Applied Neuroscience SG
1/166
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
167 Terms
What is the primary excitatory neurotransmitter used in the CNS?
Glutamate
What is the primary inhibitory neurotransmitter used in the CNS?
GABA
What are the primary neuromodulators used in the CNS? What is their purpose?
Dopamine (SNc) & serotonin (brainstem) -- facilitate or inhibit subsequent firing of neurons
R vs. L hemisphere damage: cautious and disorganized BUT aware of impairment (behavioral)
Left (dominant)
R vs. L hemisphere damage: impulsive, poor judgment, poor insight, unrealistic, safety risk (behavioral)
Right (nondominant)
R vs. L hemisphere damage: disorganized, processing delay, highly distractible (intellectual)
Left (dominant)
R vs. L hemisphere damage: difficulty w/ abstract reasoning and synthesizing, rigidity of thought, memory impairment related to perception (intellectual)
Right (nondominant)
R vs. L hemisphere damage: difficulty perceiving emotions & expressing (-) emotions
Right (nondominant)
R vs. L hemisphere damage: difficulty expressing (+) emotions
Left (dominant)
R vs. L hemisphere damage: task performance fluctuations
Right (nondominant)
R vs. L hemisphere damage: aphasias, apraxia, and impairments in analytic functions
Left (dominant)
R vs. L hemisphere damage: hemineglect, impairments in complex visual-spatial abilities
Right (nondominant)
R vs. L hemisphere damage: severe personality or emotional changes, difficulty w/ constructional ability, impaired geographic orientation
Right (nondominant)
R vs. L hemisphere function: language
Left (damage --> aphasias)
R vs. L hemisphere function: skilled motor function (aka praxis)
Left (damage --> apraxia)
R vs. L hemisphere function: sequential & analytic abilities (arithmetic, music, and sense of direction)
Left (damage --> impairments in analytics)
R vs. L hemisphere function: visual analysis and spatial attention
Right (damage --> impairment in complex visual-spatial abilities, hemineglect)
R vs. L hemisphere function: perception
Right
R vs. L hemisphere function: prosody (emotion conveyed by tone)
Right (damage --> severe personality or emotional changes--irritability, apathy, psychosis, delusional)
R vs. L hemisphere function: ability to estimate quantity and correctly line up columns of #s, novice or complex musical pieces, finding one's way by overall sense of spatial orientation
Right (damage --> difficulty w/ constructional ability, impaired geographic orientation)
__________ (type of neglect): ignore visual, tactile, auditory $ on neglected side
Sensory neglect (tested w/ sensory extinction)
__________ (type of neglect): perform fewer movements on neglected side
Motor neglect (tested w/ motor extinction)
__________ (type of neglect): tactile & crossed response, cancellation task, and/or clock test
Combined sensory and motor neglect
__________ (type of neglect): do not recognize their arm/leg on the neglected side of the body belongs to them
Conceptual--anosognosia
___________ (lobe): functions in executive function (decision making, judgment), cognition, and motor
Frontal
___________ (lobe): functions in sensation and perception
Parietal
___________ (lobe): functions in auditory/hearing, memory, interpretation of speech, & olfaction
Temporal
___________ (lobe): functions in vision
Occipital
___________ (lobe-ish): involves a compilation of specialized regions that deal w/ homeostasis, olfaction, memory, and emotion
Limbic system
Which Brodmann areas are a part of the frontal lobe?
Prefrontal association cortex, frontal eye fields, supplemental motor cortex (supplemental eye field, premotor cortex), precentral gyrus/primary motor cortex, Broca's area
Which Brodmann areas are a part of the parietal lobe?
Postcentral gyrus/primary somatosensory cortex & secondary and tertiary association/somatosensory association/parietal-temporal-occipital cortex
Which Brodmann areas are a part of the occipital lobe?
Primary visual cortex & secondary and tertiary visual cortex
Which Brodmann areas are a part of the temporal lobe?
Visual inferotemporal cortex, primary and secondary auditory cortex/Heschl's gyrus, higher-order auditory cortex/Wernicke's area, primary olfactory cortex
Which Brodmann area is a part of multiple lobes?
Limbic cortex/ cingulate gyrus/ parahippocampal gyrus
_________ are ependymal cells @ lateral ventricles that produce CSF fluid
Choroid plexus
The lateral ventricles consist of 4 connected regions: frontal horn - _________ lobe, body - __________ & __________ lobes, occipital horn - _________ lobe, & temporal horn - ___________ temporal lobe
Frontal horn - frontal lobe
Body - frontal & parietal lobes
Occipital horn - occipital lobe
Temporal horn - temporal lobe
From the lateral ventricles, CSF flows through the ____________ to reach the third ventricle
Foramen of Monro
From the third ventricle @ the diencephalon (thalamus), CSF flows through the ___________ to reach the fourth ventricle
Cerebral aqueduct/ aqueduct of Slyvius
From the fourth ventricle @ pons, cerebellum, medulla, CSF flows through the ____________ or ___________ to reach the central canal OR subarachnoid space
Foramen of Luedke & Magendie
How does CSF return to the bloodstream?
