Lecture 33: Introduction to the human microbiota and barriers to infection
1/28
Earn XP
Description and Tags
microorganisms are present on almost all of our body surfaces which are collectively called the microbiome
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
what is the microbiota?
groups of micro-organisms living in a specific environment
develops at birth
usually not harmful and are needed for health
each individuals microbiota is unique depending on their age, diet, lifetyle
what are indigenous human commensals?
bacteria that naturally lives inside the human body without causing any harm
beneficial for bacteria and the host
provides some protection against pathogens (no space for pathogens to grow)
what is the gut microbiome used for?
essential for breakdown of our food
synthesise essential vitamins B12 and k
research suggests its also involved in obesity, allergies, mental health and immune disorders
how can indigenous human commensals act as opportunistic pathogens? give examples
can cause harm when disturbed, all only cause harm during these conditions
Burns patient: Pseudomonus aeruginosa
colonic bacteria: UTI, E.coli (gram -ve)
skin flora: wound infection- staphylococcus sp. (gram +ve)
oral flora: tooth decay- streptococcus sp.(gram +ve)(bacteria imbalance in mouth)
how is the human microbiota involved in the skin?
3 microenvironments:
dry skin(arms and legs)
moist skin(armpits)
areas rich in sebaceous glands
more moist = more bacteria
thick peptidoglycan wall making it resistant to drying
They have natural G+ colonisers of bacteria
staphylococcus and streptococcus
don’t usually cause disease but skin wound can lead to infection (staphylococcus aureus)
what is MRSA?
Methicillin-resistant staphylococcus aureus
antibiotic resistant
