Clinical Correlations
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
Nerve root supply to Stomach
T6-T9
Nerve root supply to Small intestines
T8-T10
Nerve root supply to APPENDIX
T10
Nerve root supply to Ascending & Transverse colon
T10-T11
Nerve root supply to Proximal descending colon
T12-L1
Nerve root supply to Distal descending colon
L2-L3
Nerve root supply to Rectum
S2-S4
In colonic diverticulosis multiple false diverticulae develop along where
the large intestine
What are diverticulae
External evaginations or out-pocketings of the mucosa of the colon (Acquired mucosal herniations which protrude through weak areas of the muscular wall)
Where on the colon wall do diverticulae most commonly occur
on the mesenteric side of two bands of taenia coli (omental and free) due to the perforating nutrient arteries
On what section of the large intestines are diverticulae most common
Sigmoid colon
What age is most affected by Colonic Diverticulosis
middle-aged and beyond
Risk factors for Colonic Diverticulosis
Risk factors include: low fiber (high meat) diet, BMI>25
Problems that diverticulae can cause
Can become infected and rupture
gastrointestinal (GI) system has how many major venous systems - name them
2
Systemic venous system
Hepatic portal venous system
What does the Systemic venous system consist of
Veins that drain deoxygenated blood directly towards the heart
Why is the systemic venous system called the caval system
it involves the superior & inferior vena cavae
What does the Hepatic portal venous system consist of
Veins that drain nutrient rich deoxygenated blood from the intestines and the spleen directly towards the liver
In what way is blood supply to the liver unique
the liver is unique in that it receives both oxygenated and deoxygenated blood → from the proper hepatic artery and hepatic portal vein respectively
What is a portal system & 2 examples
Defined as a part of the circulation in which blood draining from the capillary bed of one structure flows through a larger vessel(s) to supply the capillary bed of another structure before returning to the heart
Examples include:
• Hypothalamus and pituitary gland
• Liver
What is Cirrhosis of the Liver
Progressive destruction of hepatocytes
Liver cells are replaced by fibrous (scar) tissue and regenerative nodules (lumps)
➢ Liver becomes firm
➢ Circulation becomes inhibited
Cirrhosis of the Liver treatment
Treatment may involve a shunt of venous blood from the portal system to the caval (systemic) system, or if the cirrhosis is very advanced then a liver transplant may be necessary
Portal hypertension can be a cause for many things. Make a list
Varices
Caput medusa
hemorroids
How does portal hypertension cause Varices, Caput medusa & hemorroids
Portacaval Anastomoses
What causes problems at Portacaval Anastomoses
The hepatic portal vein and its tributaries have no valves, therefore if the venous drainage of the gastrointestinal tract gets blocked at the hepatic portal vein, then blood can bypass the liver by flowing in a reverse direction and drain to the inferior vena cava through an alternative route, causing build up & other problems
Blockage of the left gastric vein results in backflow of blood to where, causing what
If there is a blockage in the left gastric vein, blood can flow back into the esophageal veins, leading to esophageal varices.
Blockage of the paraumbilical veins results in backflow of blood to where, causing what
if there is a blockage in the paraumbilical veins, blood can flow back into the epigastric veins, leading to caput medusae.
Blockage of the anorectal veins results in backflow of blood to where, causing what
If there is a blockage in the superior rectal vein, blood can flow back into the middle and inferior rectal veins, leading to hemorrhoids.
