Aural Rehabilitation Final
1/65
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
CI team
A group of professionals who are part of the CI process and which often includes:
Otolaryngologist
Audiologist
Clinical Coordinator
Educator
Aural Rehabilitation Specialist
SLP
Psychologist
Social Worker
May also include implanted peers, family/caregivers, or a neuroradiologist
Otologist/ENT
Determine medical candidacy/radiologic studied (CT & MRI); perform surgery; follow up medical services
Audiology
Determine audiological candidacy; program device at hook up and follow up; counseling; ongoing treatment
SLP
Initial eval to determine baseline speech/lang; counseling and ongoing treatment
Psychologist
Initial eval to determine if there are any cognitive/psychological contradictions; consider other stressors in house, ability to follow-up, realistic expectations
Educators/AR specialist (LSL, AVT, Teacher DHH)
Coordinate services and/or provide treatment
Social Worker
Assists families with resources etc.
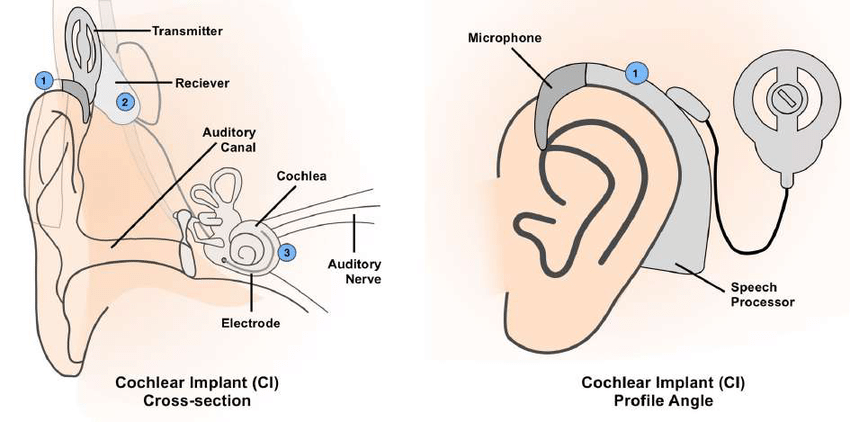
External components of CI
Microphone - picks up sound and converts sound to electrical signal
Processor - processes incoming signal
Transmitter - send radio frequency (RF) signal
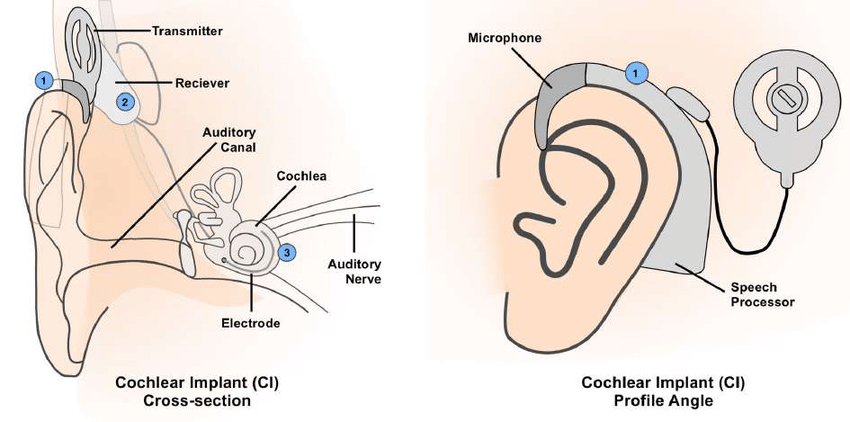
Internal components of CI
Receiver - receives RF signal
Electrode array - delivers electrical stimulation
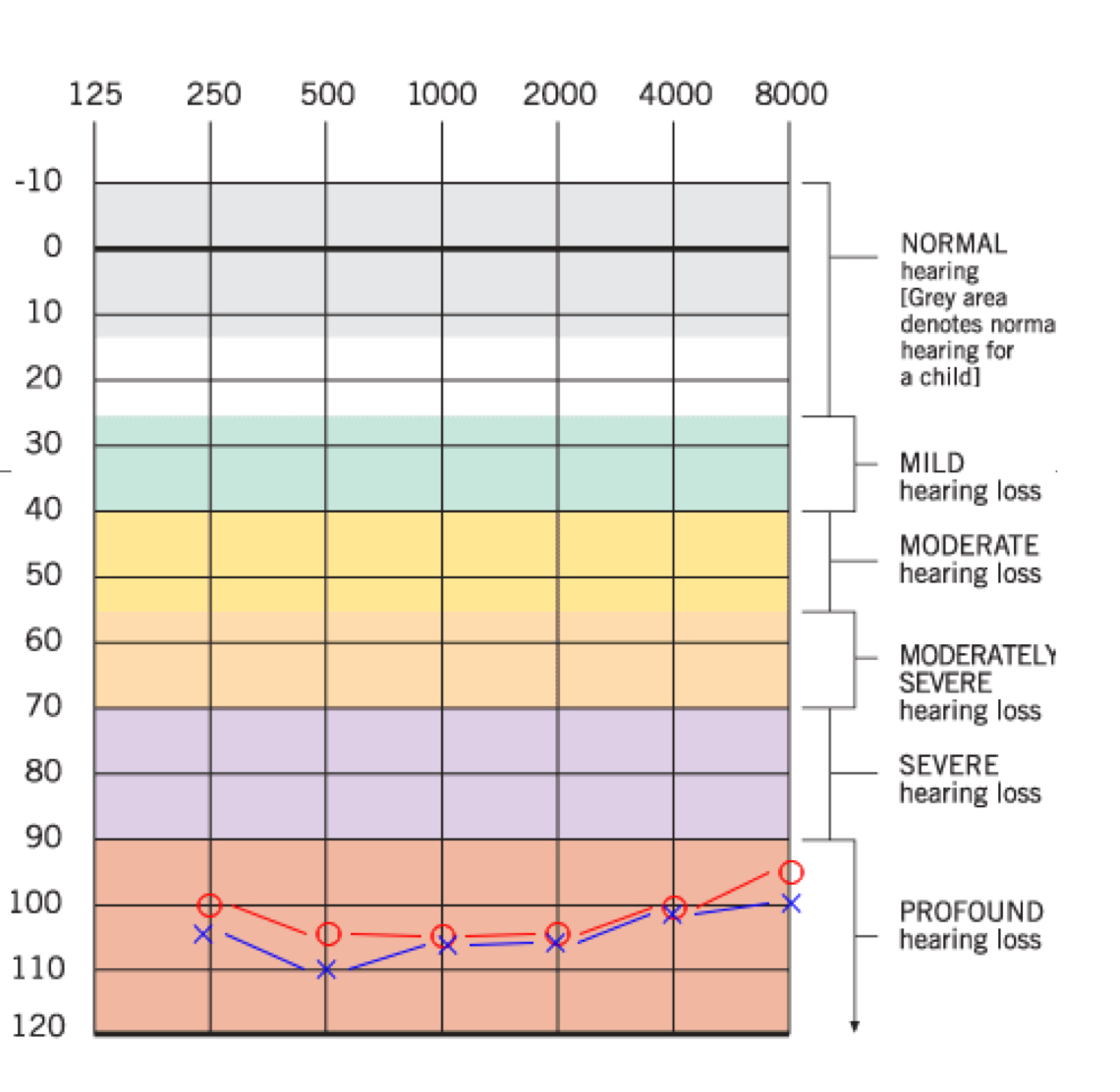
