EXAM 1 RC 111
1/254
Earn XP
Description and Tags
EXAM 1 RC 111
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
255 Terms
INTRAUTERINE FETAL LUNGS
FETAL LUNG FLUID IS CONSTANTLY RENWED AND REPLACED
THIS CONSTANT MOVEMENT OF FLUID (NEW VS OLD) HELPS TO KEEP THE LUNGS INFLATED
Positive intrapulmonary pressure the continuous secretion. If fluid creates a mild + pressure inside the lungs and keep them inflated
Fetal lungs have a high vascular resistance
WHAT IS THE BACK PRESSURE TO STENT AIRWAYS OPEN IN INFANTS IS CALLED
LARYNGEAL BRAKING
is a mechanism that maintains airway patency during breathing by creating a pressure differential.
LUNG COMPLIANCE
The ability of the lungs to stretch and expand during breathing, reflecting the elasticity and distensibility of lung tissue.
WHAT ARE PERIMETERS FOR HYPOTENSION
WHEN BP FALLS BELOWS 90/60
NORMAL TIDAL VOLUME
500 ML
7-9 ML/KG
WHAT IS NORMAL VALUES LUNG COMPLIANCE
150-200 ML PER H20
HOW DOES LUNG COMPLIANCE AFFECT TIDAL VOLUME
IT DETREMINES HOW MUCH THE LUNGS CAN EXPAND FOR A GIVEN Change IN PRESSURE
HOW DOES AIRWAY RESISTANCE IMPACT TIDAL VOLUME
INCREASES AIRWAY RESISTANCE DIRECTLY reduces tidal volume due to increased effort required for breathing.
DULL SOUND
CONSOLIDATION, FLUID
HYPER RESONANCE
EXCESS AIR
HOW ARE INFANT NERVES INVOLVED IN LARYGNEAL BRAKING
BY REGULATING the airway and preventing collapse during breathing.
MAJPR MUSCLES OF RESPIRATION
DIAGRAPHM AND INTERCOSTALS
ACCESSORY MUSCLES
WHAT ARE THE ACCESSORY MUSCLES OF INSIRATION
SCALENES
,STERNOCLEIDOMASTOID,
PECTORALIS MAJOR.
TRAPEZIUS
WHAT ARE THE ACCESSORY MUSCLES OF EXPIRATION
RECTUS ABDOMINS
EXTERNAL OBLIQUE
INTERNAL OBLIQUE
TRANSVERSUS ABDOMINUS
WHEN DO ACCESSORY MUSCLES COME INTO USE
DURING INCREASED LUNG VOL MAY USE ACCESSORY MUSCLES TO COMPENSATE BY ENLARGING THE THORAX
LESS EFFICIENT BREATHING WHEN LUNG VOLUME REQUIRES EXTRA EFFORT
WHAT IS THE PARIETAL PLEURA
THE INNER LAYER OF THE THORACIC WALL IN CONTACT WITH THE LUNGS IS LINED WITH SEROUS MEMBRANE
WHAT IS THE VISCERAL PLEURA
COVERS THE OUTER SURFACE OF THE LUNGS and is also lined with serous membrane.
WHAT IS THE PLEURAL SPACE
The space between the parietal and visceral pleura, filled with pleural fluid that reduces friction during breathing.