Eosophageal varices can occur at what anastomoses between the portal & caval venous systems
Anastomosis between:
Portal system – Left and right gastric veins
Caval system – Esophageal veins
Caput medusa can occur at what anastomoses between the portal & caval venous systems
Anastomosis between:
Portal system – Paraumbilical veins
Caval system – Epigastric veins
What causes Caput Medusa
If blood is unable to effectively flow through the liver, it can cause retroflow in the paraumbilical veins which now drain into the periumbilical veins
The superficial veins of the anterior abdominal wall (superficial epigastric and thoracoepigastric) then become extremely dilated and varicose which over time look like snakes slithering under the skin
Treatment for portal hypertension
divert the portal blood by creating a “shunt” or create communication between larger veins of the caval system in order to relieve pressure:
• Hepatic portal vein → Inferior vena cava
• Splenic vein → Left renal vein
Haemorrhoids can occur at what anastomoses between the portal & caval venous systems
Anastomosis between:
Portal system – Superior rectal veins
Caval system – Inferior rectal veins
Differences between internal & external hemorrhoids (location, pain level)
Internal hemorrhoids:
▪ Found above the pectinate line
▪ Will not be painful → visceral innervation
External hemorrhoids:
▪ Found below the pectinate line
▪ Would be extremely painful → somatic innervation!
If internal hemorrhoids were damaged, what would the result be
If damaged then would result in bright red blood in the stool as this is close to the source and the blood has not been digested → Lower GI tract bleed
How do external hemorrhoids develop
Develop from varicose perianal veins that are part of the caval system
Name the arteries involved in an anastomosis between the foregut & midgut
Superior pancreaticoduodenal artery
Inferior pancreaticoduodenal artery
Name the arteries involved in an anastomosis between the midgut & the hindgut
Middle colic artery
Left colic artery
What is The Marginal artery of Drummond
term that is used to describe the arteries supplying the midgut and hindgut when collectively they form a continuous circle along the inner border of the large colon
commonest area of colonic ischemia
splenic flexure
Why is the commonest area of colonic ischemia the splenic flexure
During development, the middle colic artery may not meet with the left colic artery
Significance of the anastomosis of the superior and inferior mesenteric arteries
provides COLLATERAL flow in the event of occlusion or significant stenosis
Peritonitis
Infection can occur if gas, fecal matter or bacteria enter the peritoneal cavity which would result in inflammation of the peritoneum
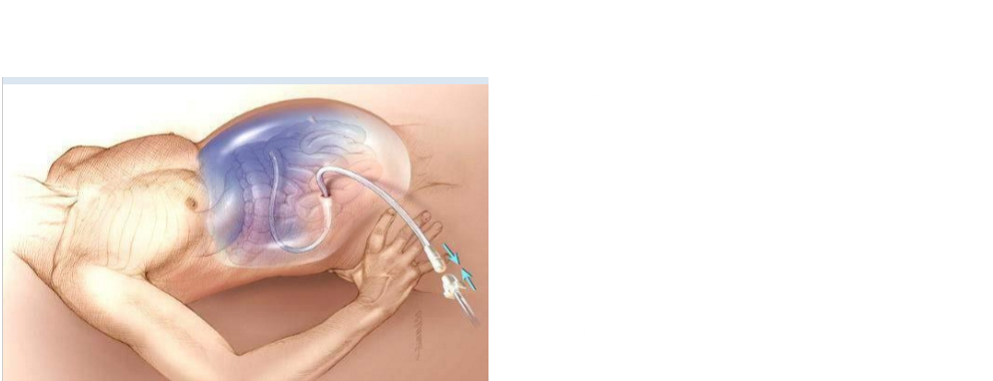
What is this procedure called
Paracentesis
Differentiate between pain felt from Inflammation of PARIETAL/VISCERAL peritoneum
Inflammation of PARIETAL peritoneum
• Sharp, well-localized pain
• Tenderness on palpation
Inflammation of VISCERAL peritoneum
-Generalized, referred pain that is felt in the associated dermatome of the organ
Excess fluid in the peritoneal cavity is called
Ascitic fluid (condition = ascites)
(can contribute to peritonitis)
A fluid rich in cellular elements, serum, fibrin, acid or pus that has seeped out and been discharged from an inflamed organ or vessel
Exudates
(can contribute to peritonitis)
What are Peritoneal adhesion
fibrous bands that form abnormal connections
Give 2 types of peritoneal adhesions