Hearing level (Profound HL)
Usually defined as PTA at 500, 1000, 2000 Hz; Hearing losses can be flat, or more of a “corner audiogram” shape. Hearing levels at high frequencies can make a significant impact on the ability to receive speech, since most consonants are high frequency in nature
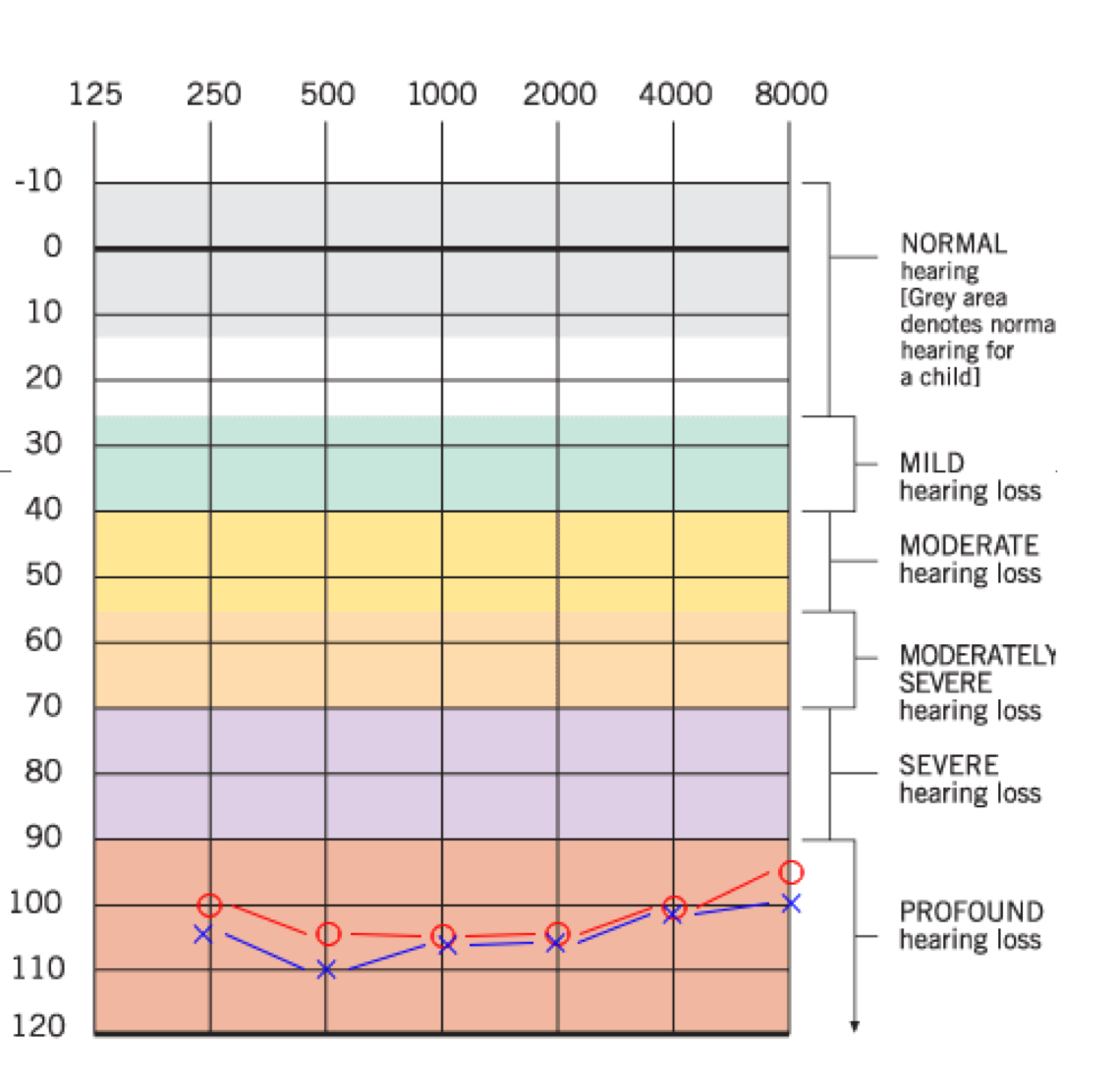
Dynamic range (Profound HL)
The decibel difference between threshold of audibility and threshold of discomfort. Typical hearing listeners have about a 100 dB dynamic range. Speech has a dynamic range of 30 dB; the range between the loudest vowel and softest consonant; we need 30 dB dynamic range minimally to hear unvoiced /th/ and not have the /a/ become uncomfortably loud.