HOW MANY LOBES OF
RIGHT LUNG
LEFT LUNG
RIGHT LUNG HAS 3 LOBES
RIGHT UPPER, MIDDLE AND LOWER
LEFT HAS 2 LOBES
LEFT UPPER AND LOWER
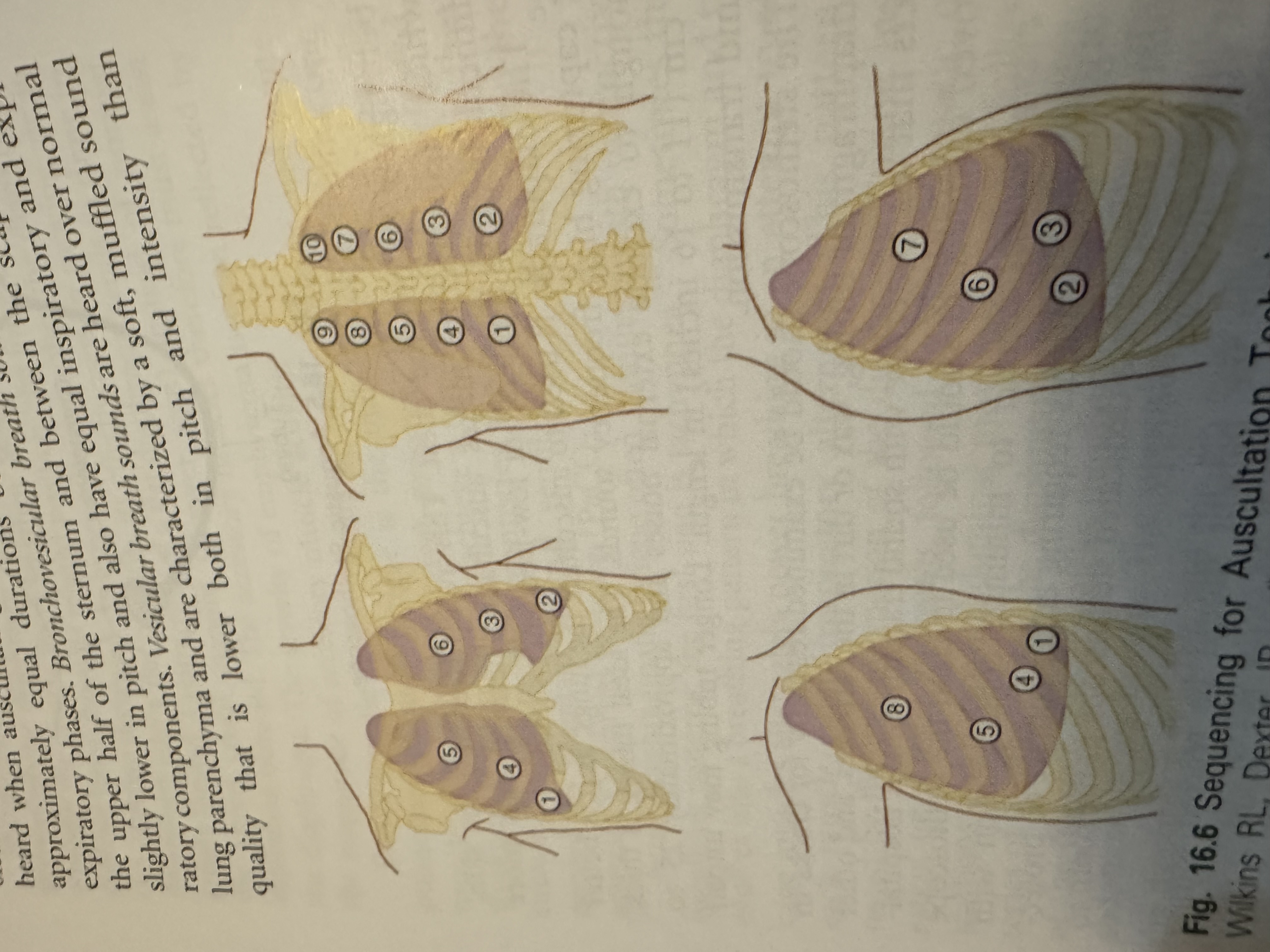
WHAT ARE THE AREAS OF AUSCULATION
WHAT IS DIFFERENCE BETWEEN SPUTUM AND PHLEGM
SPUTUM EXITS THE ORAL CAVITY AND COUGHED UP
PHELGM IS UNCONTAMINATED BY ORAL SECRETIONS
HOW TO CALCULATE PACK YEARS
FOR EX.
IF PT HAS SMOKED FOR 20 YEARS
20 CIGARETTES PER PACK
HAS SMOKED 30 CIG
TAKE THE AMOUNT OF CIG SMOKED/THE NUMBER OF CIG IN A PACK X YEARS
30/20 X 20 =30 PACK YEARS
WHAT IS THE FUNCTION OF THE LARYNX
FACILTATING SOUND
PROTECTING THE AIRWAY
VALVE TO CONTROL AIRFLOW DURING BREATHING AND SWALLOWING
WHAT IMPAIRS OR INHIBITS CILIARY ACTIVITY
SMOKING
INFECTIONS
ENVIROMENTAL POLUUTANTS
THESE CAN LEAD TO A DECREASES MUCOCILIARY ESCALTOR ACTIVITY
WHAT ARE CONDUCTING AIRWAYS
The parts of the respiratory system that transport air to the lungs,
NO GAS EXCHANGE
WHAT IS ORTHOPNEA
A condition where a person has difficulty breathing while lying flat, often relieved by sitting up.
