Pulmonary Physiology: Mechanics of Breathing
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
What factors contribute to the collapsing tendency of the lungs?
-elastic fibers in the lung CT (1/3)
-alveolar surface tension (2/3)
What creates the surface tension in the alveoli?
surface tension results from electrostatic forces btwn water molecules lining the alveolar walls ==> directed towards the center & creates a pressure in its interior
*This force is inversely proportional to the square of the distance bwtn them
The pressure created by the surface tension in alveoli is a function of?
-surface tension of the fluid
-radius of sphere
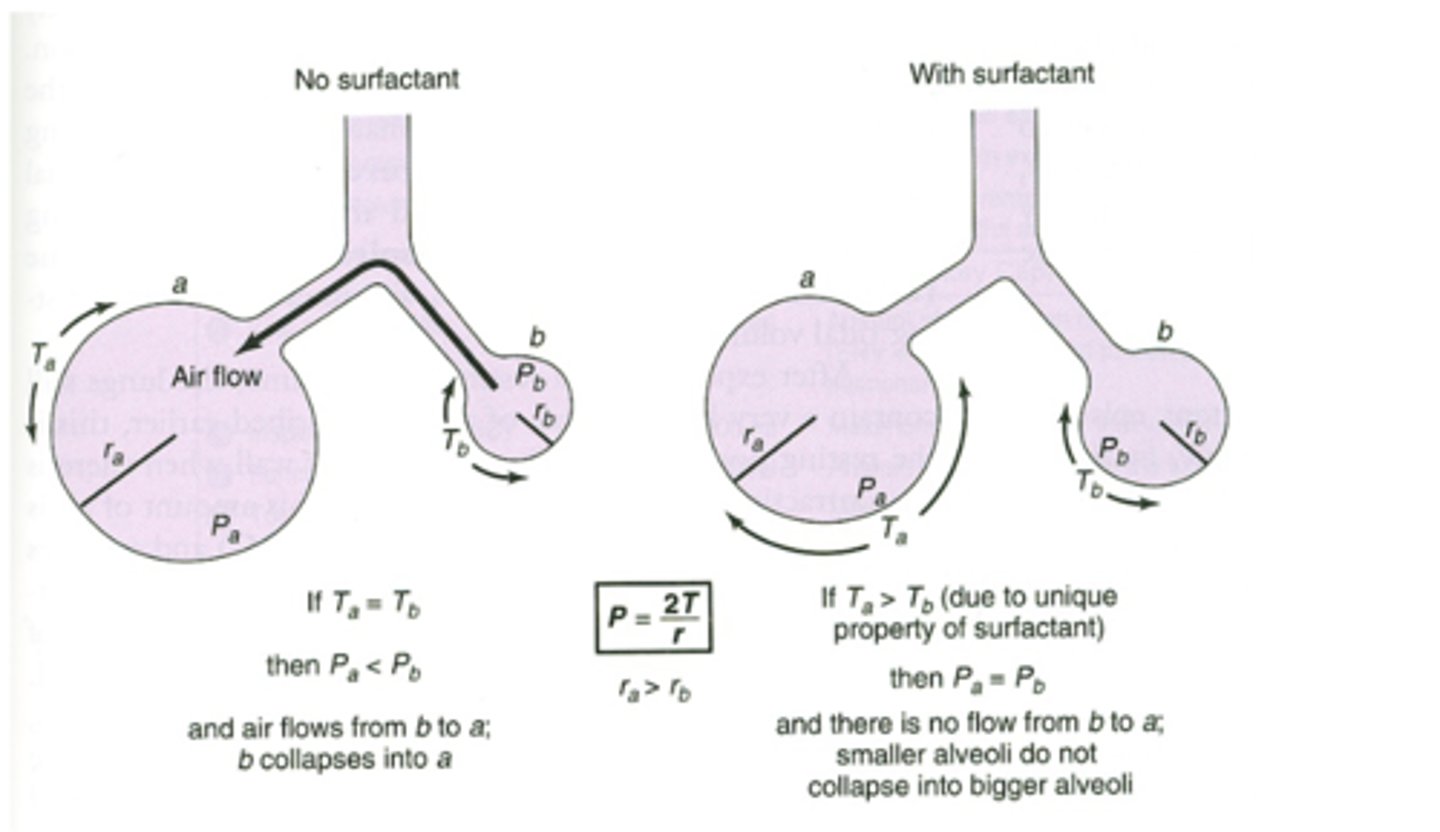
If two bubbles have the same surface tension, which bubble will have the higher pressure?
the smaller bubble ==> according to Law of LaPlace (P= 2T/r)
True or False: As a alveolus gets smaller, more pressure is required to prevent it from collapsing or to subsequently expand it
True
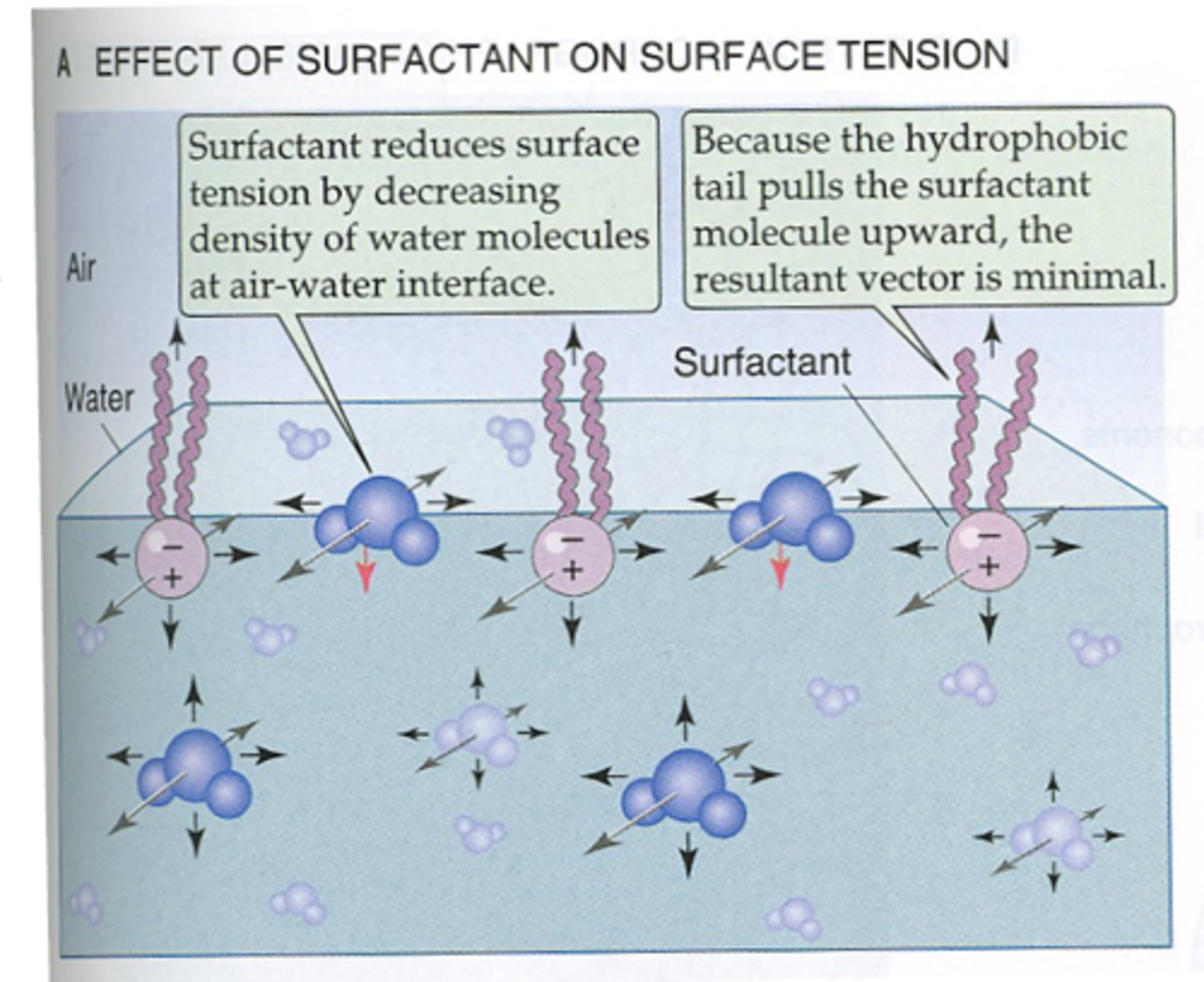
What's the purpose of surfactant in alveoli?
surfactant decreases water-water interactions to lower surface tension ==> prevents alveoli from collapsing due to surface tension (esp the smaller ones)
*If surface tension is constant smaller alveoli will have a tendency to collapse into larger ones==> surfactant allows the surface tension to vary with the radius (equalizes the surface tension in both alveoli to prevent collapse)
what is surfactant?
mixture of lipids and proteins that's secreted by type II alveolar epithelial cells
*major component = detergent dipalmitoylphosphatidylcholine
which cells in the alveoli secrete surfactant?
type II alveolar epithelial cells
What is the major component of surfactant?
detergent dipalmitoylphosphatidylcholine
Why does surfactant create a minimal vector within the lining of the alveoli?
b/c the tail pulling it upward is hydrophobic
What prevents alveoli from collapsing?
