veins?
Vortex veins are larger vessels formed by the merging of venous blood vessels in the choroid.
How many vortex veins are typically present per eye?
There are typically 4-7 vortex veins per eye, with each quadrant having at least one vortex vein.
Where do vortex veins drain?
Vortex veins traverse the sclera via the middle scleral apertures and drain into the superior and inferior ophthalmic vein.
What cranial nerve is responsible for sensory innervation of the choroid?
CN V (Trigeminal)
What are the long ciliary nerves derived from?
The nasociliary branch of the ophthalmic division of CN V.
Where do the nasal and temporal long ciliary nerves pierce the sclera?
3 mm from the optic nerve on either side.
What do the long ciliary nerves supply sensory innervation to?
Bulbar conjunctiva, cornea, anterior sclera, iris, ciliary body, and anterior choroid.
What is the role of the ciliary ganglion in sensory innervation?
It provides passage for sensory fibers from the short ciliary nerves to the nasociliary nerve.
How do short ciliary nerves travel in relation to the optic nerve?
They form a ring around the optic nerve and perforate the sclera.
What structures do short ciliary nerves provide sensory innervation to?
Posterior sclera, choroid, ciliary body, and iris.
What type of autonomic fibers travel with long and short ciliary nerves?
Sympathetic fibers from the superior cervical ganglion.
What effect do sympathetic fibers have when traveling with ciliary nerves?
They cause vasoconstriction.
What type of autonomic fibers travel with short ciliary nerves?
Parasympathetic fibers via the ciliary ganglion.
What effect do parasympathetic fibers have when traveling with short ciliary nerves?
They cause vasodilation.
What is the retinal pigment epithelium (RPE)?
The outermost layer of the retina.
What is the function of the retinal pigment epithelium?
It acts as a barrier between the choroid and retina.
Where is the retinal pigment epithelium present?
Wherever the retina exists.
Is there retinal pigment epithelium at the optic nerve?
No, there is no RPE at the optic nerve because there is no retina there.
From what is the retinal pigment epithelium derived?
It is derived from the outer layer of the optic cup.
How do the RPE and photoreceptor outer segments face each other?
They face apex-to-apex.
What is the subretinal space?
A potential space between the RPE and photoreceptor outer segments.
What fills the subretinal space?
Interphotoreceptor matrix.
What is the structure of the retinal pigment epithelium?
A monolayer of pigmented hexagonal cells.
Where is the retinal pigment epithelium located?
Between the choriocapillaris and photoreceptor outer segments.
How many cells are in the retinal pigment epithelium?
4-6 million cells.
Is the retinal pigment epithelium regenerative?
No, it is non-regenerative.
Where is the highest density of retinal pigment epithelium cells found?
In the fovea, with about 5,000 cells/mm².
How many photoreceptor outer segments does each RPE cell interface with?
30-40 photoreceptor outer segments.
What does the retinal pigment epithelium do with shed discs?
It engulfs shed discs daily: rod discs in the morning and cone discs at night.
Which membrane of the RPE faces the photoreceptor outer segments?
The apical membrane.
What surrounds the photoreceptor outer segments?
Long microvilli from the apical membrane of the RPE.
Which membrane of the RPE faces Bruch's membrane?
The basolateral membrane.
Outer zone of RPE
contains mitochondria and basal infoldings
Middle zone of RPE
contains nucleus and few other organelles
Inner zone of RPE
contains melanin granules (pigment, extends into microvilli)
-gives dark color