Pathology (3rd Year)
1/646
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
647 Terms
What is the largest organ in the body?
Liver
Where does 70-80% of the liver's blood supply come from?
Portal vein
The portal vein makes up 70-80% of the liver's blood supply, what vessel supplies the remaining 20-30%?
Hepatic artery
Bile is secreted from hepatocytes and travels through the hepatic ducts. What duct does the hepatic ducts unify with at the bile ducts?
Cystic duct of gallbladder
Bile entered the duodenum at the level of the ______________
major duodenal papilla
Blood flows towards the ____________, whereas bile flows towards the ______________
central veins, portal triad
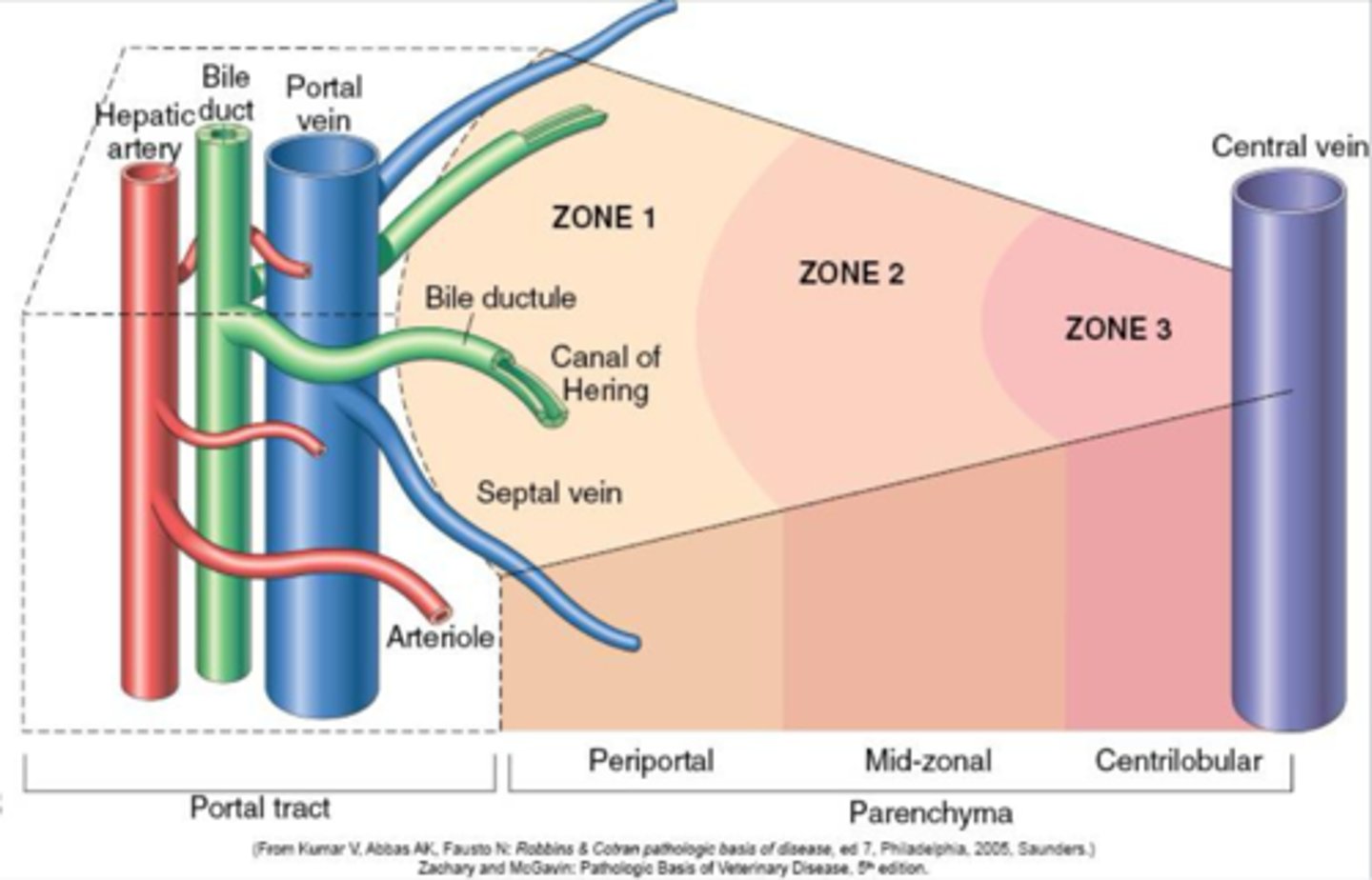
Which zone in the liver parenchyma is most prone to both hypoxic and toxic injury due to cytochrome P450 metabolites?
Zone 3 (centrilobular)
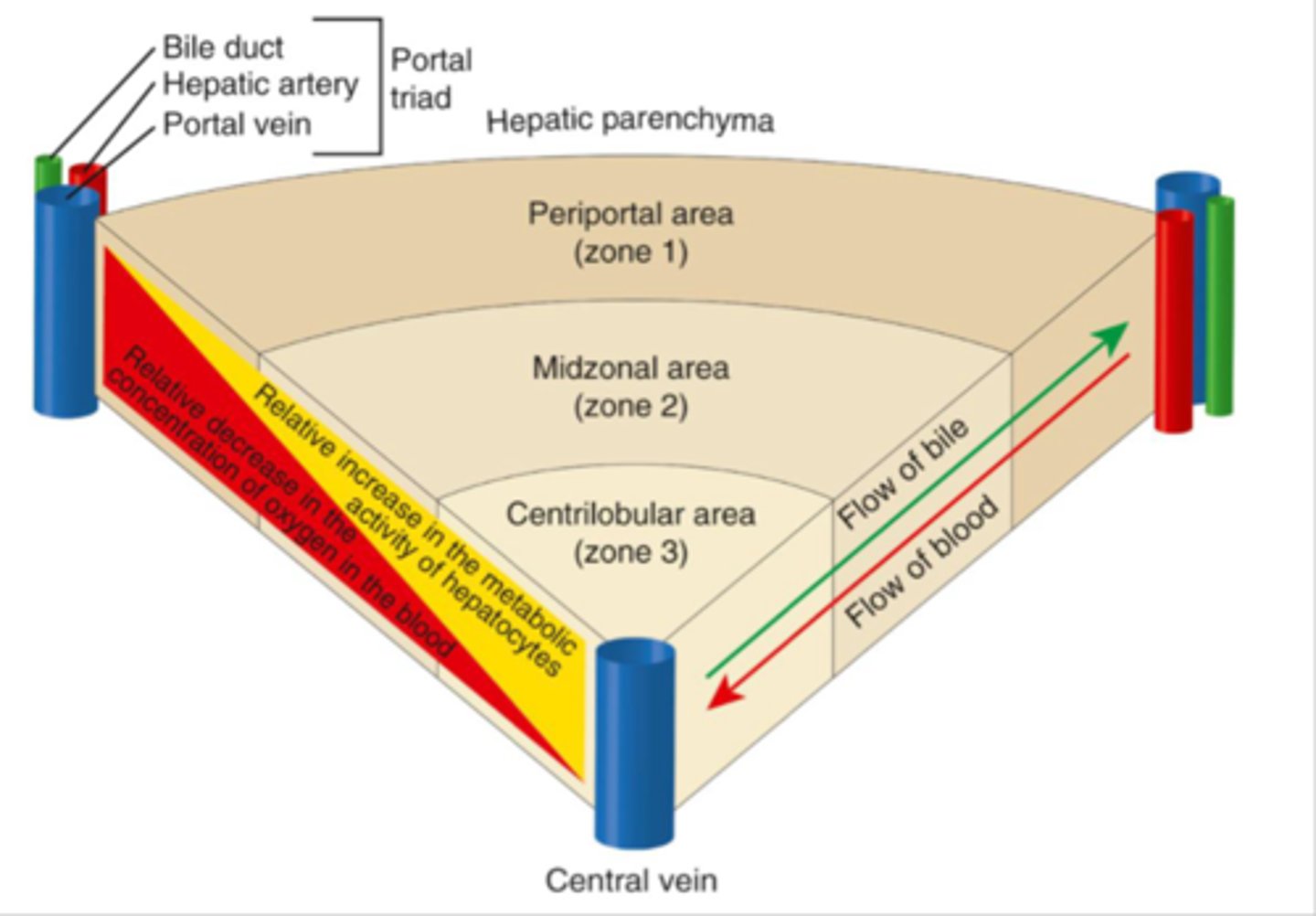
Which hepatic zone has the highest concentration of cytochrome P450?