-surfactant --> on lining of alveoli to break up surface tension
-alveolar interdependence --> alveoli tethered together by collagen fibers in interstitium that makes neighboring alveoli hold each other open
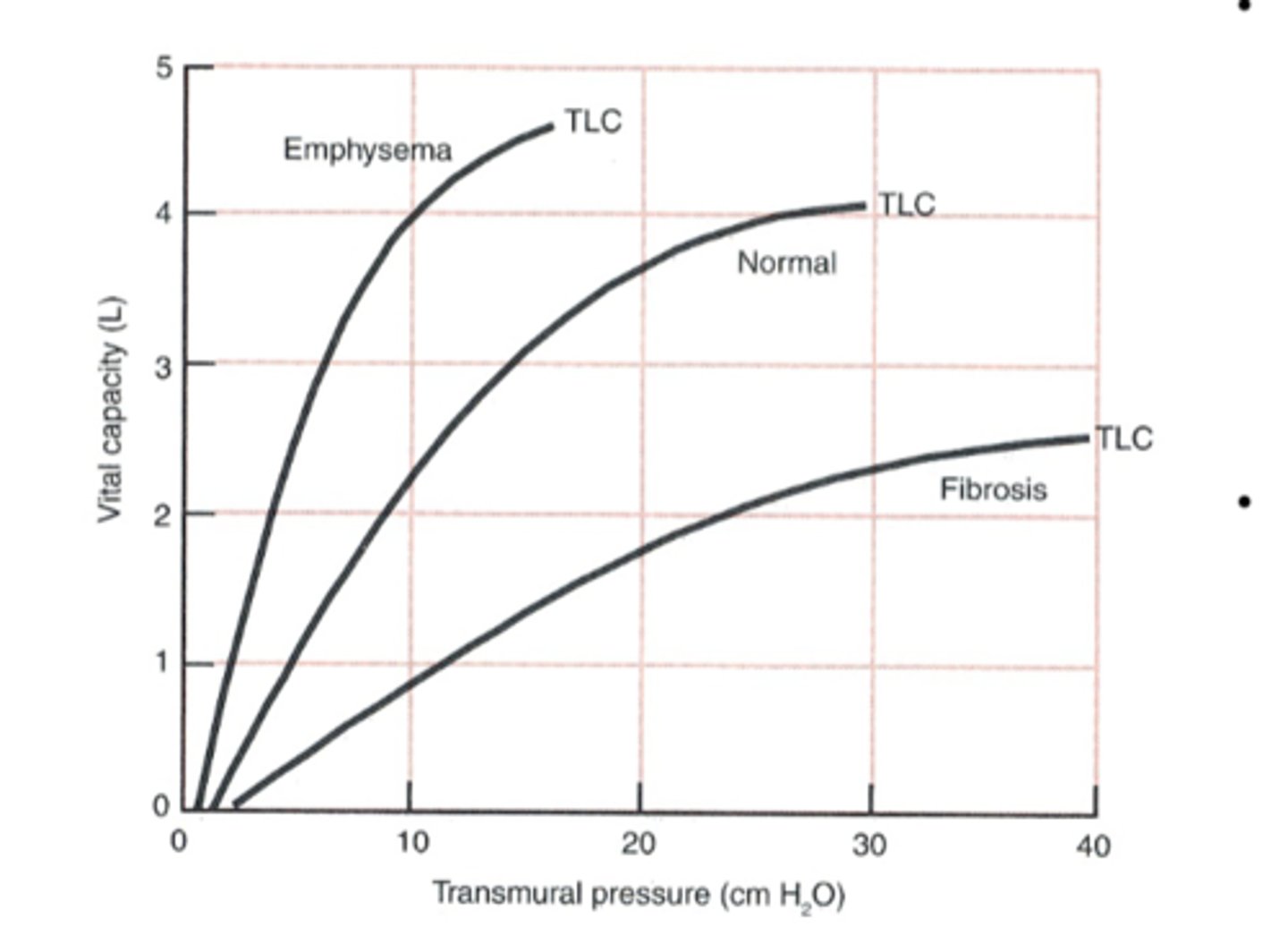
What describes the change in volume as transmural pressure is changed?
compliance
What effect does increasing volume have on compliance?
compliance decreases ==> walls approach maximum stretch
Why isn't the compliance curve of the lungs linear?
b/c it reflects the changing elastic recoil properties of he lung as a function of volume
*lungs distend easily at lower lung volumes but become increasingly stiff at higher volumes as collagen fibers resist further change
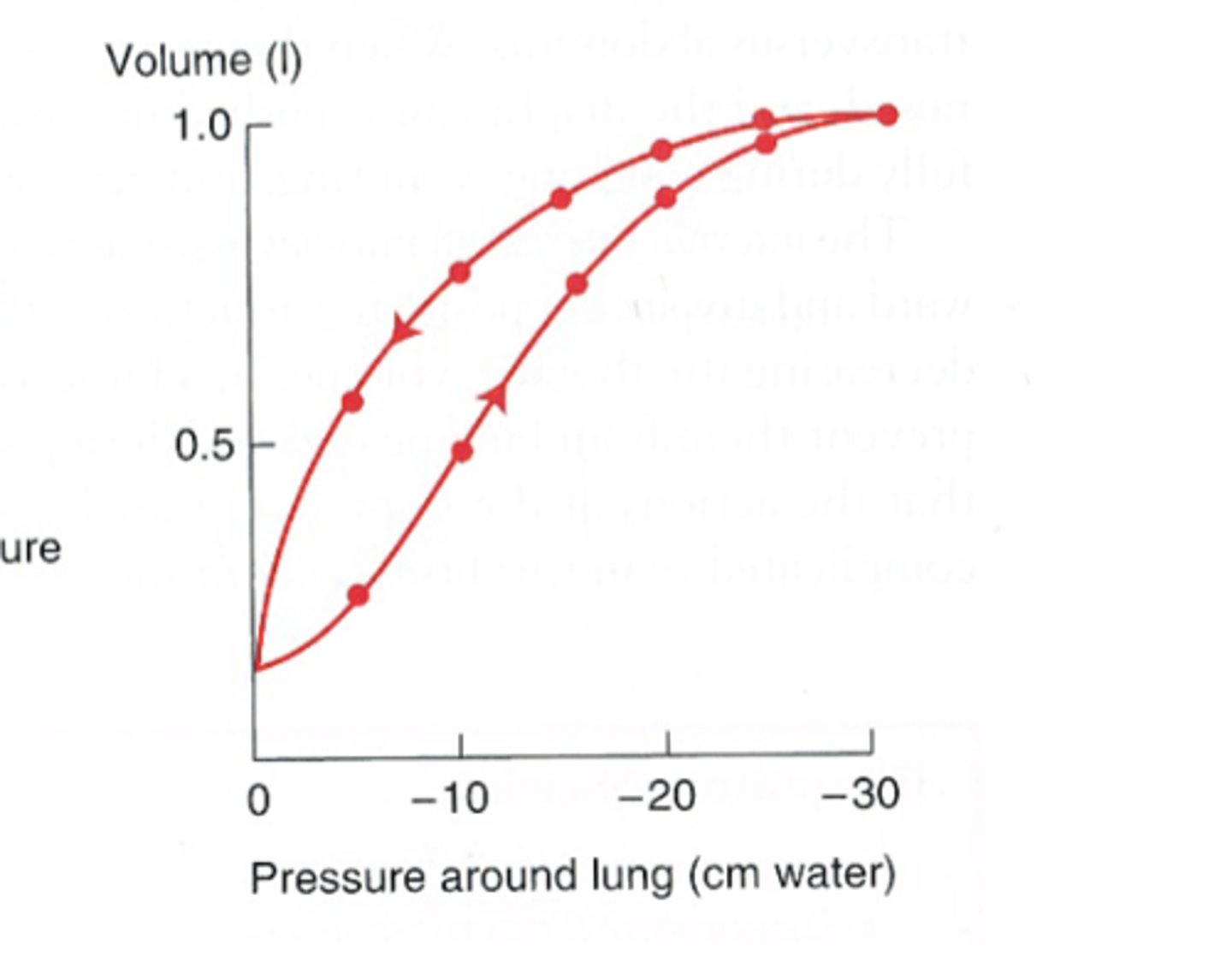
True or False: The compliance curve for lung inflation is the same as the compliance curve from lung deflation
False ==> inflation curve differs from the deflation curve = hysteresis
hysteresis
phenomenon that describes the complaince curve of the lung for inflation differs from the complaince curve of the lung for deflation
What is the compliance at low lung volumes? Why?
low compliance due to high alveolar surface tension (Law of LaPlace)
Describe the compliance of the lung during inflation.