how is the microbiota involved in the upper respiratory tract?
Nose and throat
moist and aerobic so it has extensive bacterial flora(lots of natural colonisers)
Natural colonisers:
streptococcus and staphylococcus
Streptococcus pneumoniae and others are usually found in the back of the throat and dont cause problems but can cause bacterial meningitis
how is the microbiota involved in the lower respiratory tract?
Lungs
usually sterile and we dont want bacteria there
common site of infection
streptococcus can cause pneumonia
mycobacterium tuberculosis can cause tuberculosis
most common infections here
how is the microbiota involved in the mouth(oral cavity)?
complex microbial ecosystem LOTS of bacteria
Gingival groove(teeth+gums)- anaerobes - cause gum disease
Tooth enamel- facultative aerobes - some cause plaque and tooth decay - Streptococcus
cheeks and gums- facultative aerobes - some colonise saliva - Streptococcus(microaerophile)
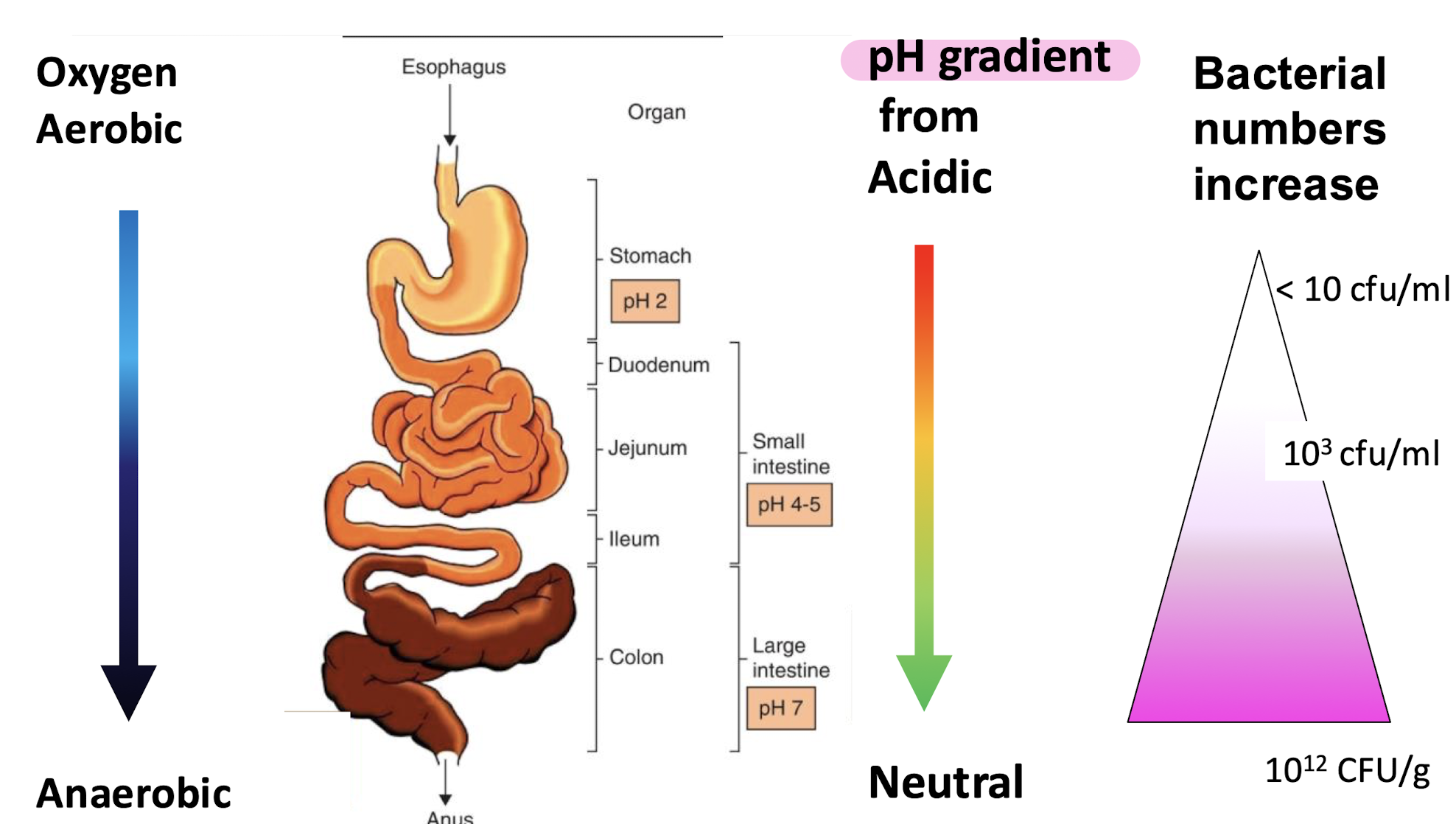
how is the microbiota involved in the digestive system?
STOMACH: least amount of bacteria
Acidic with lots of enzymes
helicobacter pylori lives in acidic conditions and causes stomach ulcers
SMALL INTESTINE:
duodenum has less bacteria as still acidic with enzymes
illeum less acidic with more bacteria
LARGE INTESTINE:
microbiome exists here
gram +ve and -ve
anaerobes and facultative anaerobes
Enterococcus faecalis causes bloodstream infections
has E COLI
how is the microbiota involved in the urinary tract?
kidneys, ureters and bladder are usually sterile as it can cause kidney infections
urethra is lighyl colonised by staphylococcus epidermidis
frequent site of UTI infections due to Escherichia coli
how is the microbiota involved in the adult female genital tract?
