Week 7 (Liver & Spleen/Wound Healing & Hernia)
1/205
Earn XP
Description and Tags
1-99 liver/spleen,
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
206 Terms
What are the lobes of the liver?
- Left lateral (very large)
- Left medial
- Quadrate
- Right medial
- Right lateral
- Caudate (caudate process and papillary process which extends to the left side)
What are the ligaments of the liver?
- Coronary ligament
- Triangular ligaments (two right, one left)
- Hepatorenal ligament (liver to right kidney; minimizes visualization of right adrenal gland)
- Hepatogastric ligament (Delineates pylorus or very close to pylorus)
- Hepatoduodenal ligament
Where is the gall bladder located?
- Between right medial and quadrate
The hepatogastric ligament can be a useful landmark for what?
- Delineating the pylorus; useful for gastropexy
It is more difficult to perform a lobectomy on which side of the liver?
- Right
Describe the blood supply to the liver.
- Hepatic artery: 20% blood volume; 50% oxygenated blood
- Portal vein: 80% blood volume, 50% oxygenated blood
The hepatic artery is a branch of what?
- Celiac artery
What vessels drain into the portal vein?
- Caudal mesenteric vein
- Cranial mesenteric vein
- Splenic vein
- Gastroduodenal vein
The portal vein branches how in the liver in the dog?
- Right → right lateral and caudate
- Left → Central (right medial and caudate), left lateral, left medial, and quadrate
The portal vein branches how in the liver in the cat?
- Right
- Central
- Left
Describe the drainage of the liver vasculature.
- 6-8 hepatic veins drain into the CaVC
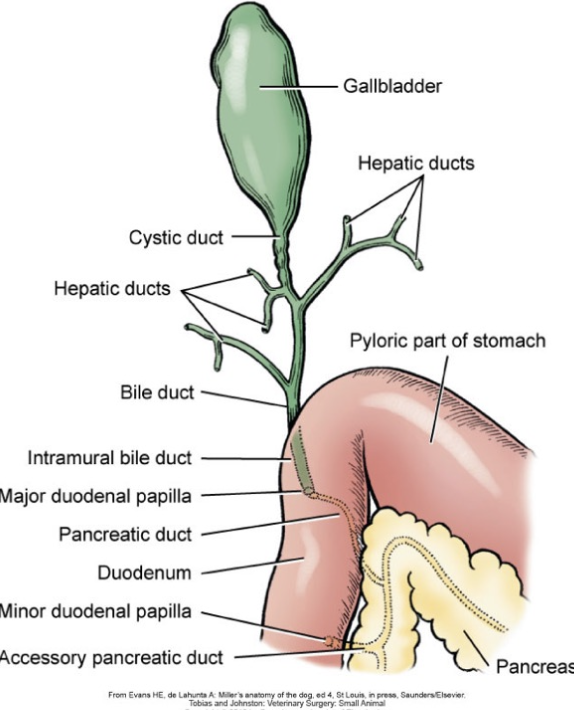
Describe the flow of bile.
Canaliculi → interlobular ducts → lobar ducts → hepatic ducts, exit liver parenchyma → common bile duct (Cystic duct to gallbladder)
Describe the common bile duct in the dog vs. cat.
- Dogs: Enters duodenum adjacent to the pancreatic duct at the major duodenal papilla
- Cats: Pancreatic duct joins the common bile duct and enters duodenum at major duodenal papilla (Only 20% have an accessory pancreatic duct)
What are some physiologic roles of the liver?
- Protein metabolism
- CHO metabolism
- Coagulation factor synthesis (all except VIII and vWf)
What are the vitamin K dependent clotting factors?
- II, VII, IX, X, protein C, protein S
What is the use of radiographs in liver assessment?
- Provide little specific information
- Can visualize choleliths which are 50% opaque in dogs and 80% opaque in cats
What is the appropriate diameter of the common bile duct on US?
- 3 to 4 mm
How can CT be used to evaluate the liver?
- CT angiography (arterial phase, portal phase, venous phase)
What are some pre-operative considerations for liver surgery?
- Hemorrhage (57% reported coagulopathies with liver disease, Blood typing, cross match, blood products)
- Hypoglycemia (Liver dysfunction, PSS and severe hepatopathy)
- Anesthesia (hepatic metabolism)
- Bacteria (Intestinal bacteria and endotoxin exposure; Broad spectrum ABX appropriate)
Biopsies are best taken on the ____________ surface of the liver.
- Diaphragmatic
What are options for liver biopsies?
- Guillotine
- Laparoscopic
- Punch
- Percutaneous Needle Core (US guided, difficult)
How is a guillotine liver biopsy performed? What lesions is it best for?
- Crush a region and place a suture around it (monofilament, PDS)
- Best for peripheral or generalized lesions
How is a laparoscopic liver biopsy performed?
- With 5 mm cup forceps and loop ligatures

What lesions are punch liver biopsies best for?
