Potassium Disorders Discussion
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
what are 4 reasons that potassium leaves cells (causing hyperkalemia)
1) hyperglycemia: increased osmolality in the ECV leads to water being drawn out of cells and K+ follows by solvent drag
2) cell necrosis/breakdown (hemolysis, rhabdomyolysis): may be associated with elevations in other cellular components (LDH, muscle enzymes such as creatinine kinase)
3) fasting: decreases basal insulin levels and may reduce insulin stimulated cellular K+ uptake
4) acidosis: H+ may move intracellularly in exchange for K+
use this case for the following questions
what are some things you might see in hypertension end organ damage?
1) heart: L ventricular hypertrophy
2) kidneys: albuminuria, decreased GFR
3) brain: stroke (angiopathy)
4) eyes: retinopathy (edema, hemorrhage, exudates)
5) vascular system: increased intima-media thickness and arterial stiffness (arteriosclerosis)
what is the rationale for using diuretics to treat the HTN of the patient in case 1?
diuretics enhance urinary Na+ losses (decrease Na+ reabsorption) which cause a small ECV depletion (decrease in pre-load). this is enough to ease arterial resistance (and decrease cardiac output), and therefore, decrease BP in >60% of people
diuretcs can be used as single agents, but are often used with other agents. what is an example of this?
diuretics plus beta blockers reduces long-term incidence of stroke and coronary heart disease
