PSYC 367: Quiz 2
1/132
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
133 Terms
what is somatosenstion?
the process of neural substrates being activated by physical stimuli resulting in perception of
touch
Kinesthesis
temperature
pain
what is touch?
sensations caused by mechanical displacements of the skin
what is kinesthesis?
perception of position and movement of limbs in space
Part of proprioception (also includes internal sensation)
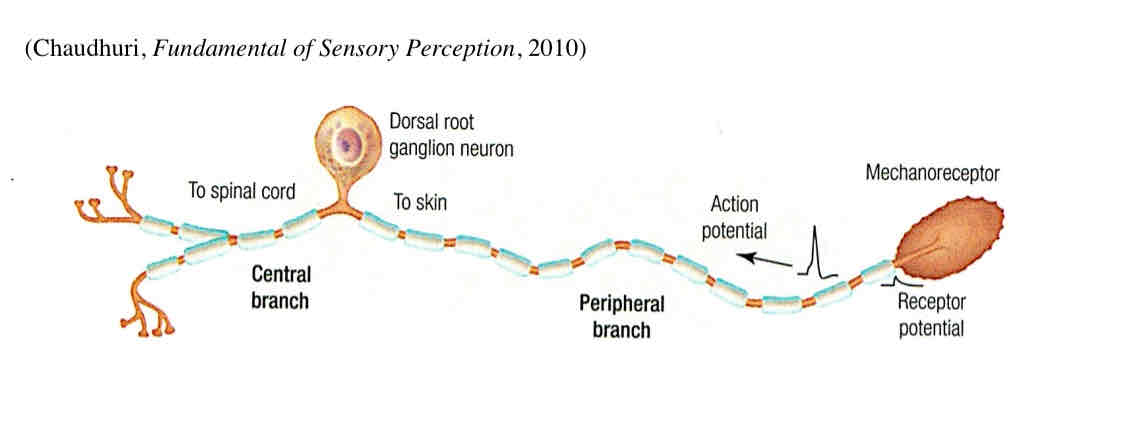
what are somatosensory receptors?
neurons with peripheral and central axons - some touch receptors have specialized endings in the skin
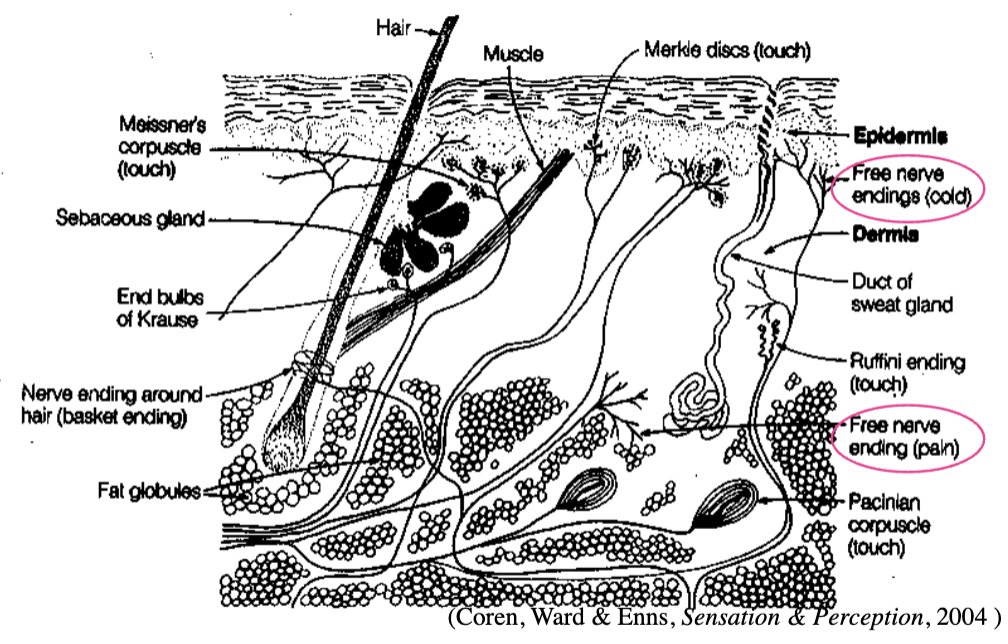
what is glabrous skin?
skin with no hair follicles - palms, soles, lips
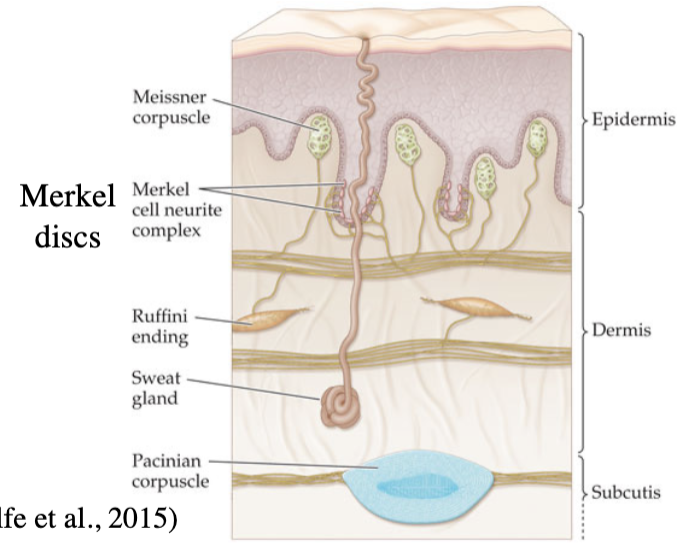
what is a mechanoreceptor?
sensory neuron that responds to mechanical stimulation
4 types in glabrous skin
what are receptive fields in the skin?
body areas that elicit responses from sensory neurons
mechanoreceptor type SA 1 (Merkel)
size of receptive field = small
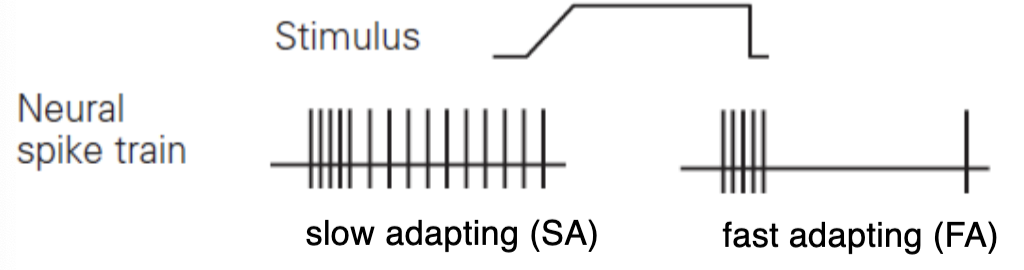
adaptation rate to new stimulus = slow
max feature sensitivity = small slow sustained pressure, very low frequency (< ~5 Hz)
primary perceptual functions = coarse texture and pattern
mechanoreceptor type FA I (Meissner)
size of receptive field = small
adaptation rate to new stimulus = fast
max feature sensitivity = small fast temporal changes in skin deformation (~5 to 50 Hz) - skin slip
primary perceptual functions = low-frequency vibration; grasp stability (fingers, lips - light touch)
mechanoreceptor SA II (Ruffini)
receptive field = large
adaptation rate to new stimulus = slow
max feature sensitivity = large slow sustained downward pressure; lateral skin stretch (~5-50 Hz)
primary perceptual functions = finger position
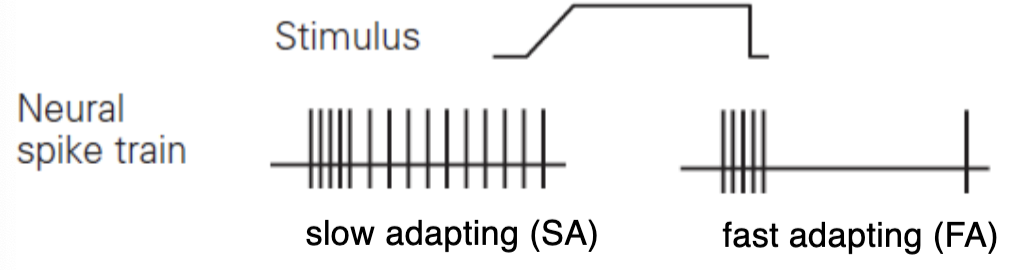
mechanoreceptor FA II (Pacinian)
size of receptive field = large
adaptation rate to new stimulus = fast
max feature sensitivity = large fast temporal changes in skin deformation (50-700 Hz)
primary functions = high-frequency vibration; fine texture
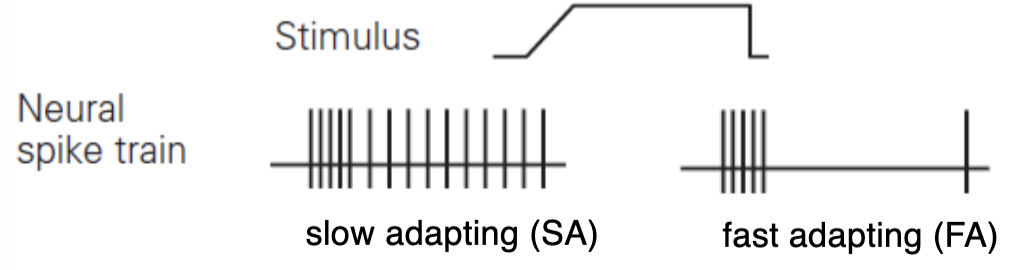
hair follicle receptor
5th type of fast-adapting tactile mechanoreceptor in hairy skin
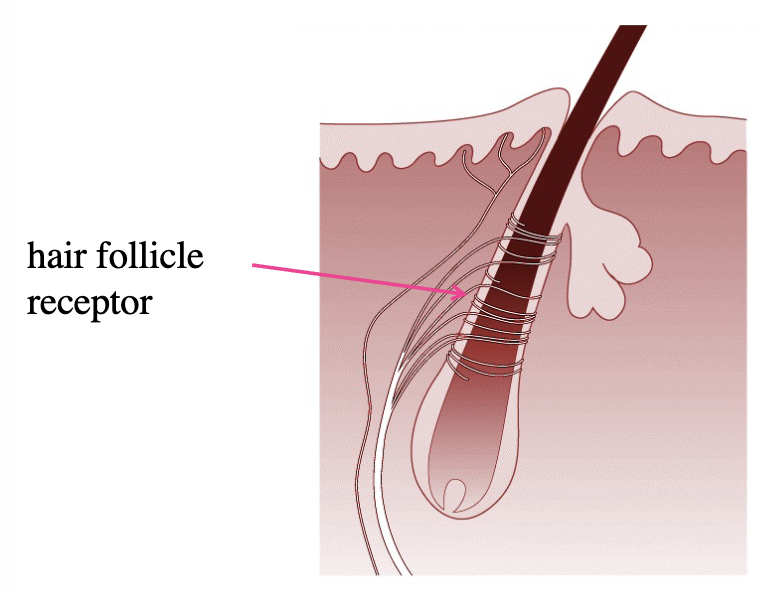
what are kinesthetic mechanoreceptors?