Arachnoid granulations
Structure: epidural space
Middle meningeal artery
Structure: dura mater
Venous sinuses
Structure: subdural space
Bridging veins
Structure: subarachnoid space
Major vessels & CSF
___________ hematoma/hemorrhage is associated w/ a lucid interval during rapid bleeding --> fast deterioration w/ compression of tissue --> death
Epidural
___________ hematoma/hemorrhage shows up as a white, biconvex lens on imaging
Epidural
___________ hematoma/hemorrhage is associated w/ slow, oozing --> headache, cognition, unsteady gait (chronic) OR quick decline w/ poorer prognosis (acute)
Subdural
___________ hematoma/hemorrhage shows up as a white (acute) or darker (chronic) crescent on imaging
Subdural
___________ hematoma/hemorrhage is associated w/ a sudden catastrophic headache ("thunderclap")
Subarachnoid
___________ hematoma/hemorrhage shows up as white blotches seeping into sulci on imaging
Subarachnoid
___________ hematoma/hemorrhage shows up as a whitened area of the brain w/ symptoms that depend on the area of the brain affected
Intracranial/intraparenchymal
_________ herniation involves the cingulate gyrus --> falx cerebri w/ no clinical presentation (typically)
Subfalcine (note: MAY impact the ACA --> motor and/or sensory loss to the contralateral leg)
_________ herniation involves uncus --> tentorium cerebelli
Transtentorial (uncal)
_________ herniation involves ipsilateral blown pupils (compression of CN III), contralateral hemiplegia (compression of cerebral peduncles), and coma (compression of reticular formation)
Transtentorial (uncal)
_________ herniation involves brainstem --> foramen magnum
Central