- Non-peripheral and targeted lesions
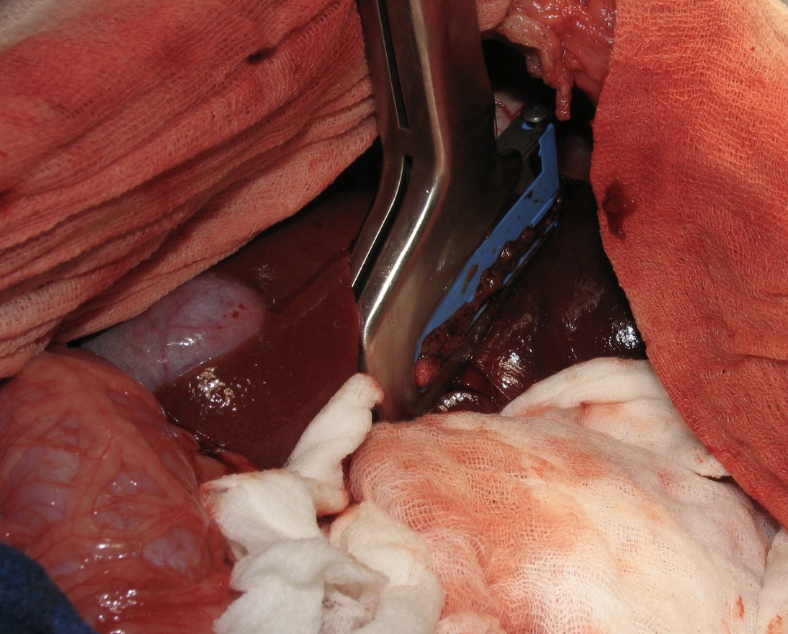
How is a partial liver lobectomy performed? Complete?
- Liver capsule transected, blunt dissection to ID large vessels
- Stapling devices
- Vessel sealant devices
Complete:
stapling devices
blunt dissection and suture ligation
Dogs can tolerate __________ acute liver removal.
- 70%
What amount of liver volume do the liver lobes constitute?
- Right lateral and caudate: 28%
- Right medial and quadrate: 28%
- Left lateral and medial: 44%
What are some causes of extrahepatic biliary obstruction common in cats?
- Complex inflammatory conditions (triaditis - pancreatitis, cholangitis, CIE)
- +/- neoplasia
What are some causes of extrahepatic biliary obstruction common in dogs?
- Pancreatitis
- Neoplasia
- Gall bladder mucoceles
- Cholangitis
- Cholelithiasis
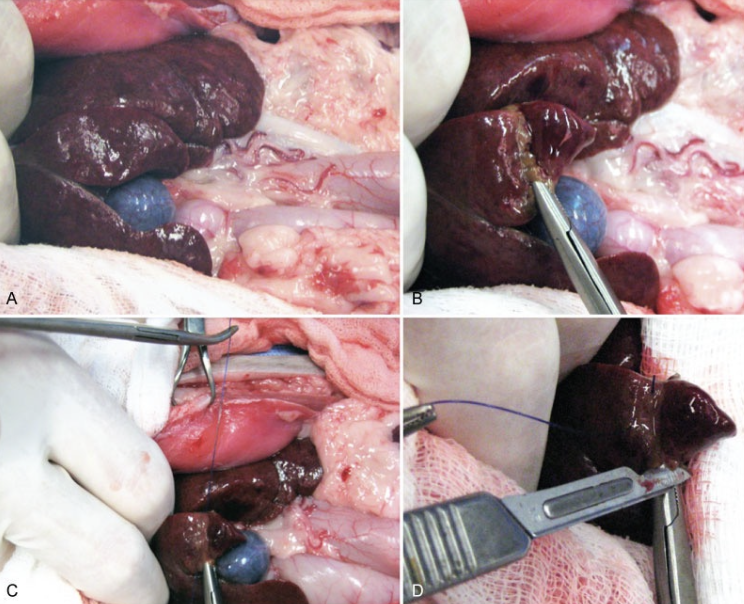
How are cholecystectomies performed?
- Ensure patency of CBD (bile needs to be able to get from liver to intestines)
- Dissect free from fossa
- Double ligate cystic duct
- Ligate cystic artery
How is the patency of the CBD assessed/maintained?
- Choledochal catheterization and stenting
- Catheterization can be normograde or retrograde (Incision into duodenum and threading through major duodenal papilla) and followed with flushing
- Stenting involves placing a red rubber in the CBD which is sutured to the duodenum aborally to the major duodenal papilla (the animal will poop it out with time)

What is a cholecystoenterostomy?
- Anastomosis of gall bladder to intestine to reroute biliary system, either to duodenum (preferred; Cholecystoduodenostomy) or jejunum (Cholecystojejunostomy)
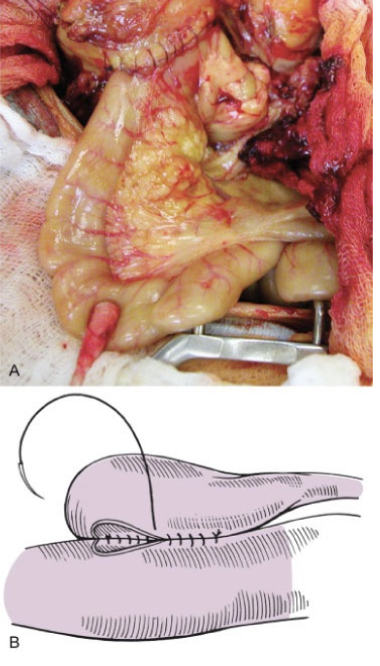
When performing a cholecystoenterostomy, a _________ is created as long as possible to avoid strictures.
- Stoma (2.5 cm)

What are complications of a cholecystoenterostomy?
- Dehiscence (septic bile peritonitis; mortality 75%)
- Stricture
- Ascending infection
- Ulceration
What are indications for a choledochotomy?