Visceral peritoneum attaching to an adjacent organ
Visceral peritoneum attaching to the parietal peritoneum
What causes peritoneal adhesions to form
Form as a result of damage to the peritoneal surface when sticky fibrin appears in order to assist with the healing process
Complications with peritoneal adhesions
Adhesions limit the normal movement of viscera and could lead to complications:
➢ Intestinal obstruction (a.k.a. volvulus)
➢ Chronic pain
Treatment for peritoneal adhesions
Laparotomy: Surgical incision into abdominal cavity prior to major surgery
Adhesiotomy: Surgical separation of adhesions Peritoneal Adhesions
2 surgical techniques for an appendectomy
1. Through a transverse or grid-iron (muscle-splitting) incision centered at McBurney’s point. 2. Through laparoscopic surgery
both appendectomy surgical techniques involve the correct ligation of what artery
appendicular artery
What nerves are most at risk in the transverse / grid-iron incision at mcBurney’s point
Nerves most at high risk of damage during this surgery due to travelling through the anterior abdominal wall musculature:
• Iliohypogastric nerve (L1)
• Ilioinguinal nerve (L1)
How does the pain differ in initial vs acute appendicitis
Initial appendicitis: General VISCERAL Afferent (GVA) pain fibers are referred to T10 dermatome
Acute appendicitis: General SOMATIC Afferent (GSA) pain fibers are localized at McBurney’s Point
most commonly injured abdominal organ
spleen
How is the spleen the most commonly injured abdominal organ
Despite being protected by the rib cage, a traumatic blow to the left side may fracture the ribs and result in fragments of bone lacerating the spleen
Example could be becoming impaled against the steering wheel during a road traffic accident
If the spleen ruptures, this will lead to
Shock
Intraperitoneal hemorrhage – profuse internal bleeding
Splenectomy
Surgical removal of the spleen to prevent bleeding to death
Splenomegaly
Pathological enlargement of the spleen (up to 10x normal size) accompanied by high blood pressure
Cholelithiasis
Gallstones
small lumps of solid stone-like deposits which form in the gallbladder
Cholelithiasis risk factors
Crystals form when there are high concentrations of cholesterol and can be associated with individuals who are regularly dehydrated
Relatively common in females
Cholelithiasis symptoms
Pain in the right upper quadrant (RUQ)
Pain may be referred to the right neck/shoulder region
Nausea
Cholecystitis → Inflammation of the gallbladder
Jaundice
What is a common constriction site where cholelithiasis often become painfully lodged
hepatopancreatic ampulla
What components make up gall stones
Cholesterol
Calcium
Phosphate
Bilirubin
Triglyceride
Bile acid
Match
hepatolithiasis
cholecystolithiasis
choledocholithiasis
a Gall bladder stones
b Extrahepatic bile duct stones
c Intrahepatic bile duct stones
1c
2a
3b
Describe content of Intrahepatic bile duct stones (hepatolithiasis)(cholesterol/pigment)
Brown pigment & cholesterol stones
Describe content of extrahepatic bile duct stones (choledocholithiasis)(cholesterol/pigment)
Primary stones = brown pigment
Secondary stones = cholesterol
Describe content of Gall bladder stones (cholecystolithiasis)(cholesterol/pigment)
Cholesterol (or black pigment) stones
Cholecystectomy
surgical procedure to remove the gallbladder
Gall stones can cause severe what
biliary colic (pain in the RUQ)
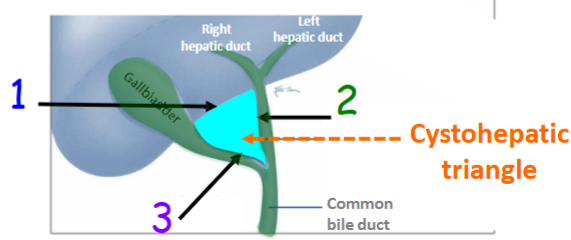
Important surgical danger area in a Cholecystectomy