_________ herniation involves traction to CN VI, bilateral uncal herniations, tonsilar herniation
Central
_________ herniation involves downward displacement of cerebellar tonsils through foremen magnum --> compresses medulla --> respiratory arrest, BP, instability
Tonsillar
Name the artery most likely involved: L hemineglect, L face and arm motor/sensory loss
R MCA - superior
Name the artery most likely involved: L hemineglect, motor neglect w/ normal strength, some L weakness w/ R gaze preference
R MCA - inferior
Name the artery most likely involved: L hemiplegia + L hemianesthesia + L homonymous hemianopia + L hemineglect + R gaze preference
R MCA - stem
Name the artery most likely involved: R face and arm motor/sensory loss, Broca's aphasia, agraphia
L MCA - superior
Name the artery most likely involved: R face and arm sensory loss (motor findings usually absent), Wernicke's aphasia, R visual field deficit
L MCA - inferior
Name the artery most likely involved: R hemiplegia + R hemianesthesia + R homonymous hemianopia + GLOBAL APHASIA + L gaze preference
L MCA - stem
Name the artery most likely involved: L leg weakness/sensory loss, grasp reflex, frontal lobe behavioral abnormalities, transcortical aphasia
R ACA
Name the artery most likely involved: R leg weakness/sensory loss, grasp reflex, frontal lobe behavioral abnormalities, transcortical aphasia
L ACA
Name the artery most likely involved: L homonymous hemianopia, L hemisensory loss and hemiparesis
R PCA
Name the artery most likely involved: R homonymous hemianopia, alexia w/o agraphia (larger --> aphasia, R hemisensory loss, R hemiparesis)
