10. β-Lactams/Cell Wall Synthesis Inhibitors
1/62
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
Describe β-lactam antibiotics.
Widely prescribed
All share common structure and mechanism of action (inhibition of bacterial cell wall synthesis)
Bactericidal
List β-lactam drugs.
Penicillins
Cephalosporins
Monobactams
Carbapenems
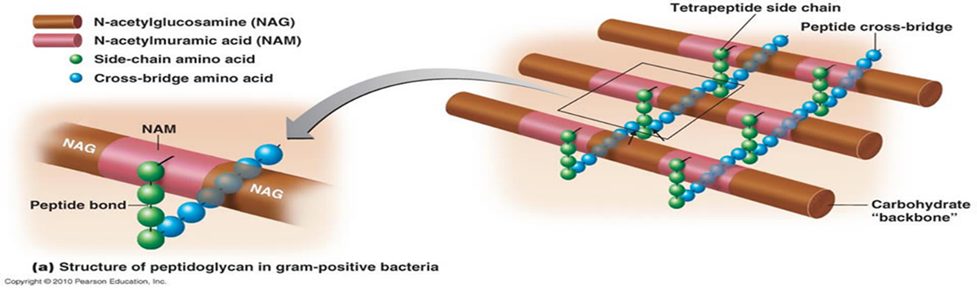
Describe the mechanism of action of β-lactams.
Bacteria do not have mechanism to regulate osmolarity; surrounded by thick cell wall that provides stability and rigidity to cell structure
Inhibit cell wall synthesis by inhibiting transpeptidases so that cross linking does not take place
Also activate autolysing enzymes (autolysins) that cause cell death
Penicillins
Where are pencillins obtained from?
Penicillium notatum
Penicillium chryosogenum
Penicillins
What is the role of the side chain on penicillins?
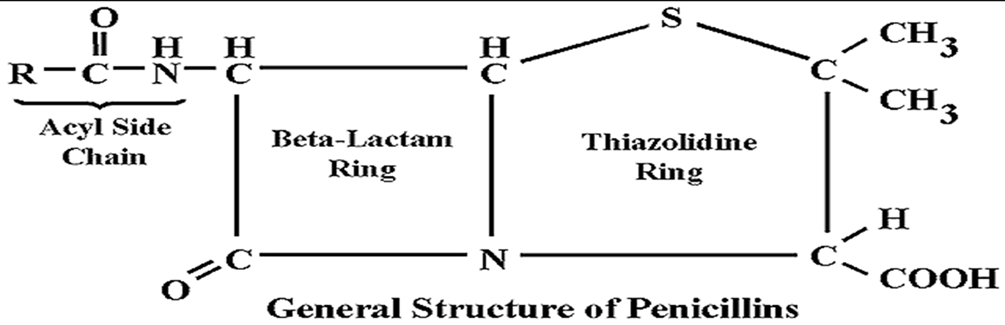
Provides antibacterial activity and stability
Penicillins
List the classifications of penicillins.
Natural
Semi-synthetic
Beta-lactamase inhibitors
Penicillins
List natural penicillins.
Penicillin-G
Penicillins
List semisynthetic penicillins.
Acid resistant (alternative to Penicillin-G): Penicillin-V
Penicillinase resistant: Methicillin, Cloxacillin
Extended spectrum: Ampicillin, Amoxicillin, Piperacillin
Penicillins
List beta-lactamase inhibitors.
Clavulanic acid
Sulbactam
Tazobactam
Penicillins
The renal tubular secretion of penicillins by __________ (anti-gout drug), a drug that competes with penicillins for the organic acid ___________ located in the ________ tubule. __________ has been used to slow down the _________ and prolong the ____-____ of penicillin G.
probenecid
transporter
proximal
Probenecid
excretion
half-life
Penicillins - Natural
Penicilin-G (PnG) are ______ spectrum penicillins and are β-lactamase _________.
narrow
sensitive
Penicillins - Natural
Describe the uses of penicillin-G.
Drug of choice for infections caused by organisms susceptible to it, unless patient is allergic
Use declined very much - fear of causing anaphylaxis
Penicillins - Natural
Which bacterial infection is penicillin-G the drug of choice for and why?
Treponema pallidum (causes syphilis); has not shown any resistance
Penicillin-G (Natural)
List the adverse effects of penicillin-G.
Pain at IM site
Hypersensitivity reactions (major problem with penicillins, 1-10% incidence)
Semisynthetic Penicillins
Why were semisynthetic penicillins synthesized?