information in skeleton, muscles, tendons of human body (force, torque, position, velocity)
muscle spindle
golgi tendon organ
what are muscle spindles?
mechanoreceptors that signal length and changes in length of muscles (stretched and shortened)
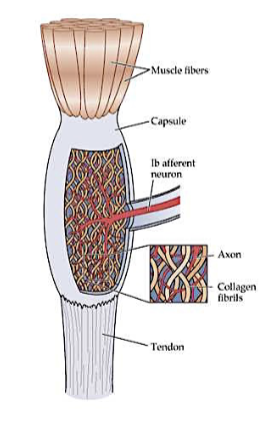
what are golgi tendon organs?
mechanoreceptors that respond to changes in muscle tension and joint position (rather than muscle stretch)
what are nociceptors?
free nerve endings that initiate pain feelings
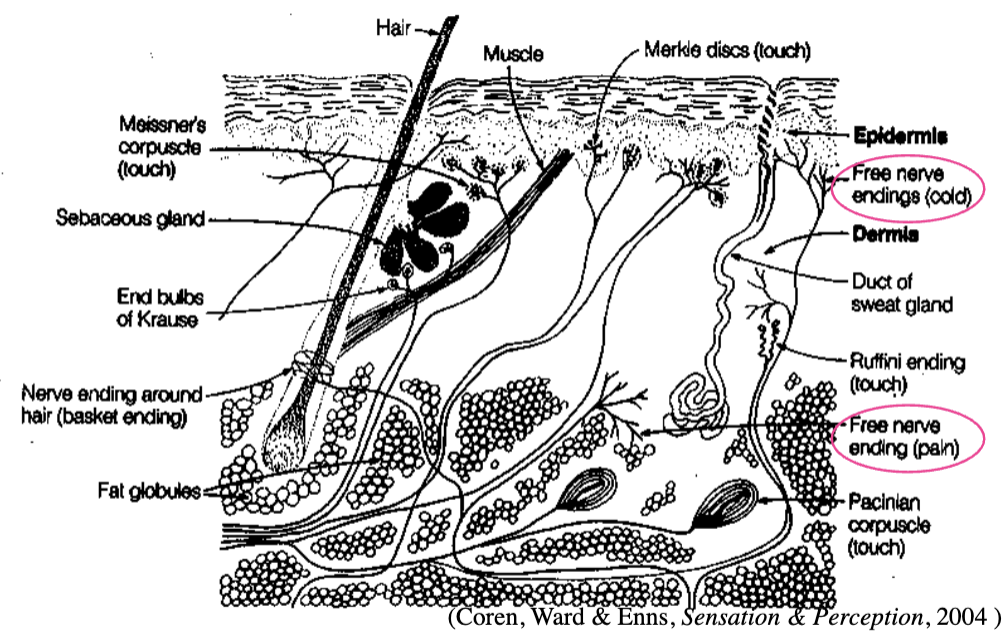
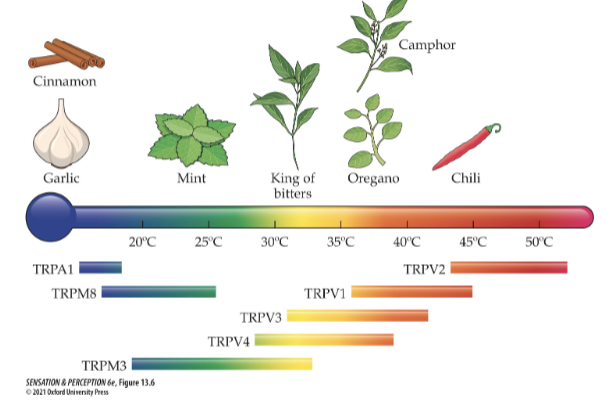
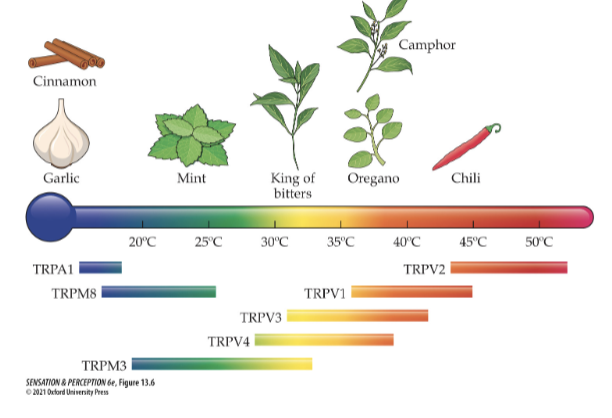
what are thermoreceptors?
free nerve endings that stimulate feelings of temperature (closer to the skin)
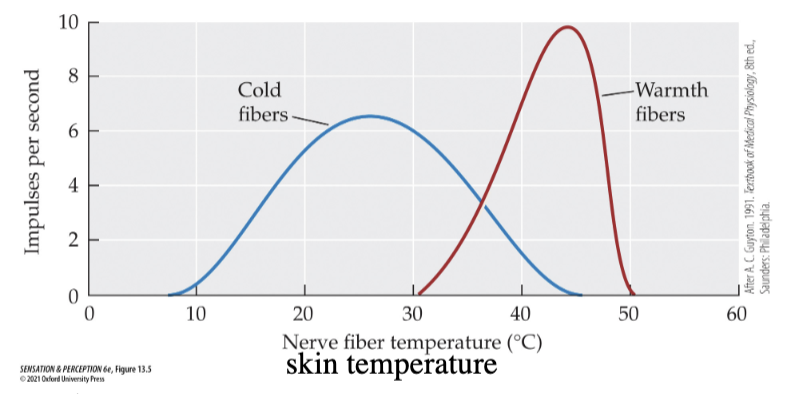
what is our physiological zero?
normal skin temperature (30-36 degrees)
feel no sensations of warmth or cold
what do different thermoreceptor firing rates look like?
warmth fibres: increase firing rate with increases in skin temperature above 36 degrees
cold fibres: increase firing rate with decreases in skin temperature below 30 degrees
what stimulates nociceptors?
extreme temperature (thermal type)
severe pressure or excessive stretching (mechano type)
intense heat, chemicals released by injured tissues, and/or spicy food (polymodal type)
how does the transduction of somatosensory signals work?
not fully known - occurs in peripheral axon, channels are sensitive to mechanical force/temperature/chemicals released by injured tissue open and Na+/Ca+ enter
neuron depolarizes (receptor potential) - action potential travels full length of axon to spinal cord if threshold is reached
what transports somatosensory info to spinal cord?
4 different-sized nerve fibres
proprioceptor
mechanoreceptor
pain and temperature
pain, temperature, itch
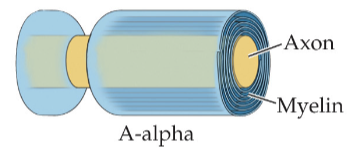
proprioceptor
A-alpha fibre - thick myelin and axon
diameter = 13-20 micrometer
conduction speed = 80-120 m/s
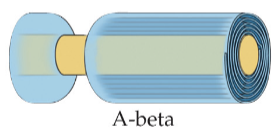
mechanoreceptor
A-beta fiber - mildly thick myelin and axon
diameter = 6-12 micrometers
conduction speed = 35-75 m/s
3 types: fast-adapting, slowly adapting II (only glabrous skin), slowly adapting I
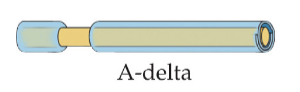
pain and temperature receptor
A-delta - thin myelin and smaller axon
diameter = 1-5 micrometers
conduction speed = 5-30 m/s
One type: A-delta (only in hairy skin - hair receptor)
pain, temperature, itch fiber
C - no myelin and smallest axon
diameter = 0.2-1.5 micrometers
conduction speed (m/s) = 0.5-2
two types: C-nociceptor, C-tactile (only hairy skin)

what is double pain?
initial sharp pain followed by slower, throbbing pain
A-delta fibre = first sharp pain
C fibre = throbbing pain
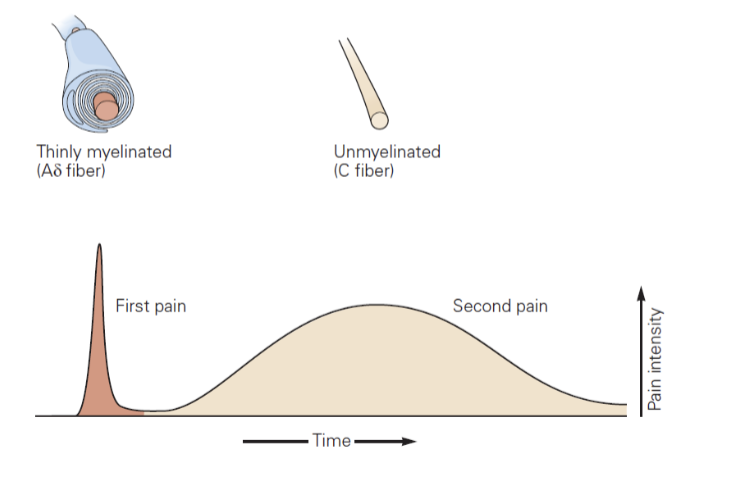
what types of fibres are A-delta fibres?
cold fibres
thermal nociceptors (TRPM8 channels, extreme cold)
mechano nociceptors (severe pressure)
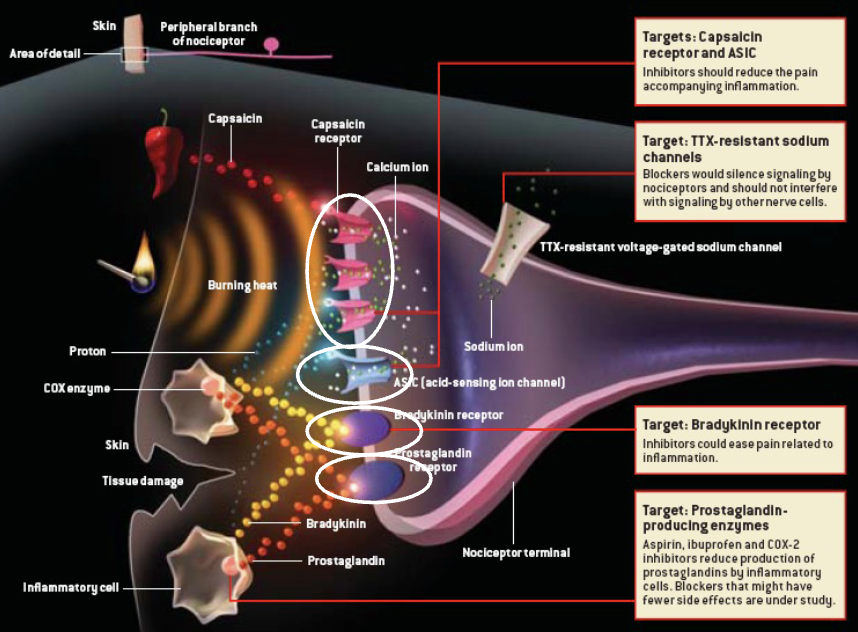
what types of fibres are C fibres?