complex microbiota
depends on age, childbirth, menopause and menstrual cycle
usually acidic
Lactobacillus stops other infections growing
Candida albicans is a yeast which when overgrown needs antibiotics(thrush)
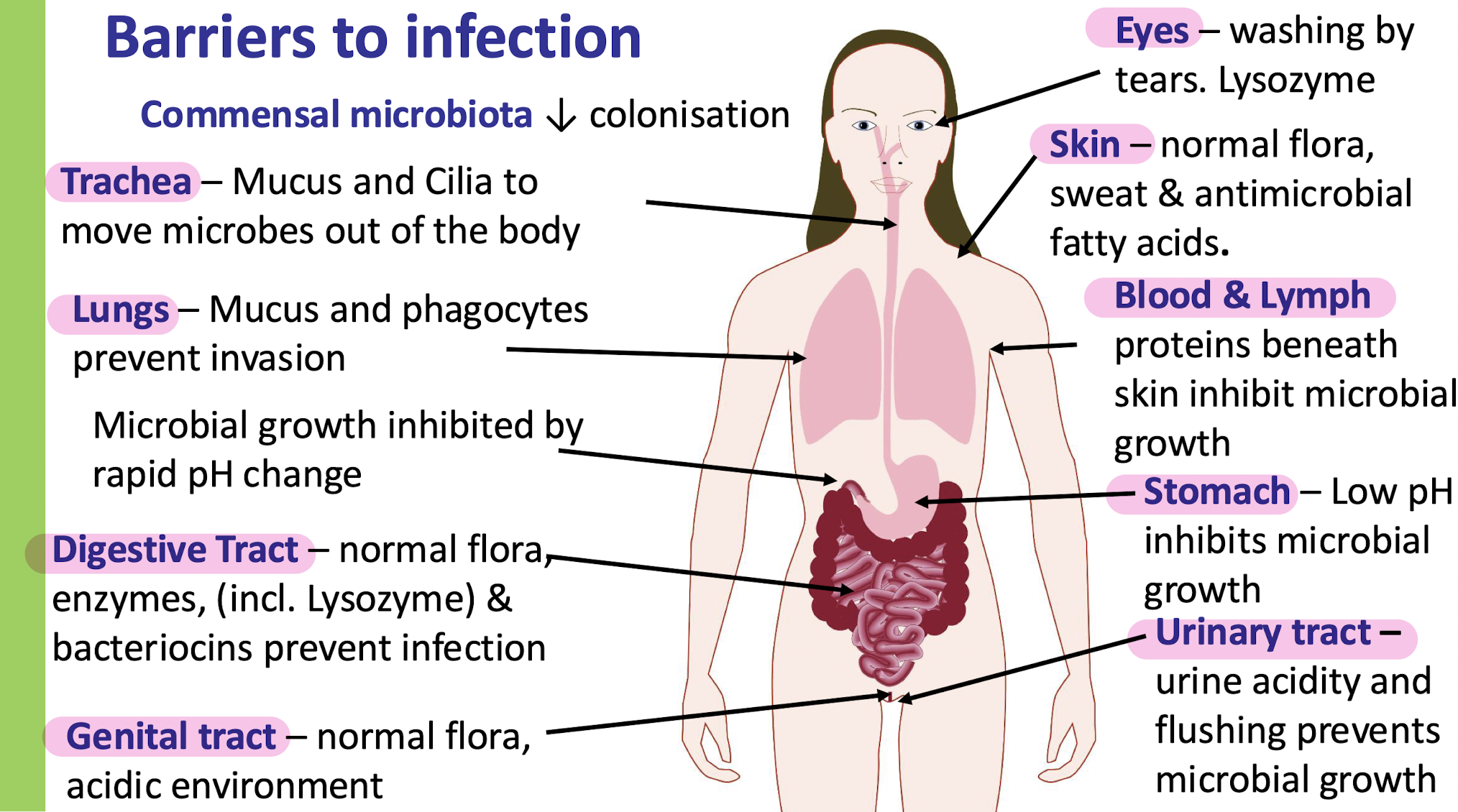
what are the non-specific defences against infection
indigenous microbiota
barriers: skin, mucosal surface, blood and tissues
commensals: the pathogen must compete with natural microflora for adhesion sites and food
what can be taken to support gut microbes?
PROBIOTICS:
live microorganisms that prevent/treat conditions
recolonise good bacteria
PREBIOTICS:
chemicals that induce growth/activity of microorganisms
promote health
both havent undergone clinical trials and are sold as food supplements
how is the epidermis a defence of the skin?
physical barrier
dry, acididc
shedding cells to prevent bacteria that penetrate to get further
indigenous bacteria therefore less colonisation
how is the sweat gland a defence of the skin?
has lysozyme
how is the sebaceous gland a defence of the skin?
(associated with hair follicles)
lysozyme breaks down peptidoglycan cell wall and gram +ve cell walls in bacteria
how is the skin associated lymphoid tissue(SALT) a defence of the skin?
induces local inflammatory response
How is mucus a defence of the mucosal surfaces?
traps bacteria
produces mucin
lysozyme kills G +ve bacteria
lactoferrin binds to iron and moves free iron around so bacteria wont use it
lactoperoxidase kills bacteria
How is epithelium a defence of the mucosal surfaces?
physicaly barrier
shedding cells
cilia
indigenous bacteria decreases colonisation
How is mucosal associated lymphoid tissue(MALT) a defence of the mucosal surfaces?
induces local inflammatory response if bacteria gets that far
what are all the barriers to infection
Trachea
Lungs
digestive tract
genital tract
eyes
skin
blood and lymph
stomach
urinary tract
what are the non specific defences of the blood and tissue?