L PCA
Name the artery most likely involved: contralateral sensory loss and hemiparesis of face and arm > leg
MCA
Name the artery most likely involved: aphasia (L hemisphere) or hemineglect (R hemisphere)
MCA
Name the artery most likely involved: hemianopia/ gaze preference to side of lesion
MCA (stem)
Name the artery most likely involved: contralateral motor and/or sensory loss of leg > face and arm
ACA
Name the artery most likely involved: frontal lobe dysfunction -- apraxia (L hemisphere > R), impaired judgment (R hemisphere > L), grasp reflex, abulia (indecisiveness), incontinence, flat affect
ACA
Name the artery most likely involved: contralateral homonymous hemianopia
PCA
Name the artery most likely involved: proximal/deep infarcts @ thalamus & posterior limb of internal capsule --> contralateral sensory loss and hemiparesis, thalamic aphasia, alexia
PCA
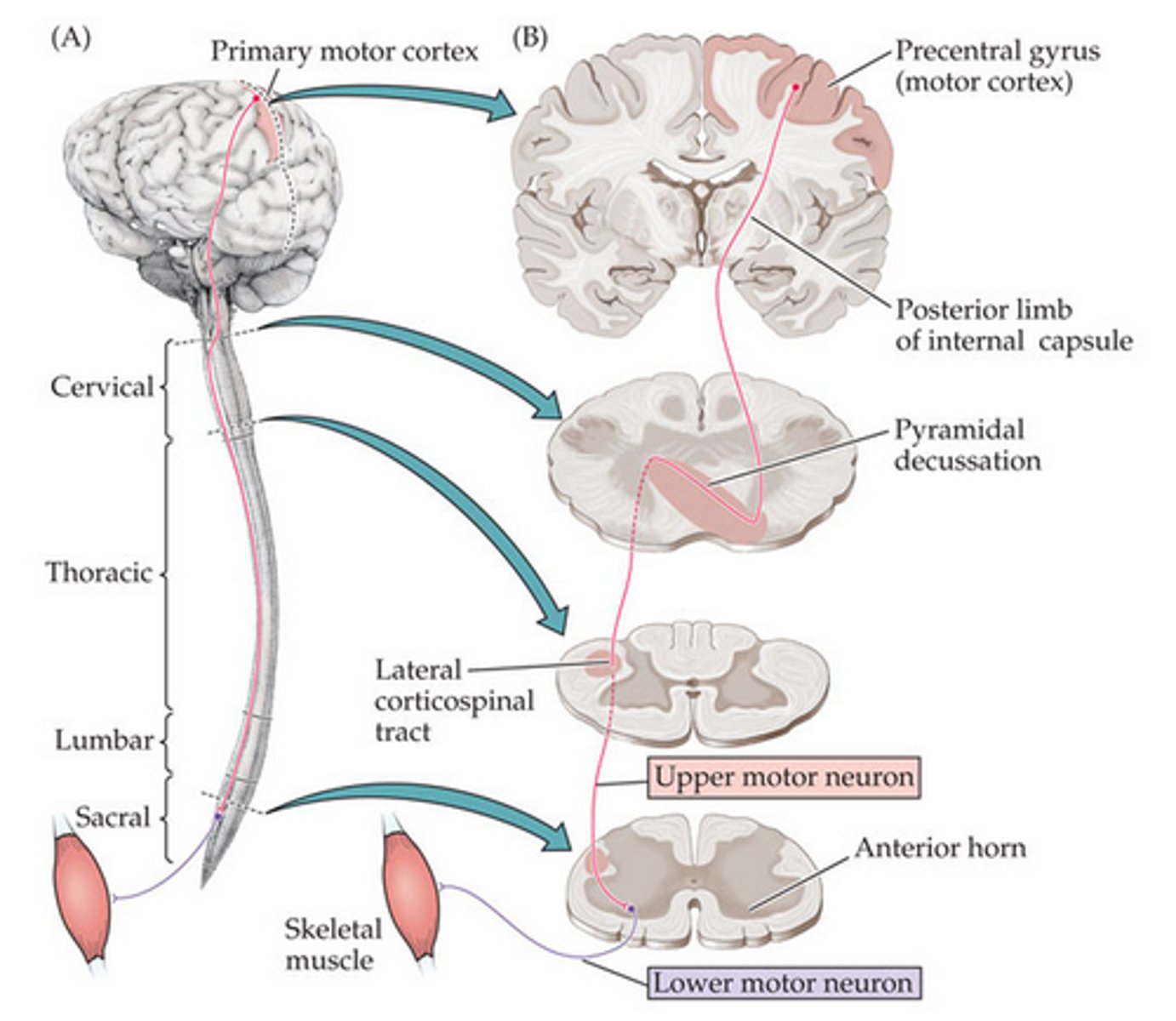
Function: lateral corticospinal tract
Voluntary movement of contralateral limbs
Crossing: lateral corticospinal tract
Pyramidal decussation of caudal medulla
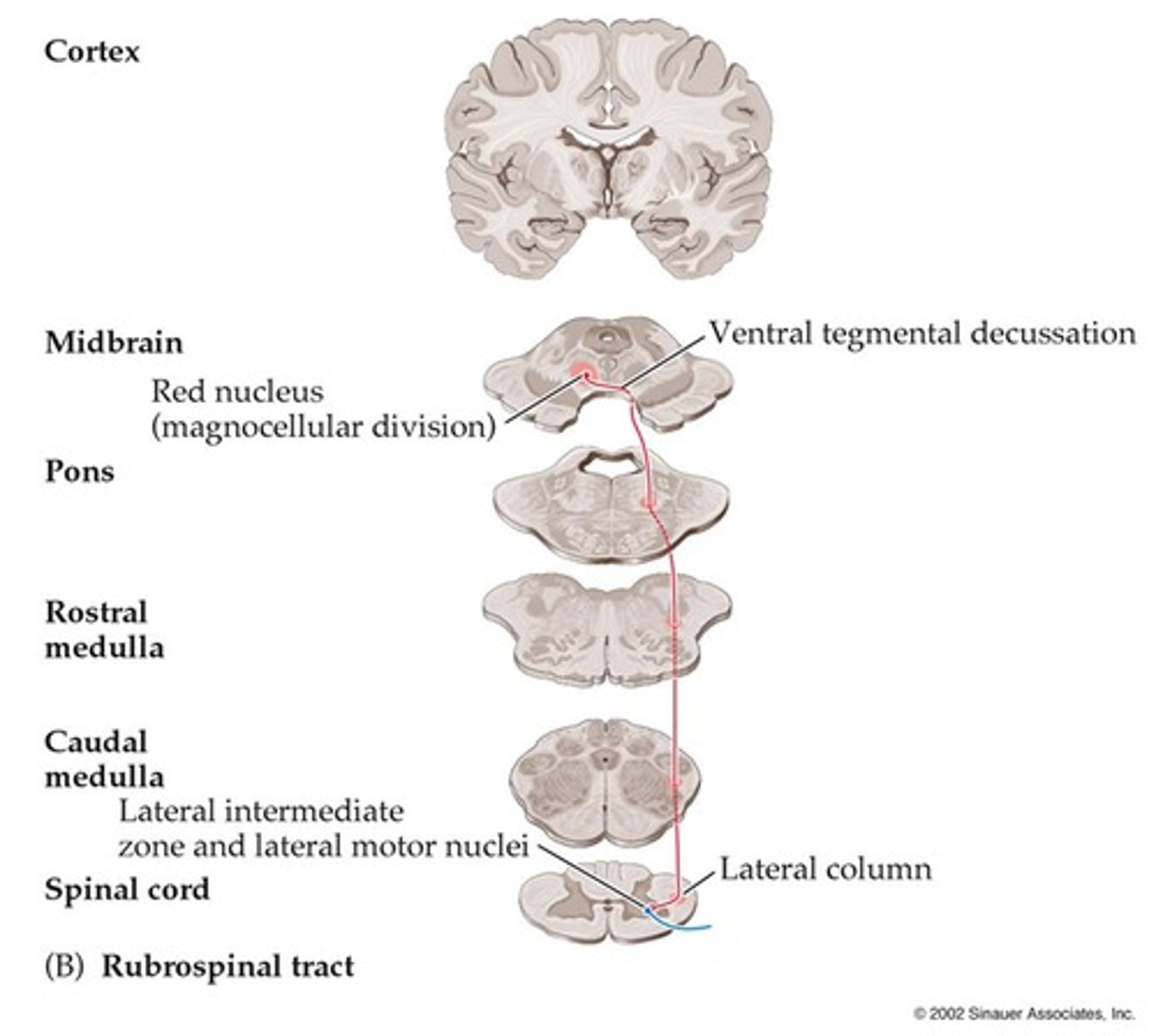
Function: rubrospinal tract
Unconscious movement of limbs; posturing (especially during injury--i.e., non-purposeful flexion)
Crossing: rubrospinal tract
Ventral tegmental decussation of midbrain
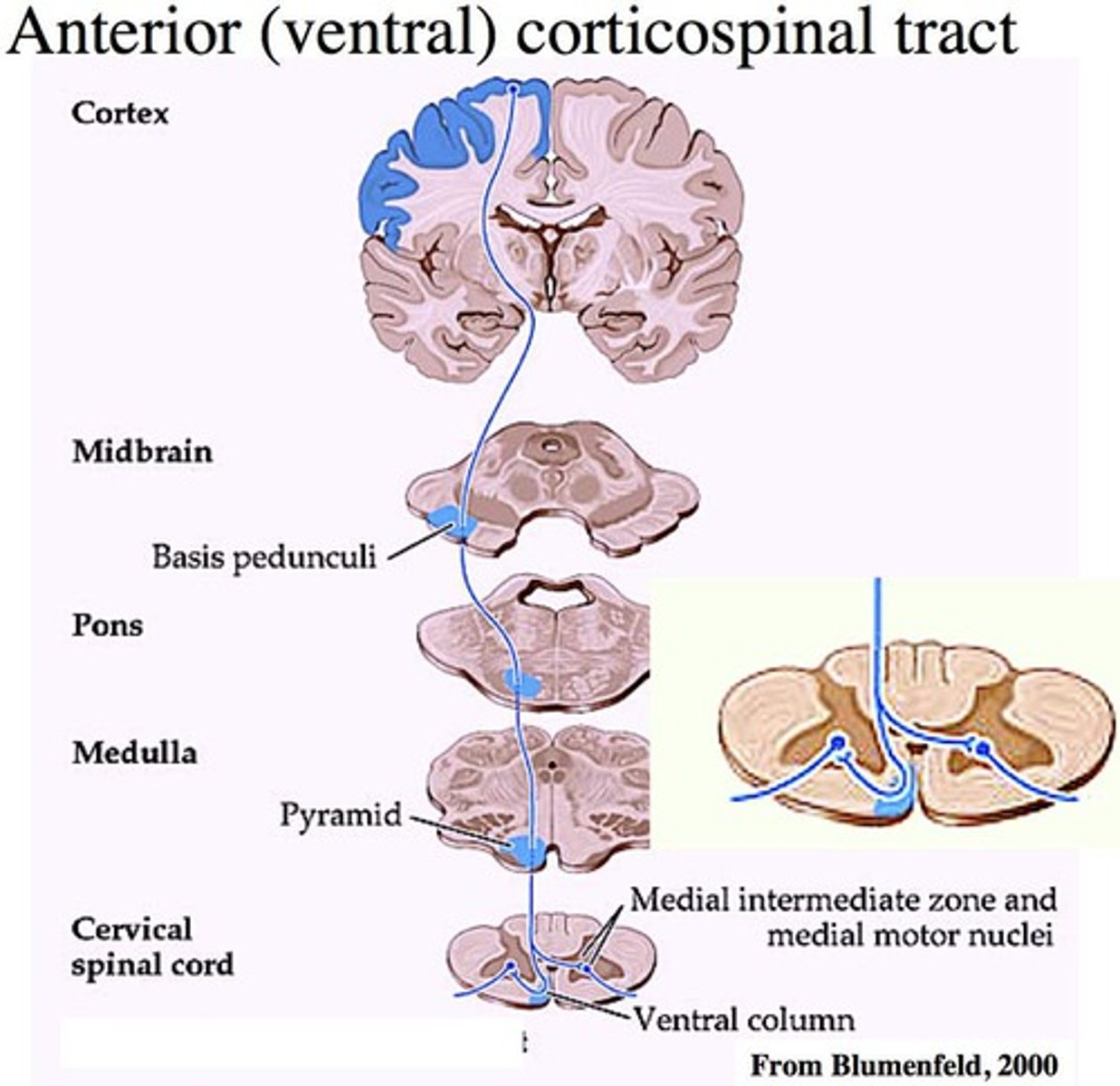
Function: anterior corticospinal tract
Voluntary trunk control and proximal girdle muscles
Crossing: anterior corticospinal tract
WARNING!! The anterior corticospinal tract does NOT cross. It remains ipsilateral throughout the spinal cord until it birfurcates @ its level of termination.