-very low lung volume --> low compliance due to high alveolar surface tension (law of LaPlace)
-when alveoli begin to expand --> decreased alv surface tension, increased compliance
-expansion reaches total lung capacity--> walls stiffen = decreased compliance (approaches max stretch)
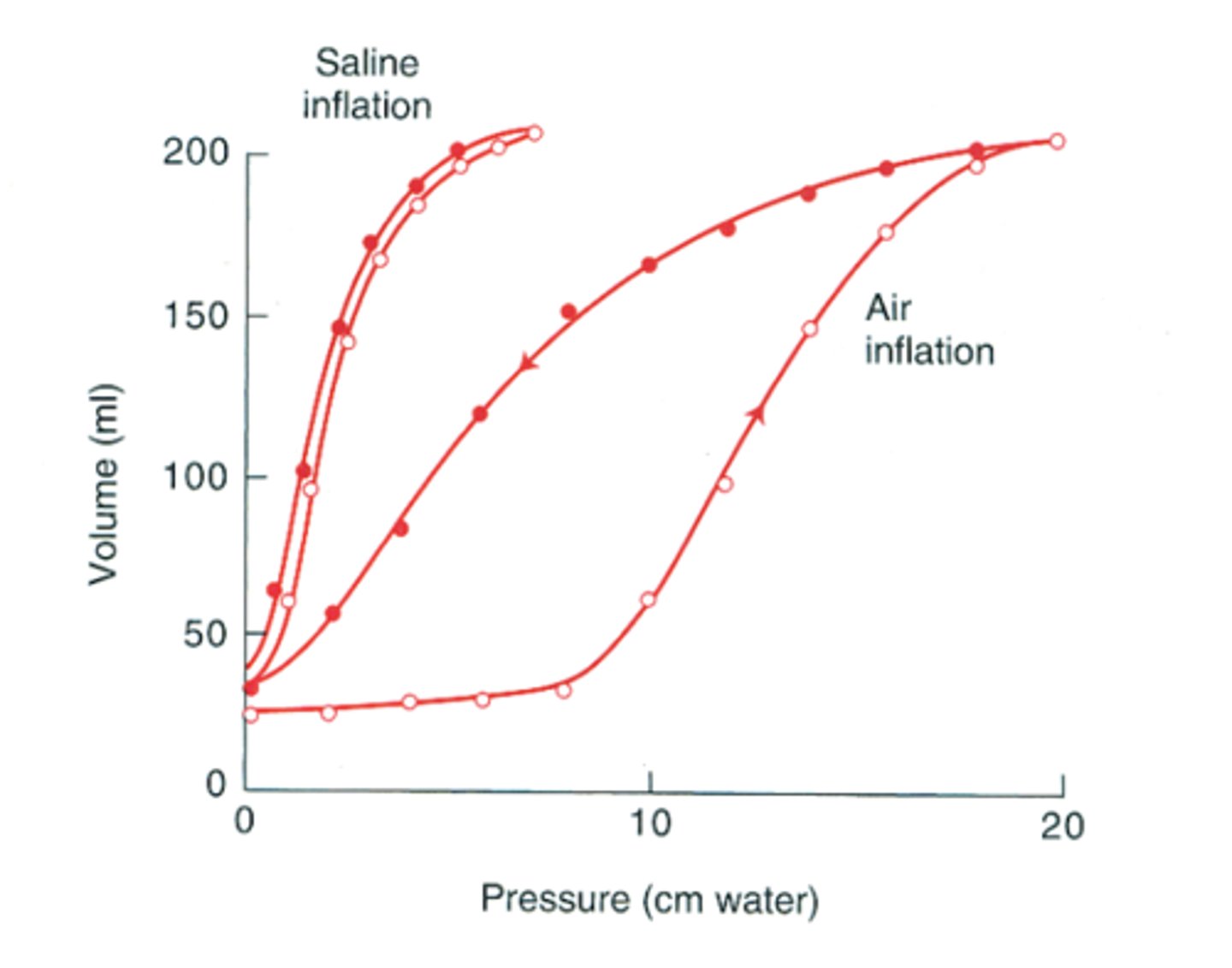
Why doesn't the compliance curve for deflation of the lungs have the same slope as the compliance curve for inflation?
easier to deflate b/c a greater pressure is needed to open a previously closed airway than to keep an open airway from closing
What can be concluded from comparing the compliance of air-filled and saline-filled lungs?
reveals the contribution of alveolar surface tension to the total compliance ==> filling the lungs with saline abolishes the air-water surface tension = increased compliance & decreased hysteresis
How is lung compliance evaluated in vivo?
esophageal balloon is used to determine the intrapleural pressure & measuring lung volume at many points during both inspiration & expiration
How may repeated pulmonary infections affect lung compliance?
can induce fibrosis --> reduces compliance --> increases the work of expanding the lungs
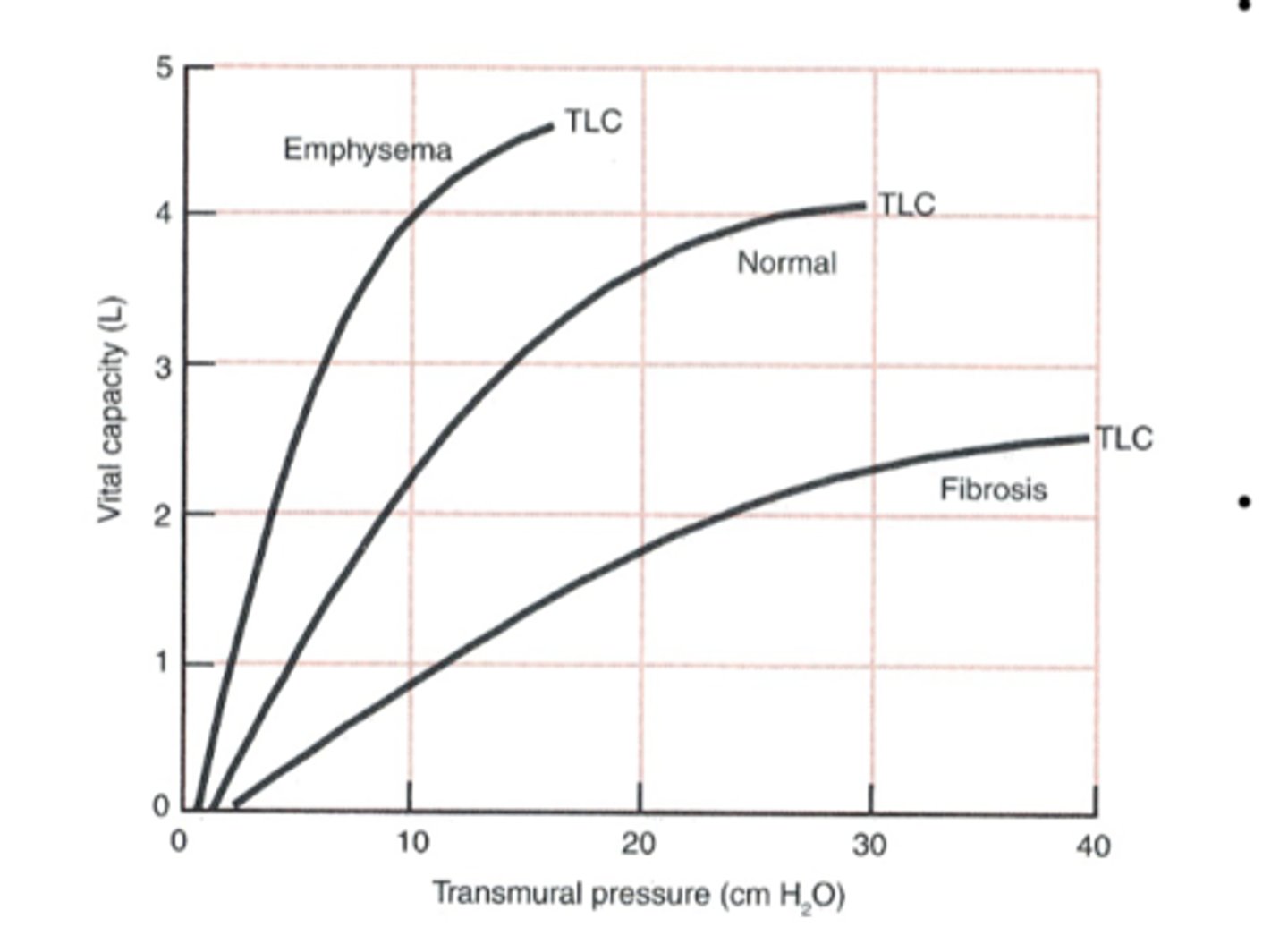
What effect does diseases such as emphysema that destroy lung parenchyma & elastic tissues have on lung compliance?