warmth fibres
polymodal nociceptors: inflammatory cells release prostaglandin, bradykinin or portions which activate their respective channels
intense heat, protons and capsaicin (in hot peppers) = capsaicin receptors (TRPV1)
what are the types of chemical membrane receptors on C fibres (polymodal nociceptor)?
capsaicin receptor and ASIC: reduce pain accompanying inflammation
TTX-resistant sodium channels: silence signalling by nociceptors
bradykinin receptor: ease pain related to inflammation
prostaglandin producing enzymes: aspirin, ibuprofen, COX-2 inhibitors reduce prostaglandin production
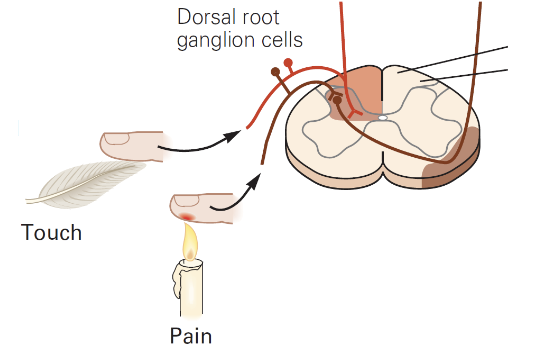
significance of the dorsal root ganglion of spinal cord to pain perception?
cell bodies of A-beta, C, A-delta fibres are located there
significance of dorsal horn of spinal cord to pain perception?
many central axons combine into a single nerve trunk and synapse there - different types of somatosensory nerve fibres project to different layers of it
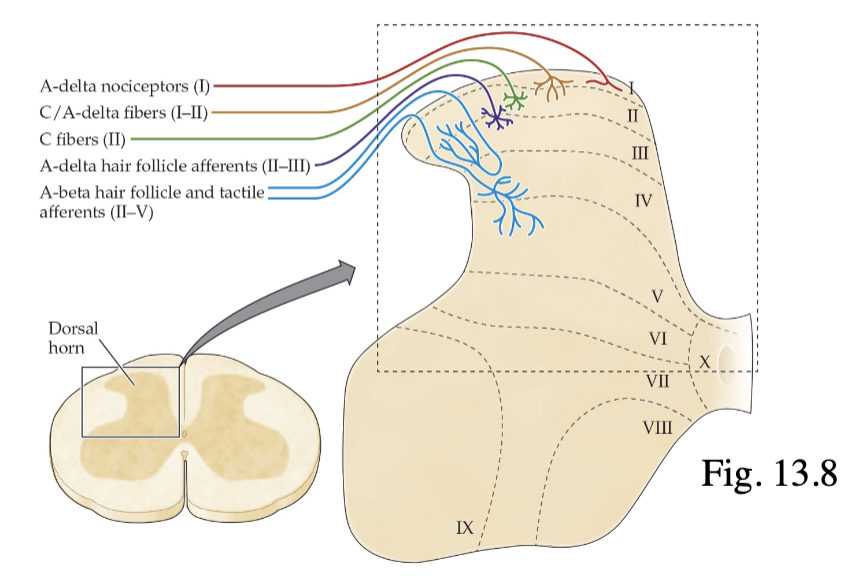
what are the somatosensory layers of the dorsal horn?
I = A-delta nociceptors
I-II = C/A delta fibres
II = C fibres (substantia gelatinosa)
II-III = A-delta hair follicle afferents
II-V = A-beta hair follicle and tactile afferents
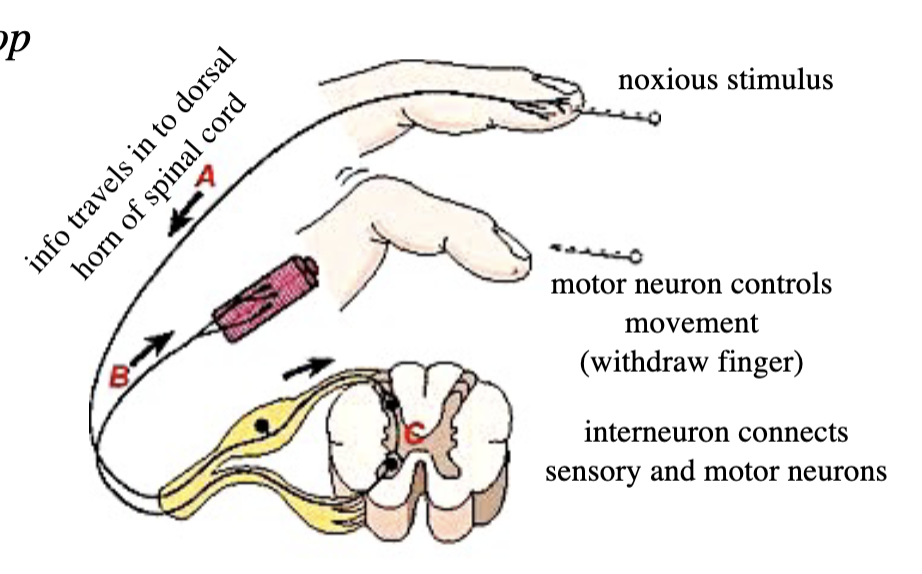
what is the process of our reflex loop?
noxious stimulus
info travels in to dorsal horn of spinal cord
interneuron connects sensory and motor neurons
motor neuron controls movement (ex. withdraw finger)
spinothalamic and dorsal column-medial lemniscal pathways contain neurons that participate
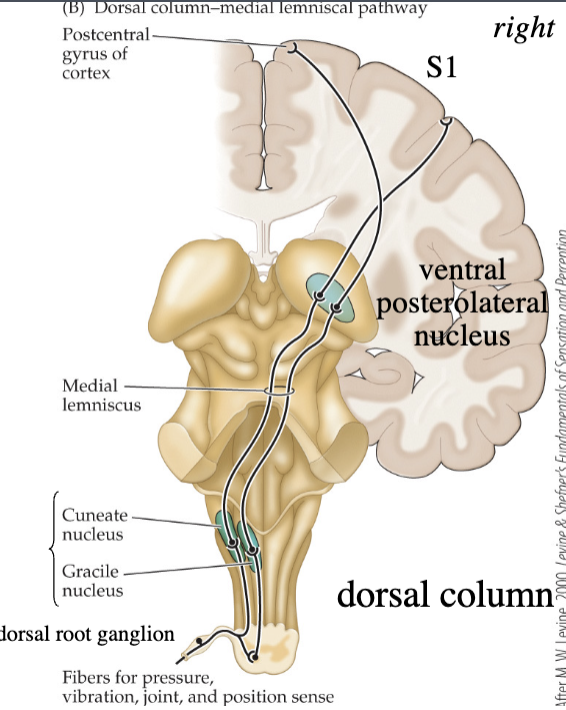
what is the somatosensory pathway for touch?
spinal cord (1st synapse for some neurons)
medulla (1st synapse for most neurons)
thalamus (synapse)
parietal cortex (synapse)
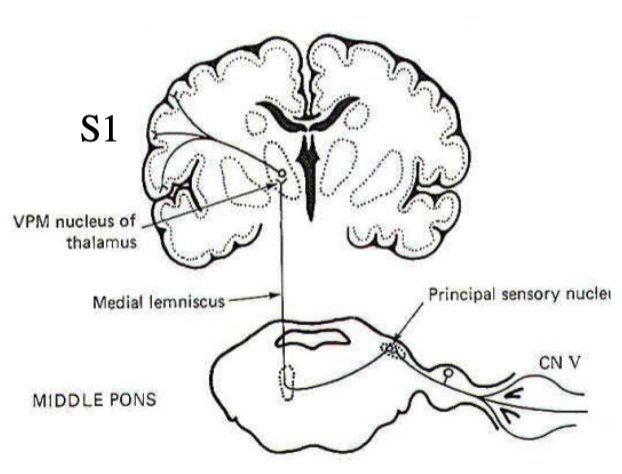
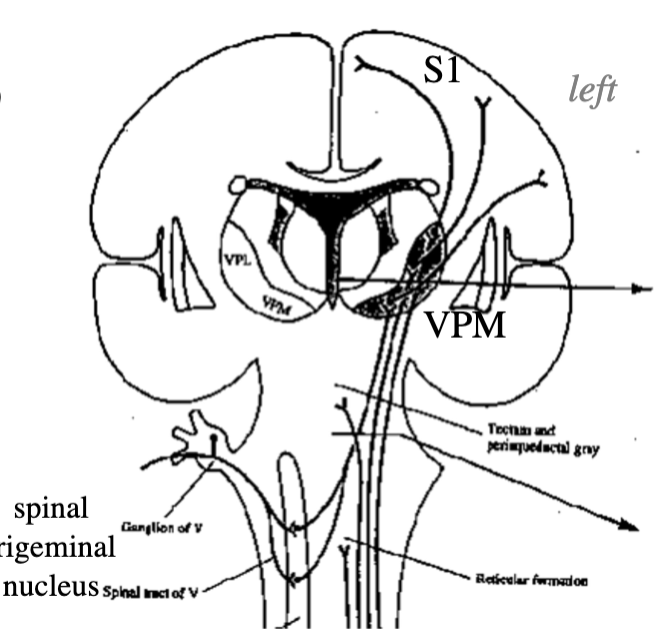
what is the head only somatosensory pathway for touch?
pons (1st synapse): principal sensory nucleus of trigeminal nerve
thalamus (2nd synapse): ventral posteromedial nucleus (VPM)
parietal cortex (3rd synapse)
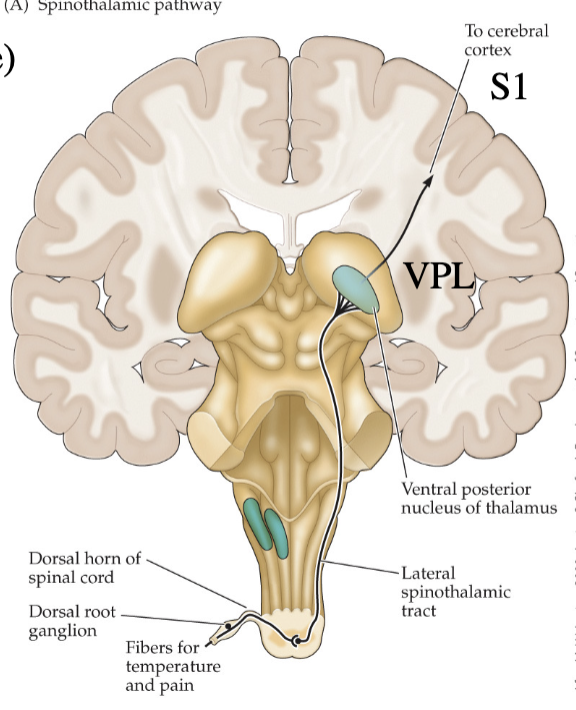
what is the somatosensory pathway for temperature and pain?