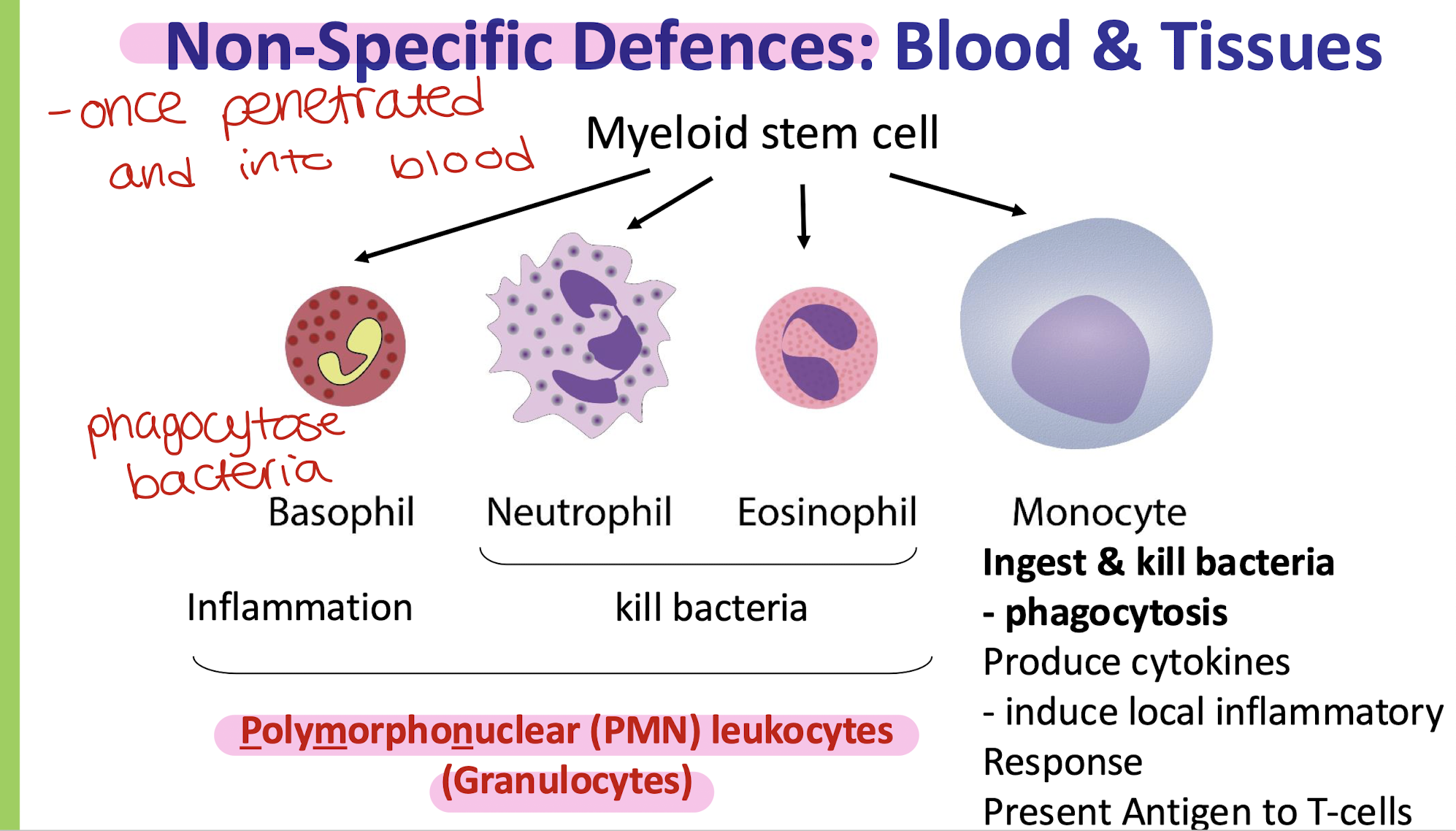
what cells do phagocytosis and what happens during?