If the threshold is at 90 dB and discomfort levels are 110 dB, then you have a bigger dynamic range available than if your thresholds are 100 and your discomfort levels still are 110.
Auditory resolution (Profound HL)
Refers to the ability of the inner ear structure and associated neural systems to code spectral (frequency/intensity) and temporal (processing of acoustic stimuli over time) differences among speech sounds.
ex: Can the ear tell the difference between /s/ and /sh/?
Profoundly deaf individuals at best might have auditory resolution to perceive rhythm, intonation, vowel contrasts, and even many consonant contrasts. At worst, only gross variations might be detected.
What are the factors that contribute to success with CI?
According to Chute & Nevins “Zone of CI Performance,” their research indicates that the factors that contribute to success with CI include:
For children, age of implantation (most important factor!)
For children, auditory neuron survival/functionality
Short duration of deafness
Amount of residual hearing/language ability prior to implantation
Motivation and family support
Vision-only speech reading ability
Commitment to auditory-oral education
Ability to use communication strategies effectively
What factors are not associated with or correlate with CI success?
Intelligence
Etiology of the deafness
Note: As many as 50% of children with severe-to-profound deafness, who are implanted, may have other attention, memory, and/or learning-type deficits or disabilities that influence performance with the CI
FDA candidacy criteria
Pediatric:
FDA approved multichannel CIs in 1990 for children between 2–17 yrs who had profound hearing losses
As of 2020, the FDA approved CI for children as young as 9 months old —> only manufacturer approved for 9 mo is Cochlear Corp, and MedEl & Advanced Bionics for 12 mo+
2 yrs of age+ : degree of HL severe to profound (bilateral)
9 mo to 2 yrs of age: degree of HL profound (bilateral)
Adults:
Widespread us of CIs began in the 1980s; moderate to profound SNHL in both ears
Single sided deafness (SSD) one ear, normal or mild other ear
Asymmetrical HL Profound SNHL one ear, other ear mild to mod-severe other ear
What is involved in a medical/audiologic evaluation?
Audiological evaluation - to determine benefits from conventional hearing aids
Medical - CT scan for status of cochlea + MRI for auditory nerve
Briefly describe CI activation session
To establish the initial electrode “map.” The hook-up usually takes place 3-4 weeks post surgery. A computer interfaces with the processor to adjust its parameters, including:
Dynamic range - establish the minimum and maximum current levels that will elicit a response (current threshold levels) and that will be uncomfortable (current discomfort levels). The difference between the two is the dynamic range of current
Loudness balance - establish that all electrodes are equally loud at the midrange of current levels
Pitch and pitch ranking - establish that all electrodes result in a different pitch; sweep from base to apex
Exclude electrodes that cause pain, that do not result in a different pitch, etc.
Activate device - after all current values have been decided as above, turn them all on and deliver speech!
Parent/patient instruction in how to use the device - similar to the hearing aid orientation
Mapping
The process of programming the speech processor of a cochlear implant
When is it indicated that an individual may need a mapping session with an audiologist?
During the follow-up stage of the implant process, the audiologist adjusts the stimulus parameters of the speech processor to optimize speech recognition.
Electrodes aren’t too stable at first, so re-map them a few days after the initial hook up. Then, re-map a few weeks later. After that, they can be remapped at least annually.
Adults usually will be able to tell if they are not hearing as well and will go for a new map.
Signs to look for that a child needs a new map:
Child’s speech perception decreases
Child reports change in sound
Child has an adverse reaction to sound
What (re)habilitation resources are available through the cochlear implant websites?
These are the rehabilitation pages of the websites that Dr. Nokes linked in the CI slides:
What should the primary focus of therapy for children with CI?
Children with HL since birth will have limited (to no) memories of spoken language. They will need to make the associations between sound and meaning, just like newborns do.
The AR process is going to involve a language-rich environment and training in speech, language, and listening, but with close monitoring of auditory skills and access to spoken language. Children usually obtain a CI to try to develop auditory/oral communication to as great a degree as possible.
