Understanding Motivational Interviewing Techniques
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
106 Terms
What is the spirit of Motivational Interviewing (MI)?
The spirit of MI involves collaboration, evocation, and autonomy, focusing on the patient's internal motivation for change.
How do the biomedical and psychosocial models of communication differ?
The biomedical model is provider-centered, focusing on information giving and dictating behavior, while the psychosocial model is patient-centered, emphasizing negotiation, adherence, and understanding.
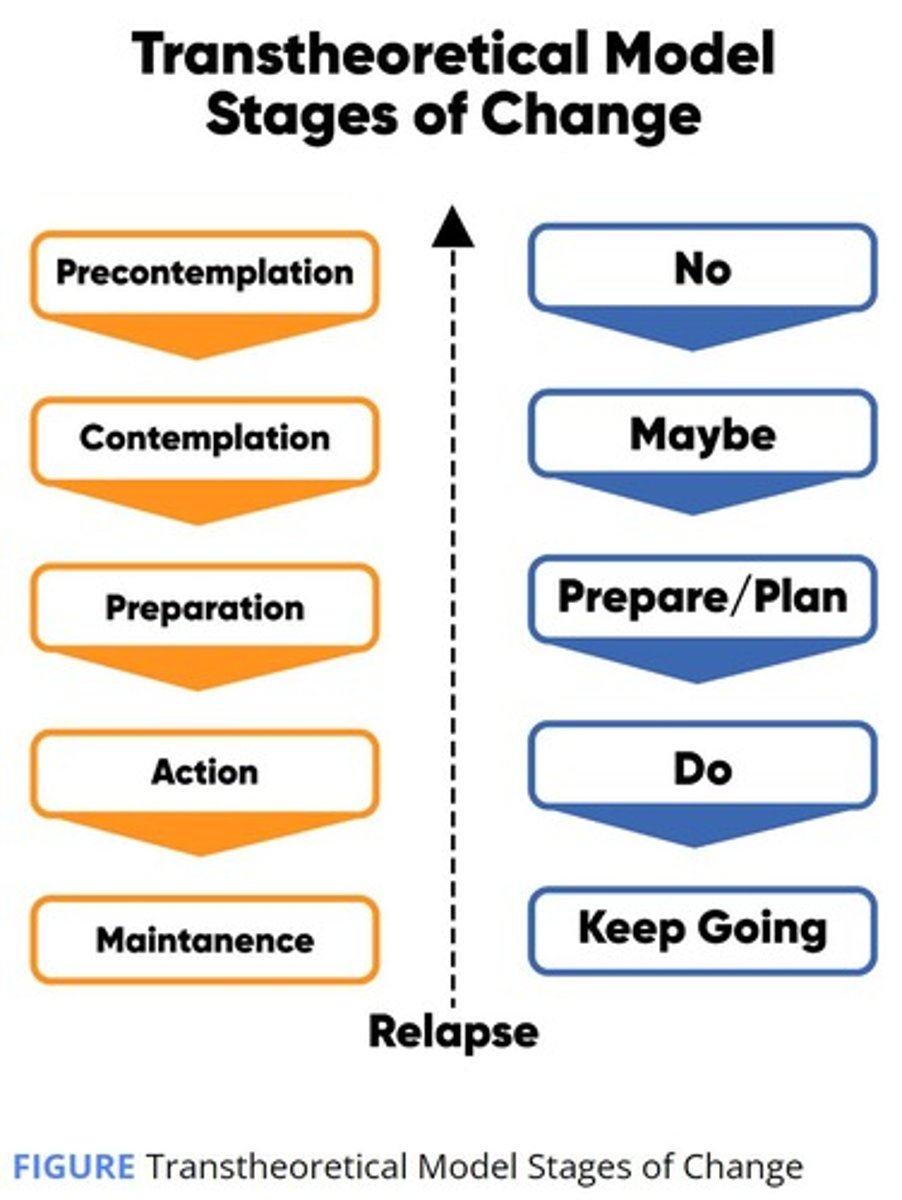
What are Prochaska's Stages of Change?
1. Precontemplation: not thinking about change ('I won't'). 2. Contemplation: thinking about change in the long run ('I might'). 3. Preparation: preparing for change in the short run ('I will'). 4. Action: engaging in behavior for less than 6 months ('I am'). 5. Maintenance: engaging in behavior for more than 6 months ('I am and I have been').
What is the decisional balance concept in health behavior decision-making?
