PT7130- Heart and Lung Transplant
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
Echocardiogram; perfusion; liver and kidney; cancer
Medical Screening:
General physical exam, ____________________, pulmonary function test, ____________________ test, maximal oxygen uptake (exercise testing or medically induced), lab test for ____________________ function, _____________________ screenings
Right heart catheterization
To screen for pulmonary hypertension, _______________________ is performed.
Blood vessels in lungs are narrowed or blocked.
Burgundy in image.

Slows blood flow through lungs.
Purple in image.

Blood pressure in the lung arteries goes up.
Teal in image.

Heart must work harder to pump blood through the lungs.
Dark green in image.

Extra effort on heart eventually causes heart muscle to become weak and fail.
Light green in image.

6 month
Medical screen includes nicotine testing: ______________________ free before initial evaluation for transplant.
Leave of absence; safely; distance; financial; reversible
Psychosocial Aspects:
- Family support → Partner _______________________ from work, childcare, pets
- Home set up → Suitable living condition, able to enter and exit home ____________________, _____________________ from post transplant check up appointments
- _____________________ stability → Anti-rejection medication: $2,500 per month
- Potentially ______________________ conditions: Smoking, drug addiction, obesity, mental distress
Multidisciplinary team
Selection for transplant is determined by ________________________.
United Network for Organ Sharing (UNOS)
Not a list but a pool of candidates.
Type; size; location; urgency
United Network for Organ Sharing (UNOS):
How candidates are matched with donor based on multitude of factors.
- Blood ____________________
- Body ___________________ (height and weight)
- _______________________ of medical facility
- Medical ________________________
Urgent; survival
The candidates who will appear highest in the ranking are those who are in most _____________________ need of the transplant, and/or those most likely to have the best chance of _______________________ if transplanted.
24 hours; travel bag; 1.5 hours; patient and 1 family member
Transplant Match Completed:
- Patient must be available by phone _________________________ a day waiting for a phone call from the transplant coordinator.
- Have a ______________________ prepped and ready for when call happens.
- Patient must live within _______________________ from transplant facility → Coordinator will arrange ride for ______________________
Heart transplant
Last-resort treatment for people who have end-stage heart failure from multiple conditions including: cardiomyopathy, coronary artery disease, and congenital heart disease.
70
Heart transplants are possible for children and adults up to age _____________________ and in some circumstances up to age 75.
Rare
Heart transplants are ________________________.
Sternal; 6 weeks; pain/sedation; post-op day 1; vent weaning; 60-100; pacing wires
Treatment Considerations s/p Heart Transplant:
- ________________________ precautions
- No driving for at least _________________________ after surgery. Plan ahead so a friend or family member can help out during this time. Unable to drive while on _________________________ medications.
- When therapy begins → Can begin as early as __________________________
- Demographic specifics which affect therapy → ___________________________, Swan line, Amiodarone, Direct current cardioversion (DCCV), orthostatics, chest tubes/JP drains, wound vac, dialysis, ____________________________
- Biggest thing /c heart transplant is passing out! → MAPS between ___________________. If below, nurse gives Neostick and re-check.
- Little white ticks on telemtry indicate ________________________.
- If asystolic /s pacing, most we are going to do is stand-pivot transfer to chair. → Ask nurse what RHR is /s pacing.
Prior; independence; stable
ICU Goals:
- Determine level of mobility _____________________ to transplant and current mobility status
- Improve ____________________ /c basic bed mobility, transfers from bed ↔ recliner ↔ BSC, and hopefully ambulate
- Patient must be _____________________ medically along /c physically to be cleared for transfer from ICU
PLOF; ambulation; patient goals; long-term
Step Down Goals:
- Return to ____________________ or obtain safe mobility skills for expected discharge disposition
- Continue to progress mobility obtained while in ICU → Initiate ____________________ if not already started, complete stair training, car transfers, home specific mobility tasks
- Ensure therapy goals align /c _____________________ → Goals must be realistic and attainable. Therapist must be able to explain why some goals are unrealistic or if the patient sells themselves short on goals.
- Short-term attainable goals lead to ______________________ success!
Removing
In some lung disorders, _______________________ part or all of the lung can effectively treat the problem.
Lung transplant
But if a disease affects both lungs, or when medical treatment has not improved the lung condition, the best treatment choice may be a _________________________.
Cystic fibrosis; COPD; pulmonary hypertension
Lung transplant may be recommended for patients with diseases such as interstitial lung disease, _______________________, pulmonary fibrosis, _______________________ (including emphysema), or ________________________.
5-10 lbs; 6-8 weeks; 6 weeks; exercise; tired; pain
Post-Lung Transplant Precautions:
- Do not lift anything over ______________________ → Including your suitcase when you leave the hospital
- Avoid strenuous physical work for at least _____________________. → After that, consult your Transplant Pulmonologist for weight restrictions.
- No driving for at least ____________________ after surgery. Plan ahead so a family member or friend can help out during this time. When you are in a motor vehicle, always wear your seat belt. You cannot drive if you are on pain/sedation medications.
- Gradually increase your physical activities. → ______________________ is encouraged! We recommend beginning /c stretching exercises and walking to help you regain your strength. Pay attention to how you feel when exercising. Stop and rest when you feel _____________________ or if you feel ______________________.
Post-op day 1
Therapy can begin as soon as ________________________ after lung transplant.
Pressure control
Orange in image.