why was hydrochlorothiazide (HCTZ) used for this pt?
thiazides are the most commonly used diuretics: they act on the DCT in small doses, are inexpensive, and time tested
loop diuretcs (furosemide) are usually reserved for acute conditions, such as?
increased edema with congestive heart failure, or in cases of resistant edema, such as in nephrotic syndrome
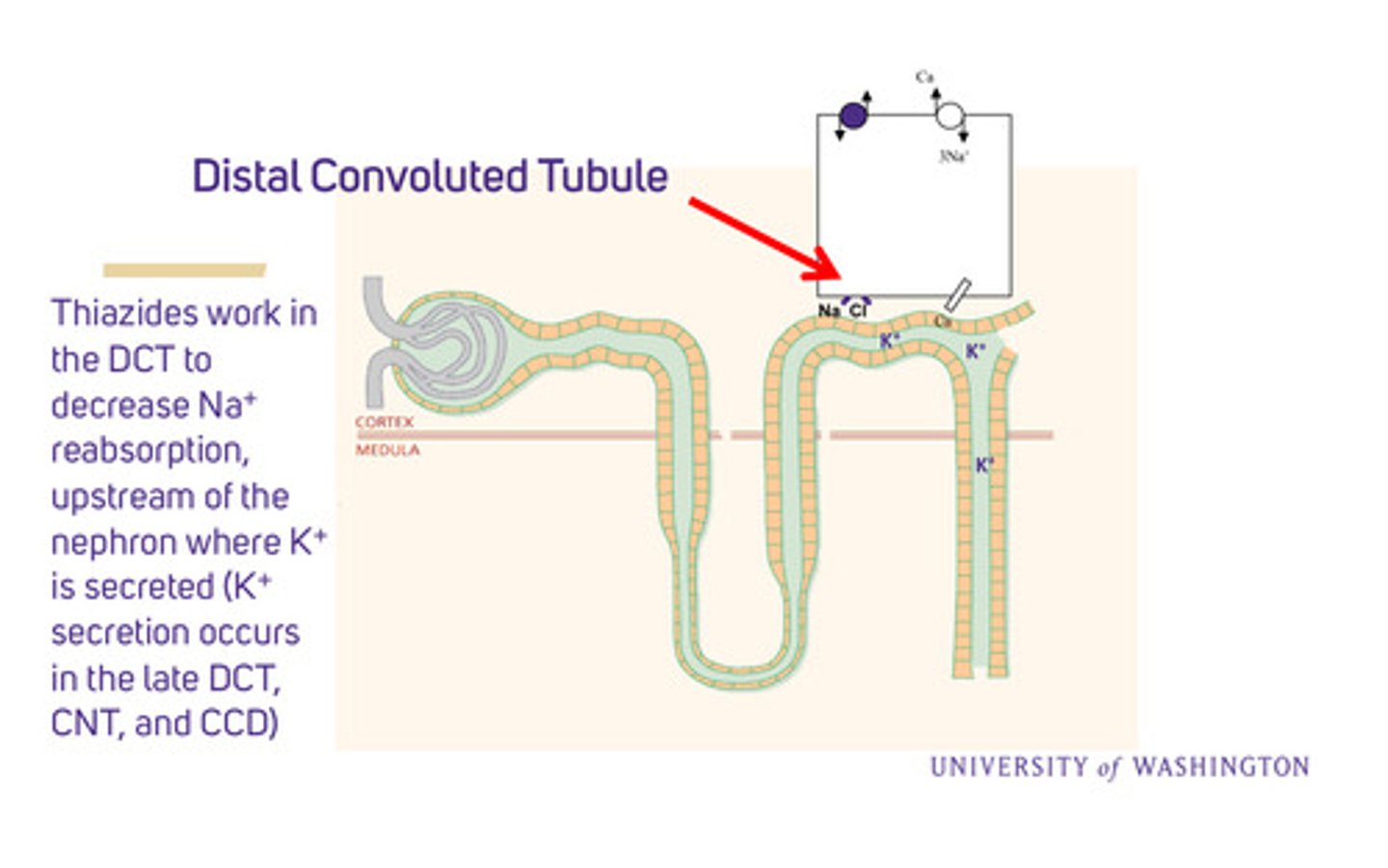
where do thiazides work in the nephron?
in the DCT to decrease Na+ reabsorption, upstream of the nephron where K+ is secreted (this occurs in the late DCT, connecting tubule, and CCD)
what are some common side effects of thiazides?
1) hypokalemia: esp in people with high angiotensin-aldosterone levels; can cause arrhythmias, including fatal ones
2) excessive diuresis: can lead to too much volume depletion, which might result in poor perfusion of the kidney, called "pre-renal" uremia
3) glucose intolerance (IFG and eventual hyperglycemia)
4) metabolic alkalosis (H+ loss)
5) gout (uricemia)
what are the 2 main mechanisms of how thiazides cause hypokalemia?
1) by inhibiting Na+ reabsorption in the DCT, increased Na+ and H2O are delivered to the K+ secreting sites (CNT and CCD), where principal cells pick up the Na+, which then secrete K+
2) urine NaCl and H2O loss —> ECV depletion —> renin (JGA granular cells) expression —> A-II —> increased aldosterone, which stimulates Na+ reabsorption in the CCD (via ENaC) in exchange for K+ secretion (via ROMK)
how do K-sparing diuretcs prevent K+ loss?