- Choleliths obstructing the CBD
- Ideally this procedure is avoided
What is a cholecystotomy tube?
- Temporary method to drain bile
- If this is needed, often just aspirate bile rather than doing this, but it can be performed (open or laparoscopic)
What is a gall bladder mucocele?
- Cystic mucosal hyperplasia resulting in hypersecretion of mucus and thick, gelatinous bile within the gall bladder which is generally sterile
- This can lead to obstruction and rupture
What animals are predisposed to gall bladder mucocele?
- Shetland Sheepdogs
- Dogs with HYPERadrenocorticism and HYPOthyroidism

How are gall bladder mucoceles diagnosed?
- Clinicopathologic abnormalities: Elevated bili, ALP, ALT, and AST
- US: Non-dependent echogenic material in a stellate pattern (looks like a kiwi)

How are gall bladder mucoceles managed?
- Medical management for early cases
- Surgical management with cholecystectomy (ensure CBD patency)
What is the prognosis for gall bladder mucoceles managed surgically?
- Better prognosis if not obstructed or showing clinical signs (i.e. "elective" type cases which involve normal bilirubin, have no obstruction or ductal distention, but have a mucocele -> mortality <5%)
True or false: Cholelithiasis is common
- False; Infrequent cause of clinically significant disease
What types of choleliths are more common in dogs?
- Pigment stones - calcium bilirubinate
What is the most common hepatobiliary neoplasia?
- Hepatocellular carcinoma
Describe the typical structure and biologic behavior of hepatocellular carcinomas.
- Massive (one large one - best), nodular (multiple nodules) or diffuse
- Metastases in local LN, lung, peritoneum
What is the treatment of choice for massive hepatocellular carcinomas? What is the MST?
- Surgical resection
- MST 1460 days (4 years) with clean margins
What are cholangiocellular neoplasias?
- Benign adenomas
- Malignant carcinomas
Describe the typical biologic behavior and structure of cholangiocellular carcinomas.
- Massive, nodular, diffuse
- Cats - Bile duct tumors 2x common as primary hepatic neoplasms
- Biliary cystadenomas 2x as common as bile duct carcinomas
What is the prognosis for malignant biliary tumors in cats?
- Poor
Describe hepatobiliary neuroendocrine tumors.
- Rare, usually diffuse
- Metastases in 90% of cases
- Poor prognosis
Describe hepatobiliary mesenchyma tumors.
- Common
- Often metastatic (HSA common)
- Prognosis generally guarded due to frequent metastases
What are some other potential metastatic neoplasms of the liver?
- MCT
- Histiocytic sarcoma
- Myelolipoma
True or false: Metastatic hepatic tumors are more common than primary hepatic tumors
- True
metastatic hepatic » primary hepatic tumor
Before performing a cholecystectomy, what must you ensure?
- Patent CBD, there must be a way for bile to get from liver to intestines - choledochal catheterization
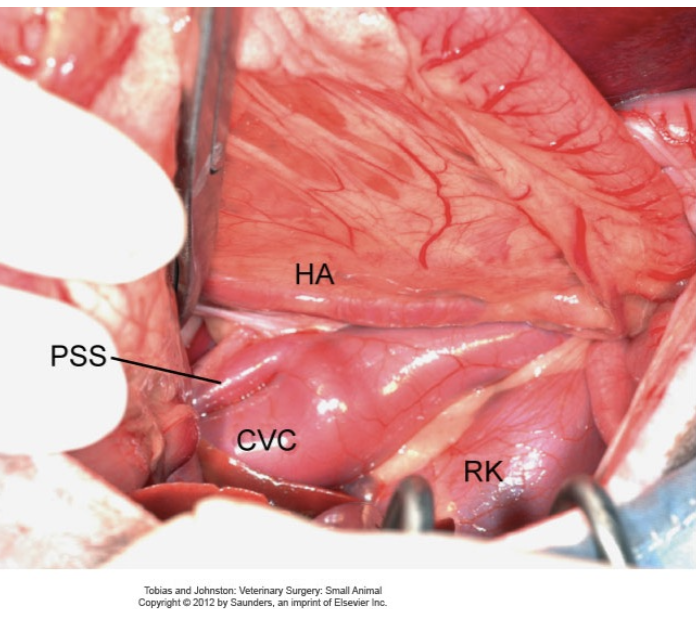
What are the types of portosystemic shunts?
- Congenital: Direct communication with the portal venous system and systemic circulation (bypasses liver) which are commonly single and can be intra- or extrahepatic
- Acquired: Secondary to chronic portal hypertension which are more commonly multiple, torturous and extrahepatic
Which type of portosystemic shunts are generally surgical?
- Congenital
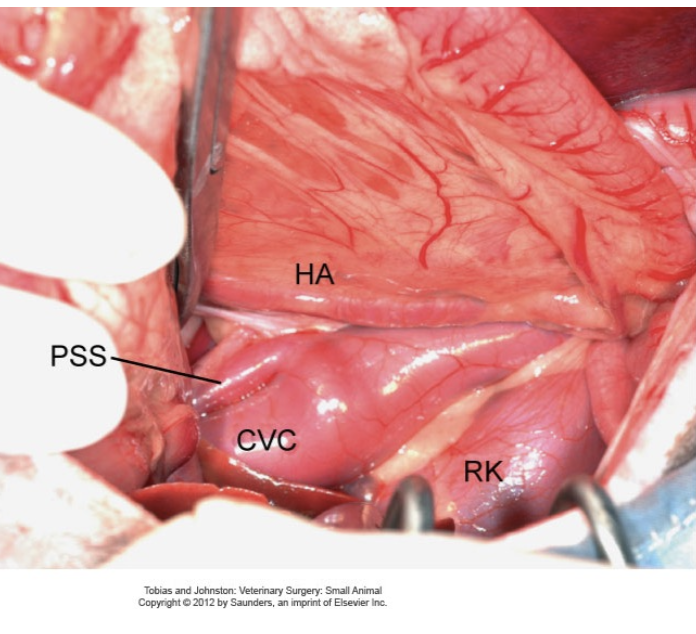
Describe the differences between extrahepatic and intrahepatic congenital PSS.