spinothalamic pathway
peripheral skin/tissue experiencing painful stimuli
nociceptors travel from injury sight to dorsal root ganglion
substantia gelatinosa (layer II) in dorsal horn (1st synapse)
thalamus (2nd synapse)
parietal cortex (3rd synapse)
what is the head only somatosensory pathway for temperature and pain?
medulla (1st synapse)
thalamus (2nd synapse)
parietal cortex (3rd synapse)
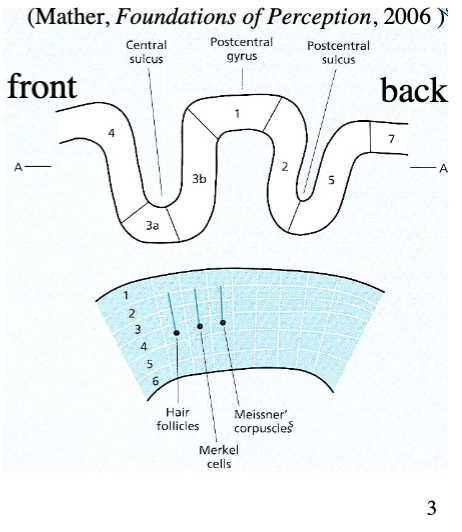
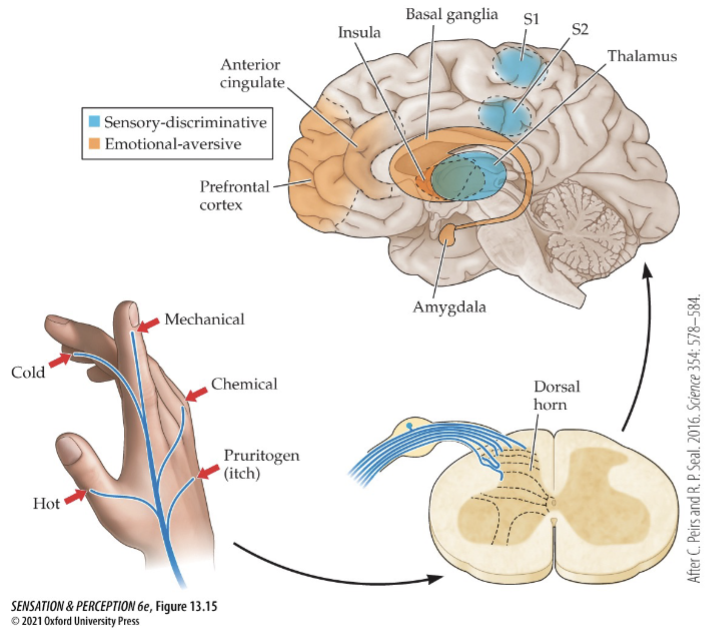
what is the S1 region in the brain?
“light blue” portion of the somatosensory cortex
Includes Brodmann areas 3a, 3b, 1 and 2 (a way of mapping the cortex/functions - numbering is not in directional order)
Brodmann area 3
where neurons from thalamus synapse - layer 4 of area 3a (proprioception) or 3b (touch)
each type of mechanocreceptor connects to different column in 3b (in pic)
projects to area 1 and 2
What is the S2 region of the brain?
“dark blue” portion of the somatosensory cortex
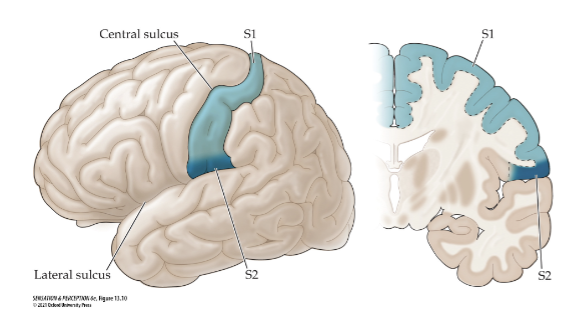
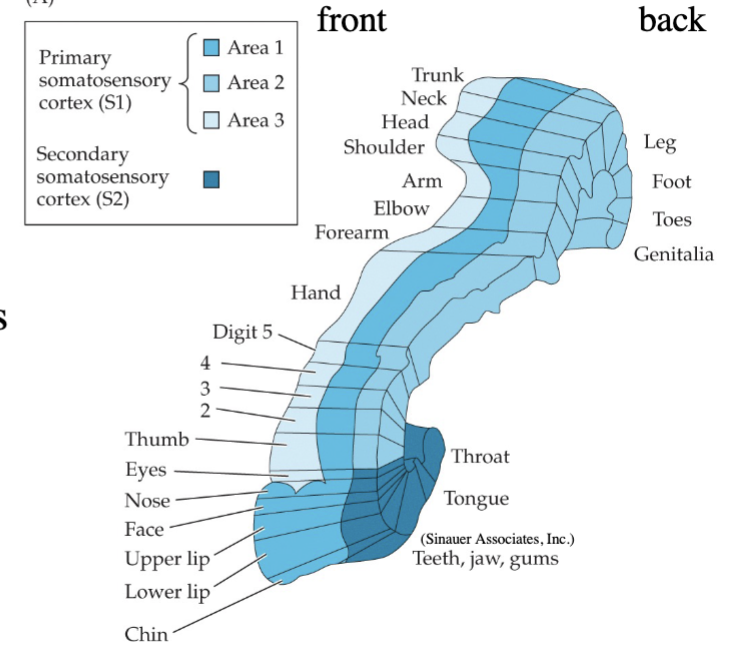
what is the somatotopic map/sensory homunculus
map of each point on skin represented by a corresponding area in contralateral cortex (map is distorted)
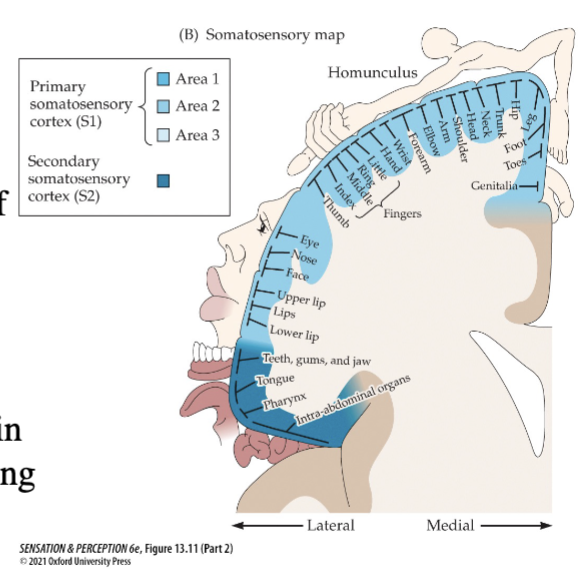
what is cortical magnification?
enlarged representation in cortical somatotopic map/sensory homunculus relative to skin area
multiple maps in S1 and S2
S1, area 1 = middle
S1, area 2 = right
S1, area 3 = left
what is tactile sensitivity?
touch detection ability (inverse of absolute threshold - high sensitivity = low threshold, low sensitivity = high threshold)
highest on face
lowest on foot
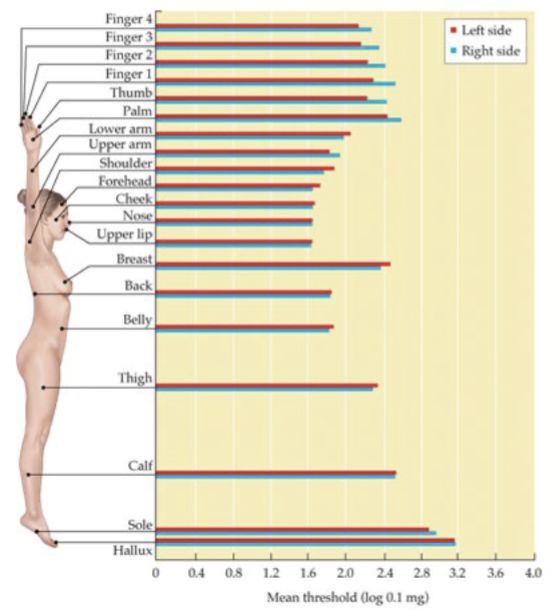
What entails touch discrimination?
JND increases with magnitude of standard stimulus (Weber) - smaller (better discrimination) for areas of skin with higher sensitivity (lower absolute threshold)
Weber fraction for touch: JND/standard
what is touch acuity?
minimum distance at which two stimuli are just perceptible as separate - 2-point threshold
better in skin regions with larger cortical representation in homunculus
can be low when detection threshold is high
how are somatosensory neurons represented in receptive fields?
each one in S1 responds to stimulation in only a specific small area of body
A region (image) = excitatory centre (middle of stimulation spot)
B region = inhibitory surround (around stimulation spot)
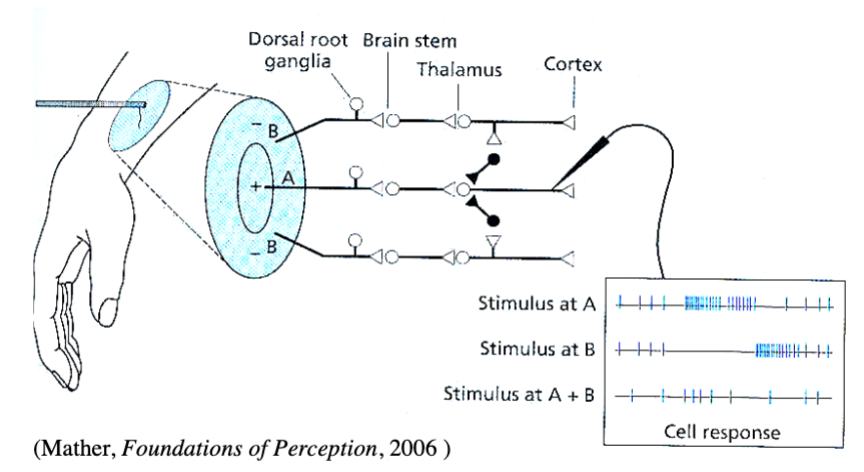
2-point threshold on body parts with small receptive fields?