What is the percentage of children identified with hearing levels outside typical range or with severe-to-profound hearing loss?
Over 1 million children with HL is the US
Approx. 3 out of every 1000 live births have congenital HL
1/1000 with profound HL
Before NHSPs, avg. age of identification was 2.5 years of age
What percentage of children with severe-to-profound hearing loss have (normal) hearing parents?
Between 95+% of children who have a severe or profound sensorineural hearing loss have parents who are normally hearing
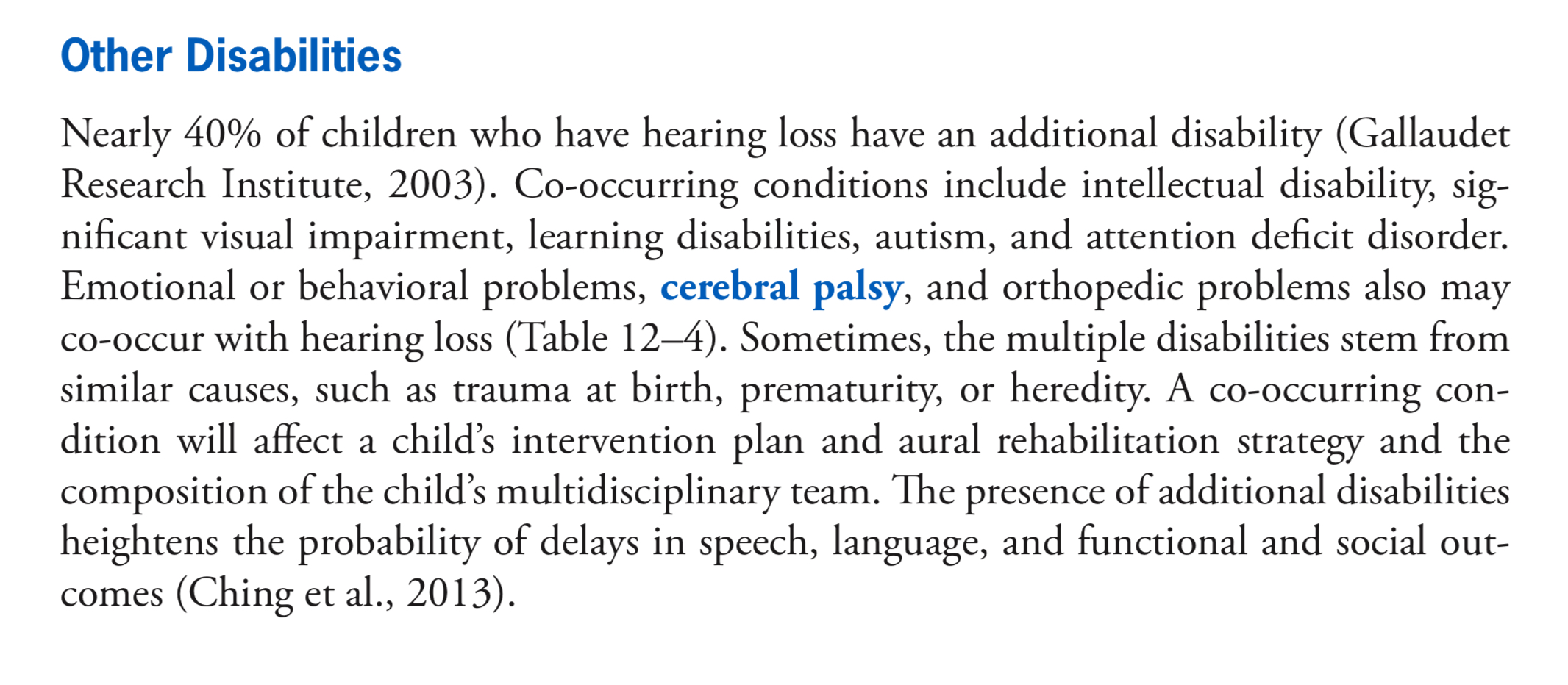
What is the percentage of children with additional disabilities (vision, learning, orthopedic, etc.)?