reduces the recoil tendency of the lung = increased compliance
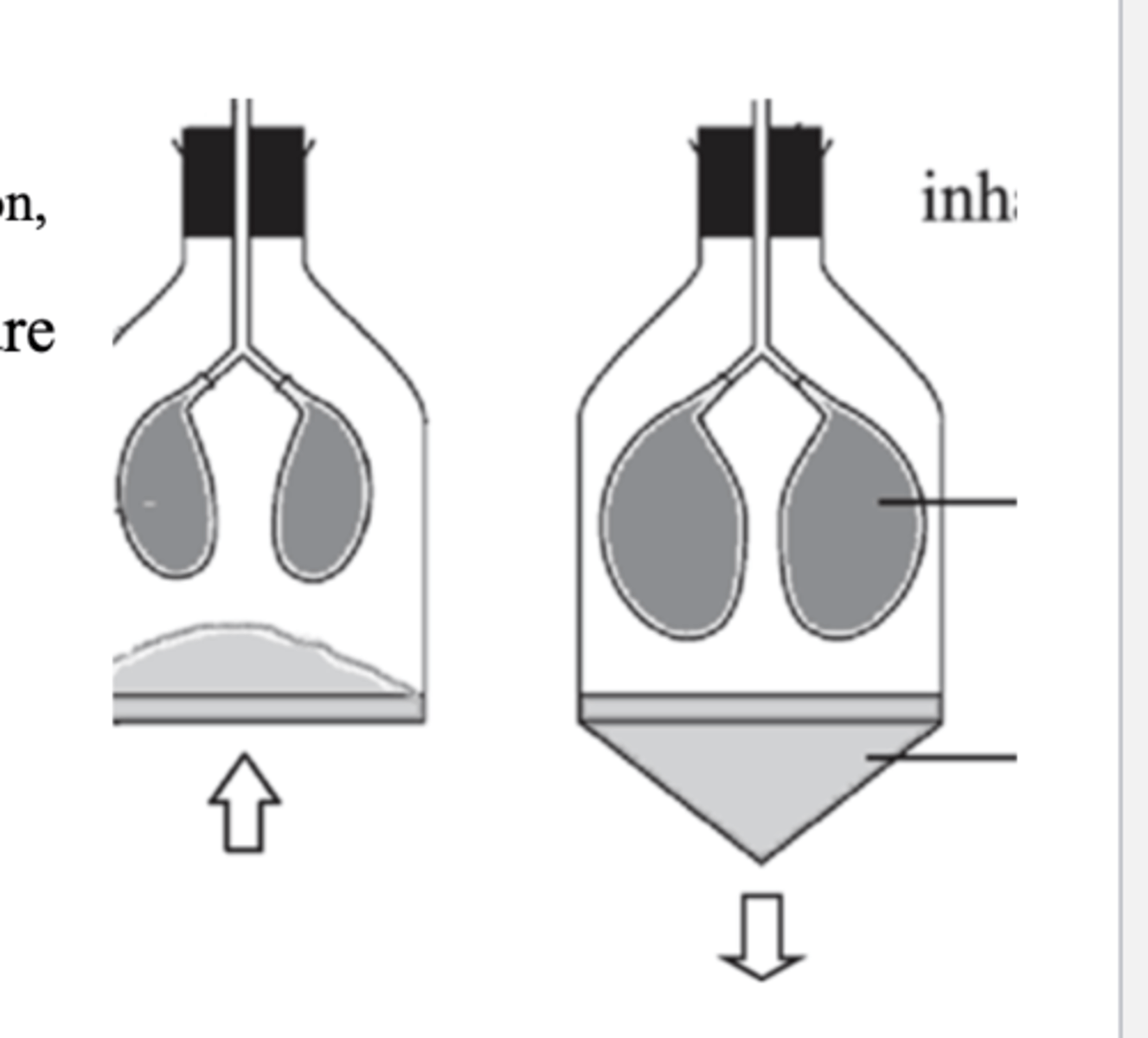
What are the 2 ways that the lungs can be inflated?
-positive pressure --> blowing it up from pressure applied to the trachea
-negative pressure --> applying negative pressure to the outside surface to suck it gainst the inner chest wall (*normal mechanism)
What is the normal mechanism of lung inflation?
applying negative pressure to the outside surface to suck it gainst the inner chest wall
What keeps the lungs expanded within the thoracic cavity?
**fact check this card after re-watch**
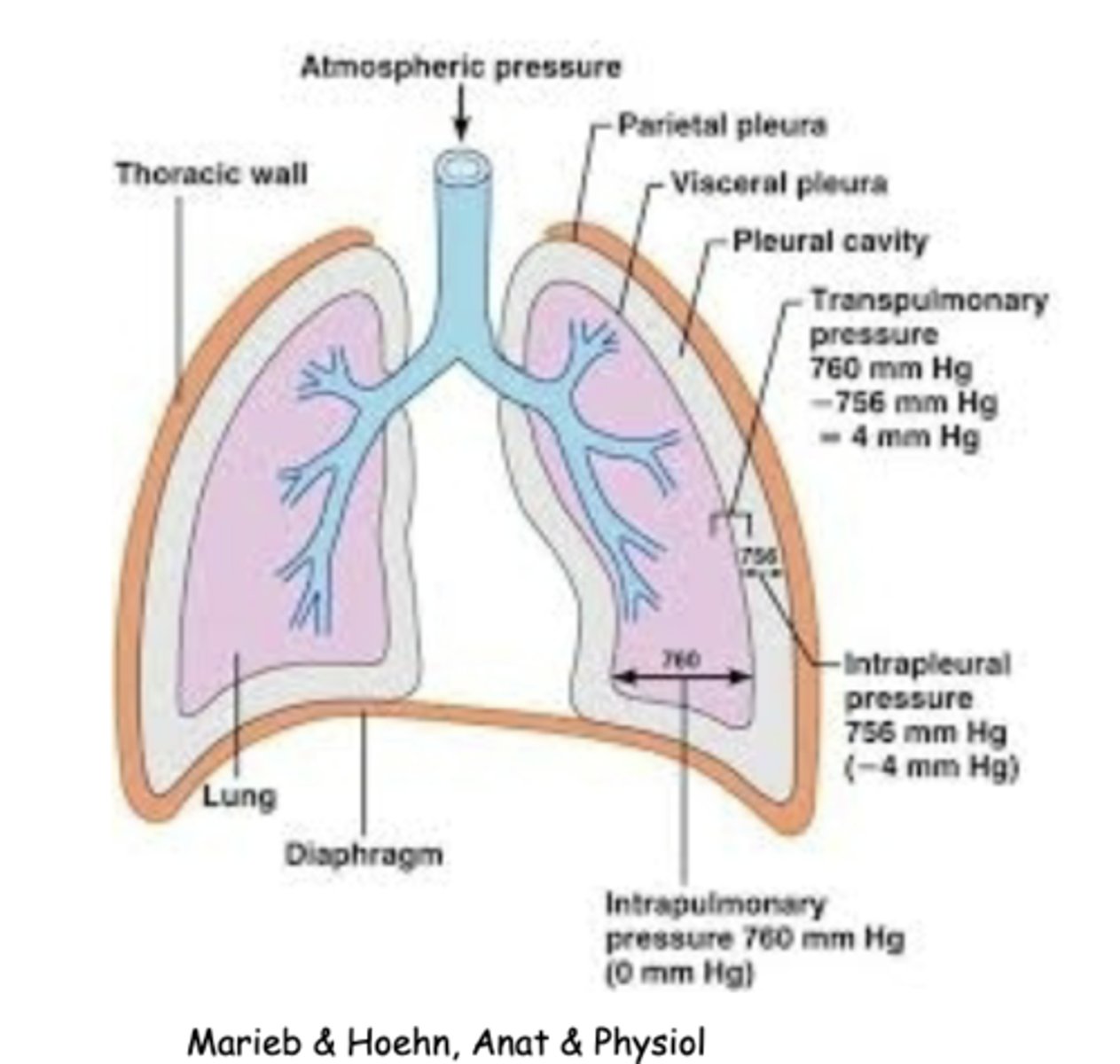
transmural pressure (PTm = P alv - P ip)
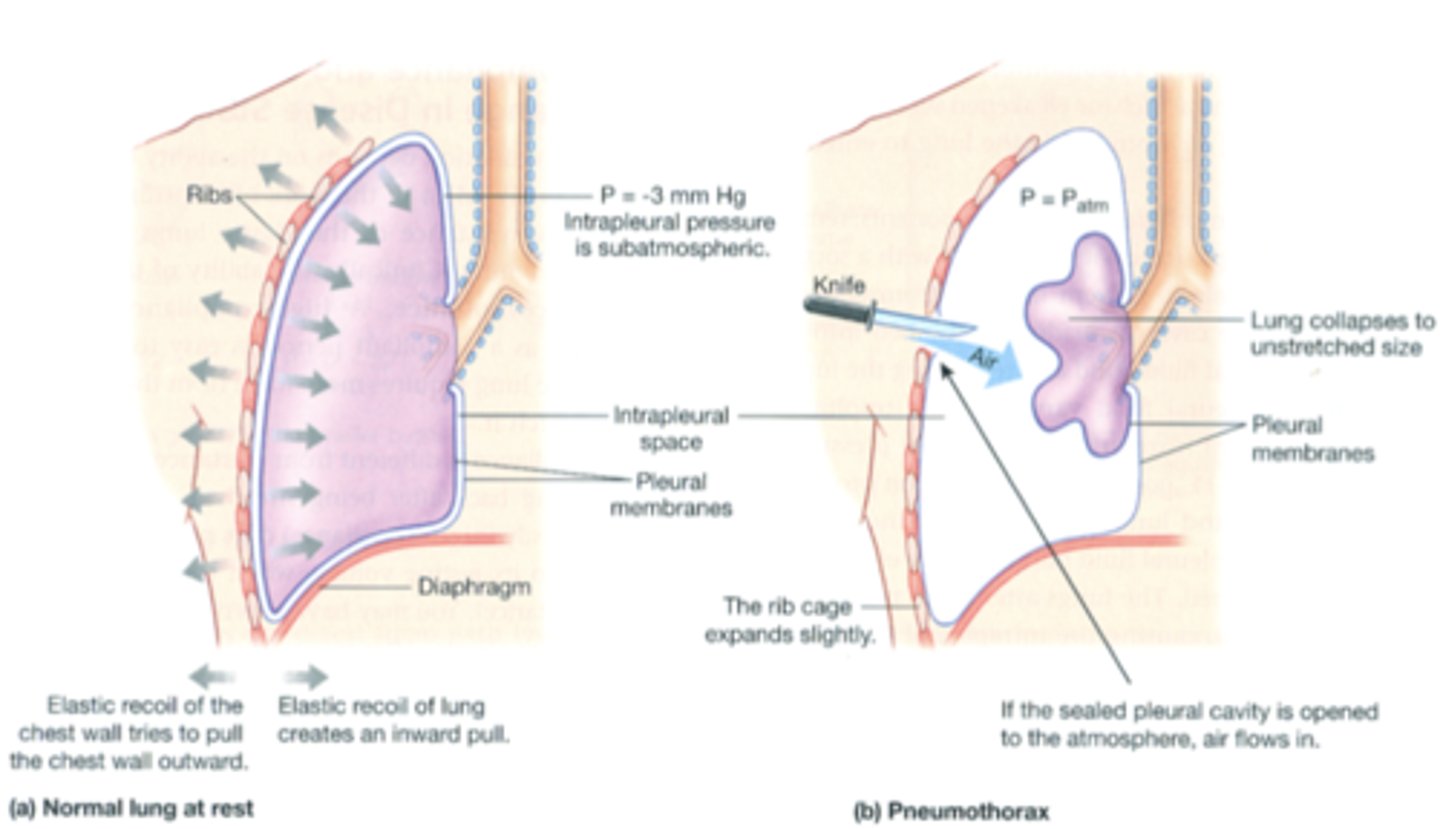
What balances the recoiling tendency of the lungs?