2 points stimulate separate receptive fields, 2 points perceived (thumb)

2-point threshold on body parts with larger receptive fields
2 points stimulate same receptive field, 1 point perceived

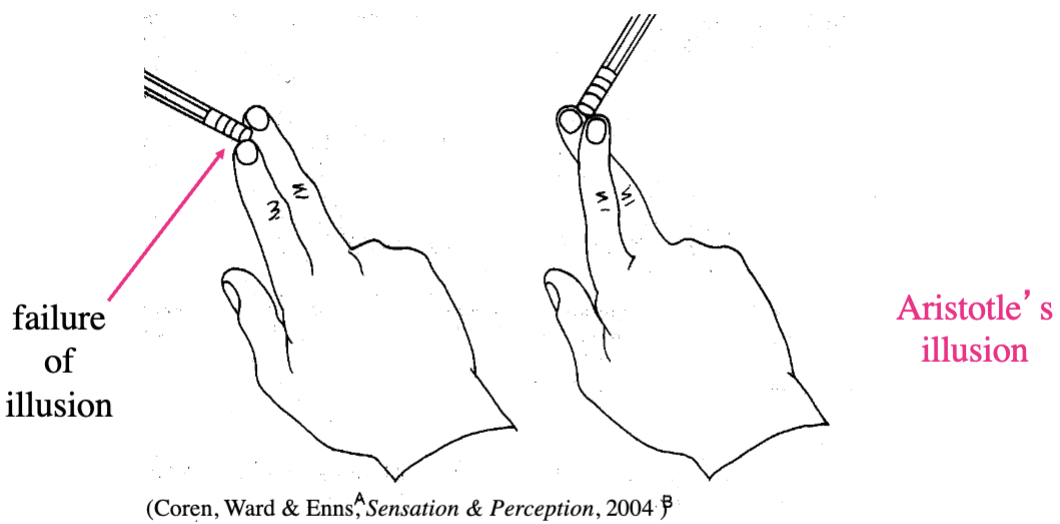
what is Aristotle’s Illusion?
2 receptive fields far apart on cortex are stimulated, but this normally only happens when 2 objects touch you
failure of illusion: receptive fields close on cortex may be stimulated, but this normally only happens when 2 objects touch you
what is nociceptive pain?
results from stimulation of free nerve endings in skin, muscles, and joints - aids survival by avoiding potentially harmful stimuli, immobilize to promote healing
what are the neuro components of pain?
limbic system (anterior cingulate, insula, amygdala): processing of emotion
prefrontal cortex: modulating pain perception, chronic pain emotional response
based on more than just sensory factors
what modulates pain sensitivity?
enkephalins and endorphins (endogenous opiates) - released by descending inputs from brain (ex. periaqueductal gray in midbrain)
block release of substance P
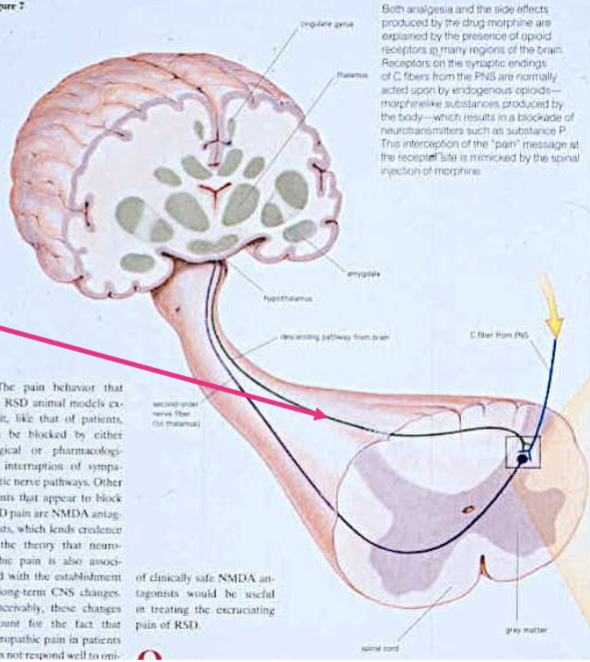
where do pain neurons transmit signals?
synapse in substantia gelatinosa
neuron from brain + C fibre from skin + spinal cord neuron to thalamus
C fibre transmits signals to brain dendrites an releases nt substance P
substance P membrane receptors are on spinal cord neuron (why athlete’s don’t notice minor injuries for hours)
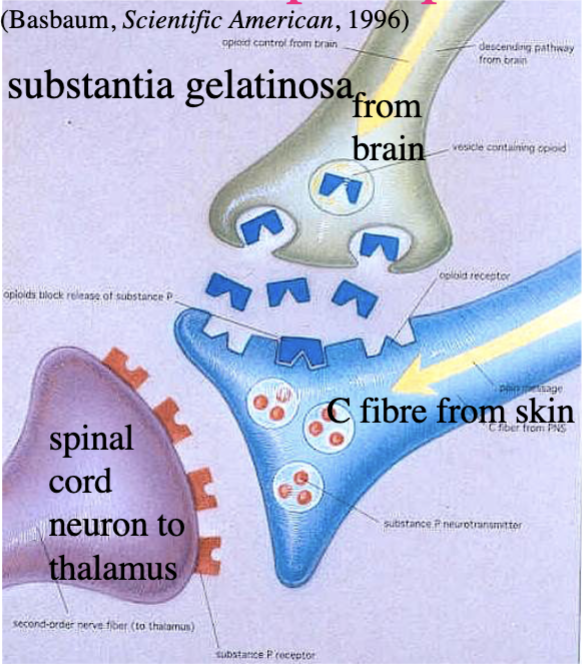
what is gate control theory?
based on interactions between fast A-beta touch fibres and slow C/A-delta pain fibres - substantia gelatinosa in dorsal horn gates flow of pain to brain, descending inputs from brain can’t close pain gate
transmission cells carry pain signal to brain when gate is open
fast mechanoreceptors = close gate
slow nociceptors = open gate
how can you treat nociceptive pain?
transcutaneous electrical nerve stimulation (TENS)
anesthetics
analgesics
acupuncture
transcutaneous electrical nerve stimulation (TENS)
based on gate control theory - electric current passed through skin near pain site → activates A-beta fibres to close pain gate → stimulates release of endogenous opiates
anesthetics
produce total loss of sensation by interrupting signals travelling to brain
local: act at site of injection - block Na channels
general: act on full brain (unconsciousness)
analgesics
produces loss of pain sensations
non-opiate: mild/moderate pain - aspirin/ibuprofen (anti-inflammatory) and acetaminophen/COX-2 inhibitors (Tylenol, Celebrex)
opiate: potent pain killers - morphine, codeine, heroin (block nociceptor nt release and inhibit spin neurons)
acupuncture
insertion of long needles into specific places - not understood but may release endogenous opiates
what is inflammatory pain?
when nociceptors become increasingly sensitized due to damage/inflammation of tissues or by tumour cells
Hyperalgesia and allodynia
hyperalgesia
Painful stimuli become more painful due to nociceptors becoming sensitized and overly reactive to noxious stimuli
allodynia
gentle touch stimuli become painful - lower thresholds for pain
what is neuropathic pain?
more serious than inflammatory, chronic - not related to stimulation of nociceptors
burning, shooting pain, numbness, itchiness
Damage/dysfunction to CNS or PNS
characterized by peripheral or central sensitization
peripheral sensitization
change in nociceptors coming into spinal cord
central sensitization
increase of number of pain receptors, rewiring of connections or loss of inhibitory cells in spinal cord
What are treatments for persistent pain?
anticonvulsants
Capsaicin
Marijuana
NMDA-receptor blockers
Anticonvulsants
inhibit specific calcium channel to prevent release of nociceptors neurotransmitters
capsaicin
stimulates nociceptors, but may kill them/use up supply of neurotransmitters causing pain initially but then relieves pain
marijuana
cannabinoids block nt release from nociceptors and reduce inflammation
NMDA-receptor blockers
prevent glutamate from binding with NMDA receptors on spinal cord neurons (involved in central sensitization)
cocaine and heroin - activate nociceptor receptors to block glutamate release
what is phantom limb syndrome?
when sensations are perceived to come from an amputated limb, neuropathic pain
central sensitization rewiring occurs during surgery
local anesthetic should reduce central sensitization, but it still occurs
how does phantom limb syndrome work? (ex. hand amputation)
the hand is normally flanked below by face representation and above by upper arm representation in the cortical homunculus - following amputation face and arm regions take over hand region of cortex → touching of face and upper arm = pain in missing hand
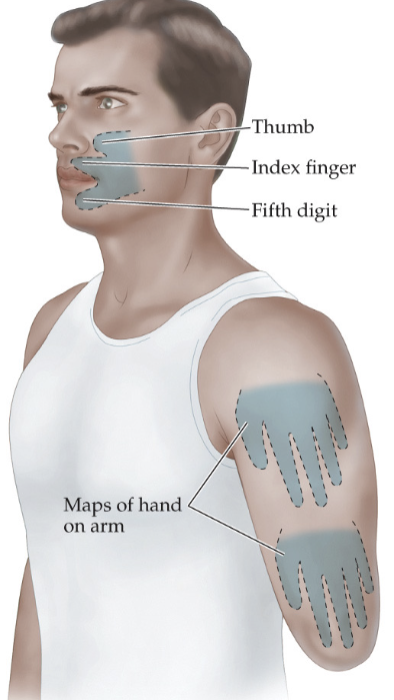
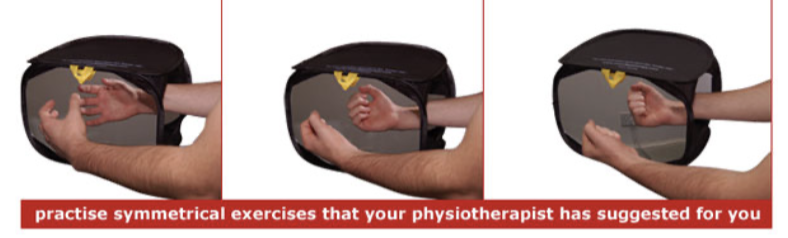
how to treat phantom limb pain?
mirror box - move uninjured limb in front of mirror to act like the missing limb
electrical stimulation in spinal dorsal column to close pain gate in spine
what is light?