- Extrahepatic: 2/3 of PSS, more common in small breeds
- Intrahepatic: More common in large breeds with a larger volume of portal blood being shunted resulting in more severe clinical signs
What are clinical signs of a PSS?
- Neurologic (HE): Dullness, lethargy, head pressing, seizures, circling
- GI: Vomiting, diarrhea, anorexia, pica, ptyalism (cats)
- Urinary: Hematuria, pollakiuria, urinary obstruction
- Copper colored irises in cats

What signalment/history is typically associated with PSS?
- Chronic or acute illness
- Young age
- Failure to thrive
- Dullness/lethargy
- Bizarre behavior
- Anesthetic intolerance
- Incidental (BW, urolith analysis)
What CBC findings are associated with PSS?
- Microcytosis, non-regenerative anemia
- +/- leukocytosis
What biochemistry changes are associated with PSS?
- Hypoalbuminemia
- Hypocholesterolemia
- Hypoglycemia
- Decreased BUN
- +/- mild to moderate liver enzyme concentrations
What UA changes are associated with PSS?
- Decreased USG
- Ammonium biurate crystalluria
What is the test of choice for PSS?
- Bile Acids
- Increased due to shunting of reabsorbed bile acids into systemic circulation
What ammonia values are expected in patient with PSS and why?
- Elevated
- Primary source of blood ammonia is GIT; Conversion to urea in the liver does not occur efficiently, resulting in increased ammonia
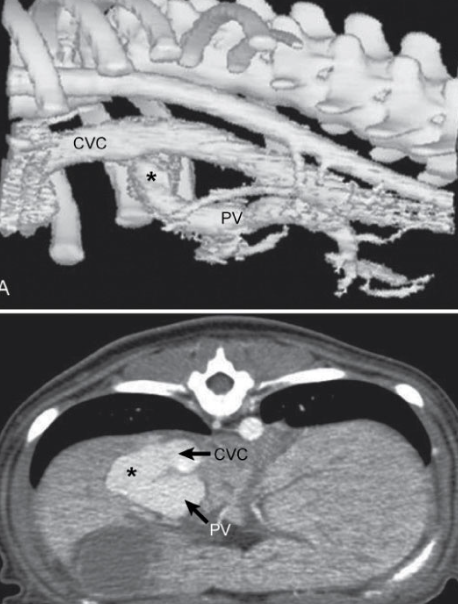
What imaging is available for PSS?
- AUS (User dependent, but can allow visualization of concurrent urinary abnormalities)
- Scintigraphy
- CT angiography (gold standard for humans (and at OSU), non-invasive, fast, imaging of all portal tributaries)
- Portovenography
- MRI (uncommon)
What are the two ways to administer scintigraphy?
1) Transplenic (preferred, lower dose)
2) Transcolonic
What is the typical flow of nuclear scintigraphy following administration? What about in cases of PSS?
- Spleen -> Liver -> Heart -> Body
- Spleen -> Heart -> Body -> Liver
When is portovenography performed? What veins are used?
- Intraoperatively
- Jejunal or splenic vein
What does portovenography indicate?
- Where shunt diverges from portal vein
- Extrahepatic - Caudal to 13th thoracic vertebrae
- Intrahepatic - Cranial to 13th thoracic vertebrae
What medical management of PSS is appropriate?
- Medical management recommended before surgery
- Lactulose (Acidifies colonic contents, traps ammonia, faster transit time)
- ABX (Neomycin, metronidazole, amoxicillin to decrease bacterial load in colon)
- Protein restricted (soy based) diet
- Leviteracetam to reduce risk of post-operative seizures
- Proton pump inhibitor or H2 blockers for intrahepatic shunts
What is the prognosis for PSS?
- Medical management survival 51% (MST 10 months with medical management alone)
- Surgical management survival 88%
What acute medical management is useful for PSS?
- IVF (with glucose) to correct electrolyte abnormalities
- Enemas - warm water with lactulose
- ABX
- Seizures: Keppra or propofol
- Anemia: Blood transfusion
What types of surgeries are preferred for PSS?
- Gradual occlusion (Ameroid constrictors or cellophane bands)
- NOT suture (less commonly used)
Describe the use of an ameroid constrictor.
- It has an inner ring of casein, a hygroscopic substance that swells as it slowly absorbs body fluid and reduces the inner ring diameter leading to thrombus formation of the vessel
- +/- outer ring of stainless steel

Describe the use of a cellophane band.