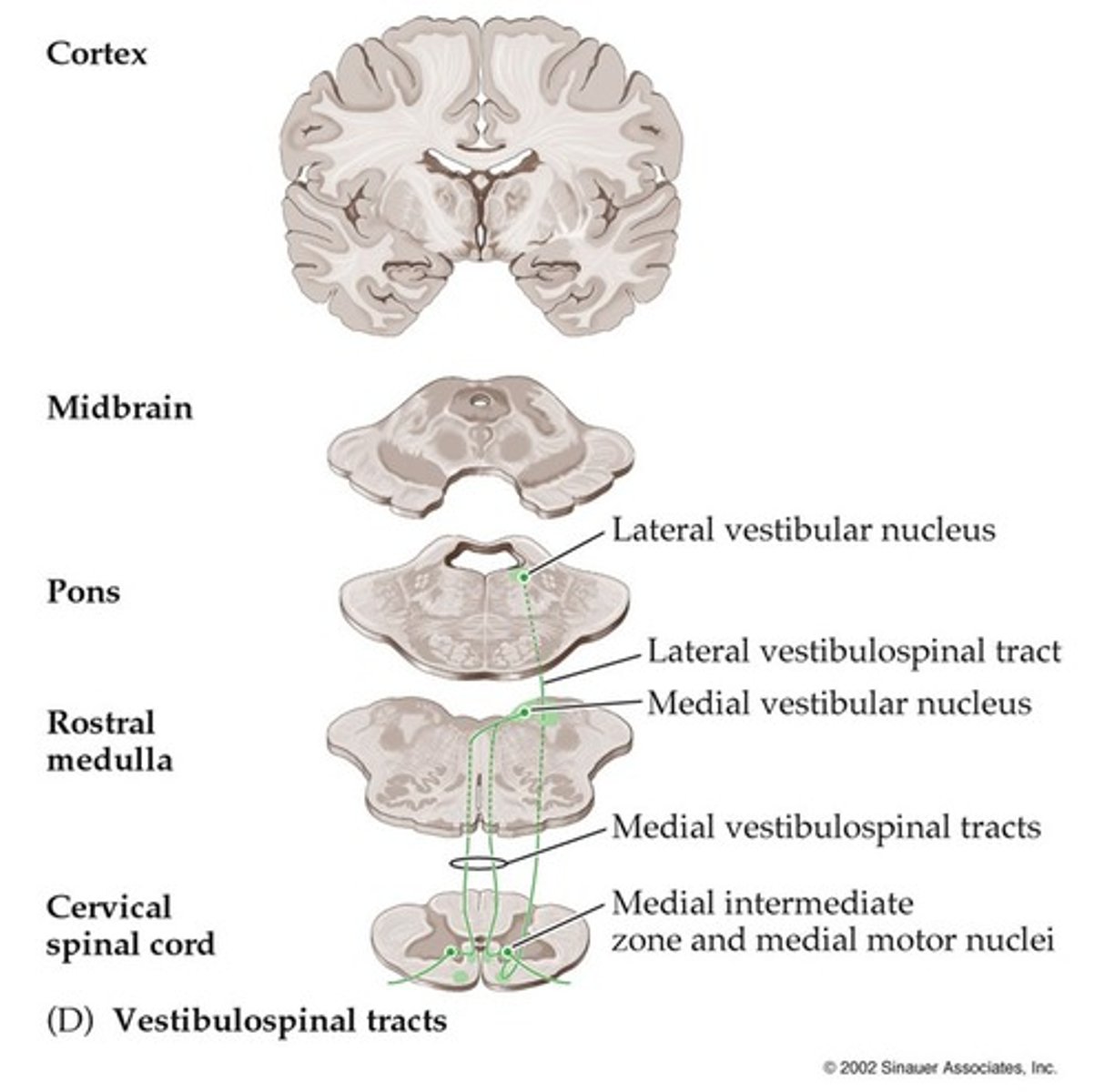
Function: medial vestibulospinal tract
Positioning of head and neck via vestibular input
Crossing: medial vestibulospinal tract
Bifurcates in medial intermediate zone of spinal cord (technically, this means it doesn't cross per say)
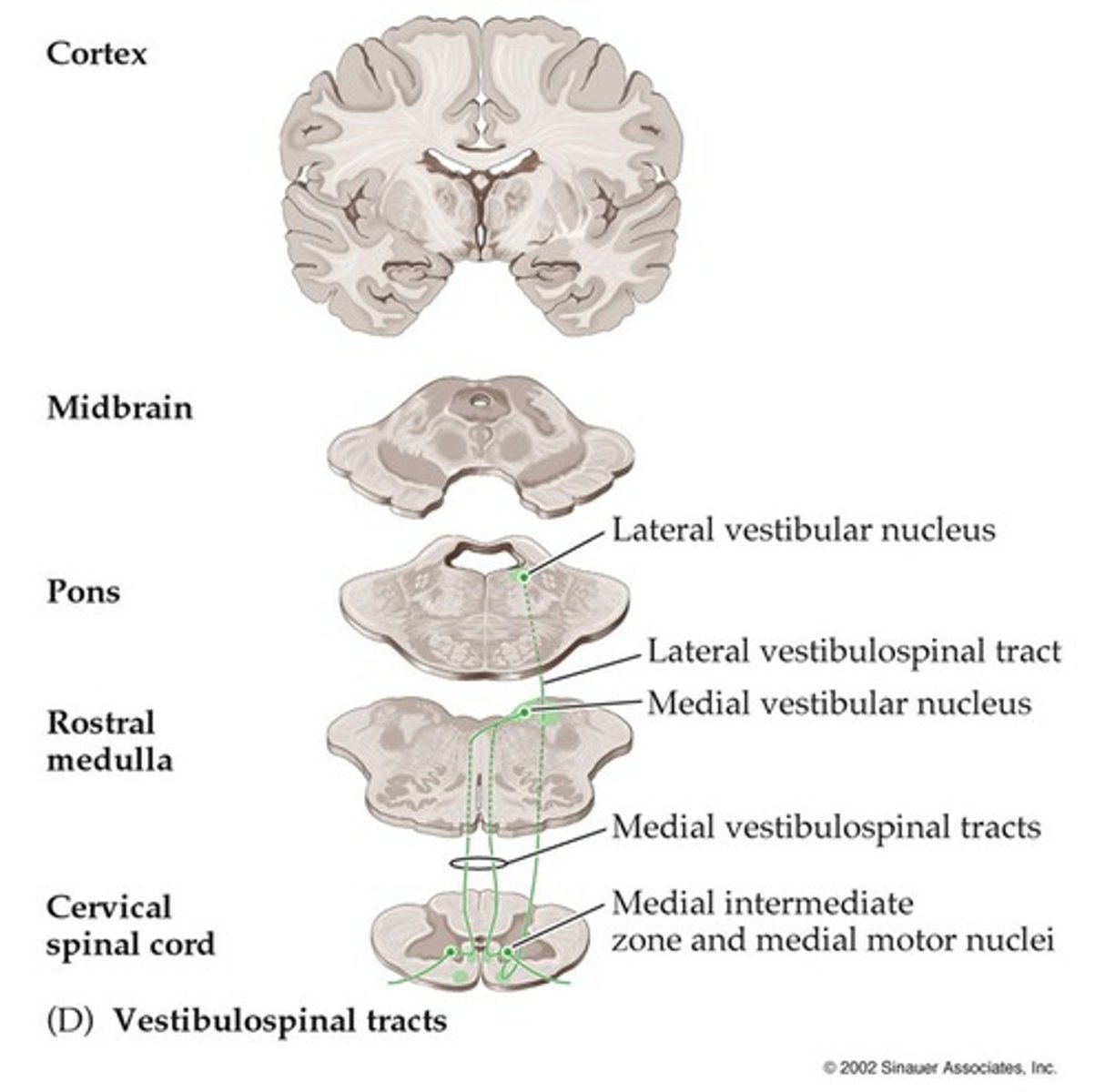
Function: lateral vestibulospinal tract
Balance via promotion of antigravity postural control and protective extension
Crossing: lateral vestibulospinal tract
WARNING!! The lateral vestibulospinal tract does NOT cross.