a wave/stream of photons/tiny particles (when wave gets absorbed by retina) that each consist of one quantum energy
what we can see = electromagnetic spectrum
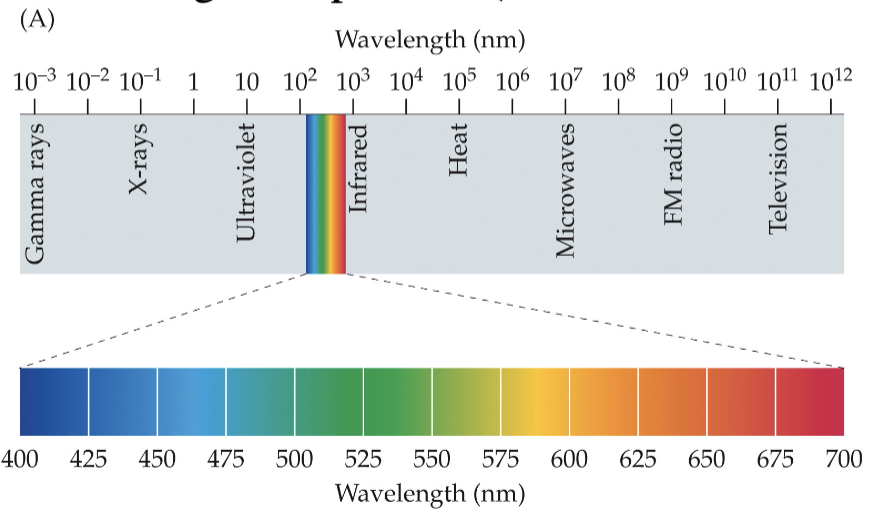
what wavelengths are visible to the human eye?
between 400-700nm (nanometer [nm] = 10^-9m)
wavelength determines colour perceived (ROYGBIV)
![<p>between 400-700nm (nanometer [nm] = 10^-9m)</p><ul><li><p>wavelength determines colour perceived (ROYGBIV)</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/89f3e988-e136-41a6-ae4d-20273dd8c2d9.png)
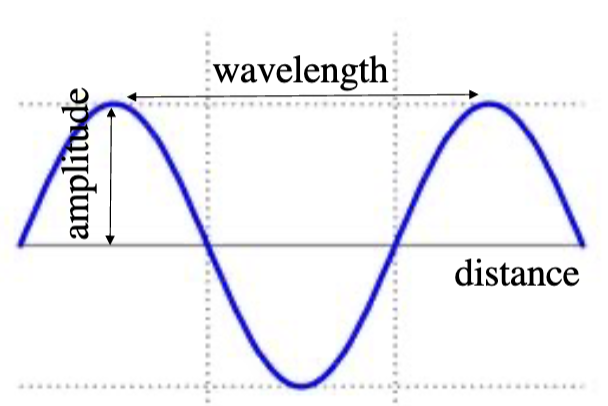
what is vision intensity?
depends on wave property (height of energy wave peaks - amplitude) and particle property (number of quanta emitted by a light source)
independent, but correlated
perceived brightness
what is the emission spectra of light sources?
sunlight = short wavelengths (blue) (florescent lightbulbs more similar to)
light bulbs = long wavelengths (yellow)
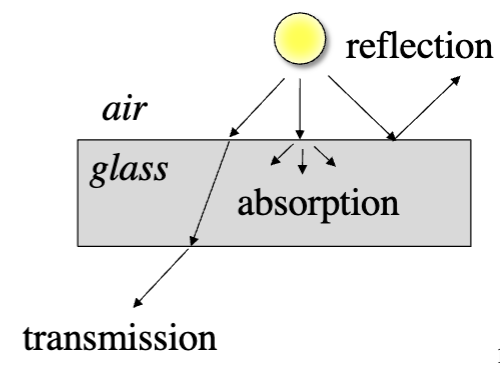
what happens to light once it is emitted?
absorbed: not transmitted at all
diffracted: scattered by dust/water particles in air
what happens once light encounters a surface?
transmitted: conveyed from one place to another, usually with refraction (colour of translucent
absorbed: medium heats up