**fact check this card after re-watch**
the outwardly-directed recoil of the chest wall
Why does pneumothorax cause the lung to collapse?
air flows into the pleural cavity --> chest is separated from the lung --> elastic recoil of chest wall that pulls the lung outward is no longer present --> lung collapsed to unstretched size
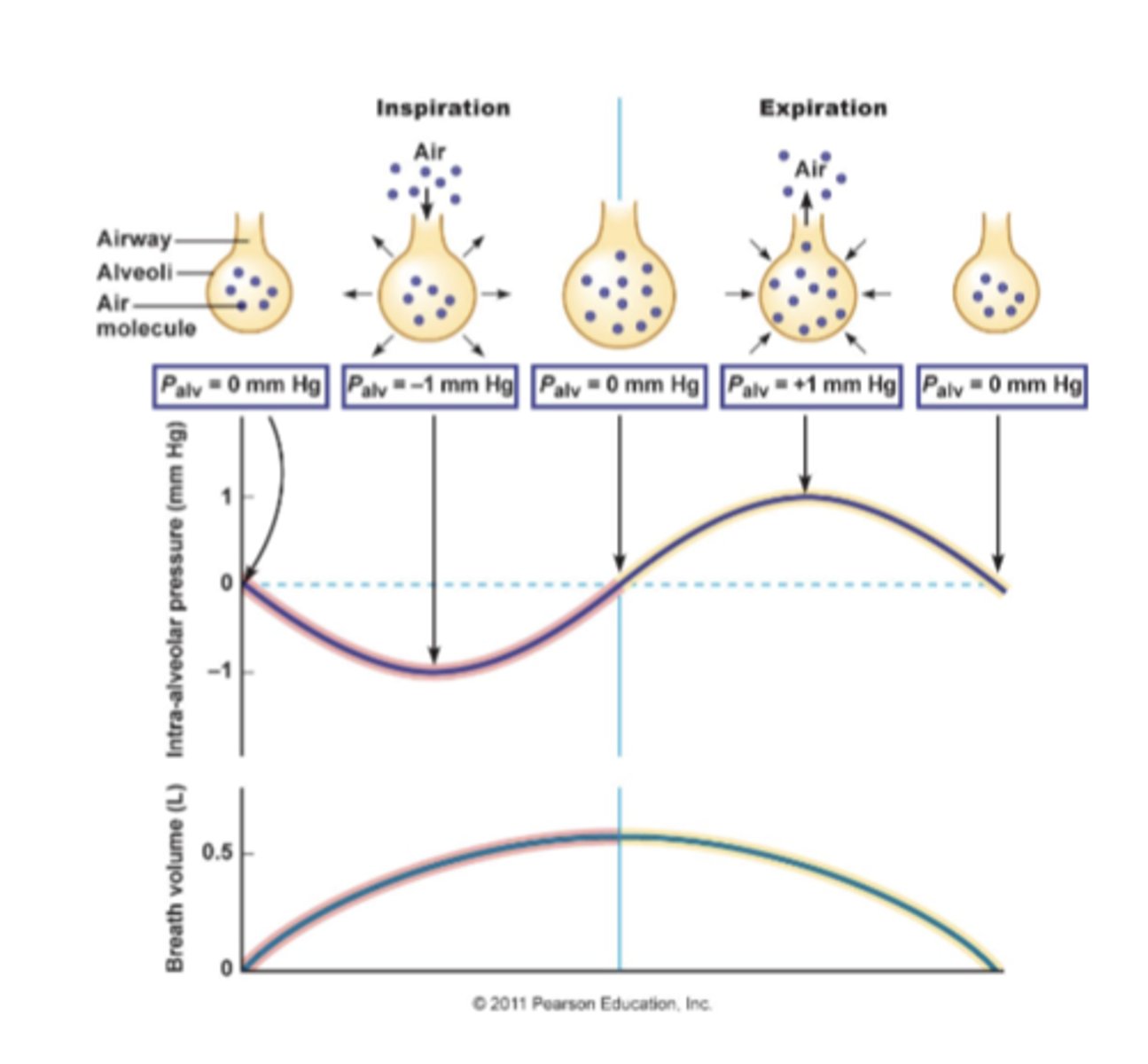
Describe the pressure-volume relationship depicted in Boyle's Law
-reduction in volume of container containing an amount of gas = increased pressure (increases collisions)
-increasing the volume of container = decreased pressure
P1V1 = P2V2
At the functional residual capacity (FRC), what is the pressure in alveoli (P alv)?
P alv = atmospheric pressure
At functional residual capacity (FRC), what is the intrapleural pressure (P ip)?