Function: tectospinal tract
Coordination of head and eye movement via visual and auditory info
Crossing: tectospinal tract
Dorsal tegmental decussation of midbrain
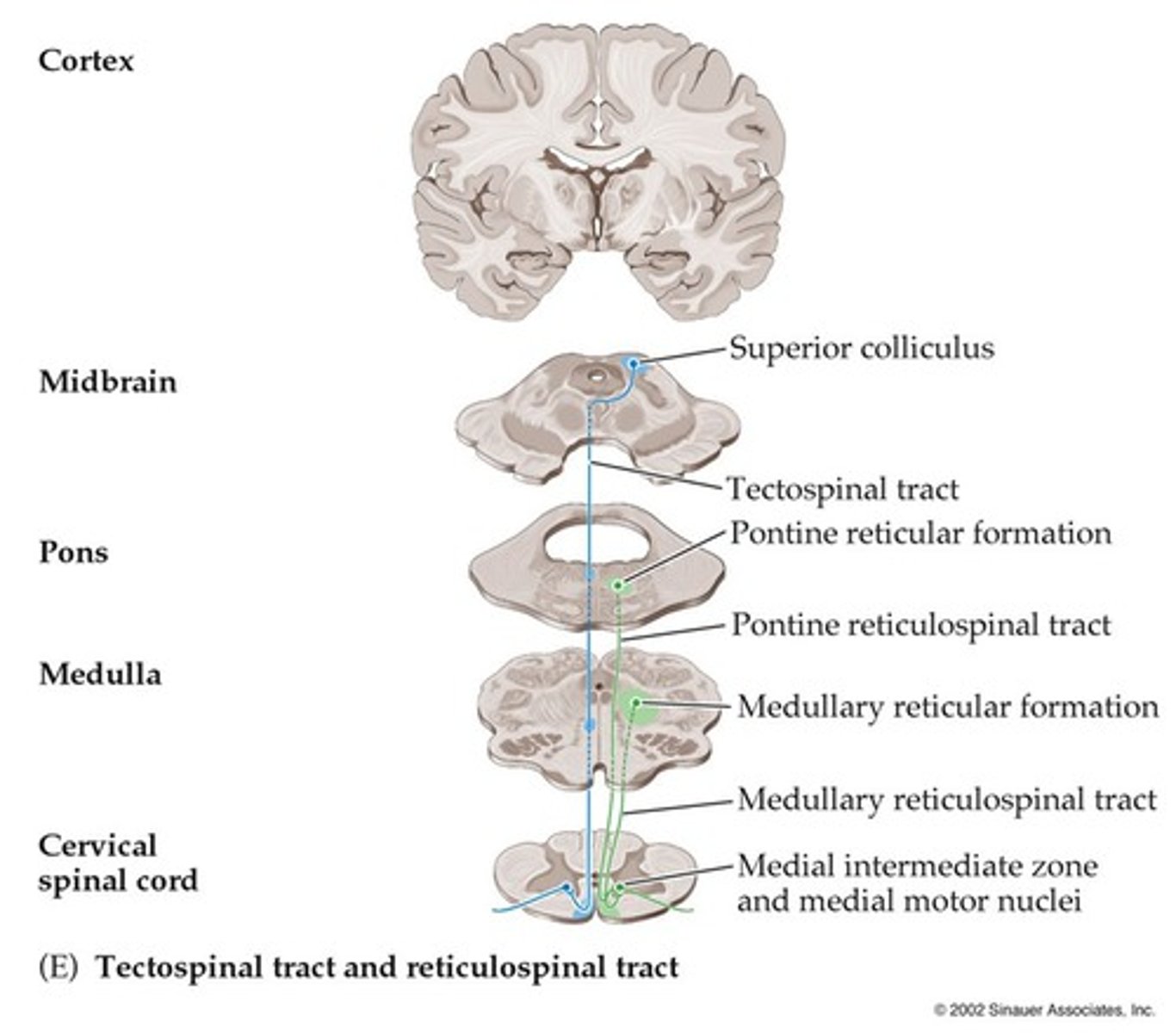
Function: reticulospinal tract
Automatic posture and gait-related movements
Crossing: reticulospinal tract
WARNING!! The reticulospinal tract does NOT cross.
Function: DCML pathway
Afferent transmission of fine & discriminative touch, CONSCIOUS proprioception, vibration
Function: anterolateral pathway