Nearly 40% of children who have hearing loss have an additional disability
Most common causes of pediatric hearing loss
Perinatal - anoxia (prolapse of the umbilical cord and blockage of blood to infant’s brain), use of forceps during birth
Postnatal - meningitis, infections, ototoxic drugs, measles, encephalitis, chicken pox, influenza, and mumps
Congenital - Waardenburg syndrome (autosomal dominant), Usher syndrome (autosomal recessive), Alport syndrome (X-linked)
What percentage of infants are born with genetic HL?
Genetic factors cause more than 50% of all incidents of congenital hearing loss in children
What is the “typical” hearing profile (if there is one) and or most common traits of individuals with:
Down Syndrome: Chronic MEE w/ Eustachian tube dysfunction, 1/3 with SNHL can be progressive
Chronic otitis media, associated conductive, mixed, or sensorineural HL —> textbook
Usher’s Syndrome: Congenital profound to progressive hearing loss, vision associated with retinitis pigmentosa
Congenital or progressive sensorineural hearing loss —> textbook
Bracio-Oto-Rental Syndrome: Conductive, sensorineural, or mixed
CHARGE Syndrome: Multiple system: Cardiac, respiratory vision, hearing, vestibular, neurologic; common deafblind syndrome
Most common features are asymmetrical mixed losses that are severe-to-profound in degree —> textbook
Treacher Collins Syndrome: Conductive HL related to aural atresia and ossicular malformation, craniofacial abnormalities tend to involve underdevelopment of the zygomatic complex, cheekbones, jaws, palate, and mouth
Padlet for more information: https://sjsu.padlet.org/eringinney/hearing-loss-conditions-infographics-and-or-slide-deck-dzmi054cg58yq08l
What is meant by the term non-syndromic?
A hearing loss that has no other associated findings
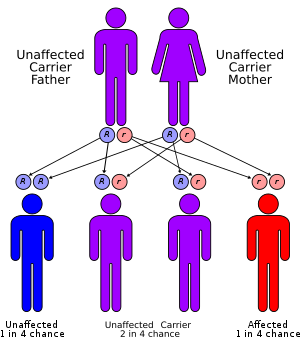
In an autosomal recessive inheritance pattern, what is the chance of an offspring having a condition?
A condition that requires both parents to have the affected gene in order to pass a trait on to an offspring; parents may not exhibit the trait, and it has a ¼ chance of being inherited
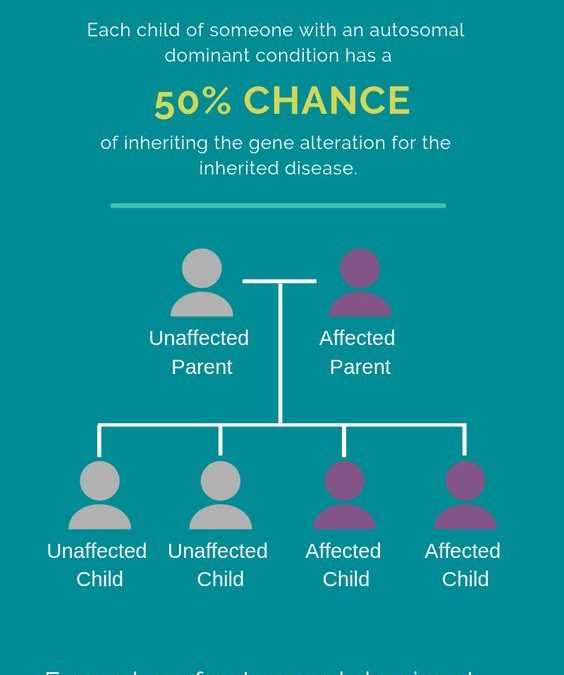
In an autosomal dominant inheritance pattern, what is the chance of an offspring having a condition?
A condition that requires only one parent to have the affected gene in order to pass a trait on to an offspring with a 50% chance of being inherited
How does X-linked manner of inheritance occur?