Zone 3 (centrilobular)
What are the functions of the liver?
Bile production and excretion, bilirubin, carbohydrate, lipid, xenobiotic, and ammonia metabolism, protein synthesis, immunity
Necrosis of zone 3 associated with hypoxia
Centrilobular necrosis
What are the causes of centrilobular necrosis?
Anemia, cardiac dysfunction, toxins, some viral infections (adenovirus 1)
Zone 2 necrosis that can spread to centrilobular areas
Midzonal necrosis
What causes midzonal necrosis?
Some toxins
Uncommon necrosis of zone 1.
Periportal necrosis
What causes periportal necrosis?
Direct acting hepatotoxins that do not require metabolism
Necrosis of zone 1 that indicates ischemic injury
Paracentral necrosis
What causes paracentral necrosis?
Infarcts, thrombosed vessels, DIC
Paracentral necrosis can occur with _____________
anemia
Necrosis of the entire hepatic lobule
Massive necrosis
What can cause massive necrosis in the liver?
Amanita mushroom, blue-green algae, aflatoxin, sago palm, xylitol, vitamin E/selenium deficiency in pigs
What can cause individual cell necrosis?
Immune mediated disease (chronic interface hepatitis), certain toxins, certain infections
Why is the centrilobular region more prone to hepatocelluar injury?
Hypoxia may occur due to distance from portal vein, increased concentration of P450 enzymes which generates a toxic metabolite
What is the mechanisms of hepatocellular lipidosis/steatosis?
Lipid accumulation in response to injury; Too much lipid/triglycerides going in, too much lipid being synthesize and stored, not enough lipid going out
What are some potential causes of hepatic lipidosis?
Excessive dietary intake, starvation, late pregnancy, lactation, hypoxia, mitochondrial damage
Type of fibrosis that occurs in response to massive necrosis or infarcts
Postnecrotic scarring
Type of fibrosis often in response to ongoing hepatic injury, such as, individual cell necrosis, chronic toxicity
Portal fibrosis
Type of fibrosis that occurs in chronic passive venous congestion
Centrilobular fibrosis
What are some potential causes of centrilobular fibrosis?
Right heart failure, chronic hypoxia injury, certain toxins
Fibrosis that occurs with chronic extra hepatic biliary obstruction
Biliary/peribiliary fibrosis
What are some causes of biliary fibrosis?
Chronic biliary tract infections, GB mucocele, neoplasia in biliary tract
Diffuse process characterized by fibrosis and the conversion of normal liver architecture into structurally abnormal nodules
Cirrhosis
What are the features of cirrhosis?
Bridging fibrosis, formation of regenerative nodules

Most domestic species do not develop cirrhosis with chronic hepatic injury, what is the exception?
Dogs with chronic hepatitis
Both fibrosis and cirrhosis can lead to __________
Acquired portosystemic shunting
Which region of the hepatic lobule has the least amount of oxygen?
Centrilobular
Which pattern of hepatic necrosis would you associate with anemia?
Centrilobular necrosis
What are the sequela of hepatic dysfunction?
Cholestasis, icterus, hemorrhage, ascites and edema, hepatic encephalopathy, hepatocutaneous syndrome, hepatorenal syndrome, photosensitization
What type of cholestasis occurs due impaired uptake, metabolism, secretion, or transport of bile components
Hepatocellular cholestasis
What type of cholestasis occurs due to bile flow obstruction of major bile ducts or gall bladder?
Obstructive cholestasis
Icterus/jaundice occurs due to excess ____________ in plasma
bile pigments (bilirubin)
What type of icterus occurs due to hemolytic anemia causing a large release of bilirubin accumulating in the liver and overwhelming the system > Unconjugated bilirubinemia
Pre-hepatic
What type of icterus occurs do to hepatic dysfunction and an inability to adequately conjugate bilirubin?
Hepatic
What type of icterus occurs due to an obstruction of the biliary drainage system?
Post-hepatic
Why does hemorrhage occur in hepatic dysfunction?
Clotting factor consumption (acute liver necrosis), reduced synthesis of clotting factors (chronic liver disease)
Why does ascites and edema occur in hepatic dysfunction?
Decreased synthesis of albumin leading to a low Oncotic pressure, altered blood flow through the liver
Why does hepatic encephalopathy occur in liver dysfunction?
Ammonia not converted to urea, ammonia crosses BBB and accumulates in the brain
What kind of dermatitis occurs with hepatic dysfunction?
Superficial Necrolytic dermatitis
What is the pathogenesis of hepatorenal syndrome as sequela to hepatic dysfunction?
Splanchnic vasodilation leading to decreased venous return and CO, Compensatory renal arterial vasoconstriction which decreased GFR
What are the hepatocellular leakage enzymes that elevate due to hepatic necrosis or sublethal injury?
AST, ALT (SDH, LDH, GDH)
What are the induced hepatic enzymes that increase due to activity associated with cholestasis, drugs, or hormones?
ALP, GGT
Breakdown product of hemoglobin and myoglobin. Conjugated in the liver and excreted via bile. Elevates in liver disease
Bilirubin
Secreted in the bile to help solubilize lipids and aid in fat digestion, Brought back to portal circulation and recycled. Elevated in liver disease.
Bile acids
From protein/AA breakdown in GI. Converted to urea in the liver. Will elevate if liver is not functioning properly since it cannot be converted.