P ip = -5 mmHg (approx)
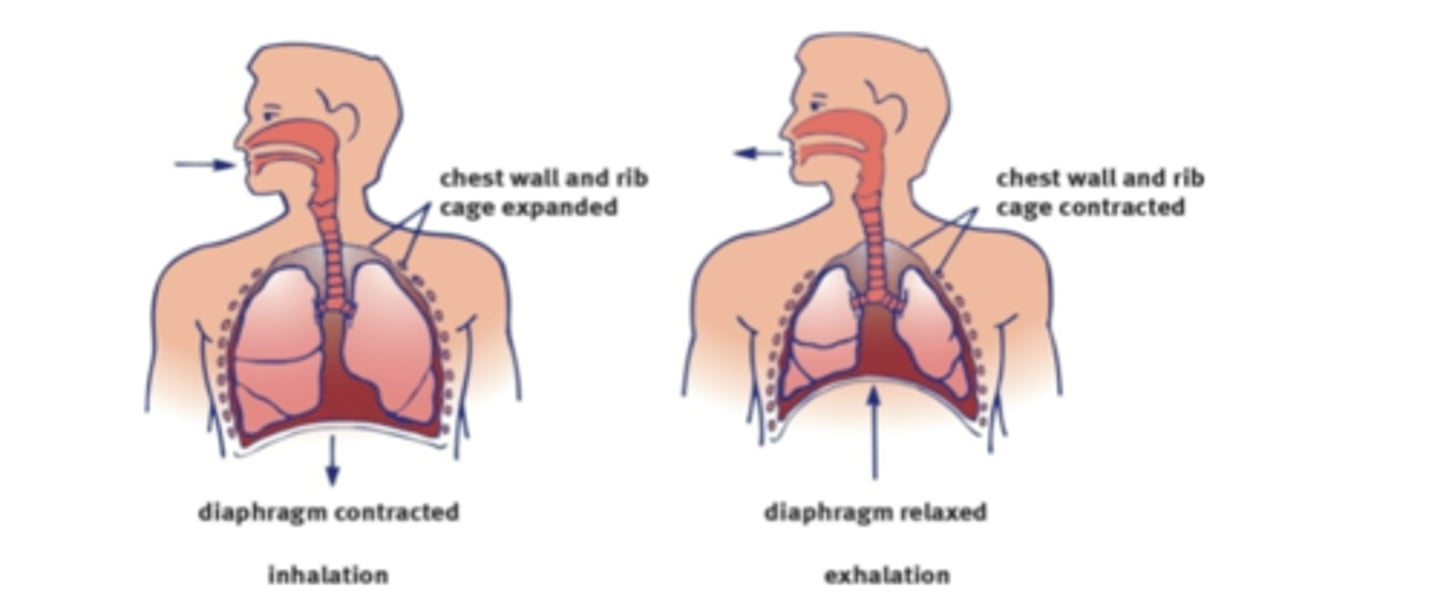
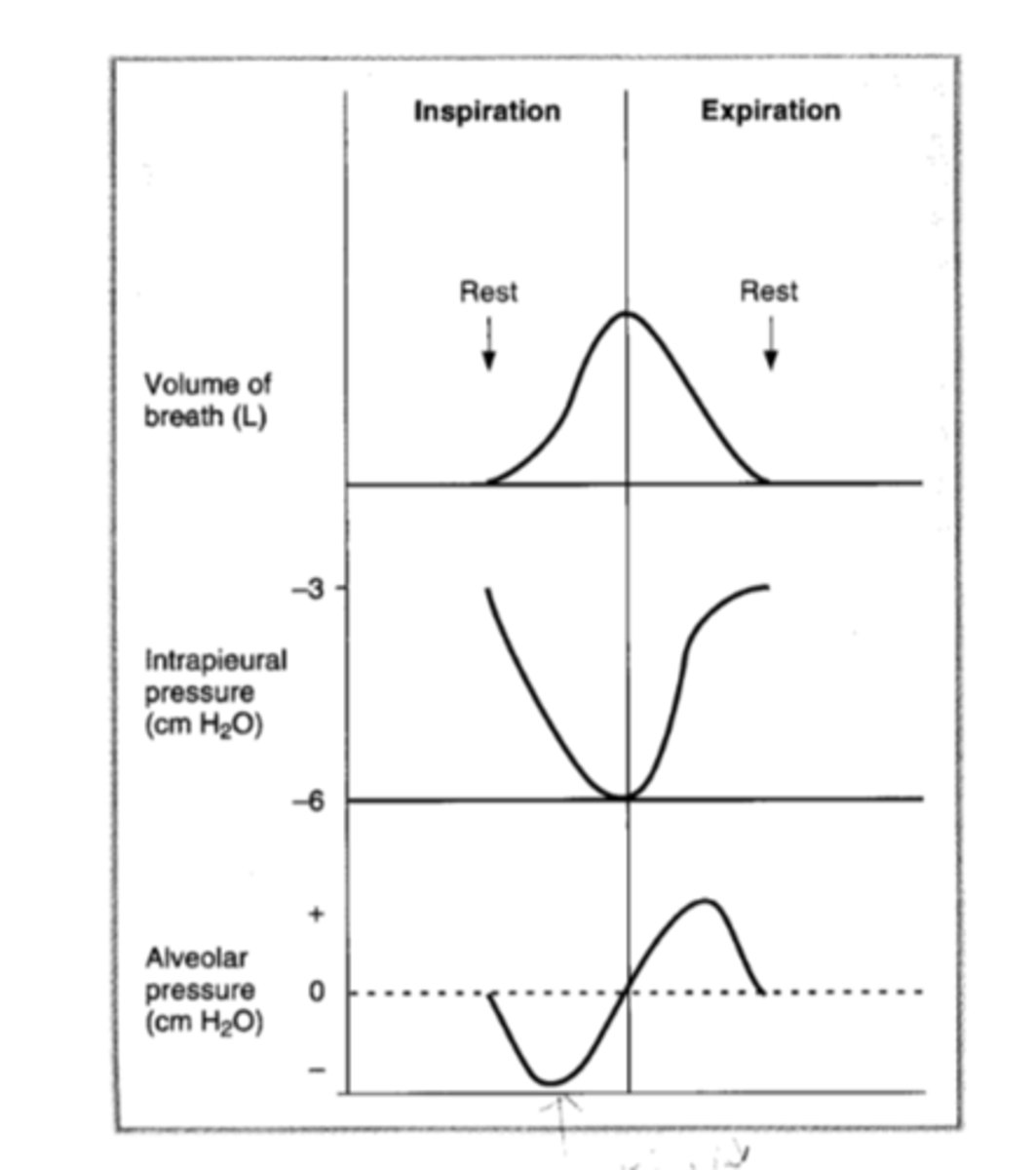
Describe the how inspiration is carried out by pressure changes.
intrapleural pressure drops when the diaphragm contracts & the external intercostals expand the chest wall--> increases the transmural pressure (P Tm) --> lung is pulled outward --> alveoli expand --> alveolar pressure (P alv) drops below atmospheric pressure --> air flows into the lung
When is Boyle's Law demonstrated during inspiration?
when the lung is pulled outward when the chest expands, the alveoli expand and their pressure drops below atmospheric pressure
*increased volume = decreased pressure
Why is the diaphragm convex at rest?
b/c it is pushed into the thoracic cavity by the abdominal organs
What is the primary muscle of respiration during quiet breathing?
diaphragm
-contraction straightens the diaphragm --> increases thoracic volume in the inferior dimension to allow for inspiration
-relaxation makes the diaphragm return to being convex --> allows passive expiration
Which muscles play a role in forced inspiration?
-scalenes
-external intercostals
-pectoralis minor
-intercartilaginous part of internal intercostals
-diaphragm (always involved in breathing tho, the it girl)
How do the scalenes aid in inspiration?
fix or elevate ribs 1-2
How do the external intercostals aid in inspiration?
elevates ribs 2 -12 to widen the thoracic cavity
How does the pectoralis minor aid in inspiration?
elevates ribs 3-5
How does the intercartilaginous part of internal intercostals aid in inspiration?
aid in elevating the ribs
Which muscles are involved in force expiration?
-interosseous part of internal intercostals
-rectus abdominis
-diaphragm (the it girl of breathing)
What is the function of interosseous portion of internal intercostals during forced expiration?
depress ribs 1 - 11 to narrow the thoracic cavity
What is the function of the rectus abdominis in forced expiration?
-depresses lower ribs
-pushes diaphragm upward by compressing abdominal organs
Before inspiration, what is the average alveolar pressure (P alv)?
760mmHg = atmospheric pressure
During inspiration, what is the average alveolar pressure (P alv)?
decreases to 758 mmHg
During expiration, how is the average alveolar pressure increased to 762 mmHg?
via compression of the alveoli = decreased volume = increased pressure
True or False: The intrapleural pressure becomes more negative as the lungs are pulled out by the expanding chest wall
True
How is minute ventilation increased with increasing physical activity?
-increasing the frequency of breathing
-increasing tidal volume by including inspiratory & expiratory reserve volumes in each breath
How is airway resistance assessed?