- Folded piece of cellophane which is secured with hemoclips
- Fibrous tissue reaction
- Gradual occlusion
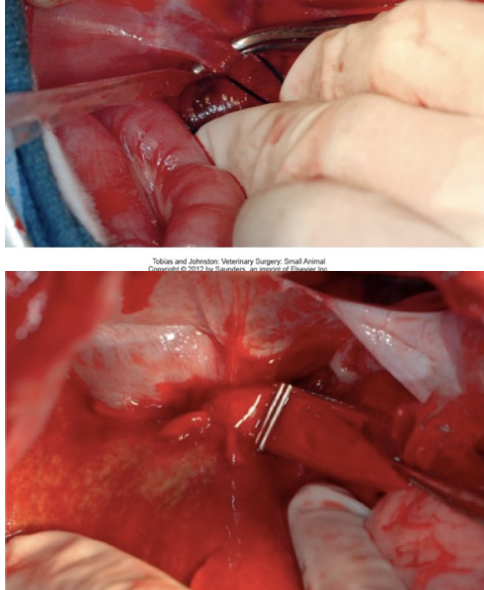
Where should gradual occlusion devices for PSS be placed?
- Close to the insertion site (systemic venous site) as there might be one large vessel, but there could another branch going into that shunt
If using suture for occlusion of PSS, what must also be done?
- Measure portal pressures (They can't change too much)
- Maximal portal pressure 17-24cm H20
- Maximal change in portal pressures 9-10cm H20
- Maximal decrease in central venous pressure 1cm H20
What should always be performed at the same time as surgical correction of a PSS?
- Biopsy of liver
- Assess for any grossly visible portal hypertension changes (cyanotic pancreas, hypermotile jejunum)
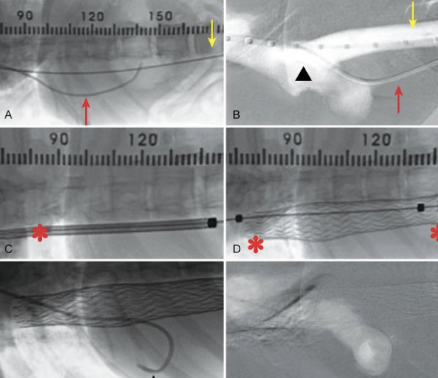
How are intrahepatic shunts managed?
- Minimally invasive with intravascular stents and coils (challenging, left easiest to surgically correct)
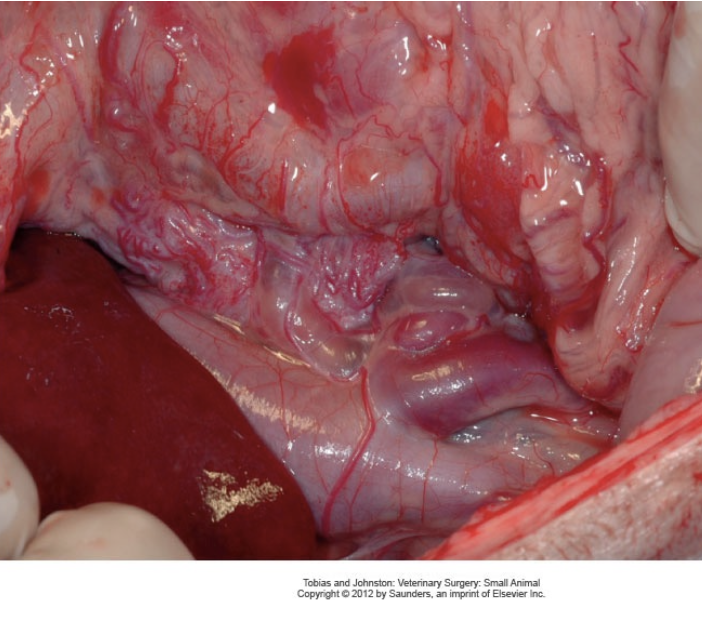
What are complications of PSS and their repairs?
- Hypoglycemia
- Hemorrhage and anemia
- Portal hypertension (hypovolemic shock, abdominal pain, abdominal distention, diarrhea, vomiting)
- Seizures and encephalopathy
- Recurrence of clinical signs
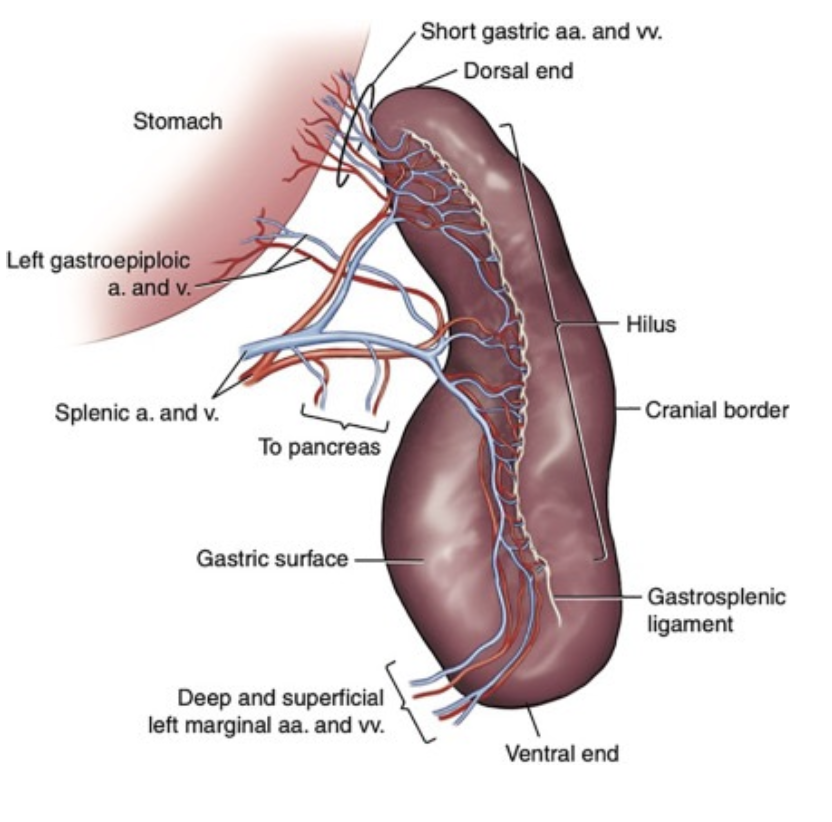
Describe the blood supply to the spleen.