reflected: redirected back to origin (colour of solid objects depends on wavelengths reflected off object to eye)
what is refraction?
change in direction (bending) of light ray passing from one transmitting medium to another - also depends on wavelength of the source
violet refracts the most
red refracts the least
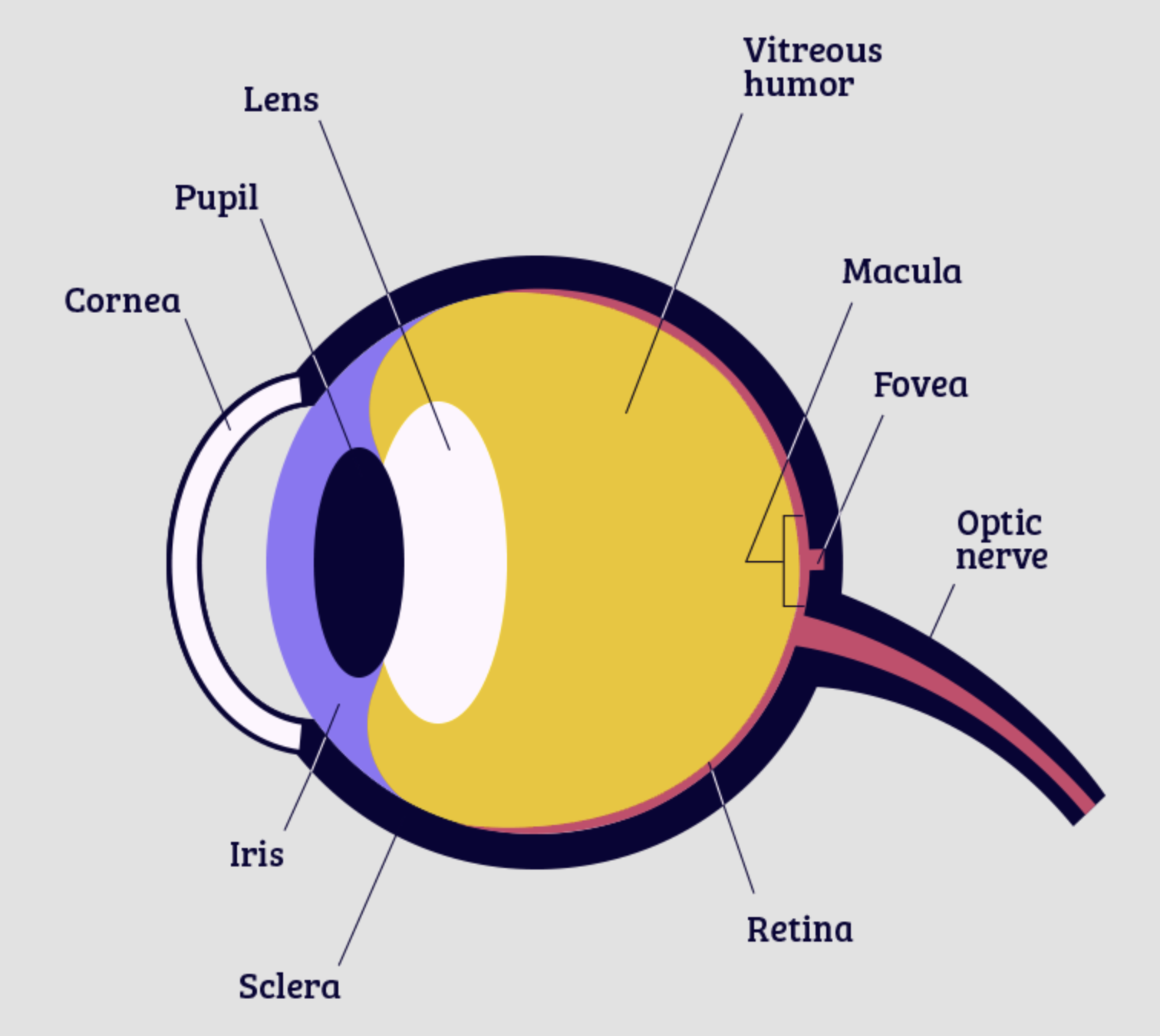
pupil
eye opening, light energy passes through
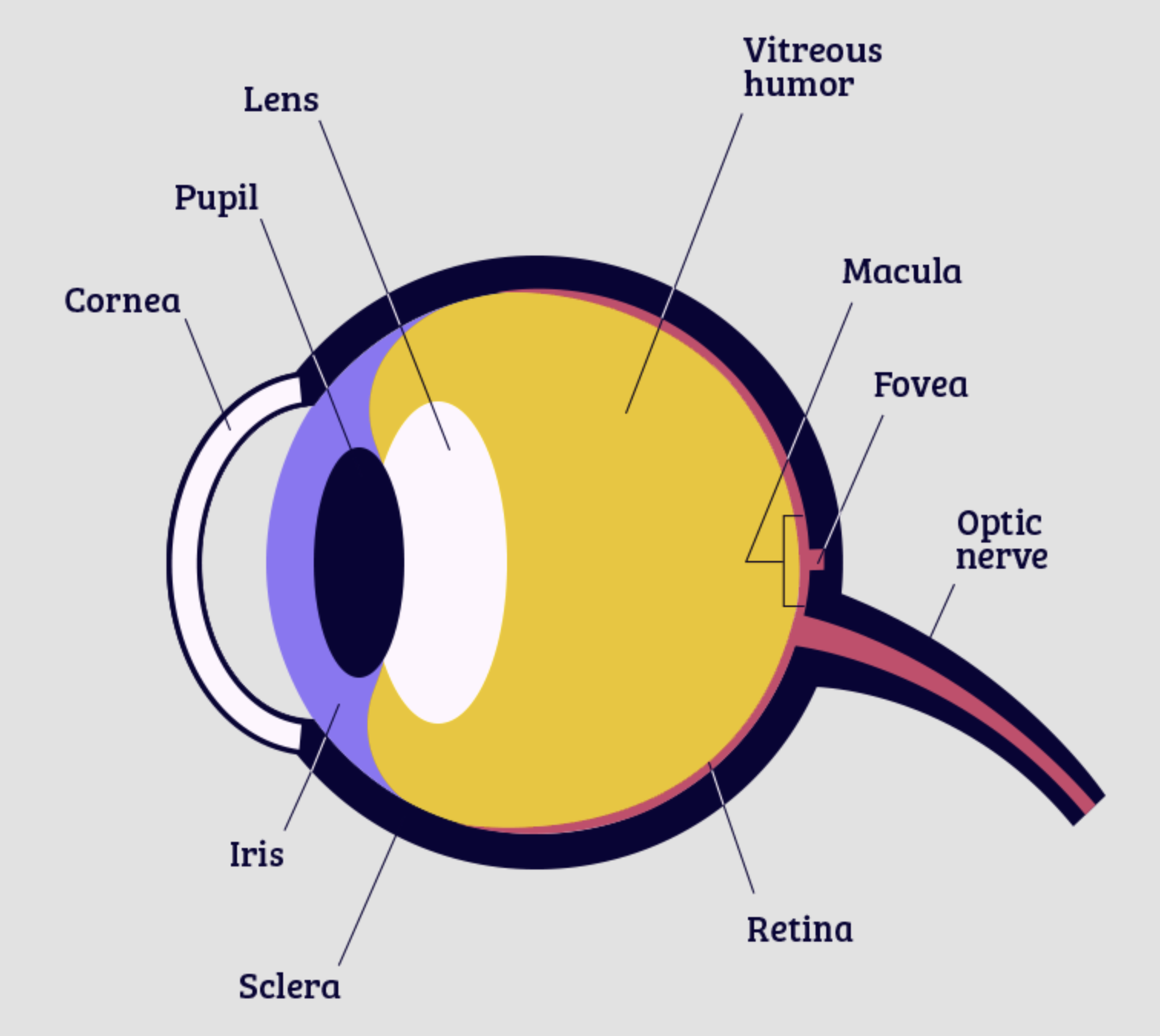
sclera
protective white outer surface of eye
iris
outer pigmented layer, inner layer of blood vessels

cornea
covers iris and pupil, very sensitive to touch
ciliary muscle
controls shape of lens
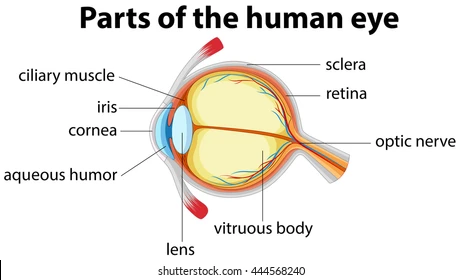
aqueous humour
fluid in anterior chamber, continually replenished
virtuous humour
fluid in posterior chamber, not replenished, floaters form
choroid
blood vessels in eye, nourishes retina
retina
detects light and initiates neural messages
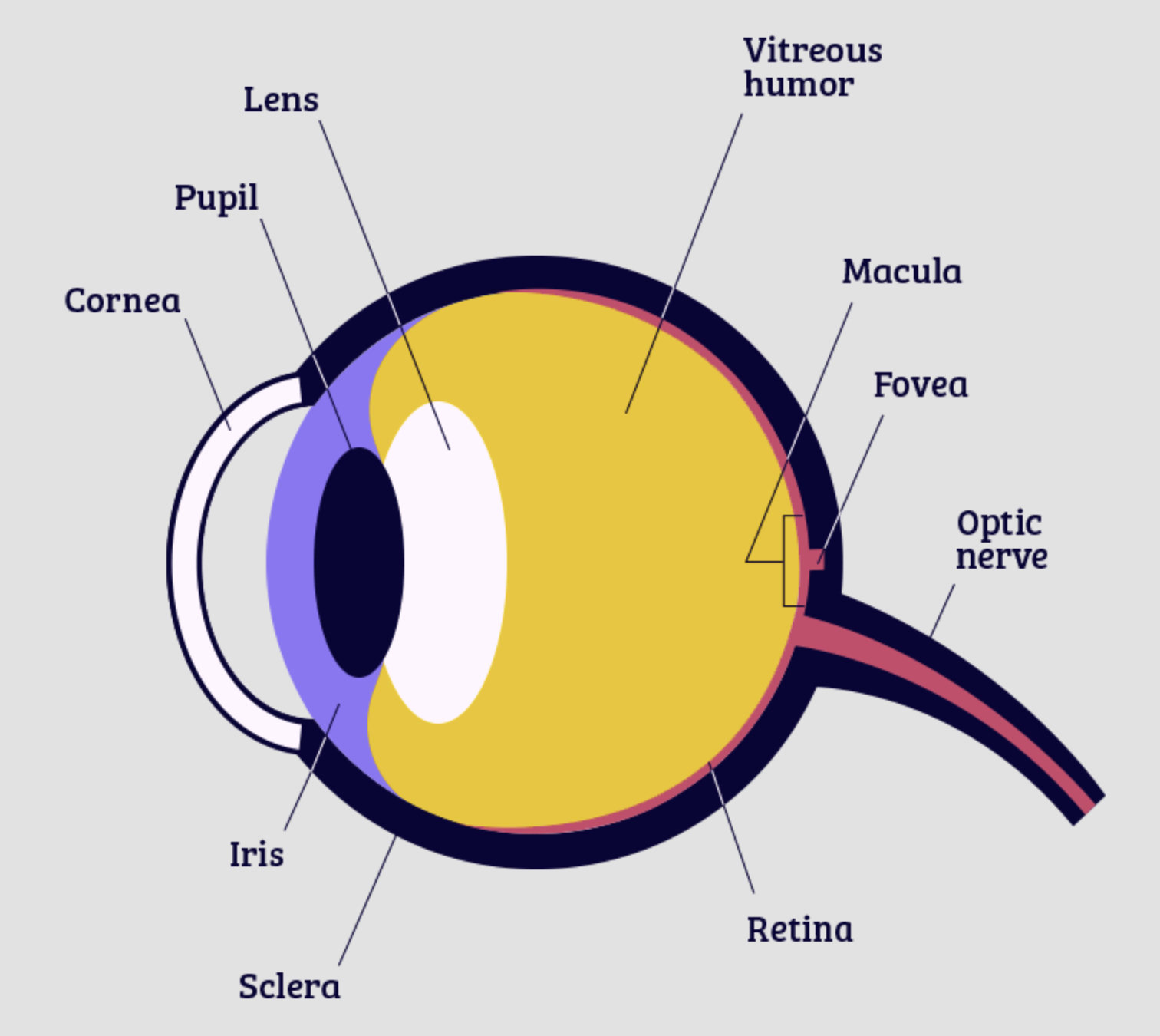
macula
process what is in front of us, yellow pigmented spot
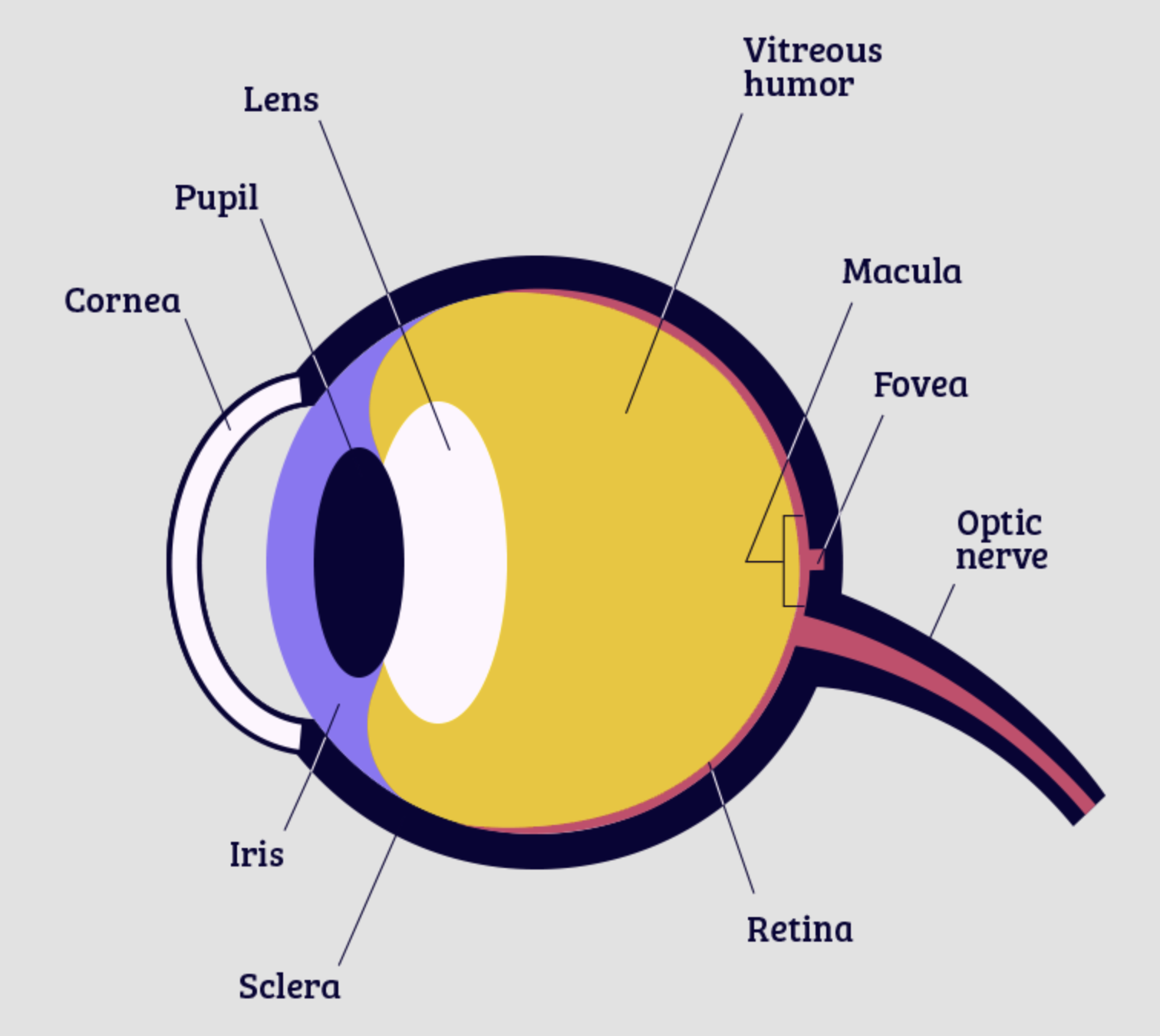
fovea
depression in retina where visual acuity is highest
light passes through shallowest layer
centre = only cones, densely packed
away = more rods and fewer cones, less dense
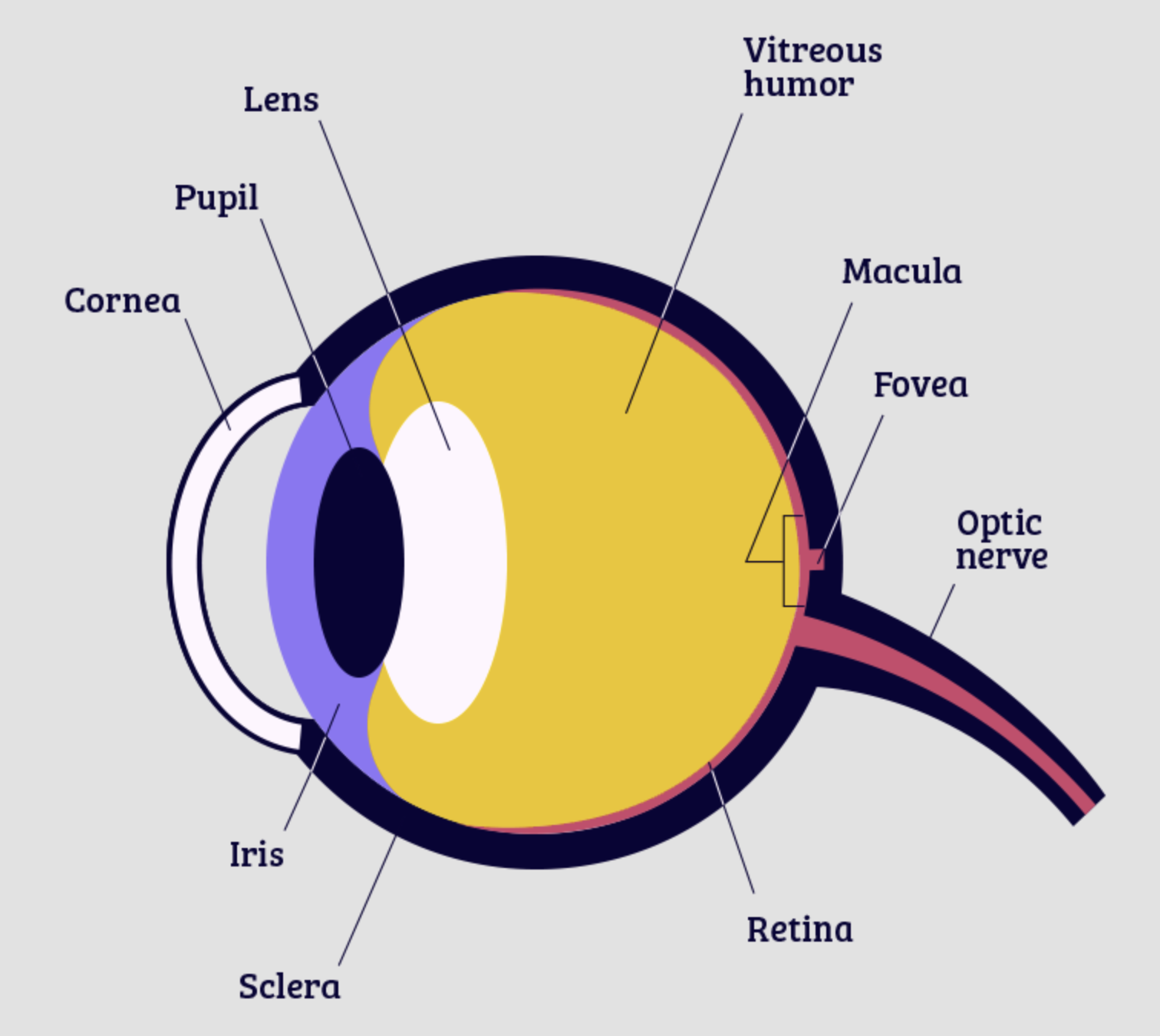
optic disc