Ammonia
Besides, enzymes, bilirubin, bile acids, and ammonia, what are some other biochemical markers of liver disease?
Albumin, glucose, cholesterol, BUN
What type of icterus would you expect in an animal with hemolytic anemia?
Pre-hepatic
Excess of which compound causes hepatic encephalopathy?
Ammonia
What breeds are predisposed to congenital extrahepatic portosystemic shunts?
Mainly small breed dogs, yorkies (can affect cats too)
What breeds are predisposed to congenital intrahepatic shunts? (Porto-azygous shunt, Porto-caval shunt)
Mainly large breed dogs
What are the consequences of congenital portosystemic shunting? (PDA)
Portal blood supply is diverted away from liver, hepatotrophc factors, nutrients, and blood supply do not get to liver, bile acids not recycles, ammonia bypasses liver
What gross features would you find with portosystemic shunting?
Hypoplastic liver, smooth, normal color
What histo features would you find with portosystemic shunting?
Centrilobular atrophy, portal vein hypoplasia, portal arteriolar hyperplasia, closer apposition of portal triads to central veins, smaller hepatocytes
What breeds are predisposed to primary hypoplasia of the portal vein (microvascular dysplasia)?
Yorkies, cairn terriers
T/F: Primary hypoplasia of the portal vein can involve intrahepatic or extrahepatic portal veins
T
Why does primary hypoplasia of the portal vein present very similar to congenital portosystemic shunting?
Decreased portal venous perfusion to liver
Animals with primary hypoplasia of the portal vein will develop portal _________. This disease can occur concurrently with ___________________
hypertension, congenital PSS
Will a dog with congenital PSS or a dog with primary hypoplasia of the portal vein have ascites?
Primary hypoplasia of the portal vein
What are some chemistry features of impaired portal venous blood flow?
Low albumin, TP, BUN, glucose, cholesterol, High bile acids, ammonia. ALP and ALT may be mildly elevated
What are some hematology findings with impaired portal venous blood flow?
Low MCV, microcytic anemia
What are some urinalysis findings with impaired portal venous blood flow?
Ammonium bifurcate crystalluria, bilirubinuria
What are some clinical signs of portal venous blood shunting?
Failure to thrive, depression, lethargy, neuro signs (elevated ammonia, hepatic encephalopathy)
Ductal plate malformations are persistent remodeling of embryonic ductal plate which can give rise to a variety of cystic biliary disease, what is this referred to?
Congenital hepatic fibrocystic disease
Blood pressure in hepatic veins increases relative to portal veins
Passive congestion
What is the general cause of passive congestion in the liver?
Cardiac dysfunction (right sided heart failure)
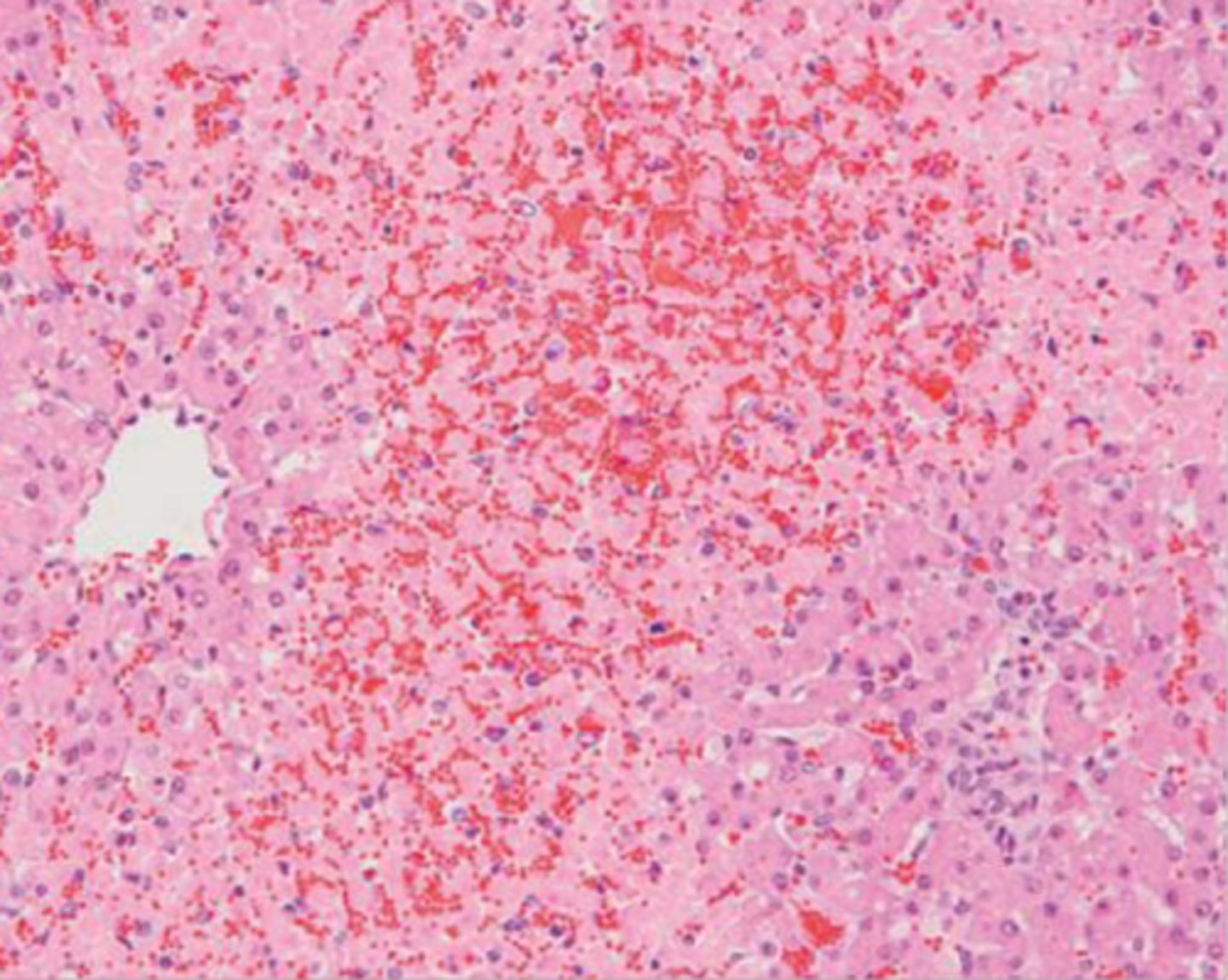
What causes acute passive congestion in the liver?
Sudden cardiac decompensation, shock
What gross findings would you see with ACUTE passive congestion?