- Splenic artery (two primary branches) arises from the celiac artery; has pancreatic branches to the left lobe of the pancreas (need to preserve these branches) and left gastroepiploic artery to the stomach (also try to preserve)
- Splenic vein drains to the portal vein (metastasis from spleen to liver is common)
- Short gastric arteries and veins shared with stomach
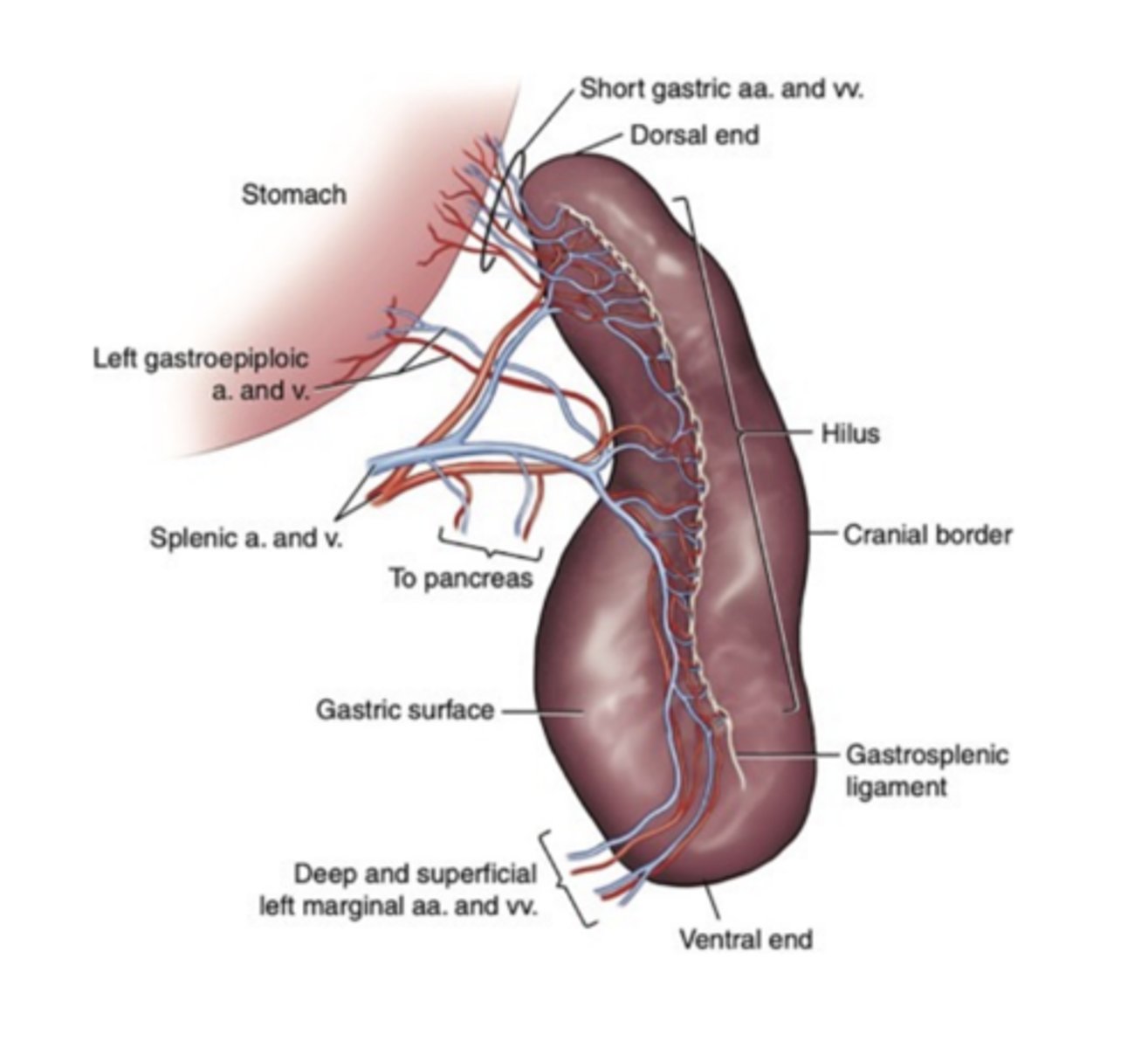
How can one find the splenic artery and pancreatic branches to the left limb of the pancreas?
- Under the superficial leaf of the greater omentum
What are functions of the spleen?