Decisional balance involves weighing the pros and cons of changing a behavior; patients influenced by cons are less ready to change, while those influenced by pros are more ready.
What is the righting reflex and its impact on patients?
The righting reflex is the natural tendency of helping professionals to fix what's wrong with patients, which can hinder patient adherence and motivation.
Define empathy in the context of Motivational Interviewing.
Empathy is the ability to understand and share the feelings of another, crucial for building rapport and trust in MI.
What are some examples of empathic responding?
Examples include reflective listening, validating feelings, and expressing understanding of the patient's perspective.
What are the MI communication principles?
The principles include expressing empathy, developing discrepancy, rolling with resistance, and supporting self-efficacy.
What is change talk and why is it important?
Change talk refers to the patient's own statements about wanting or needing to change, which is crucial for fostering motivation.
What are the types of change talk?
Types include desire (wanting to change), ability (believing one can change), reasons (understanding why change is important), and need (feeling a need to change).
What are the roles of the readiness, importance, and confidence rulers in MI?
These rulers help explore a patient's ambivalence and resistance, and engage them in change talk by assessing their readiness to change.
How can agenda-setting enhance patient autonomy?
Agenda-setting involves collaboratively determining the topics to discuss, which empowers patients and respects their autonomy.
What feelings can make change difficult?
Feelings such as anger, unresolved grief, depression, and guilt can hinder the change process.
What thoughts can impede behavior change?
Thoughts like health beliefs, feelings of powerlessness, and limited confidence can create barriers to change.
What practical barriers might patients face in changing behavior?
Barriers include literacy level, cost, and access to resources.
What percentage of individuals needing to change a behavior are often not ready?
50-70% of individuals needing to change are not ready.
What behaviors indicate patient ambivalence?
Behaviors include feeling stuck, procrastination, lack of motivation, and inconsistency between attitudes and behaviors.
What behaviors indicate patient resistance?
Resistance behaviors include blaming, disagreeing, arguing, excusing, minimizing, becoming hostile, interrupting, and ignoring the provider.
What is the role of self-efficacy in the Action and Maintenance stages of change?
In the Action stage, self-efficacy supports the patient in maintaining behavior change, while in the Maintenance stage, it reinforces continued adherence.
How does the provider-centered approach differ from the patient-centered approach in MI?
The provider-centered approach focuses on information giving and compliance, while the patient-centered approach emphasizes negotiation, adherence, and understanding the patient's perspective.
What is the significance of respecting patients in MI?
Respecting patients is foundational in MI, where respect is expected rather than earned, fostering a collaborative relationship.
What are some pros of medication adherence?
Control my own health, prevent complications, have more energy, avoid hospitalization, peace of mind, make my family happy.
What are some cons of medication adherence?
Inconvenient regimen, expense of co-payments, unpleasant side effects, food interactions with favorites, embarrassment, and not wanting to be reminded of illness.
What is the key point in facilitating a person's decision-making process regarding medication adherence?
Help facilitate the person's own decision-making process; interview to elicit internal motivation.
What is 'Change Talk' in the context of motivational interviewing?
The patient makes the argument for change by what comes out of his/her own mouth.
What is Motivational Interviewing (MI)?
A way of relating or communicating with people in a purposeful, genuine, and person-centered way.
Who can motivational interviewing be used with?
Patients, employees, bosses, friends, and colleagues.
What are the major assumptions of motivational interviewing?
Building ongoing relationships/trust, not motivating the patient but helping them find their internal motivation, the patient should do most of the talking, using a toolbox of communication strategies, and addressing ambivalence and resistance.
What are the core processes in motivational interviewing?
Engaging, focusing, evoking, and planning.
What are some micro skills used in motivational interviewing?
Open-ended questions, affirmation, reflection, and summaries.
What are the primary principles of motivational interviewing?
Expressing empathy, developing discrepancy, rolling with resistance and avoiding argumentation, supporting self-efficacy, and supporting patients' autonomy.
How does honesty and assertiveness contribute to trustworthiness in motivational interviewing?
By providing clear and direct information about health metrics and discussing strategies for improvement.
What is the purpose of the 'Readiness Ruler' in motivational interviewing?
To assess a patient's readiness to change by asking them to rate their readiness on a scale of 1 to 10.
What should a practitioner do if a patient rates their readiness as a 7 on the Readiness Ruler?
Ask why they rated it a 7 and what would need to happen for it to be an 8 or 9.