spironolactone and amiloride prevent K+ loss in the urine by inhibiting Na+ reabsorption in the CCD, thus inhibiting K+ secretion
what are 2 ways to manage hypokalemia
1) oral potassium supplements (least expensive)
2) potassium sparing diuretics (spironolactone, amiloride)
sometimes potassium wasting (thiazides) and potassium sparing diuretics (aldosterone receptor antagonists, ENaC inhibitors) are used together
use this case for the following questions
case 2 pt's labs
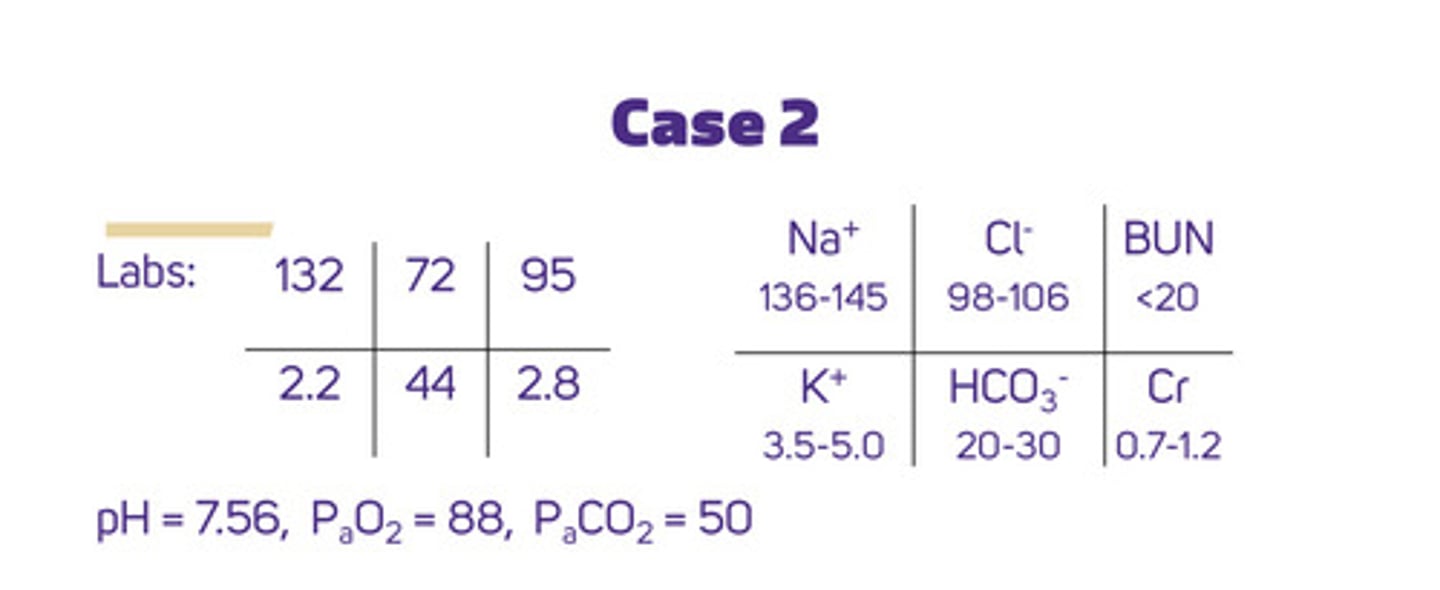
what is the pt's volume status (how do we determine this) and what does that tell us?
volume status can be determined from history, physical exam (key determinant), and labs:
1) history: clear hx of vomiting; pt may describe thirst, weakness, and lightheadedness
2) PE: has orthostatic hypotension (postural drop in BP), tachycardia, and poor skin turgor; there is absence of signs of volume overload (edema, raised JVP, etc)
3) labs: he has a raised BUN:creatinine ratio (>20:1), suggestive of volume depletion, but not specific
overall: having signs of volume depletion = he has a total salt (Na+) deficit
what does his serum sodium tell us?
hyponatremia —> he has an excess of total body water
what is happening with his potassium?
hypokalemia —> initially he is losing K+ in his emesis (vomiting), but gastric secretions only contain a small amount of K+ (5-10 mEq/L) [note that diarrhea can have a much higher potassium concentration (35-60 mEq/L)] —> main reason for his hypokalemia is potassium wasting by the kidneys
volume depletion stimulates the production of ? to try to do what
aldosterone (reabsorb Na+, secrete K+) to try to increase volume, but since his hypokalemia is dangerously low, he needs K+ supplementation immediately (either IV, or PO if vomiting can be controlled)
what kind of tx would the case 2 patient benefit from?
he has a total Na+ deficit (volume depletion) and a total water excess (relative to Na+), so he would benefit from IV fluids to rapidly correct his volume status; his elevated creatinine levels indicate poor kidney function, so his electrolyte levels would have to be closely monitored