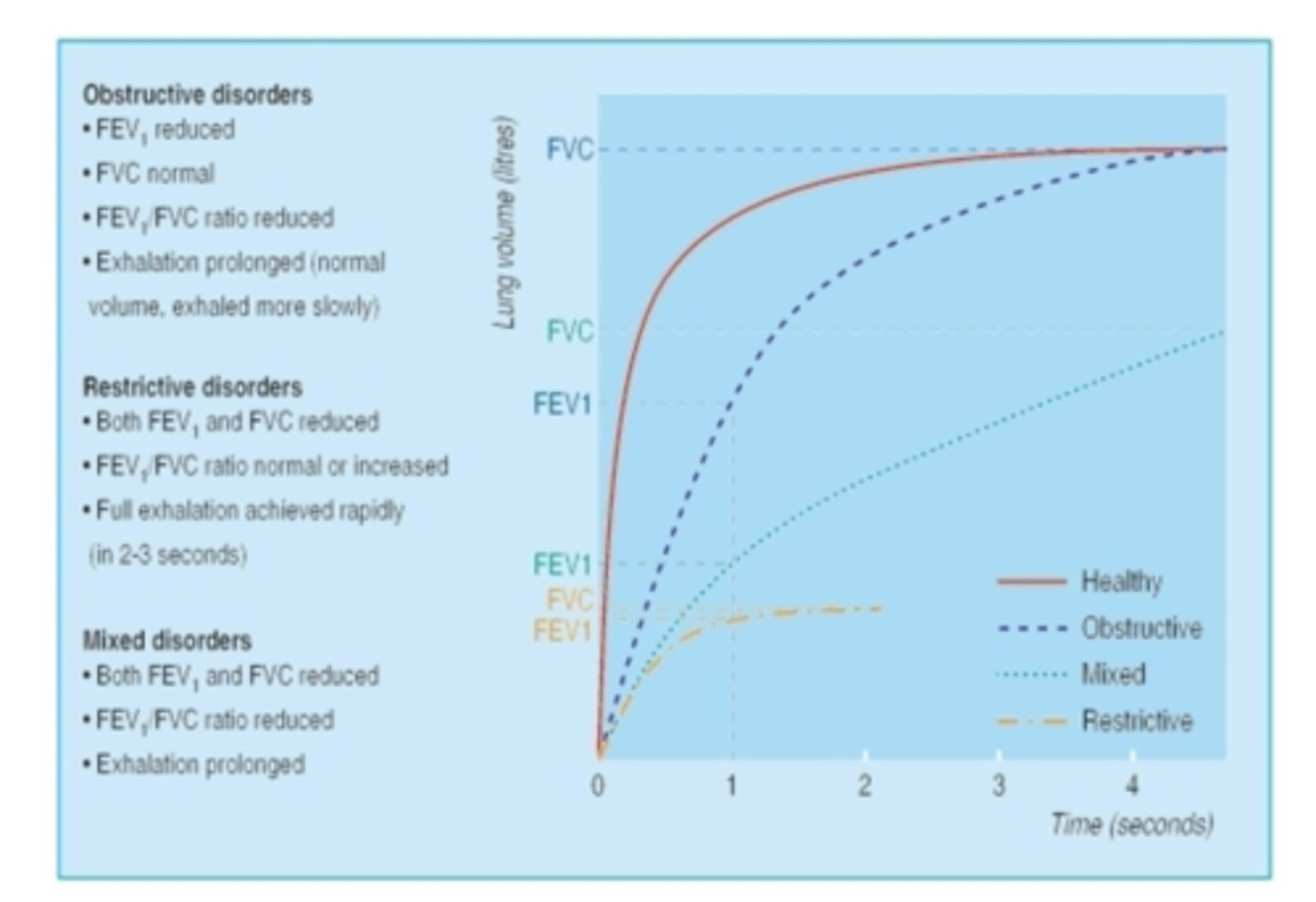
FEV1/ FVC ==> volume of air forcefully expired in 1 second/forced vital capacity (how much air pt can force into lungs)
1.) pt fills lungs to vital capacity = FVC
2.) forcefully expires & FEV1 recorded
3.) FEV1/ FVC should be at least 70% or it indicates increased airway resistance (obstruction)
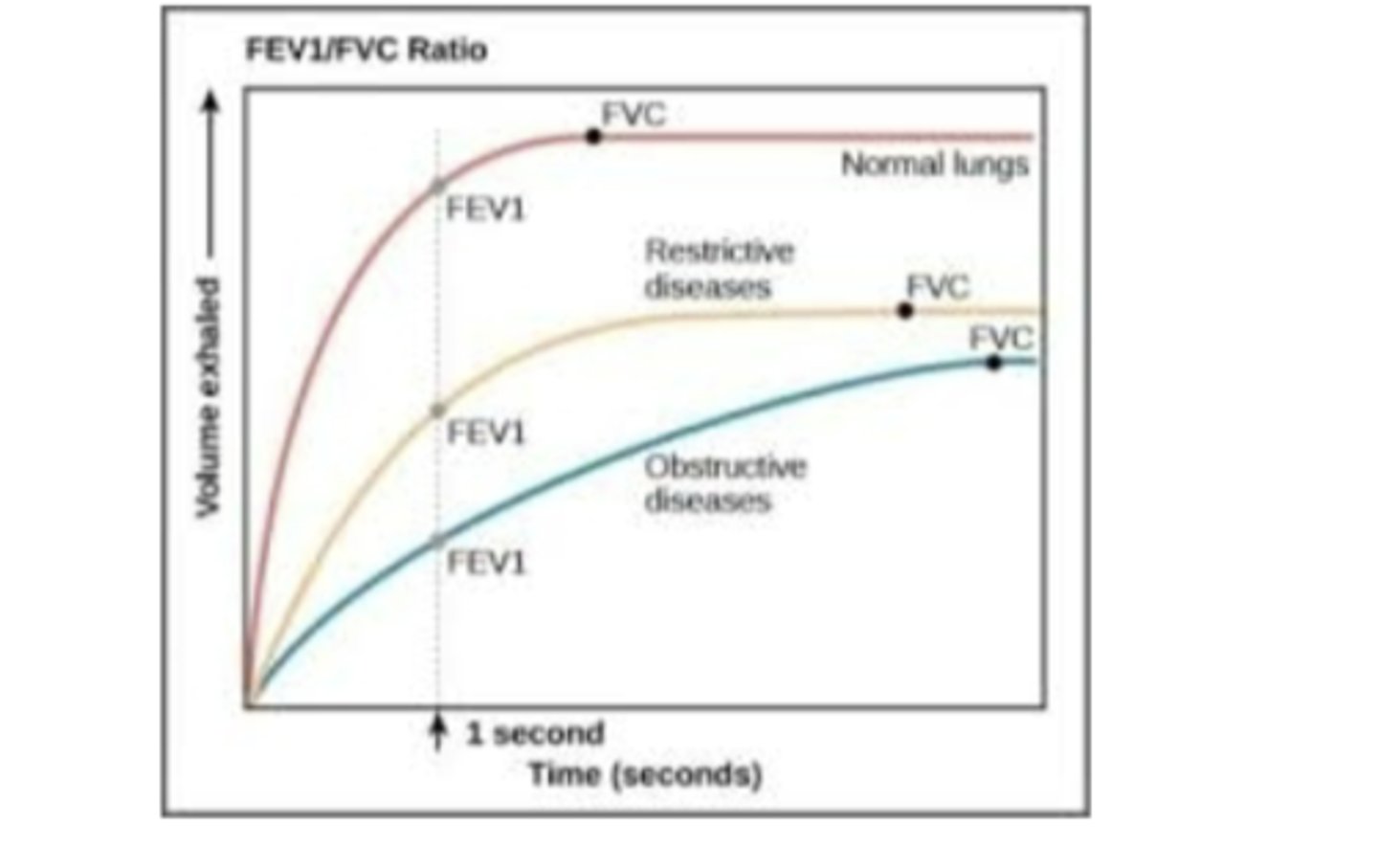
A patient with an airway obstruction will have a FEV1/FVC that's _______________________.
less than 70%
What are some factors affecting forced expiratory flow?
-airway diameter --> varies with the size of the lung b/c larger lung volumes tend to pull airways open = decreased resistance
-pressure in the airways is the same as the pleural pressure + elastic recoil during forced expiration (beginning at the total lung capacity)
-equal pressure point (EPP) -->during expiration when airway pressure & pleural pressure are equal = flow limitation when airway pressure drops below EPP b/c smaller airways become compressed
equal pressure point (EPP)
during expiration when airway pressure & pleural pressure are equal ==> flow limitation when airway pressure drops below EPP b/c smaller airways become compressed
*a factor that affects forced expiratory flow
What effect does obstructive disorders have on FEV1 & FVC
-reduced FEV1
-normal FVC
-reduced FEV1/FVC
*exhalation prolonged--> normal volume, but exhaled more slowly
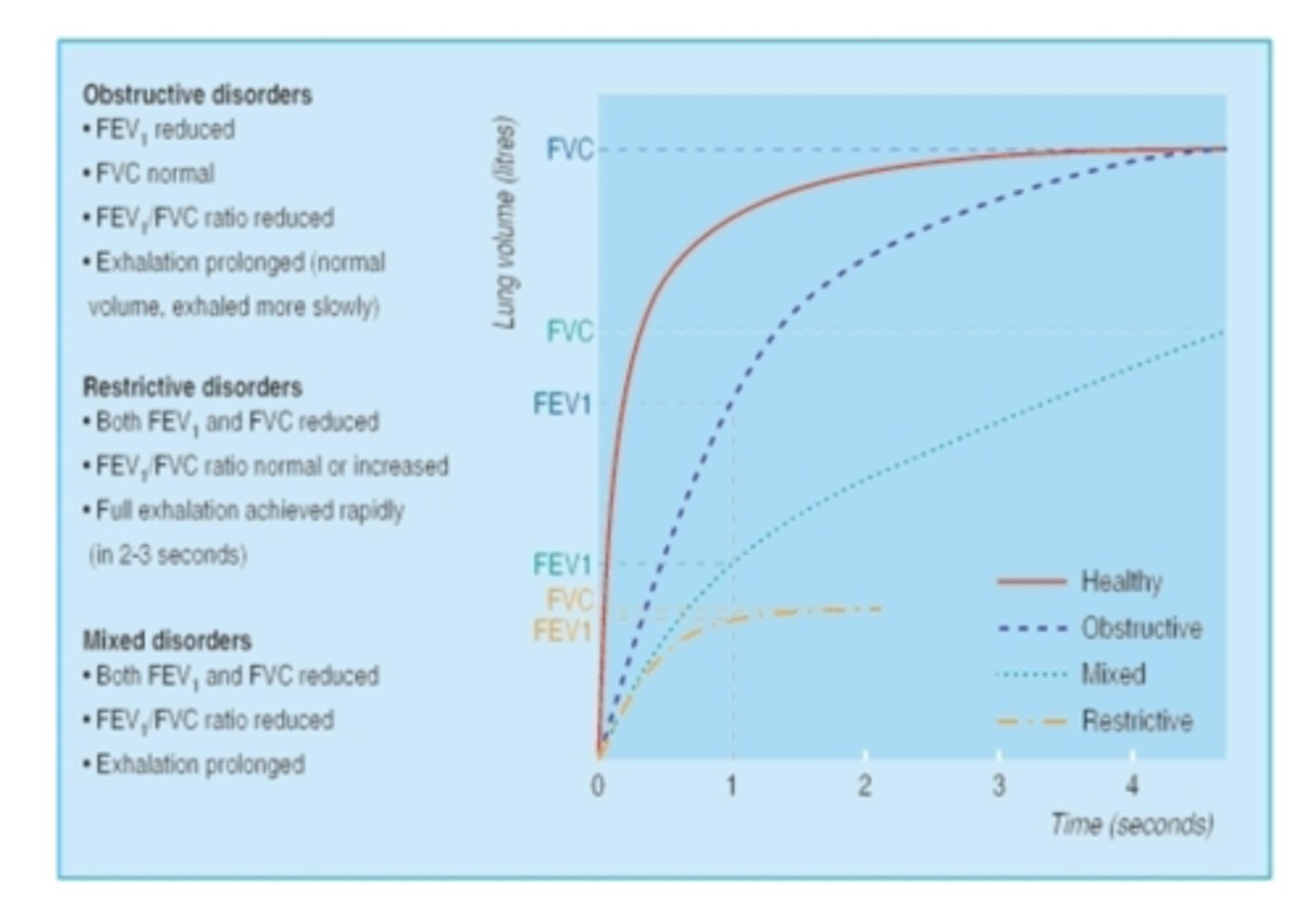
How does obstructive disorders affect exhalation?
prolonged exhalation
*normal volume, just exhaled more slowly

How does restrictive disorders affect FEV1 & FVC?