Afferent transmission of noxious $, temperature, & crude touch
Crossing: DCML pathway
Arcuate fibers of medulla
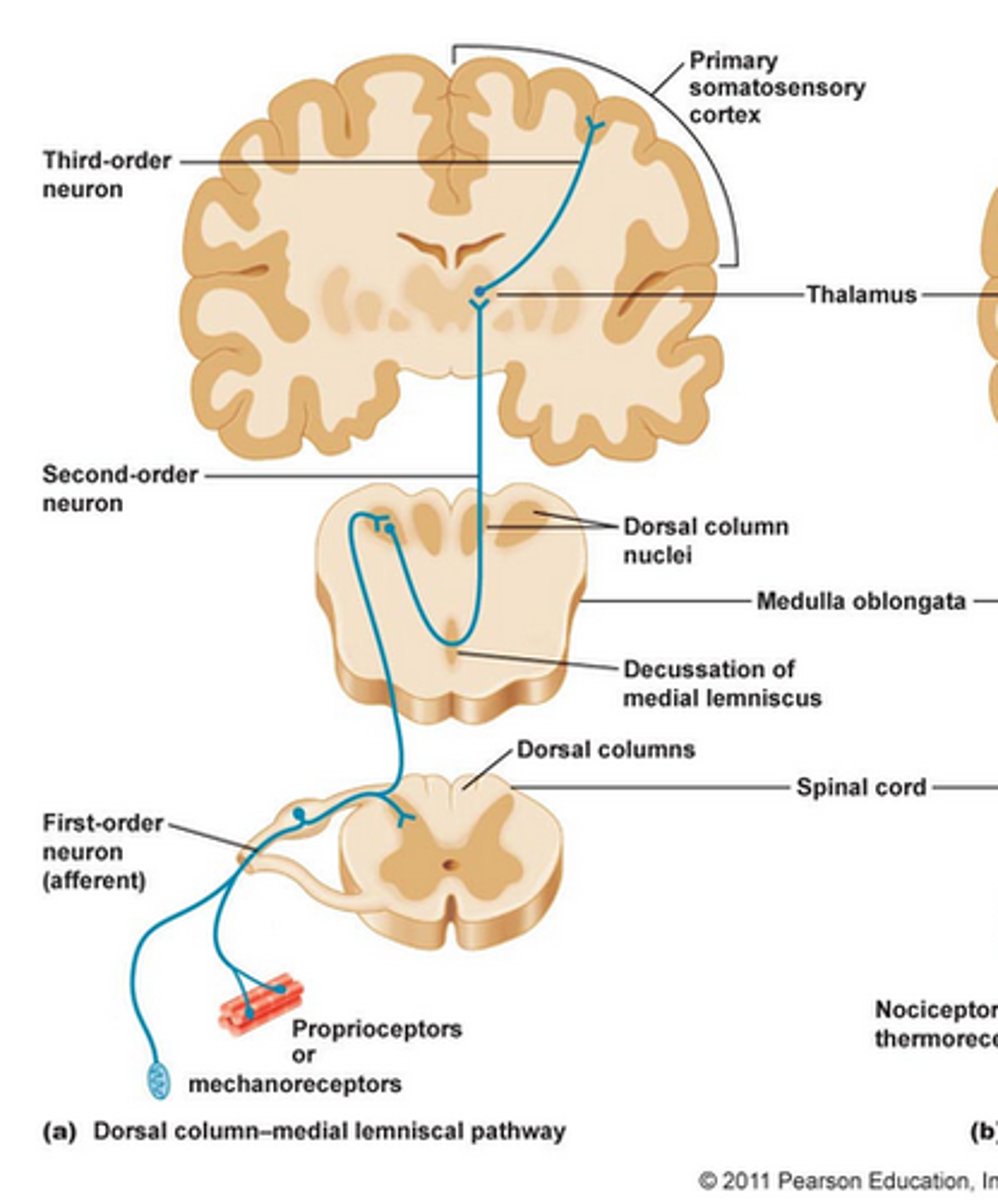
S/S: DCML pathway
Patient may report tingling, numbness
S/S: anterolateral pathway
Patient may report sharp, burning, and/or severe pain
Crossing: anterolateral pathway
Anterior white commissure of spinal cord -- IMMEDIATE CROSSING
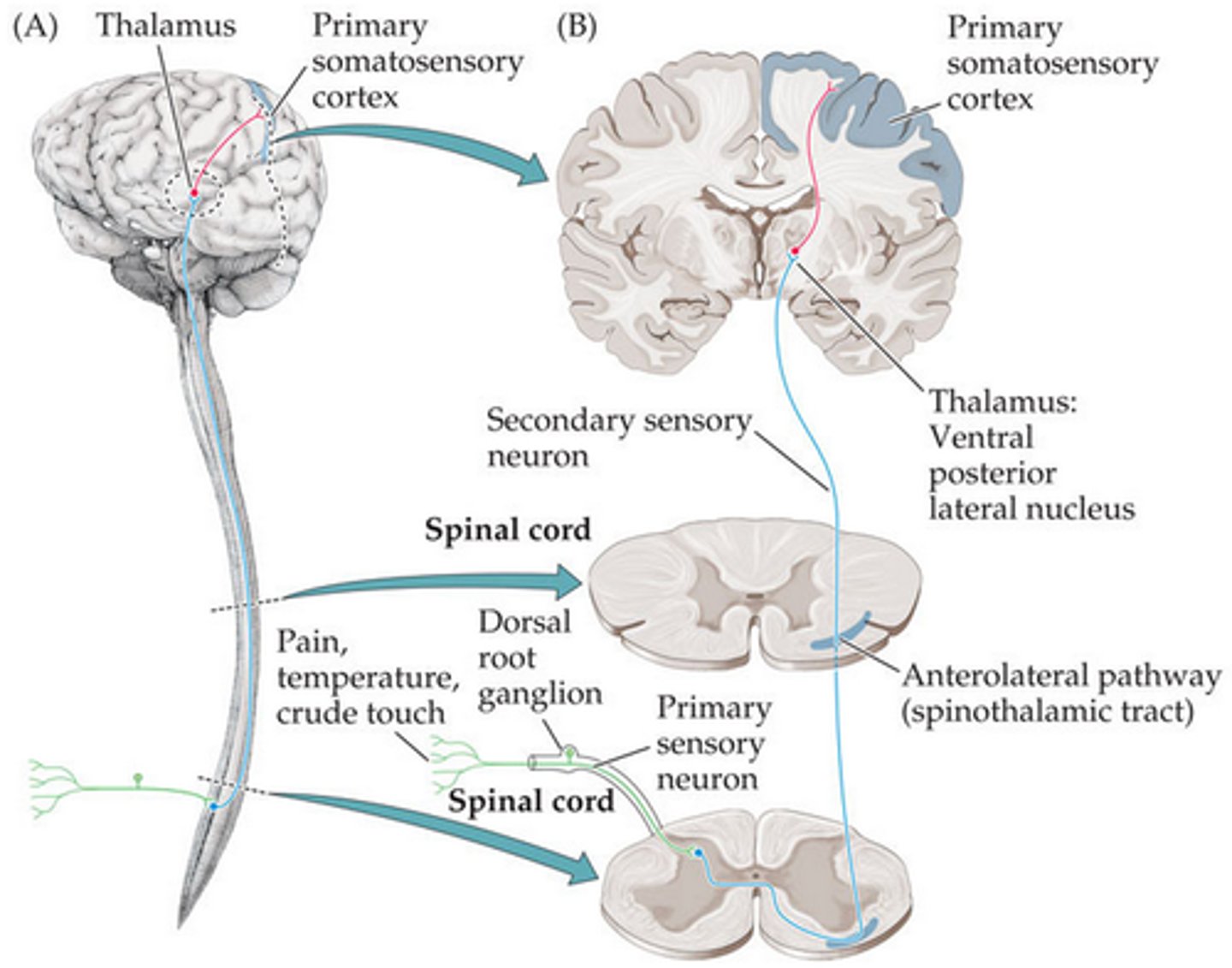
Name the anterolateral pathway: discrimination of location & intensity of $ -- "sharp pain in my heel, hot water on my hand"
Spinothalamic
Name the anterolateral pathway: emotional & arousal aspects to medulla-pontine reticular formations -- "ouch, that hurts"
Spinoreticular
Name the anterolateral pathway: central modulation of $ to periaqueductal gray -- "aah, that feels better"
Spinomesencephalic
PNS vs. SNS: pupil constriction
PNS (via CN III)
PNS vs. SNS: heart rate increases
SNS
PNS vs. SNS: bronchodilation
SNS (hint: bronchodilation vs. bronchoconstriction always follows pupillary repsonse)