Important to identify the the cystohepatic triangle to determine if there is a variation the cystic artery or biliary apparatus
What is done in the cystohepatic triangle to prevent bleeding & release of bile
Once identified, the cystic duct and cystic artery are ligated and divided to prevent bleeding and the release of bile
Cystohepatic Triangle / Triangle of Calot borders
Superior border: Inferior border of the Liver
Medial border: Common hepatic duct
Lateral border: Cystic duct
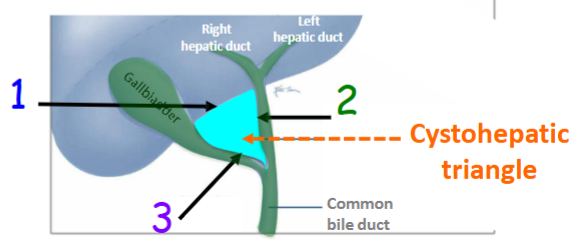
What is regarded as the key component to performing a safe laparoscopic cholecystectomy
Dissection of the cystohepatic triangle
most common type of pancreatic cancer
Cancer of the head of the pancreas
A tumour in the head of the pancreas could obstruct what
Common bile duct
Hepatopancreatic ampulla
A tumour in the neck/body of the pancreas could obstruct what
Hepatic portal vein
Inferior vena cava
Retention of bile pigments (like in pancreatic cancer) will lead to what
jaundice
What is jaundice
Yellowing of the skin and sclera of the eyes usually results if bile is unable to be released into the duodenum
Jaundice can lead to what change in faeces
can lead to stools/faeces becoming acholic
Another name for a whipple procedure & its use
Conventional pancreaticoduodenectomy
surgical treatment for tumours and other diseases of the pancreatic head, duodenum, bile duct, or periampullary region. It involves the removal of:
The head of the pancreas
The duodenum (first part of the small intestine)
The gallbladder
Part of the common bile duct
Sometimes part of the stomach (pylorus-preserving variant spares it)
After removing these structures, the surgeon reconstructs the digestive tract to allow for the continued flow of bile and pancreatic enzymes.
Pyrosis
Heartburn
Pyrosis is the most common type of esophageal discomfort and substernal pain - what does it involve
Typically a result of regurgitation of gastric acid into the abdominal part of the esophagus
What is pyrosis a symptom of (2)
Gastro Esophageal Reflux Disorder (GERD)
Hiatal Hernia
What has the job of preventing acid reflux
inferior esophageal sphincter
2 most common stomach diseases
Gastric ulcers and gastritis
What is a peptic ulcer
A distinct lesion (or necrosis) of the mucosa in either the stomach, pyloric canal or duodenum as a result of acid erosion
Peptic Ulcers symptoms
Haematesmesis: vomiting “coffee ground” blood
Melena: black, foul-smelling faeces
Problem associated with peptic ulcer on lesser curvature of the stomach
Erode GASTRIC artery
Problem associated with peptic ulcer on the anterior wall of the stomach
Erode the LIVER and cause peritonitis
Problem associated with peptic ulcer on the posterior wall of the stomach
Erode SPLENIC a. & the PANCREAS
Majority of gastric cancers are what
adenocarcinomas
Why is surgery on carcinoma of the stomach difficult
Surgery is difficult due to the inability to remove all of the lymphatic nodes associated with the stomach
can help identify small gastric tumors
Transillumination
What is a sign that carcinoma of the stomach is advanced
if Virchow’s lymph nodes (left supraclavicular) are palpable, the malignancy is advanced and prognosis is poor
Troisier’s Sign
Hard, palpable, enlarged LEFT supraclavicular lymph nodes indicate metastatic cancer in the abdomen
Name 2 types of Inflammatory Bowel Disease (IBD)
Crohn’s Disease & Colitis
Difference between Crohn’s Disease & Colitis
Crohn’s disease has very similar symptoms as ulcerative colitis, however, colitis is limited to the colon