SEEN IN CHF
WHAT IS PLATYPNEA
A condition characterized by difficulty breathing when sitting or standing, often relieved by lying down.
It is less common than orthopnea and may be associated with certain medical conditions.
WHAT IS APNEA
CESSATION OF BREATHING
CAUSES OF PEDAL EDEMA
SWELLING IN LOWER EXTREMITIES
CAUSED BY THE HEARTS INABILITTY TO PUMP BLOOD EFFECTIVELY
THE INCREASE IN VENOUS HYDOSTATIC PRESSURE PUSHES FLUID INTO THE INTERSTIAL SPACE
CHF
, kidney disease, liver disease, or venous insufficiency.
NORMAL VALUES OF
BP
RR
SPO2
TEMP
HR
120/80
12-20
95-100
37 C (98.6 F)
60-100
COMMON CAUSES FOR HYPOTENSION
DEFINED AS:
A SYSTOLIC PRESSURE LESS THAN 90 MMHG
A MEAN ARTERIAL PRESSURE OF LESS THAN 65 MMHG
A DECREASE IN SYSTOLIC OF 40 MMG HG FROM BASELINE
RETRATCTIONS
INWARD SINKING OF THE CHEST WALL DURING INSPIRATION
INSP MUSCLES CONTRACTIONS GENERATE LARGE NEGATIVE INTRATHORACIC PRESSURE
KUSSMAUL BREATHING
DEEP AND FAST RESPIRATIONS
is a deep, labored breathing pattern often associated with metabolic acidosis, particularly diabetic ketoacidosis.
BIOT BREATHING
CHAOTIC BREATHING PATTERN
DAMAGE TO MEDULLA CHARACTERIZED BY FREQUENT IRREGULARITY IN BOTH RATE AND TIDAL VOLUME
APNEUSTIC BREATHING
DEEP GASPING INSPIRATION WITH BRIEF PARTIAL EXPIRATION
WHAT CAN CAUSE DECREASED BREATH SOUNDS
PLUERAL EFFUSION
PNEUMOTHORAX, ATELECTASIS, OR OBSTRUCTION
WHAT IS HOOVER SIGN
A clinical sign indicating paradoxical movement of the abdomen during breathing, often associated with respiratory distress or diaphragm weakness.
WHAT IS TRACHEAL TUGGING
A clinical sign characterized by an inward movement of the trachea during inspiration, often indicating respiratory distress or airway obstruction.
WHAT IS THE DEAD SPACE VOLUME CALCULATION
WHAT IS DEAD SPACE VENTILATION
The portion of each breath that does not participate in gas exchange, which includes the anatomical and physiological dead space.
WHAT IS THE MEDIASTINUM
The central compartment of the thoracic cavity, located between the lungs, containing the heart, great vessels, trachea, esophagus, and other structures.
WHAT IS PERCUSSION
A physical examination technique used to assess the condition of the thoracic or abdominal organs by tapping on the surface and listening for sounds.
WHAT ARE THE CLINICAL IMPLICATIONS OF PERCUSSION
DIFFERENCE BETWEEN SIGNS AND SYMPTOMS
Signs are objective evidence of disease observed by a healthcare professional,
symptoms are subjective experiences reported by the patient.
BREATHLESSNESS
AN UMPLEASANT URGE TO BREATHE
COUGH
MOST COMMON YET NONSPECIFIC SYMPTOM OOBSERVED IN PATIENTS WITH PULM DIS.
THE EFFECTIVENESS OF A COUGH DEPENDS ON WHAT
THE ABILITY TO TAKE A DEEP BREATH
LUNG ELSATIC RECOIL
EXPIRATORY MUSCLE STRENGTH
LEVEL OF AIRWAY RESISTANCE
WHAT IS A CHRONIC COUGH
A cough lasting more than eight weeks, often indicative of underlying conditions such as asthma, bronchitis, or gastroesophageal reflux disease.