Pressure support /c CPAP
Dark green in image.

HFTC (AirVo)
Teal in image.

TC (/c and /s speaking valve)
Burgundy in image.

Red cap nasal cannula
Light green in image.

Anxiety
_________________________ management utilizes a multidisciplinary approach.
Organ rejection and infection
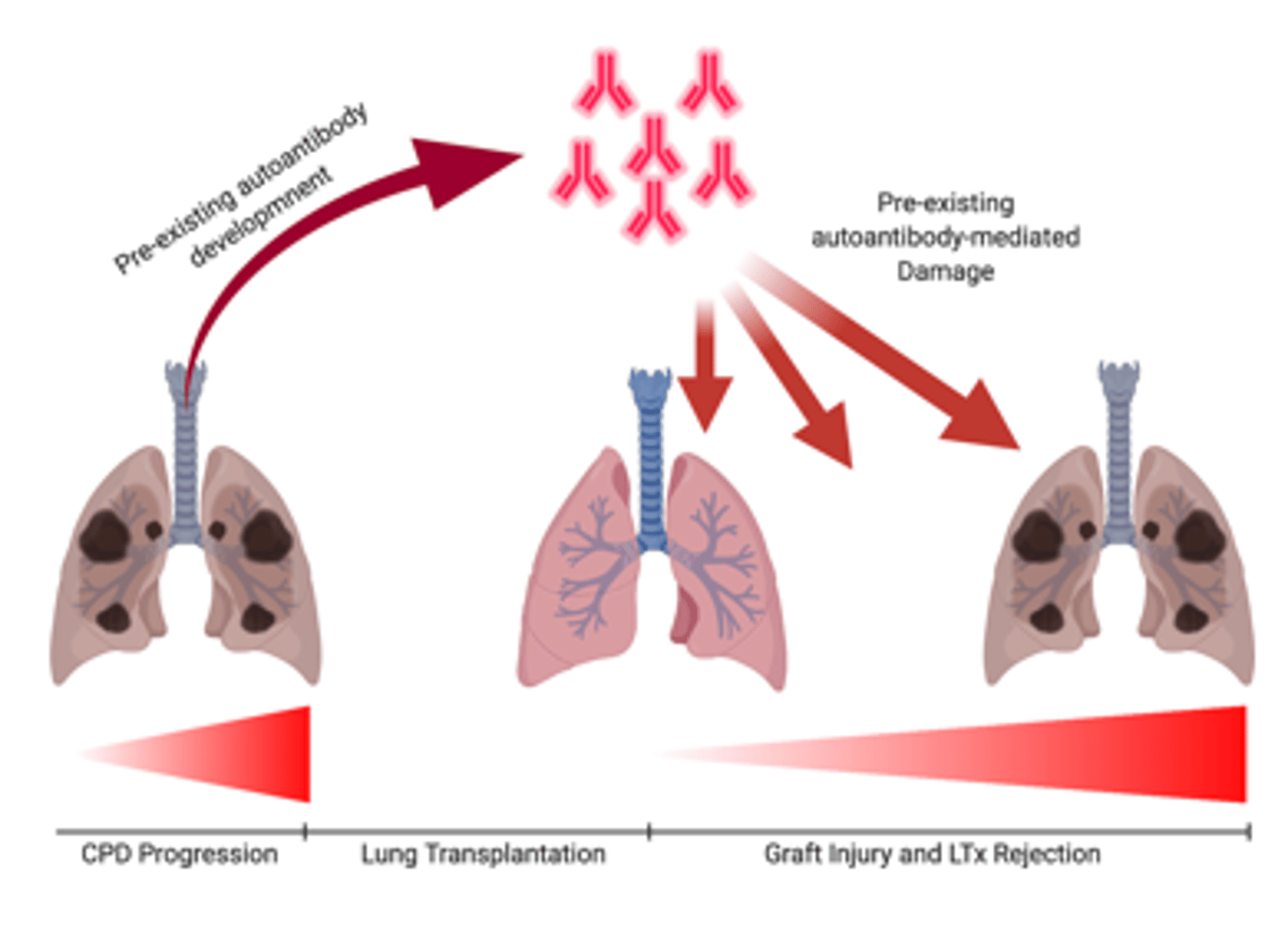
What are the two main complications of transplant surgery?
Rejection
Immune celles recognive the transplanted lung as different from the rest of the body and attempts to destroy it.
Immunosuppressive drugs; rest of your life
After transplant surgery, you are prescribed __________________________ to "fool" your immune system into thinking your new lungs belong. These medications will be taken for the ________________________.
Six months
Acute rejection is most common in first _________________________ after surgery, but it can occur at any time. Fortunately, acute rejection can be treated, especially if the signs of rejection are recognized early.
100°; nausea/vomiting; fatigue; tenderness
Rejection Symptoms:
- Fever over ____________________
- Flu-like symptoms → Chills, aches, headaches, dizziness, ______________________
- Cough, SOB, _______________________
- New pain or _______________________ around lung
Pulmonary function testing; lab values
Rejection Identification:
- Daily _________________________
- Chest x-ray or CT
- Bronchoscopy
- Symptoms
- ________________________
Tacrolimus (Prograf)
Rejection medication that may cause kidney damage → Leads to many patients being on dialysis.
Tremors
What is another major side effect of Tacrolimus (Prograf)?
Prednisone
Started in high doses post-transplant and tapered down.
Pressure ulcers; retention; insomnia; blood sugar
Side Effects of Prednisone:
- Inhibits wound healing → _________________________, especially in ICU
- Sodium and water _______________________ → Further exacerbating kidney issues and dialysis need
- _________________________
- Increased ________________________
Months; mental; letter
Return to Work s/p Transplant:
- May return to work within a few ______________________ after surgery.
- Appropriateness depends on not only physical but _______________________ aspects of the work environment.
- Will need to discuss /c transplant coordinator and doctor to have "return to work" ________________________ provided for employer
You feel better; on hand; emergency medical identification; transplant coordinator
Vacation s/p Transplant:
- May travel as soon as _________________________
- Must ensure all medications are ________________________ and wear your ________________________
- Must notify ________________________ of trip and have their number on hand in case of emergency
6 weeks; 2 flights; not recommended; 1 year; medications
Sexual Activity s/p Transplant:
- _____________________ after transplant and able to walk _______________________ of steps /c minimal shortness of breath
Females:
- Birth control _______________________ post transplant due to birth control complication /c medications