What is the significance of expressing empathy in motivational interviewing?
It involves careful listening, reflecting understanding, making the patient feel understood, reducing anxiety, and improving adherence and patient outcomes.
How can a pharmacist express empathy to a patient concerned about medication adherence?
By acknowledging the patient's feelings and asking about their specific concerns.
What is an example of expressing empathy in a conversation with a patient?
Pharmacist: 'You seem really discouraged, Mrs. Smith.' after the patient expresses frustration with medication side effects.
What is the role of reflection in motivational interviewing?
To show understanding and validate the patient's feelings, which can enhance the therapeutic relationship.
How does motivational interviewing address patient ambivalence?
By recognizing and exploring the patient's mixed feelings about change, allowing for a more supportive dialogue.
What does the 'SPIRIT of MI' refer to?
The patient-centered approach that underlies the principles and practices of motivational interviewing.
What is the goal of motivational interviewing?
To help patients find their own motivation for change rather than imposing motivation from the outside.
How can motivational interviewing improve patient outcomes?
By fostering a supportive environment that encourages patients to express their concerns and motivations, leading to better adherence and health management.
What are some examples of empathic responses?
Examples include: 'You seem _____', 'In other words...', 'You feel ___ because ___', 'It seems to you...', 'As I understand it, you seem to be saying...', 'I sense that...', 'It sounds like you are...'.
What should be avoided in empathic responses?
Avoid saying 'I understand how you feel.'
How can developing discrepancy motivate change in patients?
Motivation for change increases when patients become aware of discrepancies between their current situation and their goals or hopes for the future, creating dissonance.
What is a strategy for developing discrepancy in patients?
Strategy 1: Repeat back the pros and cons stated by the patient.
Give an example of repeating back pros and cons to a patient.
Example: 'So, on the one hand, you want to reduce your risk of dialysis by lowering your blood sugar, but on the other hand, you don't like to take medication and you feel fine.'
What is another strategy for developing discrepancy?
Strategy 2: Ask questions about behaviors that don't support the goals set by the patient.
What is a thought-provoking question to develop discrepancy?
Examples include: 'If I were to give you an envelope, what would the message inside have to say for you to think about quitting smoking?' or 'What will life be like for you when you lose the 30 pounds you have set as your goal this year?'.
What is the purpose of supporting self-efficacy in patients?
To notice, support, and encourage patient attempts or thoughts about change.
How should praise be given to patients?
Praise the behavior, not the person, and avoid over-praising to prevent sounding insincere.
What is an example of supporting self-efficacy?
Example: 'Mr. Richards, it's great that you take your diabetes medicine every day the way you planned. Keep it up!'
What are the MI micro skills to establish patient understanding?
Establish patient understanding about diagnosis & risks/susceptibility, maintain patient autonomy, engage in change talk, and build self-efficacy with incremental goals.
Why is it important to establish risk/susceptibility with patients?
Patients need to understand why change is needed and how it ties to their health goals.
How should risk/susceptibility be addressed in conversation?
Ask early in the conversation to get it out on the table and encourage patients to express their understanding.
What is an example of establishing risk/susceptibility dialog?
Example: 'Mrs. Smith, tell me what you know about what this blood sugar number (A1C) puts you at risk for?' followed by sharing information and discussing prevention.
What is the purpose of agenda-setting in patient autonomy?
To maintain autonomy and choice while organizing the structure of the conversation.
How can a provider use agenda-setting in a conversation?
Example: 'We can talk about taking medication, small changes you can make in the foods you eat, and getting more activity into your daily routine. Which of these would you like to talk about first?'
What type of questions should be used to promote patient autonomy?
Use open-ended questions to get patient input and explore their thoughts.
What is the benefit of using open-ended questions with patients?
They prevent the patient from feeling judged or interrogated.
What is an example of an open-ended question to explore patient thoughts?
Example: 'What are some things you can do to remind yourself to take this medication?'
How does engaging the patient in 'change talk' benefit the conversation?
It encourages the patient to discuss the change, benefits, and their prior successes, reinforcing their motivation.
What are the steps involved in Patient Autonomy when giving information?
1. Ask what they know, 2. Affirm that, 3. Ask permission to fill in the blanks, 4. Give the information/advice about disease and/or treatment.
What is Change Talk and why is it important?
Change Talk is a strategy that predicts action and is core to deciding to change; stated intention predicts change.
What questions can be asked to elicit Change Talk?