- Immune functions
- Erythrocyte maintenance
- RBC reservoir
- Extramedullary hematopoiesis
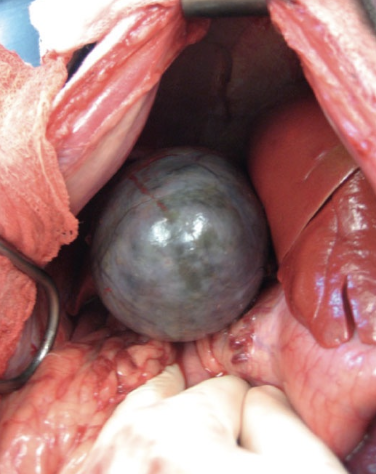
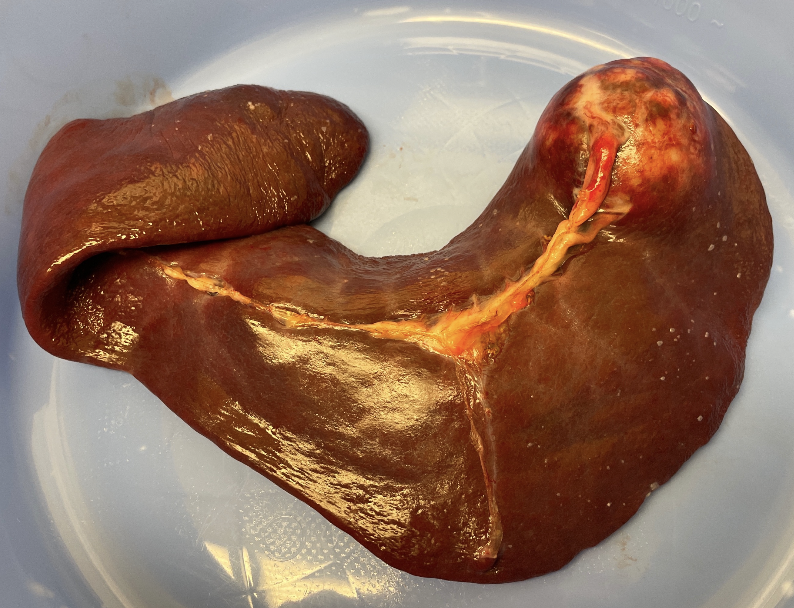
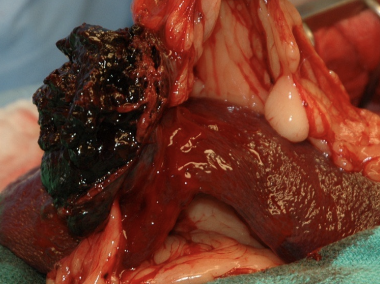
What is the structure of splenic masses?
- More commonly cystic/cavitated (malignant or benign)
- Less commonly solid
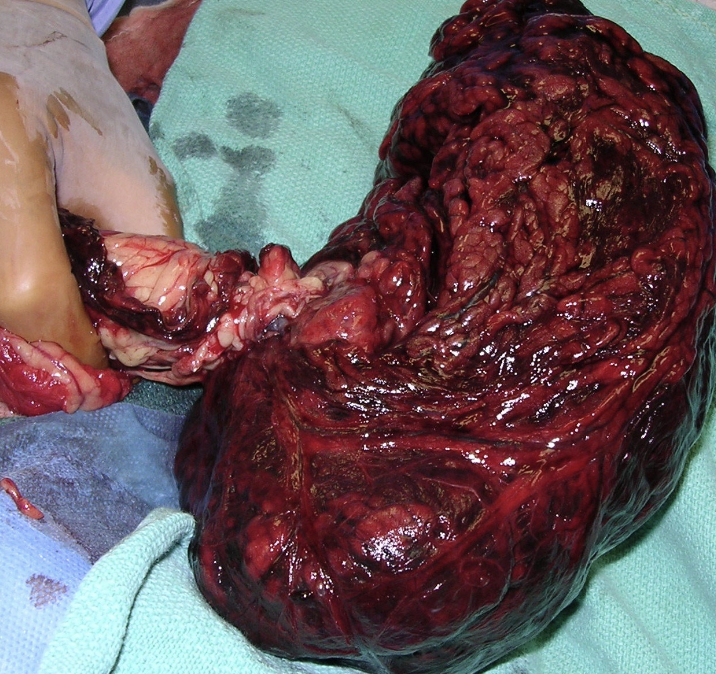
In large breed dogs with non-traumatic hemoabdomen and a splenic mass, 63-80% are malignant or benign? In dogs without a non-traumatic hemoabdomen and a splenic mass, almost the opposite is true with ~60% being ___________.
- Malignant
- Benign
True or False? Spelenectomy is indicated in either malignant or benign masses.
True, regardless of pathology, splenectomy is indicated. Do not venture a “guess” on pathology to owner
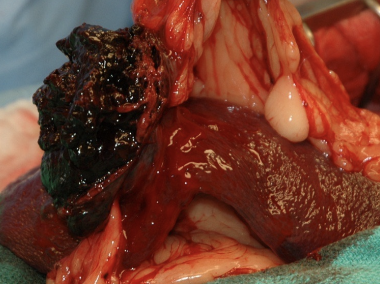
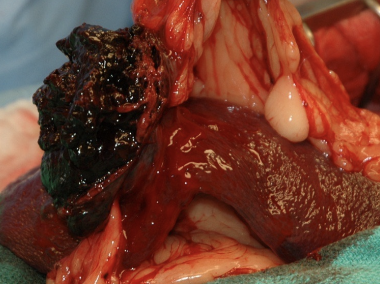
Splenic torsions can occur with what other pathology?
- GDV
- They can also occur independently
What is the typical clinical presentation of animals with a splenic torsion?