HEMOPYTSIS
COUGHING UP BLOOD OR BLOOD STAINED SPUTUM
HEMATOEMESIS
BLOOD VOMITED FROM GI TRACT
WHAT IS THE TRI-POD SIGN
A position assumed by patients with respiratory distress, where they lean forward with their arms braced on their knees or a surface to aid breathing.
PULSUS ALTERNAS
A condition characterized by alternating strong and weak pulses, often indicative of heart failure or other cardiac issues.
PULSUS PARADOXUS
IS A SIGNIFANCT DECREASE IN PULSE STRENGTH DURING SPONTANEOUS INSPIRATION
SYSTOLIC PRESSURE
The pressure in the arteries during the contraction of the heart muscles, specifically when the ventricles pump blood. It is the higher number recorded in a blood pressure reading.
DIASTOLIC PRESSURE
The pressure in the arteries when the heart is at rest between beats, specifically when the ventricles fill with blood. It is the lower number recorded in a blood pressure reading.
CENTRAL NEUROGENIC HYPERVENTILATION
CHARACTERIZED BY BY PERSISTENT HYPERVENTILATION DRIVEN BY ABNORMAL NEURAL STIMULI that affects the respiratory centers in the brain, often leading to respiratory alkalosis.
WHAT IS SUBCUTANEOUS EMPYSEMA
FINE AIR BUBBLES COLLECTING IN SUBCUTANEAOUS TISSUE PRODUCES A CRACKLING SOUND AND SENSATION WHEN PALPATED
It occurs when air leaks into the subcutaneous tissue, often due to trauma, surgical procedures, or infection.
BRONCHOPHONY
A clinical test used to assess lung function where the patient is asked to speak while the clinician listens to the lungs. Increased resonance of the voice indicates underlying lung pathology.
HOW ARE GASES CLASSIFIED
THERAPEUTIC
LABARATORY
ANESTHETIC
SIGNS AND SYMPTOMS OF HYPOXEMIA
include shortness of breath, confusion, cyanosis, and increased heart rate. These manifestations indicate insufficient oxygen levels in the blood.
CHEST XRAY PRESENT AFTER PROLONGED EXPOSURE TO HIGH FIO2
may show bilateral pulmonary infiltrates or signs of oxygen toxicity, indicating lung damage due to excessive oxygen exposure.
WHAT IS HYPOXIC DRIVE
A mechanism that stimulates breathing in response to low oxygen levels, rather than high carbon dioxide levels. This is particularly important in patients with chronic respiratory diseases.
HOW IS THE HYPOXIC DRIVE IN PT WITH HYPERCAPNIA
The hypoxic drive in patients with hypercapnia is often diminished, as their primary respiratory drive is based on elevated carbon dioxide levels. In such cases, low oxygen levels become the key stimulus for breathing.
WHAT IS THE DIFFERENCE BETWEEN LOW FLOW AND HIGH FLOW O2 DELIVERY SYSTEMS
Low flow systems provide oxygen mixed with room air, while high flow systems deliver a fixed concentration of oxygen regardless of the patient's breathing pattern. This distinction is crucial in determining the appropriate oxygen therapy for patients with varying respiratory needs.
NASAL CANNULA
1 TO 6 LPM
24% -44% FIO2
NON-REBREATHER
10-15 LPM
FIO2 -60%-80%
INVREASE LITER FLOW IF BAG DEFLATES MORE THAN 50%
BAG HAS A VALVE
that prevents exhaled air from entering the bag, ensuring a higher concentration of oxygen is delivered to the patient.
AIR ENTRAINMENT SYSTEM
2 TO 15 LPM
ALSO CALLED VENTURI
24% TO 50% FIO2
CAN’T GUARANTEE ABOVE 40% PER PT DEMAND
NO HUMIDITY NEEDED
USED FOR COPD PTS/CO2 RETAINERB
HBO SYSTEM
A system that delivers hyperbaric oxygen therapy, providing high concentrations of oxygen at elevated atmospheric pressure to treat various medical conditions.