Monocytes, Macrophages and Neutrophils
bacteria is identified and it adheres
bacteria is ingested and then lysozyme fuses with the vesicle and forms a phagolysosome
bacteria is digested and then discharged
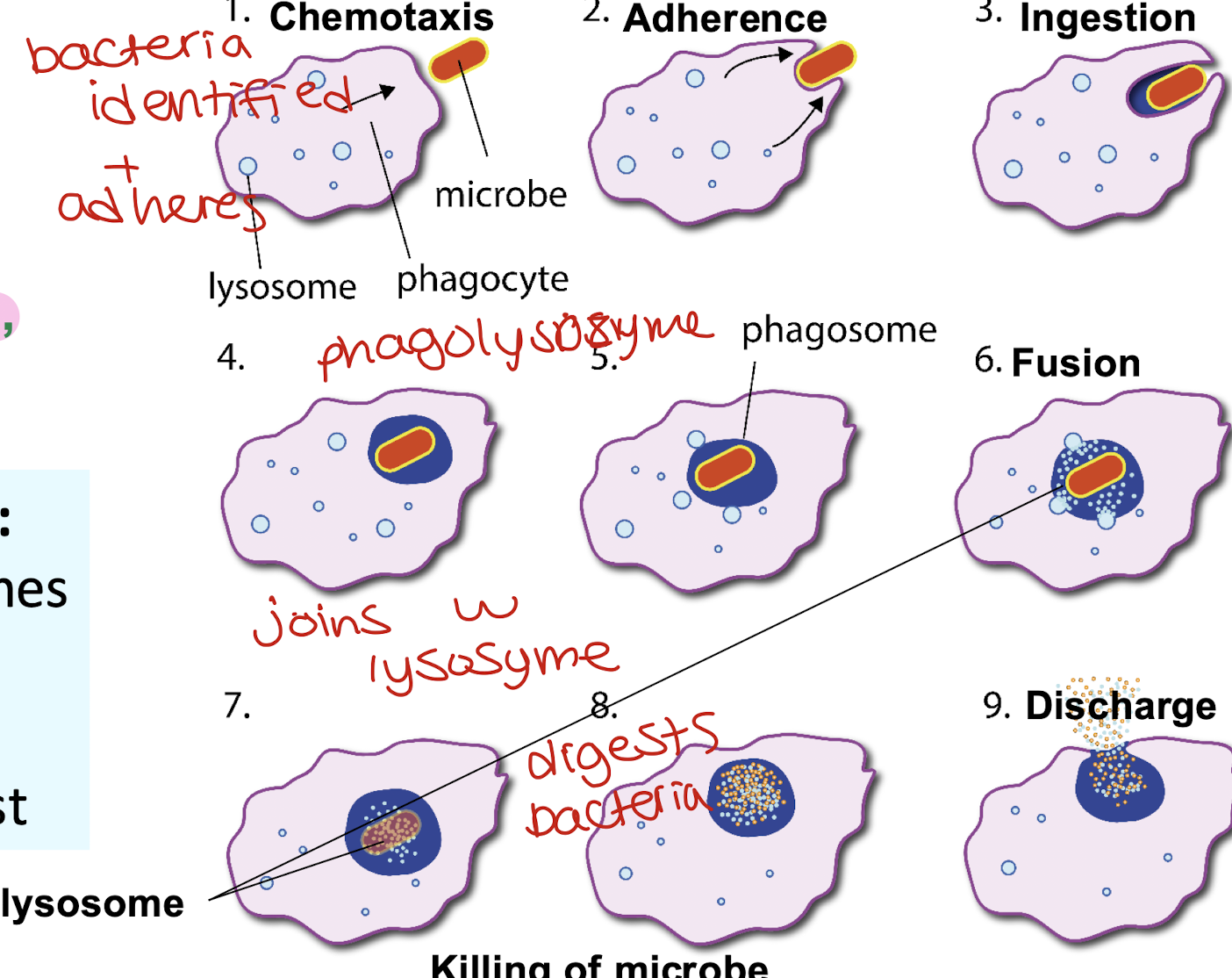
what do lysosomes contain?