- Pregnancy is not recommended, especially within _________________________ after transplant surgery. The medicines you take after surgery are harmful to a developing baby, and the stress of pregnancy on your body can be harmful to your health.
Males:
- Difficulty /c erections after surgery. This might be caused by a reduction of blood flow to the penis, or it might be a result of the transplant _________________________. In most cases, this situation can be corrected.
Absorption; alcohol; burn
Dietary Modifications s/p Transplant:
- No grapefruit, starfruit, pomengrate → Dramatically change _______________________ of anti-rejection meds
- No _______________________ d/t liver involvement and medication interaction
- Do not ________________________ food d/t absorption of medication differences
Aspergillosis
Gardening s/p Transplant:
No gardening or yard work post transplant d/t risk of ________________________ exposure → Infection from mold which targets the respiratory system
C. Difficile colitis
Gastrointestinal Post-Transplant Lifestyle Modifications:
_________________________ is a bacterial infection of the colon.
Birds or exotic pets; feces; change litter
Pets s/p Transplant:
- No ________________________
- Dogs allowed but unable to clean up _____________________
- Cats allowed but unable to _____________________. If scratched by a cat, contact transplant coordinator immediately.
Sitting in front seat
Driving s/p Transplant:
No driving or _______________________ for 6 weeks.
Pulmonary rehab phase 2; 20-30 minutes
Pulmonary Rehabilitation:
- _____________________________: 3 times per week when returning home
- Additionally, 2 days per week at home for ________________________ should be done
Quality of life; traumatic stressor; resilience; self-efficacy; social support
Psychosocial Aspects:
- __________________________ after transplantation varies greatly from patient to patient.
- Majority of patients appear to cope very well, while others seem to struggle postoperatively.
- For many patients, the transplantation itself, as well as the ICU stay, might be perceived as a _________________________ that can decrease QOL and trigger mental distress.
- A high degree of _____________________ and _____________________ as well as _____________________, are essential to coping successfully /c the transplant experience.
Patient and family members; comfort and reassurance
Dealing with Death:
- Death of a patient is a very real possibility everyday you walk onto the ICU unit. Being able to discuss the topic of death with not only the medical team but the _________________________ themselves is a crucial skill the therapist must have.
- Can provide _______________________ to the patient and family but there are medical professionals on the team who can handle these situations if you feel uncomfortable (chaplains, psych, MDs, hospice, palliative medicine, Lifebanc)
- Coping for therapist → There are resources available for therapist to deal /c patient death including therapy and support groups.