- May be acute or chronic
- Vague clinical signs when chronic: lethargy, inappetence, etc.
How are splenic torsions diagnosed?
- "C-shape" on R lat abdominal radiograph
- Best diagnostic: ultrasound w/ color flow doppler
What prophylactic procedure is recommended for large breed dogs with splenic torsion?
- Gastropexy
ALWAYS complete ___ first before splenectomy.
workup
What workup is recommended prior to a splenectomy?
- History and physical exam
- CBC/chem/UA
- Met check (3 view thoracic rads or thoracic CT scan)
What peri-operative ABX are recommended for a splenectomy?
- Cefazolin 22 mg/kg IV q90minutes in surgery
When performing a splenectomy, biopsy the ______________ if any lesions are present.
- Liver
Describe the "three(ish)" vessel technique for a splenectomy.
1) Short gastric artery and vein (treat them like an ovarian pedicle); Start here -> Improves mobility
2) Left gastroepiploic artery and vein (caudal/omental vessels)
3) Splenic artery/vein
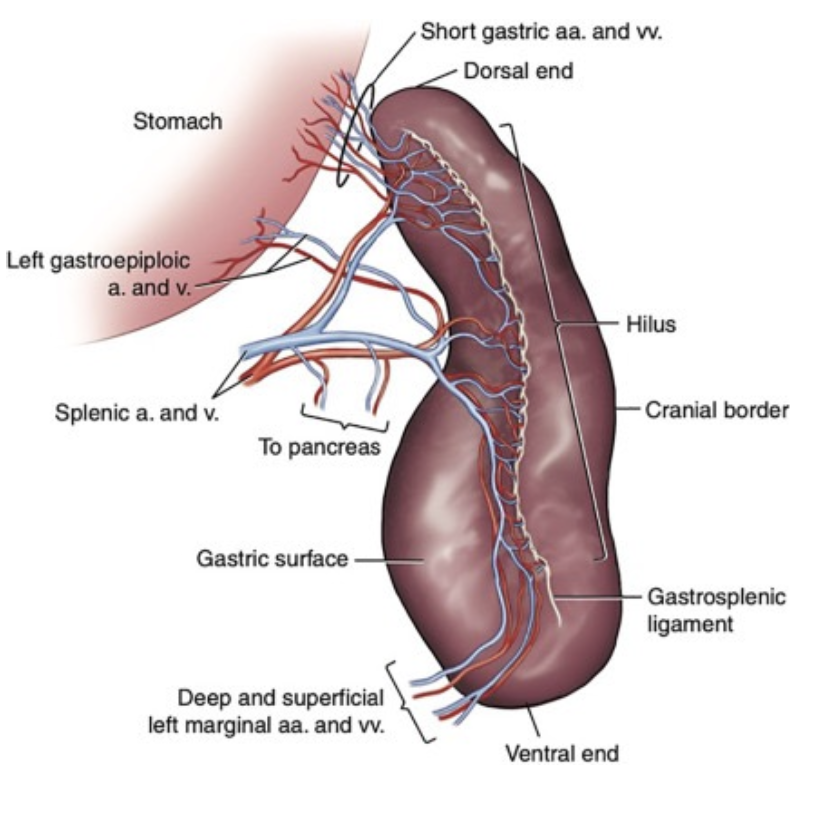
Describe Dr. T's 5 vessel technique for a splenectomy/
1) Short gastric artery and vein (treat them like an ovarian pedicle); Start here -> Improves mobility
2) Splenic artery/vein branch
3) Splenic artery/vein branch distal to left gastroepiploic
4) Splenic artery/vein adjacent to left gastroepoploic
5) Deep and superficial left marginal artery and vein
What are some potential post-operative complications for a splenectomy?
- Ventricular arrhythmias - 44% of dogs (often don't require Tx)
- Hemorrhage
- Tumor spread if malignant
- Pancreatitis
- GDV (Consider prophylactic gastropexy for high risk breeds; always do a prophylactic gaastropexy for splenic torsion)
What are some non-surgical diseases of the spleen?
- Nodular hyperplasia (Monitor with AUS over time)
- Hemosiderotic plaques
- Splenosis - "Daughter spleens"
- Lymphoma (usually not surgical)
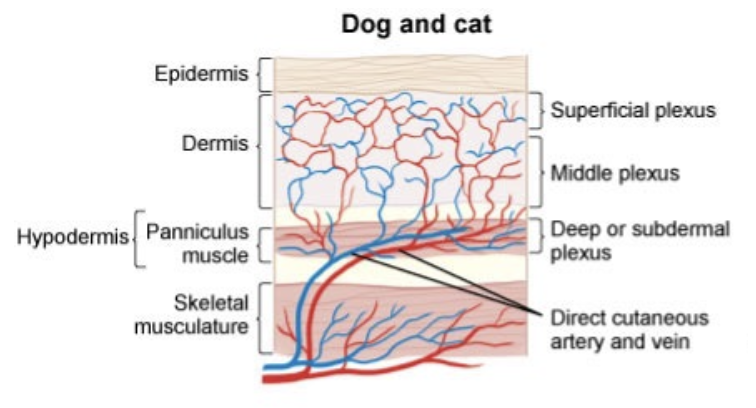
What blood supply to the hypodermis is important?
- Direct cutaneous artery and vein
What are the stages of wound healing?
1) Inflammation
2) Proliferation/repair
3) Maturation/remodeling