digestive enzymes
defensins
enzymes of respiratory burst
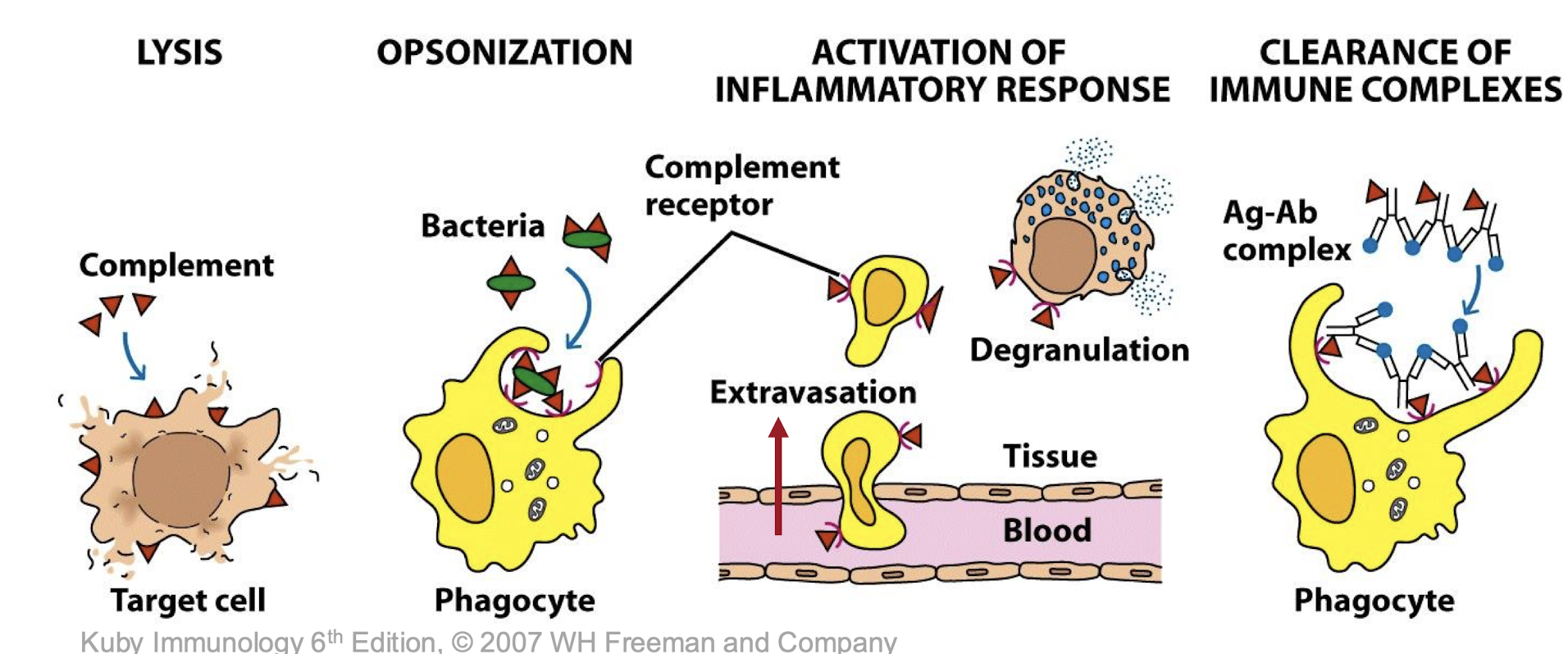
what is the complement system?
a biochemical cascaed involving more than 30 proteins in the blood and tissues which is activated following infection
Destroy pathogens (e.g., bacteria, viruses)
Mark pathogens for destruction (opsonization)
Recruit immune cells to sites of infection (inflammation)
Help antibodies and phagocytic cells clear microbes and damaged cells
what is mannose binding lectin?
a soluble factor produced following infection by the liver
it binds to patterns on microbial surfaces not specific antigens( structures it recognises )
increases complement activation and increases opsonisation
positive feedback
rewatch bit