-reduced FEV1
-reduced FVC
-FEV1/ FVC ratio is normal or increased
*full exhalation achieved rapidly (2-3 seconds)
How does restrictive disorders affect exhalation?
full exhalation is achieved rapidly (2-3 seconds)
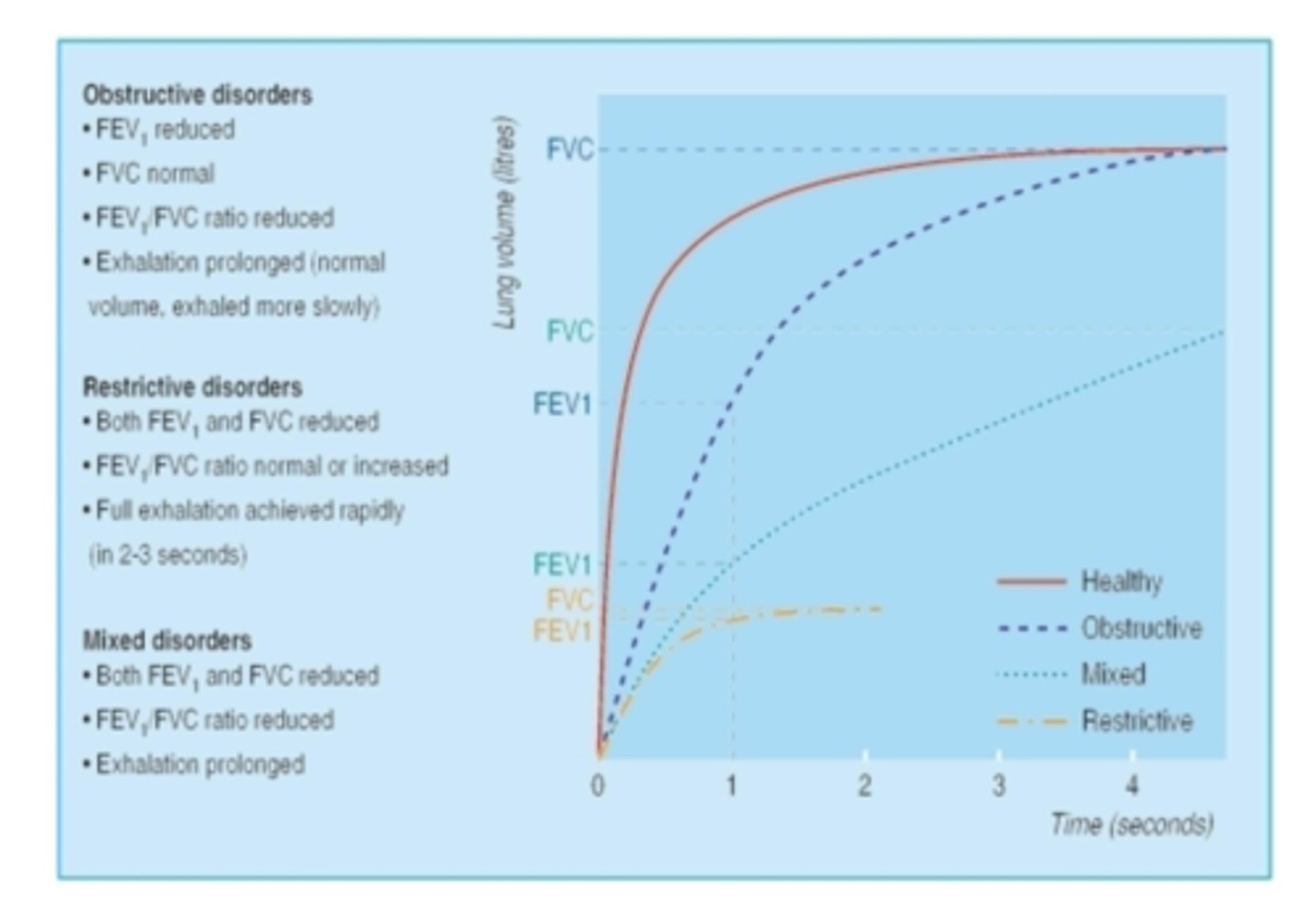
In mixed disorders (obstructive & restrictive) how FEV1 & FVC affected?
-reduced FEV1
-reduced FVC
-reduced FEV1/FVC
*exhalation prolonged
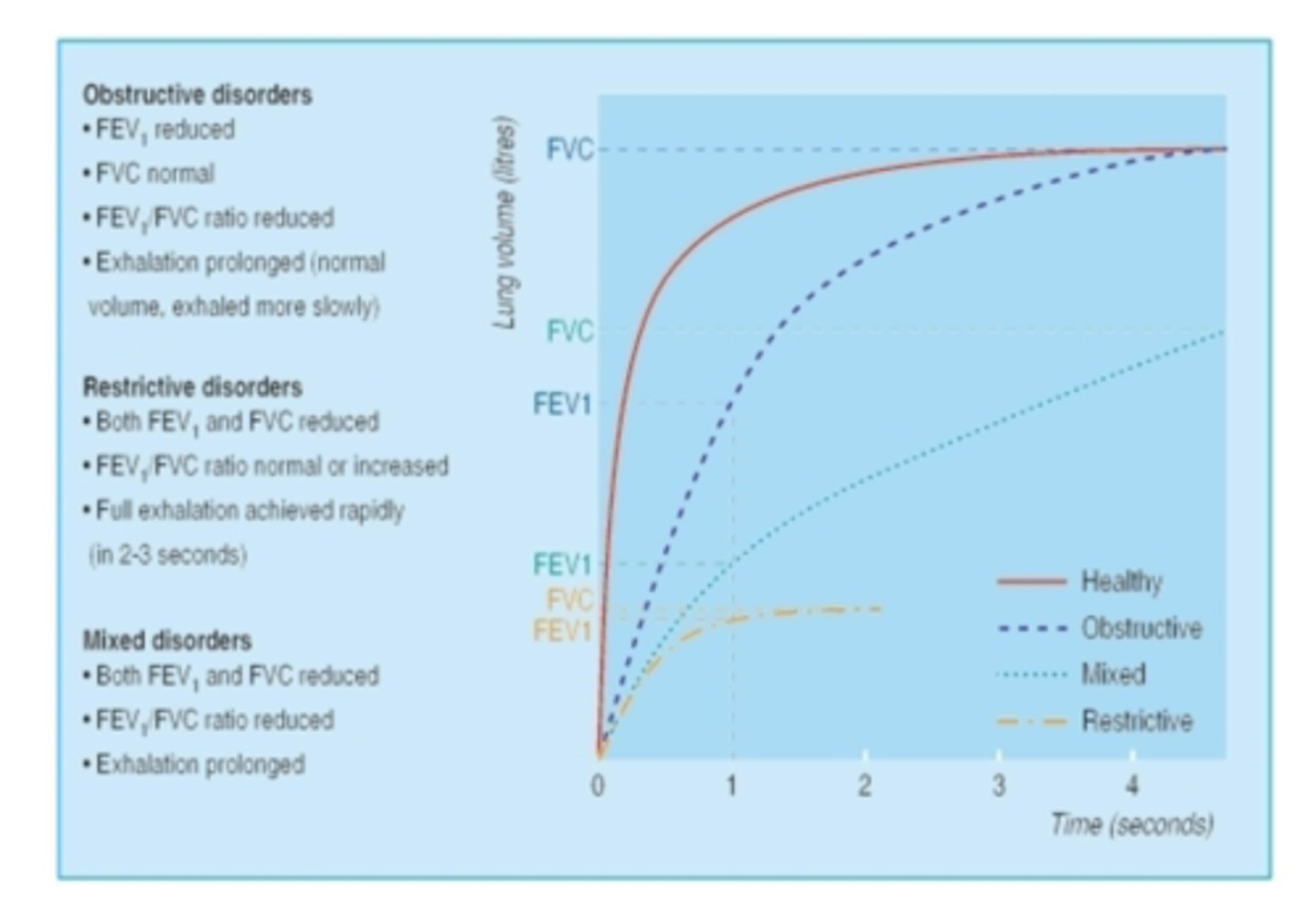
How does mixed disorders (obstructive & restrictive) affect exhalation?
prolongs exhalation