Mildly enlarged dark red liver, bleeds on cut section, enhanced lobular pattern
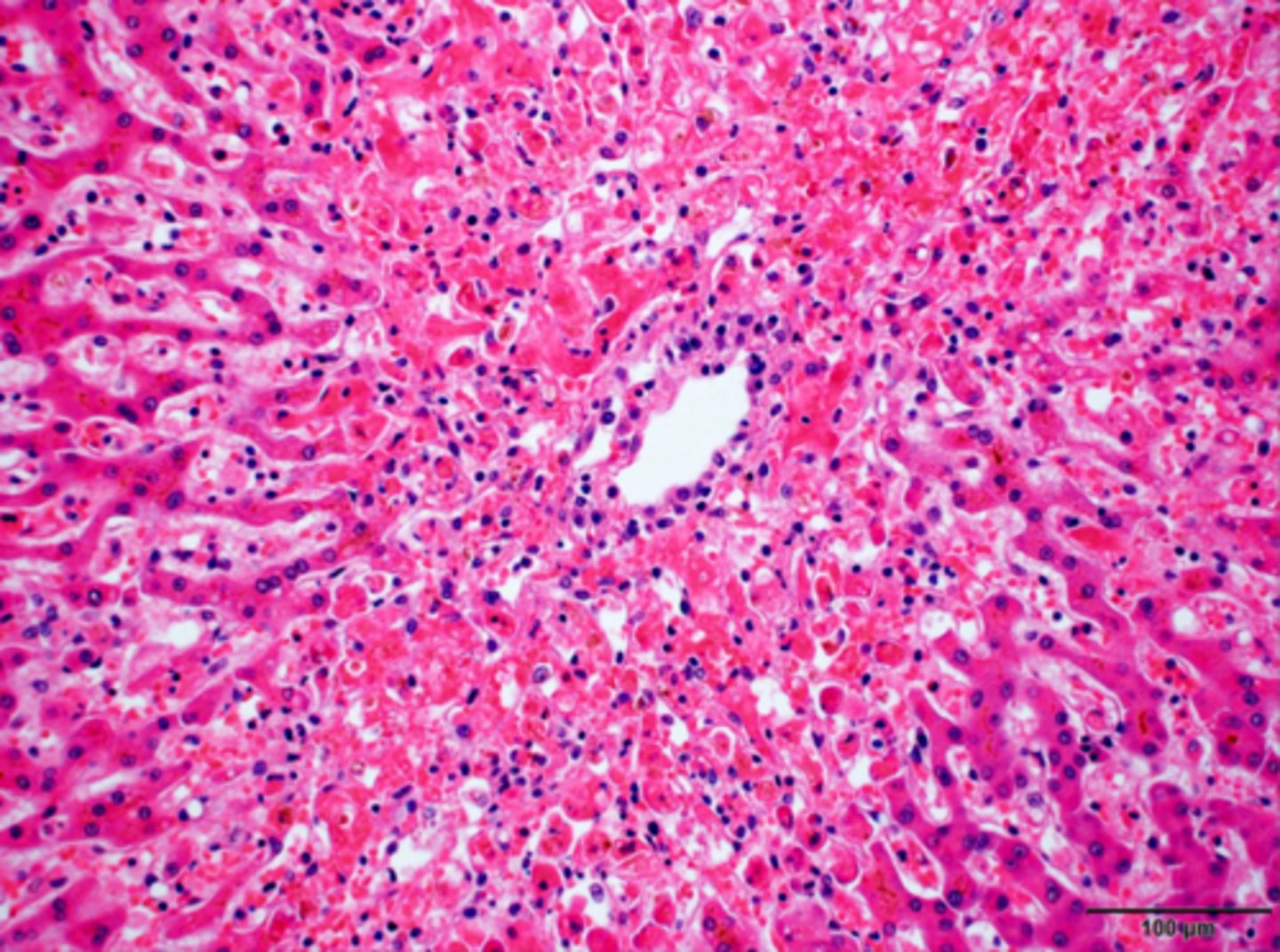
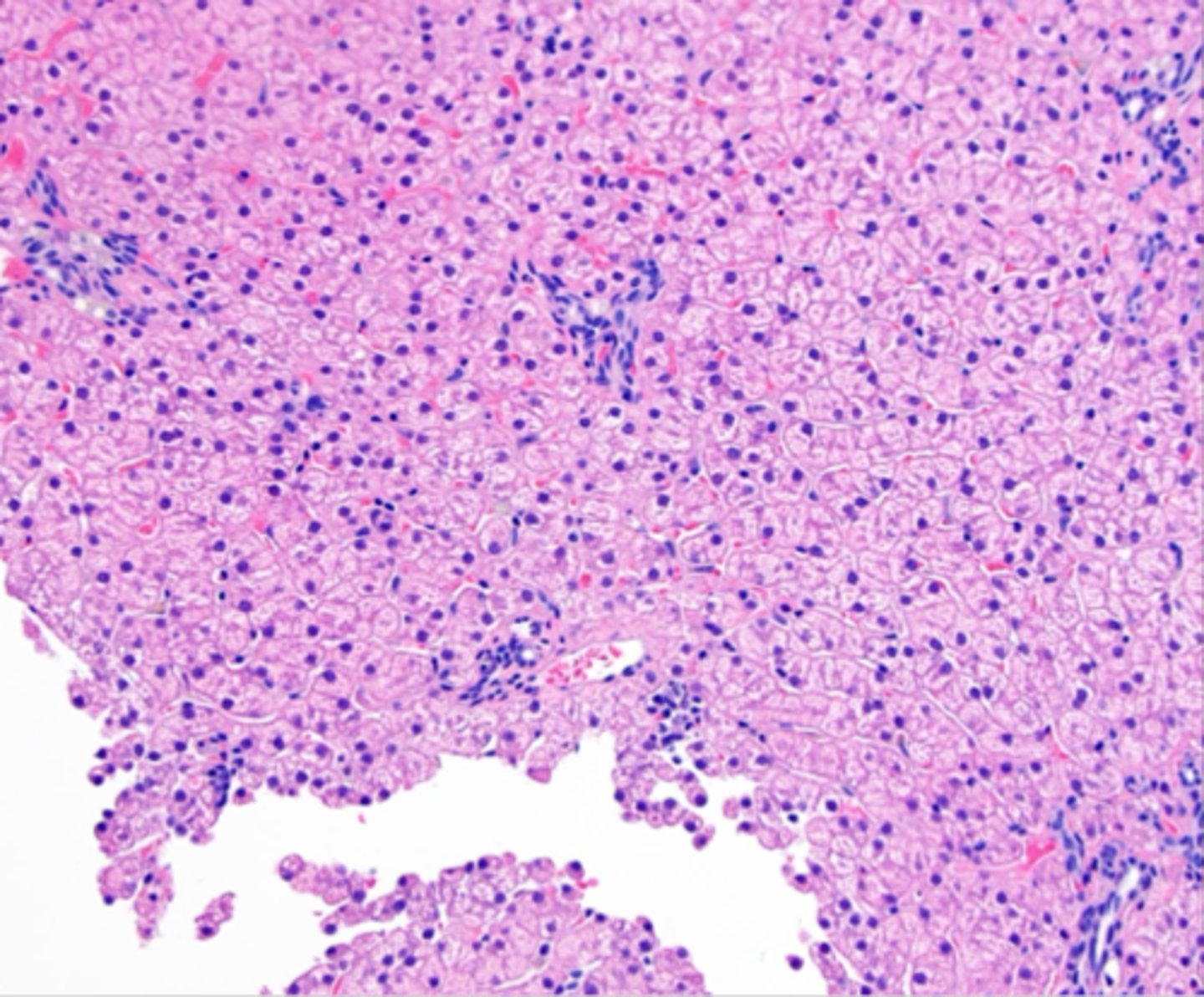
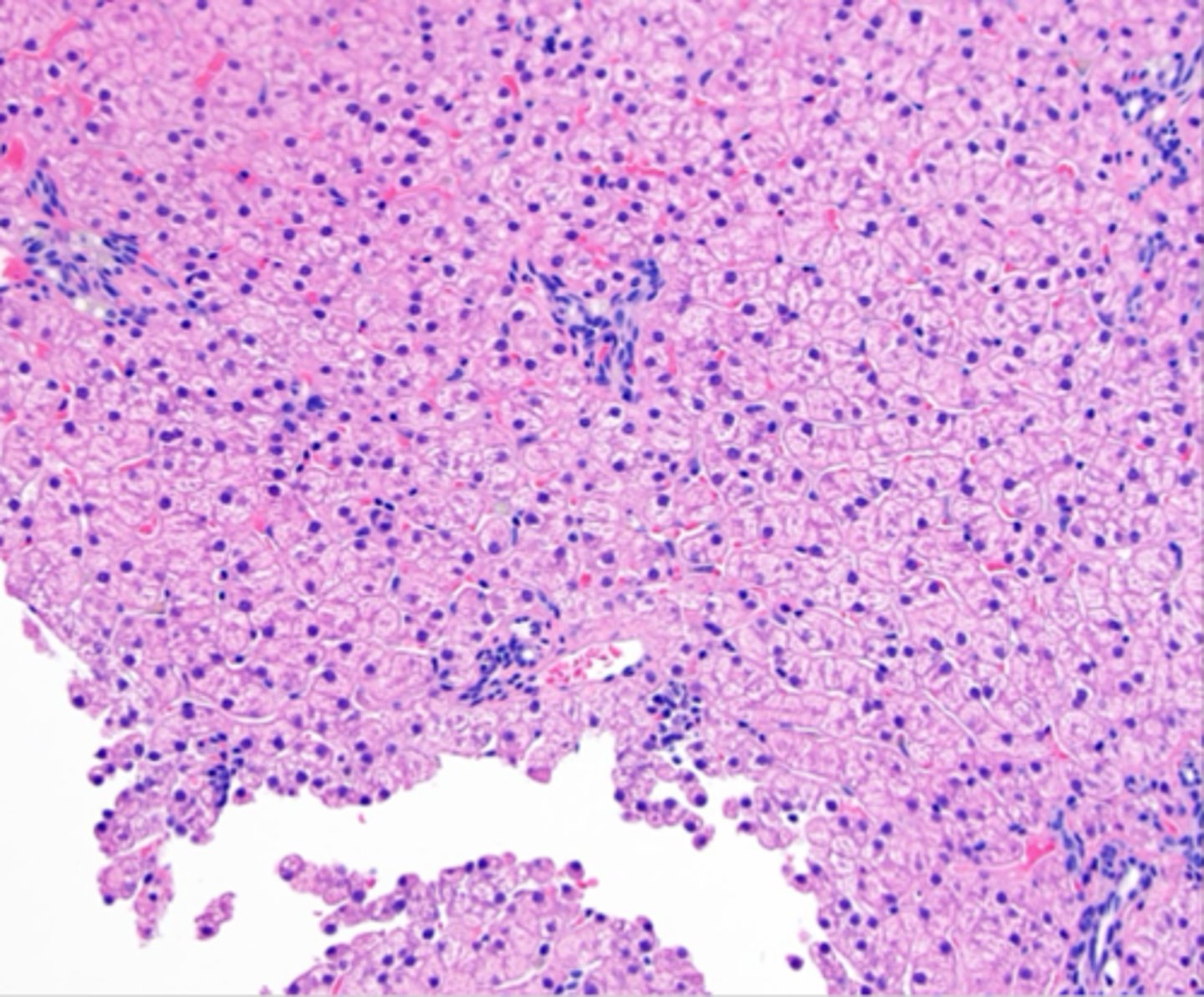