WHEN DO WE SUGGEST A HBO FOR A PT BASED ON CARBOXYHEMOGLOBIN
It is used to reduce the effects of carbon monoxide poisoning by displacing carbon monoxide from hemoglobin, thereby restoring the blood's oxygen-carrying capacity.
WHY ARE POST OP PTS MORE PRONE TO DEVELOP ATELECTASIS
as reduced lung volumes, shallow breathing, and pain that limits effective coughing, which can lead to the collapse of alveoli.
WHAT LUNG EXPANSION METHODS INCREASE TRANSPULMONARY PRESSURE GRADIENT
incentive spirometry, deep breathing exercises, and positive pressure ventilation increase the transpulmonary pressure gradient,
promoting lung expansion and preventing atelectasis.
IS
IPPB
CPAP
BIPAP
EZPAP
PEAK FLOWand other lung expansion techniques.
WHAT IS INCENTIVE SPIROMETRY
DECREASE PLEURAL PRESSURE
PTS DO 1O BREATHS PER HOUR
CK FOR BREATH SOUNDS
CAN ONLY BE DONE IN PTS WHO ARE ABLE TO FOLLOW THROUGH DIRECTIONS AND ARE SPONTANEOUSLY BREATHING
SLOW AND STEADY INHALE AND HOLD BREATH 5-10 SEC
USE PILLOW TO SPLINT
MEASUREMENT BASED ON AGE, HEIGHT, AND GENDER
CONTRAINDICTIONS OFR IPPB
include untreated pneumothorax, recent facial or skull surgery, and certain respiratory conditions that prevent effective ventilation.
WHAT ARE GOALS OF IPPB
To improve lung expansion, increase tidal volume, and enhance ventilation in patients who cannot take deep breaths effectively.
WHICH CLINICAL SIGNS INDICATE A PROBLEM WITH RETAINED SECRETIONS
Clinical signs include wheezing, decreased breath sounds, increased respiratory rate, and productive cough. These signs suggest airway obstruction or inadequate clearance of secretions.
WHAT IS MIE
MIE, or Mechanical Insufflation-Exsufflation, is a technique used to assist patients in clearing secretions from their airways through a combination of positive and negative pressure.
HOW DOES PEP WORK
Positive Expiratory Pressure (PEP) works by creating resistance during expiration, which helps keep airways open, promotes lung expansion, and aids in the clearance of secretions.
WHAT IS TOTAL FLOW CALCULATION
TOTAL FLOW =AIR TO O2 RATIO X O2 FLOW RATE
GIVEN FIO2 = 40%
O2 FLOW RATE - 10 L/MIN
AIR TO O2 RATIO = 3:1 = 4
TOTAL FLOW = 4 X10 = 40 L/MIN
SIMPLE MASK
5 TO 10 LPM
35% -50% FIO2
CAN’T USE ON LESS THAN 5 LBECAUSE CO2 WONT BE WASHED OUT
MASK WILL SERVE AS DEAD SPACE FOR EXHALED C02 IS RUN BELOW 5 LPM
PT CANT EAT OR DRINK
USED ON MOUTH BREATHERS
CAN’T USE HUMIDITY
BVM
A Bag-Valve-Mask (BVM) is a medical apparatus used to provide positive pressure ventilation to individuals who are not breathing or not breathing adequately. It consists of a self-expanding bag, a unidirectional valve, and a facial mask.