1. What do you see as the benefits of changing? 2. What would you like about your life if this changed? 3. How ready are you to change? 4. How confident are you that you can change?
What does the acronym DARN-CAT stand for in the context of Change Talk?
Desire, Ability, Reasons, Need, Commitment, Activation, Taking Steps.
How can you elicit Desire Change Talk?
Ask, 'What do you wish to achieve by taking your medication as prescribed?'
What is the purpose of Incremental Goals in behavior change?
To build self-efficacy through small successes, progressively building confidence towards bigger changes.
What is the significance of avoiding big words like 'diet' and 'exercise' when discussing change?
Using smaller, more manageable terms helps patients feel less overwhelmed and more capable of making changes.
What are Tiny Habits according to BJ Fogg?
Tiny Habits are new habits that follow after something already habituated, have a short duration goal, and celebrate every tiny success.
What does SMARTA stand for in goal setting?
Specific, Measurable, Achievable, Realistic, Timely, Attractive (to self), OR Accountability.
What should be avoided in goal-setting conversations according to MI principles?
Avoid the righting reflex.
What should be done if a patient relapses?
Use an MI-based relapse approach that includes empathy, self-efficacy building, change talk, and problem-solving.
What is a key phrase to use when a patient feels discouraged after a relapse?
'You sound discouraged; this must be hard for you.'
What does it mean that change is a process, not an event?
Change involves ongoing efforts and adjustments rather than a single moment of transformation.
How can you support a patient's self-efficacy during Change Talk?
Acknowledge their awareness of the need for change, e.g., 'That's great that you know you need to quit smoking.'
What is the role of vision in goal setting?
Goals are steps on a path to the desired future, and articulating vision is a form of change talk.
What is an example of a small change to suggest to a patient?
Cutting one soda out of your daily routine for the next week and see how that goes.
What should be included in both long-term and short-term goals?
Both should align with the patient's vision for their desired future.
How can you help a patient who has experienced a relapse?
Ask what they would like to do differently and what other things they would like to try.
What is the importance of celebrating tiny successes in behavior change?
Celebrating small wins reinforces positive behavior and builds confidence.
How can you affirm a patient's current knowledge during a conversation?
By acknowledging what they already know before providing additional information.
What is the purpose of asking permission before giving advice?
It respects the patient's autonomy and encourages engagement in their care.
What is the significance of customizing a plan that fits a patient's routine?
It increases the likelihood of adherence and success in behavior change.
What is the role of a healthcare provider in motivational interviewing (MI)?
To plant a gentle seed of dissonance that encourages the patient to return for resolution.
How can incremental goals benefit the process of change in MI?
They provide small, progressive accomplishments that build self-efficacy in the change.
What is a critical aspect of communication in motivational interviewing?
Voice tone and non-verbal signals are critical.
What should a healthcare provider encourage a patient to do before offering their own ideas for change?
Ask the patient to verbalize their own ideas for how they can change.
What is the recommended approach when a patient has a knowledge deficit?
1. Ask what they know, 2. Affirm that, 3. Ask permission to fill in the blanks, 4. Provide the information.
What does it mean to preserve a patient's 'FACE' in MI?
It refers to making efforts to maintain the patient's dignity and self-esteem during the conversation.
Why is considering the time factor important in motivational interviewing?
Efficiency is crucial to ensure that the conversation is productive and respects the patient's time.
Who are the authors of the book 'Motivational Interviewing in Health Care'?
Rollnick S, Miller W, Butler C.
What is the focus of the book 'Health Behavior Change: A Guide for Practitioners'?
It provides guidance for practitioners on facilitating health behavior changes.
What is the title of the 3rd edition book by Miller and Rollnick on motivational interviewing?
Motivational Interviewing: Preparing People for Change.
What type of study did DiIorio et al. conduct regarding motivational interviewing?
A randomized controlled study to promote adherence to antiretroviral medications.
What is the main finding of Burke et al.'s meta-analysis on motivational interviewing?
It assesses the efficacy of motivational interviewing across controlled clinical trials.
What does the systematic review by Knight et al. focus on?
Motivational interviewing in physical health care settings.
What is the significance of the study by Ogedegbe et al. regarding MI?
It evaluates the effect of motivational interviewing on medication adherence in hypertensive African Americans.
What was the focus of the systematic review by Rubak et al.?
A systematic review and meta-analysis of motivational interviewing.
What does the study by Dunn et al. review?
The use of brief interventions adapted from motivational interviewing across behavioral domains.