What Histopathologic findings would you see with ACUTE passive congestion in the liver?
Distention of central vein and sinusoids, progression to hepatic steatosis to atrophy to centrilobular necrosis with hemorrhage
What is the classic cause of CHRONIC passive congestion in the liver?
Chronic heart failure (right sided usually)
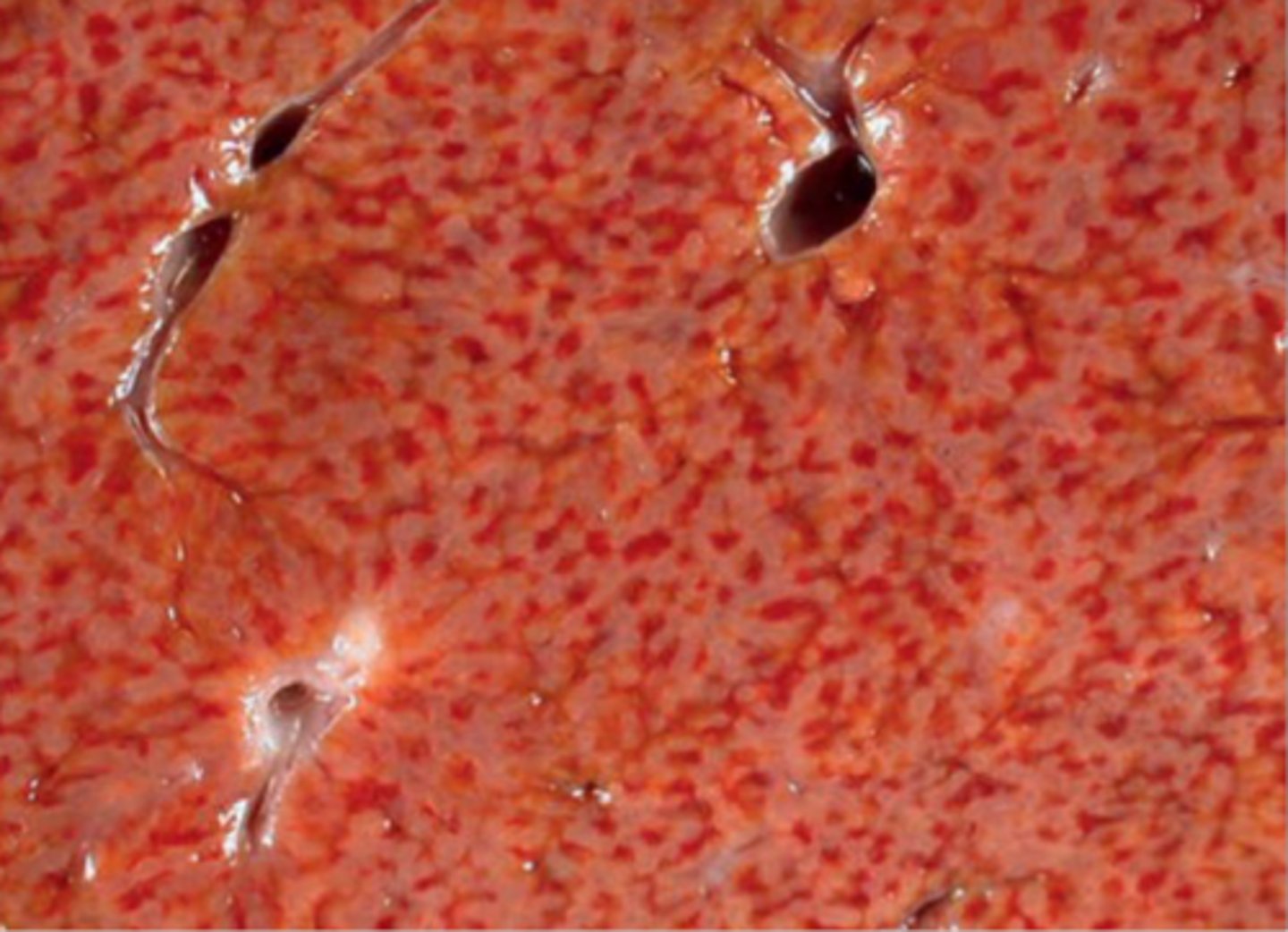
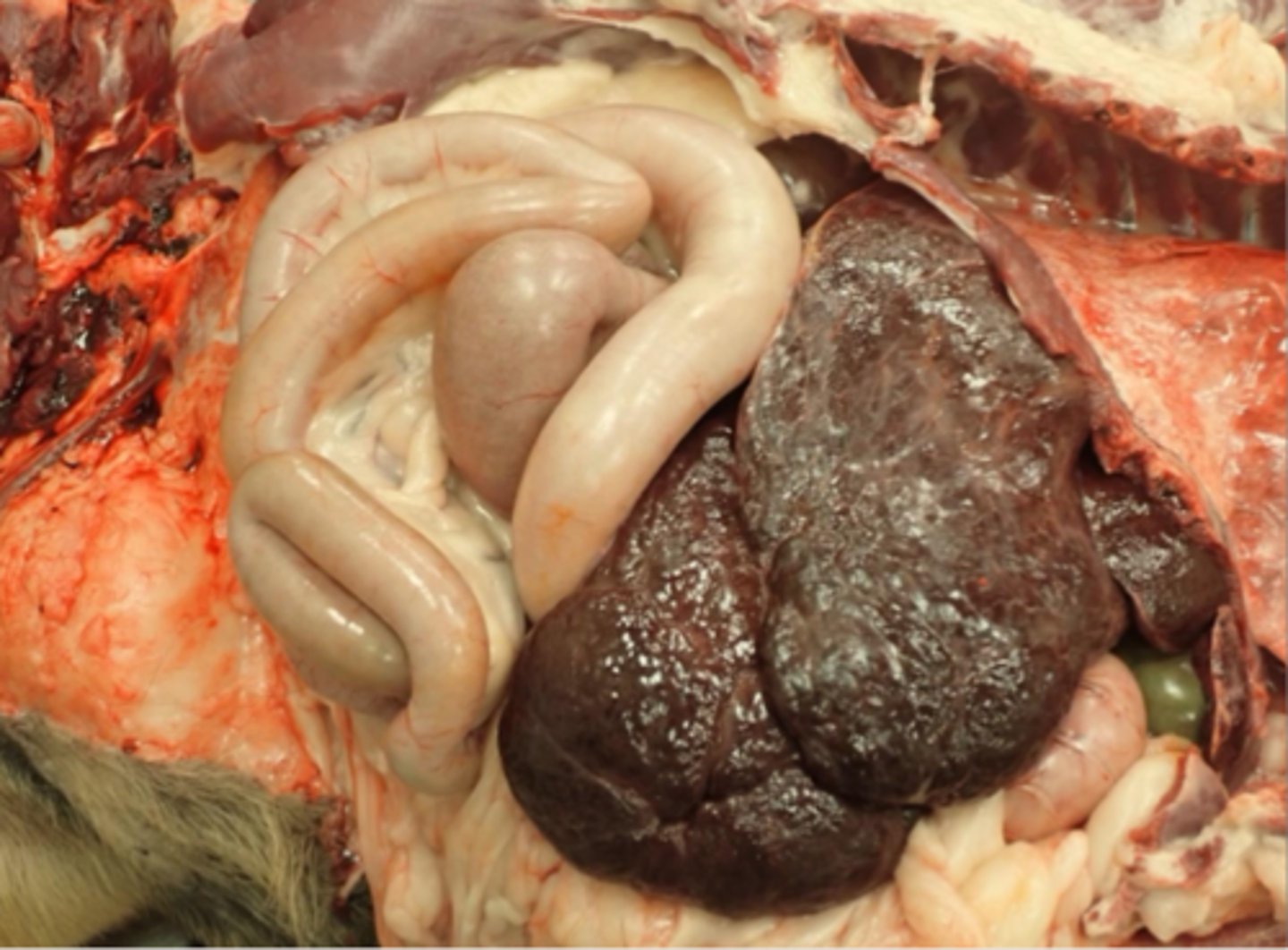
What gross findings would you see in an animal with CHRONIC passive congestion in the liver?