C/E HOLD
DON’T PRESS MORE THAN 50% OF THE BAG 500 ML
HAS A BAG OR OR TUBE AS RESEVOIR
USED FOR PT WHO ARE NOT BREATHING OR INSUFFICIENT BREATHING
USE OPA OR NPA IF PT IS UNCONSCIOUS
PRESS BAG EVERY 6 SEC
HIGH FLOW NASAL CANNULA
FLOW RATE UP TO 50 LPM
FIO2 - 35% TO 90%
BRAND AIRVO
START WITH 40LPM AND TITRATE
TEMP 35-37 C
AVOIDING INTUBATION
USE STERILE WATER FOR INHALATION
METAL PLATE ATTACHED TO BLENDER FOR HEATING
BLENDER : TEMP AND FIO2
LVN
5-10 LPM
FI02 - 28%-98%
HAS A VENTURI DIAL TO ADJUST FLOW
BUBBLE HUMIDIFIER ATTACHED TO FLOW METER
USE 2 LARGE BORE TUBING
MDI
EXAMPLE ALBUTEROL
PRESET DOSE
SHAKE BEFORE USE
PRIME IF NEW
SLOW, STEADY INHALE
1 MIN GAP IN BETWEEN ACTUATION/PUFF
BAN
BREATH ACTUATED NEB
RUN AT 5 LPM
DELIVERS 0.5 -6 ML MEDICATIONS
AIR DRY ONCE DONE USING
HAS A DIAL THAT CONTROLS WHETHER THE PT IS SPONTANEOUSLY BREATHING
USE CONTINOUS SETTING = MASK
GREEN DIAPHRAGM INSIDE CONTROLS AEROSOL
MORE EXPENSIVE
WHAT IS Pa02
PARTIAL PRESSURE of oxygen in arterial blood, indicating oxygenation status.
CLINICAL OBJECTIVES FOR O2 THERAPY
MAINTAINS ADEQUATE TISSUE OXYGENATION
DECREASES THE WORKLOAD HYPOXEMIA IMPOSES ON THE CARDIOPULM SYSTEM
HOW DOES 02 THERAPY CORRECT HYPOXEMIA
INCREASING ALVEOLAR AND BLOOD LEVELS OF O2
RELIEVES DYSPNEA AND IMPORVES MENTAL FUNCTION
CARDIOPULMONARY SYSTEM COMPENSATES FOR DECREASED 02 BY
INCREASING VENT TO INCREASE CARDIAC OUTPUT
TO INCREASE 02 PERFUSION TO MEET METABOLIC 02 DEMANDS
HYPOXEMIA CAUSES
VASOCONSTRICTION
AND IF IT IS CHRONIC HYPOXEMIA IT CAN CAUSE PULM HYPERTENSION
INDICATIONS FOR 02 THERAPY
PAO2 LESS THAN 60 MM HG OR SPO2 LESS THAN 90% IN PT BREATHING ROOM AIR
ACUTE CARE SETTINGS IN WHICH HYPOXEMIA IS SUSPECTED
SEVERE TRTAUMA
ACUTE MI
SHORT TERM THERAPY OR SURGICAL INTERVENTIONS
WHAT IS THE RULE OF O2 TEHRAPY
TO GIVE JUST ENOUGH TO MEET THE SPECIFCATIONS , NOT EXCESSIVE
TITRATE DOWN AS SOON AS POSSIBLE
USE LEAST AMOUNT OF 02 TO GET TEHJOB DONE
FOR FIO2 GREATER THAN 50%
BE WORRIED ABOUT:
ABSORPTION ATELECTASIS
02 TOXICITY
OR DEPRESSION OF CILIARY OR LEUKOCYTE FUNCTION MAY OCCUR
EXUDATE
FLUID THAT OOZES FROM CELLS AND TISSUES USUALLY FROM IMFLAMMATION OR INJURY
A PAO2 GREATER THAN 80MMHG IN INFANTS MAY LEAD TO
RETINOPATHY OF PREMATURITY
O2 IS NOT FLAMMABLE BUT
PROMOTES A FIRE
WHAT IS O2 TOXICITY
IS DUE TO PAO2 AND EXPOSURE TIME
THE GREATER THE EXPOSURE TIME AND THE HIGHER THE PO2 (FIO2) THE GREATEST THE LIKLIHOOD OF DAMAGE
DURING O2 TOXICITY WHAT HAPPENS
OXYGEN FREE RADICALS DAMAGES CAPILLARY ENDOTHELIUM
TYPE 1 CELLS - DESTORYED
TYPE 2 CELLS - THICKEN
WHAT IS THE V/Q MISMATCH
A condition where the ventilation and perfusion of the lungs are not properly matched, leading to impaired gas exchange.
3 BASIC 02 DELIVERY SYSTEMS
LOW FLOW
HI FLOW
RESERVOIR
WHAT IS FIO2 FOR A NASAL CATHETER
22-45
USED SHORT TERM FOR SPECIFIC PROCEDURES