To overcome shortcomings of PnG
What are penicillinase enzymes/β-lactamase enzymes?
Enzymes produced by some bacteria to provide resistance to antibiotics (open the ring)
Penicillin-V
Describe Penicillin-V.
Narrow-spectrum
β-lactamase sensitive
Antibacterial spectrum is similar to PnG
Penicillin-V
List the uses of Penicillin-V.
Streptococcal pharyngitis
Sinusitis
Otitis media
Prophylaxis of rheumatic fever
Less serious pneumococcal infections
List some bacteria that produce β-lactamase, which inactivate the β-lactam ring and hydrolyze penicillins.
S. aureus
H. influenzae
E. coli
Which bacteria can hydrolyze penicillins and cephalosporins?
Pseudomonas
Neisseria gonorrhoeae
Name 2 penicillinase/β-lactamase resistant penicillins.
Cloxacillin
Methicillin
β-lactamase-resistance penicillins protect the β-lactam ring from attack by _______________ _____________.
staphylococcal penicillinase
Describe methicillin.
Not used; nephrotoxic (causes interstitial nephritis)
Only used in lab tests to identify resistant strains of S. aureus (Methicillin Resistant S. aureus, MRSA)
Which penicillins are S. aureus resistant to?
Methicillin, Cloxacillin, Nafcillin
Describe MRSA.
Currently source of serious community and nosocomial infections
Is resistant to most commercially available β-lactam antibiotics
Penicillinase-resistant penicillins have minimal to no activity against
gram-negative infections
List extended spectrum penicillins.
Ampicillin
Amoxicillin
Piperacillin (Antipseudomonal)
Ticarcillin (Antipseudomonal)
Extended Spectrum Penicillins
Describe ampicillin and amoxicillin.
Acid stable
Given orally
Penicillinase/β-lactamase sensitive; hence used w/β-lactamase inhibitors
Extended Spectrum Penicillins
List the uses of ampicillin and amoxicillin.
Respiratory tract infections
Meningitis
Gonorrhea
Cholecystitis
Extended Spectrum Penicillins
Amoxicillin is used in multidrug regimens for eradication of
H. pylori in ulcers
Extended Spectrum Penicillins
List the adverse effects of ampicillin and amoxicillin.
Diarrhea
GI irritation
Rashes (up to 10%)
Hypersensitivity
Extended Spectrum Penicillins
Which is preferred between amoxicillin and ampicillin and why?
Amoxicillin
Better oral absorption
Food does not interfere with absorption
Less diarrhea
Extended Spectrum Penicillins - Antipseudomonal
List the uses of piperacillin and ticarcillin.
Active against gram-positive and gram-negative bacteria
Used for serious infections due to Pseudomonas, Proteus in burns
Septicemia
UTI
Neutropic/immuno-compromised patients with serious gram-negative infections
Usually combination of piperacillin with gentamycin/tobramycin is preferred
Define and describe β-lactamase.
Family of enzymes produced by Gram-positive and Gram-negative bacteria that inactivate β-lactam antibiotics
Different β-lactamases differ in their substrate affinities
List β-lactamase inhibitors.
Clavulinic acid
Sulbactam
Tazobactam
They do not possess any antibacterial action
Describe the mechanism of β-lactamase inhibitors.
Bind irreversibly to catalytic site of susceptible β-lactamase (produced by bacteria) to prevent hydrolysis of penicillins
Based on their pharmacokinetic features, which β-lactamase inhibitors are combined with each other and why?
Clavulanic acid is combined with amoxycillin (Augmentin)
Addition of clavulinic acid with amoxycillin extends the antimicrobial spectrum of amoxycillin against β-lactamase producing enzyme
Sulbactam with ampicillin
Tazobactam with pipercillin
List the uses of β-lactamase inhibitors.
Skin and soft tissue infections
Intra-abdominal and gynecological sepsis
Urinary, biliary and respiratory tract infections
Gonorrhea
Used when empiric antibiotic therapy is to be given for hospital acquired infections
List the adverse effects of β-lactamase inhibitors (clavulanic acid).
Rare except GI intolerance esp. in children
Stomatitis
Rashes
Same for amoxycillin alone
Describe cephalosporins.
Semi-synthetic antibiotics derived from “Cephalosporin-C” obtained from fungus Cephalosporium
All are bactericidal
Similar to penicillins in mechanism of action and adverse effects
Describe the mechanism of action of cephalosporins.
Inhibition of transpeptidation process, leading to formation of imperfect cell wall
Bind to different proteins than those which bind penicillins; may explain differences in spectrum, potency, and lack of cross-resistance
Describe and list the classifications of cephalosporins.