Nutmeg liver (red centrilobular areas with pale surrounding areas), rounded margins of central lobes, capsular fibrosis
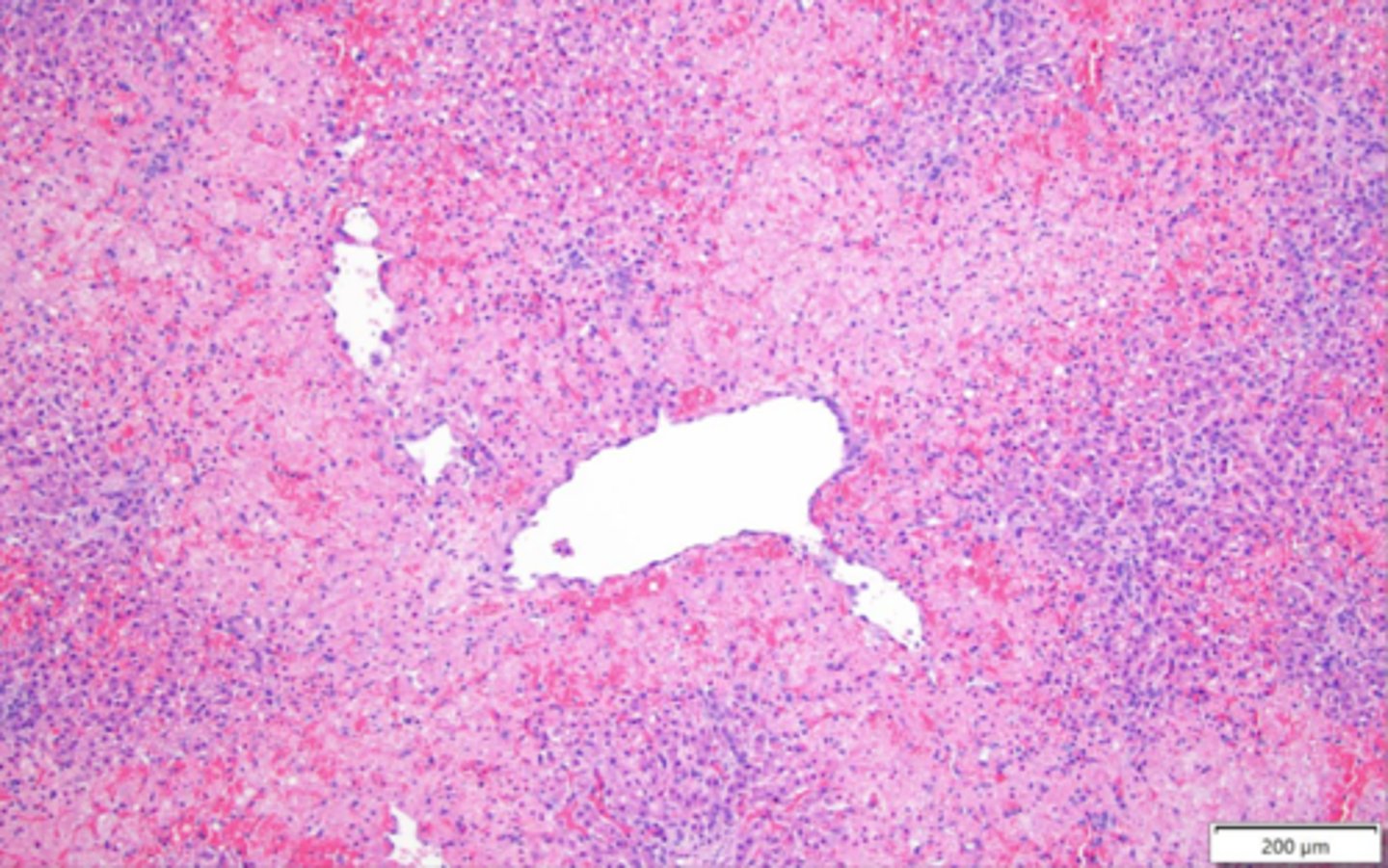
What histopathologic findings would you see in an animal with CHRONIC passive congestion in the liver?
Centrilobular fibrosis, hemosiderin laden macrophages around fibrotic central vein
What is the pathogenesis of dirofilaria immitis causing hepatic passive congestion?
Adult heartworms living in pulmonary vessels causing endarteritis (inflammation of artery wall lining), right heart failure
High dirofilaria immitis worm burden (>100) results in worms filing right atrium and vena cava
Vena Caval syndrome
What does vena caval syndrome result in?
vena cava obstruction, severe hepatic congestion, acute liver failure, hemolytic anemia
A 1 year old yorkie presents for intermittent seizures and is small for its age. Histopath shows portal vein collapse and lobular atrophy. What biochemistry patterns would you likely see?
Normal ALT, ALP, low BUN, BG, albumin, increased bile acids
A 1 year old yorkie presents for intermittent seizures and is small for its age. Histopath shows portal vein collapse and lobular atrophy. On biochemistry, you see normal ALT, ALP, low BUN, BG, albumin and increased bile acids. What's the most likely cause?
Primary portal vein hypoplasia
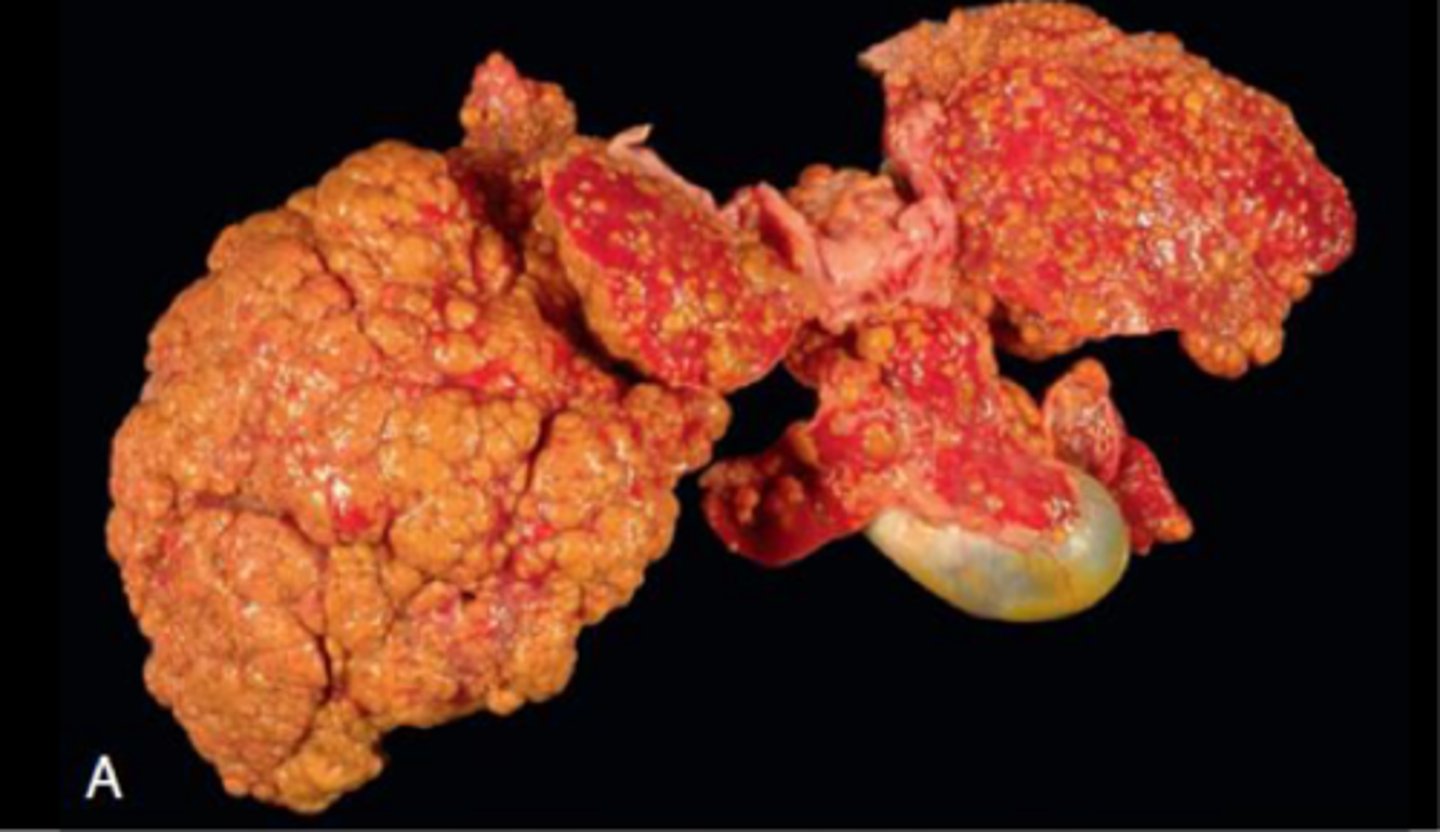
An 8 year old Dottie presents for an enlarged spleen and liver masses. What would be your diagnosis? The liver is rough diffusely but there are no nodules.
hepatocellular carcinoma
Granulomatous hepatitis
Chronic passive congestion
Cirrhosis
Chronic passive congestion
Inflammation along the portal interface. Also called chronic activity hepatitis. Primarily seen in dogs.