point of exit for axons leaving eye
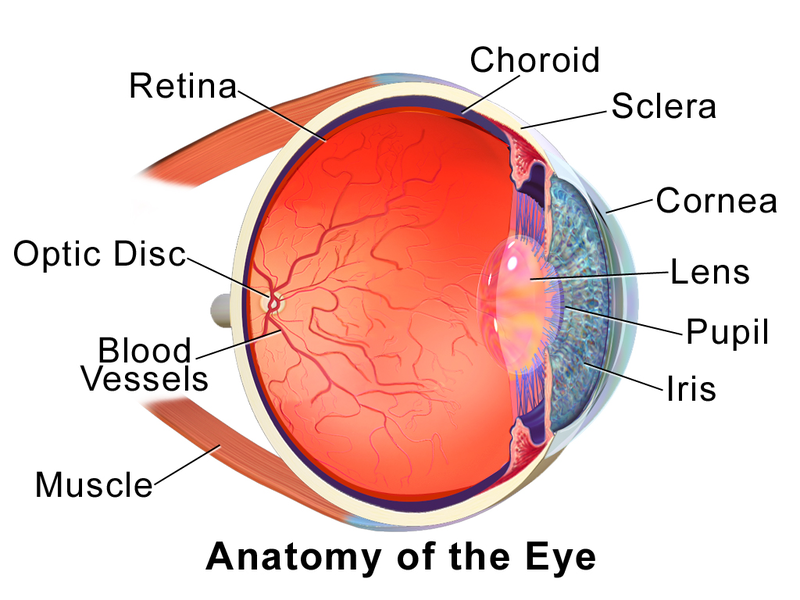
optic nerve (III)
send visual messages to brain to help you see
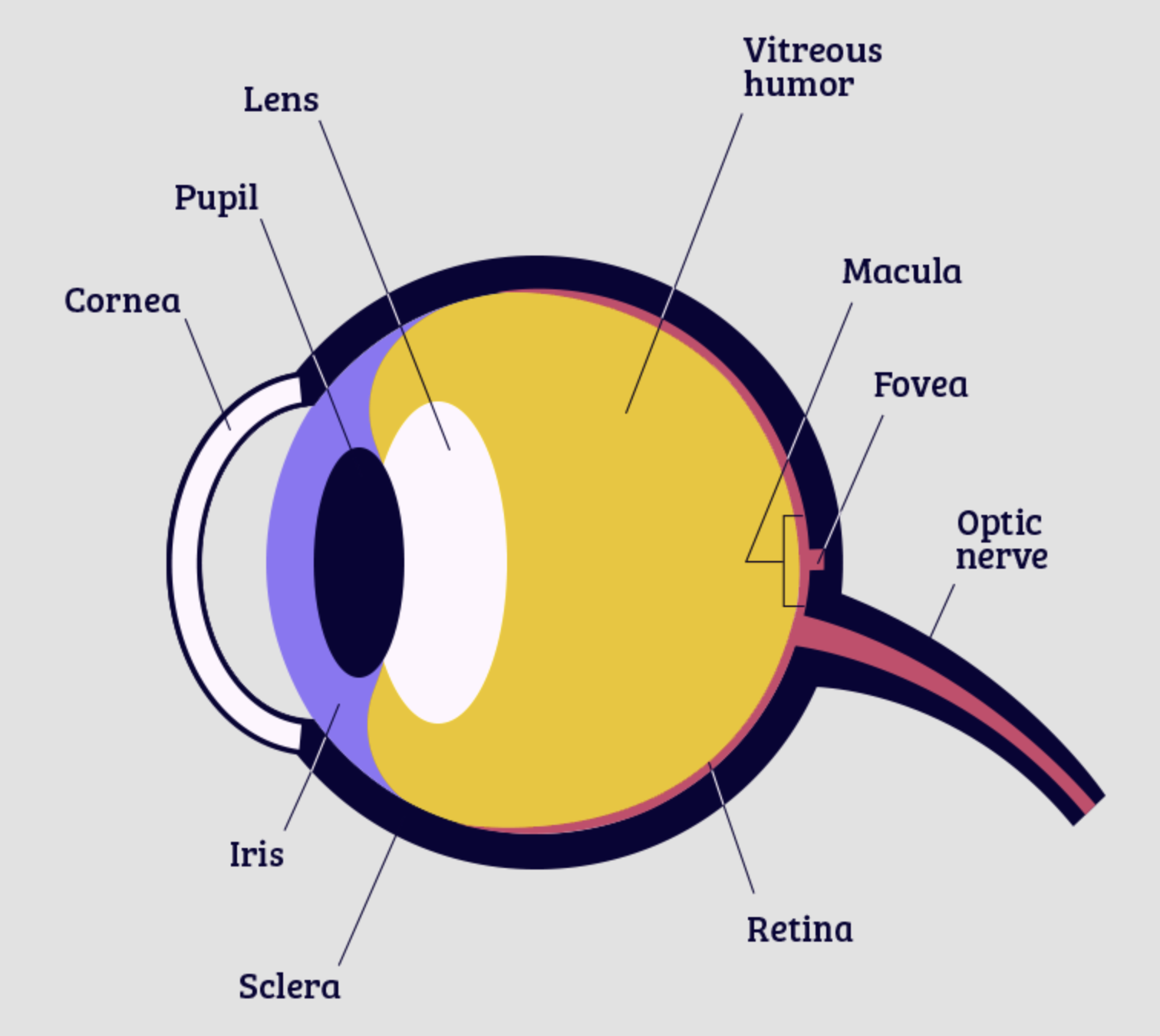
what parts of the eye are for seeing?
optical apparatus: cornea, aqueous humour, lens, vitreous humour, iris
neural apparatus: retina - macula, fovea, optic disc, blood vessels
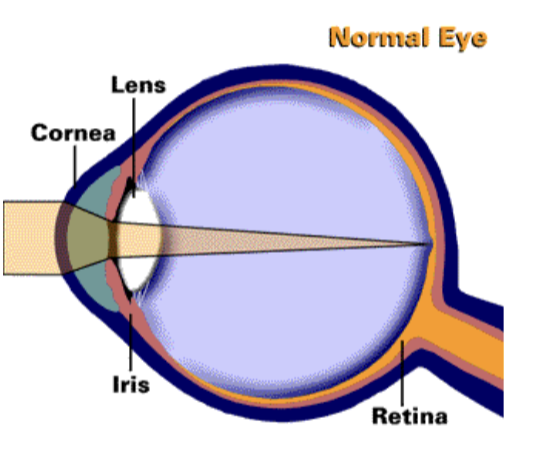
what does the optical apparatus do?
light emitted is transmitted or reflected to eye and is then transmitted through cornea, aqueous humour, lens, and vitreous humour → image is focused on the retina (photoreceptors absorb light)
what does sharpness of an image depend o?
2/3 ability of cornea, 1/3 ability of lens, aqueous, and vitreous humours to refract light
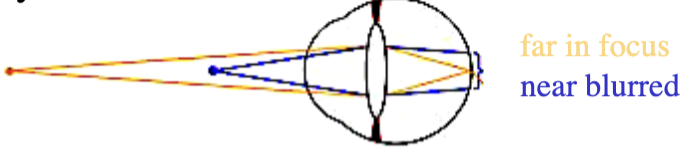
what does the eye look like in a relaxed state?
farther away is in focus, nearer is blurred
accommodation
process by which eye changes its focus by changing shape of the lens
fatter lens = increase of optical power of eye to bring images of near objects into focus (like a camera lens)
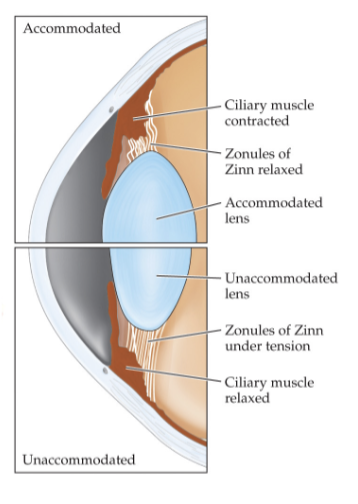
cataract
opacity of crystalline lens of eye can be congenital or develop in later adulthood - interferes with retinal image quality
treated by surgical removal and replacement of lens