A condition that involves genes carried on the X chromosome, or the sex chromosome
What are the syndromes most commonly associated with combined hearing and vision differences (deafblindness)?
CHARGE Syndrome
Usher Syndrome
Down Syndrome
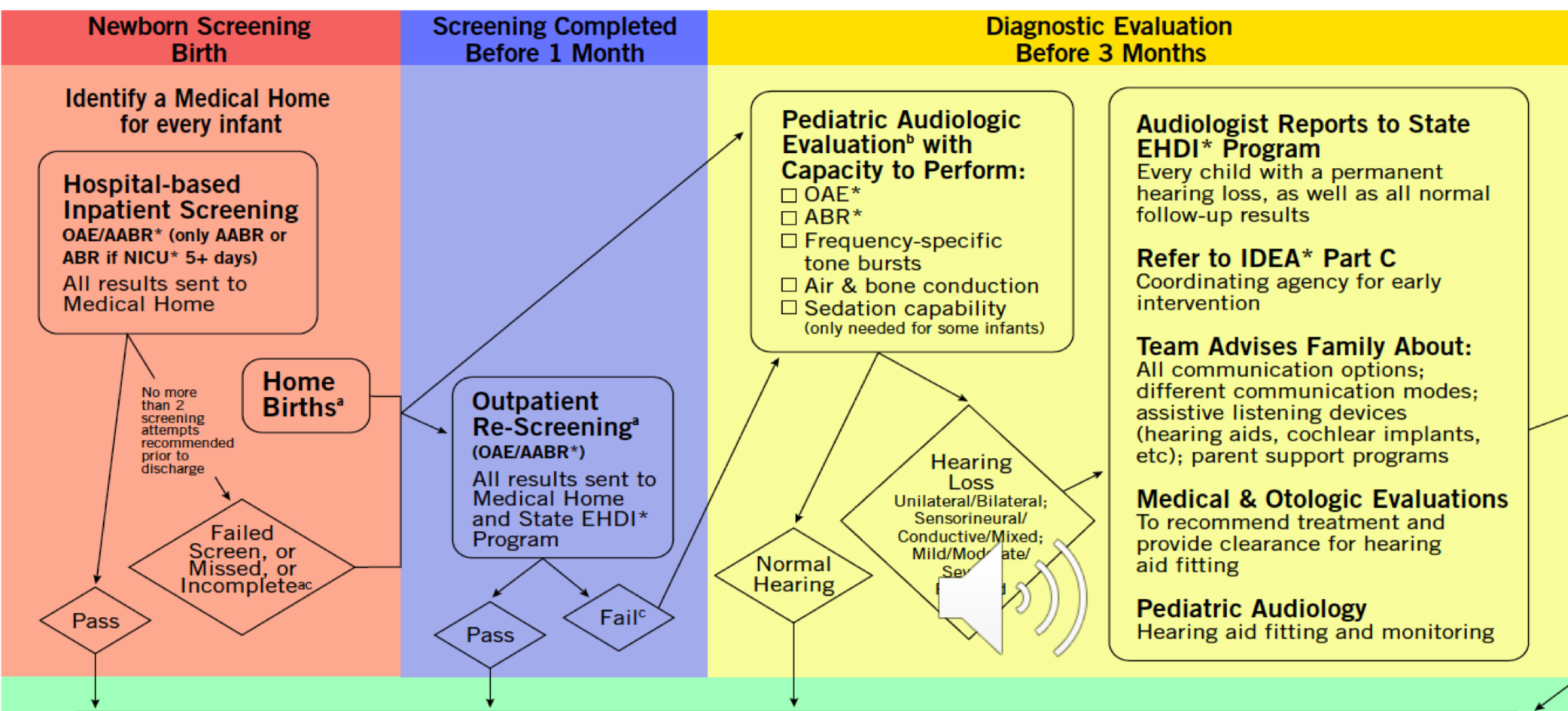
1-3-6 Rule of EHDI - What do the numbers mean?