Chronic interface hepatitis
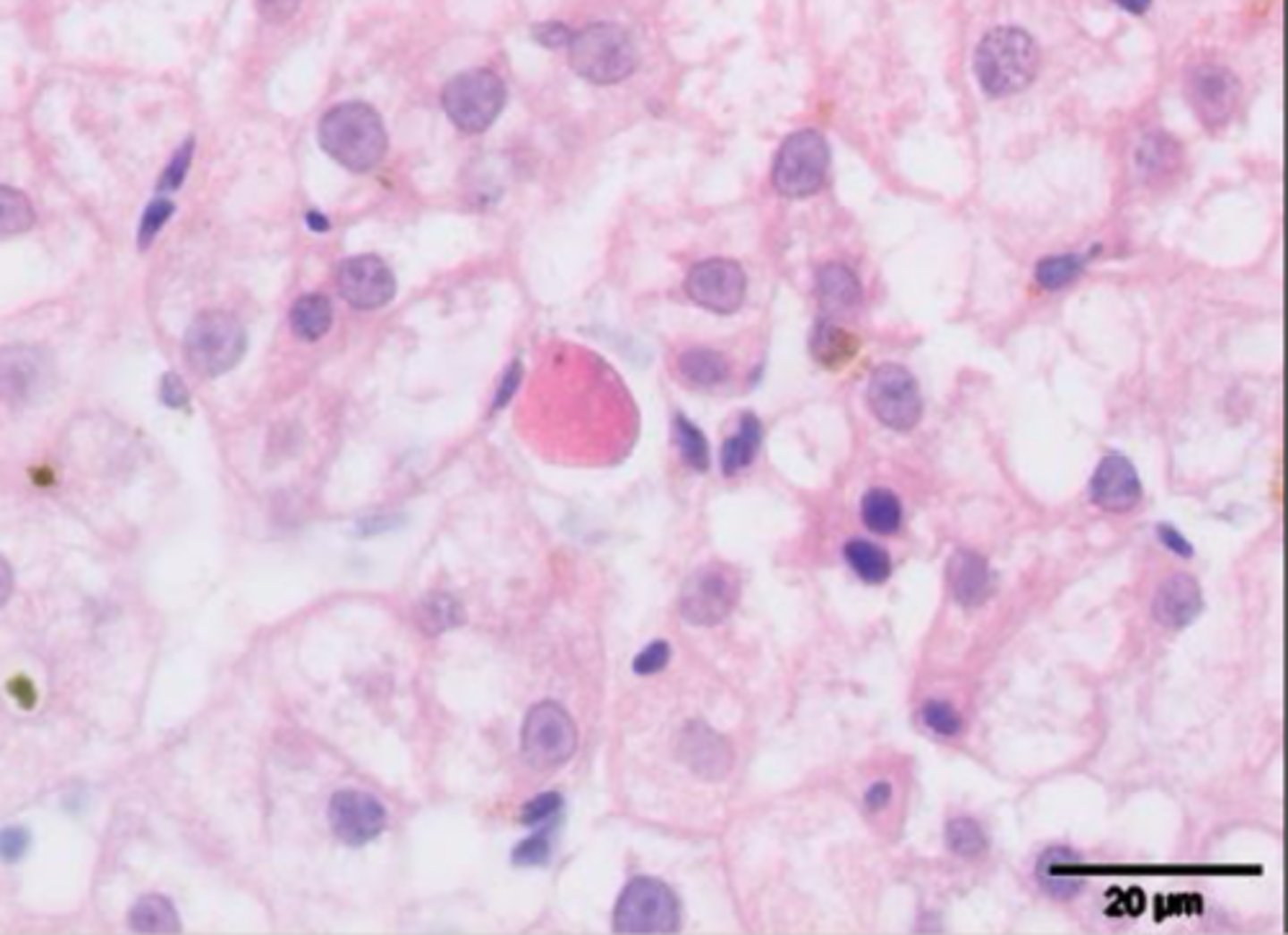
What are the histologic features of chronic interface hepatitis in dogs?
Inflammation along portal interface, lymphocytes, plasma cells, neutrophils, individual hepatocytes necrosis, fibrosis, biliary hyperplasia (may progress to cirrhosis)
What breeds are predisposed to chronic interface hepatitis?
Bedlington terriers, westies, dobies, Skye terriers, labs, Dalmatians, spaniels
What are some possible etiologies of chronic interface hepatitis in dogs?
Unknown, associated with copper. maybe viruses, toxin/drug reactions, immune-mediated, autoimmune, familial/genetic component
Majority of canine chronic hepatitis in dogs are __________
idiopathic
Chronic interface hepatitis is likely to be associated with _______
copper
What is the role of copper in chronic hepatitis?
Liver is central to copper hemostasis and is regulated via biliary excretion
How can copper accumulate in chronic hepatitis?
Primary metabolic defect in metabolism, secondary to abnormal hepatic function and altered biliary copper excretion, excess dietary intake
Where does copper accumulate in the liver?
Centrilobular areas (with genetic storage disorder or excess dietary intake), periportal areas (impaired hepatic function)
What genetic component is associated with copper and chronic hepatitis?
In bedlington terriers, there is an autosomal recessive mutation in the COMMD1 gene (causes copper-associated hepatopathy with impaired biliary copper excretion and progressive copper accumulation)
Evidence suggests primary accumulation plays a role for chronic hepatitis in the following breeds:
Dobies, westies, labs, Skye terriers, dalmations
Unique form of chronic hepatitis that affects juvenile to young dogs. Has a rapid clinical progression
Lobular dissecting hepatitis
Chronic hepatitis in cats is ___________. Cases have been associated with excessive ________ accumulation. Can lead to __________
uncommon, copper, cirrhosis
Chronic hepatitis in cats with an unknown etiology but suspected to be an immune-mediated disease. Also referred to as lymphocytic cholangiohepatitis
Lymphocytic cholangitis
Lymphocytic cholangitis in cats can be difficult to distinguish from _________
lymphoma