Classified into generations based on antibacterial spectrum, stability to β-lactamase, and year of introduction
First generation
Second generation
Third generation
Fourth generation
Fifth generation
List first generation cephalosporins.
Cephalexin and Cefadroxil
List second generation cephalosporins.
Cefaclor and Cefuroxime
List third generation cephalosporins.
Ceftriaxone and Cefpodoxime
List fourth generation cephalosporins.
Cefepime and Cefpirome
List fifth generation cephalosporins.
Ceftaroline and Ceftobiprole
First Generation Cephalosporins
Describe first generation cephalosporins and list their uses.
Developed in 1960s
High activity against Gram-positive but weaker against Gram-negative bacteria
UTI
Minor Staphylococcal infections
Soft tissue abscesses
First Generation Cephalosporins
Which is the most commonly used first gen drug and which one is preferred for surgical prophylaxis/prophylaxis against infection?
Most commonly used: cephalexin
Surgical prophylaxis: cefazolin
Second Generation Cephalosporins
Describe second gen cephalosporins.
More effective against Gram-negative bacteria, with some members active against anaerobes as well
Second Generation Cephalosporins
Describe cefuroxime.
Resistant to Gram-negative β-lactamase
Has high activity against organisms producing these enzymes, including penicillin-producing Neisseria gonorrhea (PPNG) and ampicillin-resistant H. influenza and Klebsiella pneumonia
Second Generation Cephalosporins
List the uses of second gen cephalosporins.
Gonorrhea due to PPNG
URTI
Community acquired pneumonia
Meningitis (3rd gen preferred)
Anaerobic infections e.g. lower abdominal and gynecological infections
Third Generation Cephalosporins
Describe third gen cephalosporins.
Introduced in 1980s
Have highly augmented activity against Gram-negative cocci, bacilli, and anaerobes
All highly resistant to β-lactamases from Gram-negative bacteria; less active on Gram-positive cocci and anaerobes
Cross BBB, so provides adequate therapeutic levels in CSF
Third Generation Cephalosporins
How is ceftriaxone excreted? What is the significance of this?
In bile
No dose adjustment required for renal insufficiency
Third Generation Cephalosporins
List the uses of third gen cephalosporins.
Meningitis
Life-threatening/hospital-acquired infections
Gonorrhea
Septiciemias
Infections in immuno-compromised patients
Fourth Generation Cephalosporins
Describe fourth generation cephalosporins.
Developed in 1990s
Antibacterial spectrum is similar to third generation
Widest antibacterial spectrum - Gram-positive activity of first gen. and Gram-negative activity of third gen.
Highly resistant to beta-lactamase, thus active against many bacteria resistant to earlier drugs
P. aeruginosa and S. aureus are also inhibited, but not MRSA
Fourth Generation Cephalosporins
Which infections are fourth gen cephalosporins effective in and why?
Due to its high potency and extended spectrum, it is effective in many serious infections:
hospital-acquired pneumonia
febrile neutropenia
bacterima
septicemia
Fifth Generation Cephalosporins
List the parenteral fifth generation cephalosporins that are currently undergoing clinical trials.
Ceftaroline and Ceftobiprole (cleared Phase III clinical trials)
Fifth Generation Cephalosporins
Describe ceftaroline.
Is the only commercially available β-lactam with activity against MRSA
Is indicated for treatment of complicated skin and skin structure infections and community-acquired pneumonia
List the adverse effects of cephalosporins.
Pain after IM injection
Diarrhea
Hypersensitivity reactions (lower than penicillins): skin rash, fever, eosinophilia
Nephrotoxicity: used in combination with aminoglycosides
Bleeding/coagulation abnormalities: reduces synthesis of Vitamin K-dependent clotting factors (treatment for this is Vitamin K)
Superinfections, pseudomembranous colitis (PMC), and diarrhea can result from use of 3rd, 4th, and 5th gens
List another inhibitor of cell wall synthesis.
Vancomycin
Describe vancomycin.
Damages cell membrane and alters cytoplasmic membrane permeability (bactericidal)
Exclusively acts against aerobic and anaerobic Gram-positive species, including drug-resistant Gram-negative bacteria, MRSA, penicillin-resistant S. pneumoniae, S. enterocolitis, and S. endocarditis
List the adverse effects of vancomycin.
Red-neck syndrome (histamine release, given as slow IV)
Minor incidences of ototoxicity
Nephrotoxicity
Skin rash
Fever
Chills