Screen all infants by 1 month of age
Diagnose all infants by 3 months of age
Begin intervention by 6 months of age
Note: For some states that have met these, now 1-2-3 (CA is still at 1-3-6)
Do hospitals just offer newborn hearing screens, or are they mandated?
The US federal Newborn Infant Hearing Screening and Intervention Act was signed into law and then reauthorized as the EHDI Act. About 95-98% of babies in the US are screening before going home.
Universal Newborn Hearing Screening has been law in CA since 2007
Typically, how many screenings are performed before an infant is referring for outpatient screening?
Maximum of 2 screens in the hospital, as there is an increased change of missing infants with hearing loss (false positive)
What happens after the REFER result on the outpatient screen?
After the 2nd REFER (either unilateral or bilateral), an OUTPATIENT hearing screening is scheduled; outpatient screen occurs 2–4 weeks after discharge AABR is performed
What is an audiologist responsible to do after identifying hearing loss?
Audiologist makes referral following confirmation of HL:
any permanent or prolonged hearing loss, regardless of degree or severity, and whether it be unilateral, bilateral permanent, or fluctuating, may result in delays of the development of language; consequently, any infant with a confirmed permanent or prolonged HL is eligible for Early Start Services
Individualized Family Service Plan (IFSP) is developed following assessment
IFSP
A federally mandated plan for children up to 3 yrs that ensures appropriate early-intervention services for infants and toddlers and their families
IEP
Designed to meet each child’s unique needs, support progress in school, and prepare students for further education, employment, and independent living. For students aged 3-21 years of age.
Typical team members of IFSPs and IEPs
Audiologist
SLP
Educator
Psychologist
Interpreter
Itinerant Teacher
Known communication opportunities/modalities for students who are DHH
Sign (ASL, SEE) - Manual/visual communication: usually ASL (bilingual approach) or SEE sign. If ASL is chosen, the child will likely attend school for the Deaf. Parents must be fluent signers ASPA to have a chance at providing a rich language environment. Need language models. Most deaf children still wear hearing aids (helps with speech reading, environmental awareness, etc.)
Listening and Spoken Language (LSL)/AVT - Child must be aided ASAP and family begins to establish an auditory rich environment
Total Communication/Simultaneous Communication - refers to a combined use of sign and speech, whatever modality is best suited for learning at any particular moment for the child
Note: most important factor is to ensure the child has CONSISTENT exposure to language whether spoken or signed
Under IDEA Part C, services are provided in natural environments, why?
Promoting natural environments w/ accommodations is to ensure a child has equal access to the language of the environment
What are pros and cons for services in natural environments for young DHH children?
Pros:
More comfortable with familiar settings ex: home sessions, daycare, park
Cons:
High expectations for child
Some settings may not be conducive to language development, ex: daycares are noisy
What are typical roles of SLP and Ed. Audiologist when providing services to DHH students?
Audiologist:
evaluate hearing and speech recognition skills
assess central auditory function
select, fit, and help maintain appropriate hearing devices, including hearing aids and FM systems
analyze classroom environment and make recommendations about improving classroom acoustics and reducing classroom noise
provide speech perception training
provide consultation to parents and other professionals on the team
SLP
evaluate speech and language performance
evaluate pre-literacy and literacy skills, including phonological awareness
evaluate speech reading skills
select assistive listening devices and perform visual inspection and listening check on amplification devices
collaborate in assessment of central auditory processing disorders
provide speech and language therapy
consult with parents and classroom teachers
provide instruction in sign language to the child, classroom, and home, and ensure that therapy objectives are reinforced informally throughout a child’s day
advise audiologists about appropriate language levels for audiological tests
provide speech perception training
What tests/questionnaires could you include in the test battery to show the impact of hearing loss in education and accessing spoken instruction?
Seeing how a person’s speech perception changes when visual cues are not present (speechreading)
Testing a listener under different circumstances
1. auditory only close/quiet, 2. auditory only close/noise, 3. auditory only far/quiet, 4. auditory only far/noise, 5. auditory + visual close/quiet, 6. auditory + visual close/noise 7, auditory + visual far/quiet, 8. auditory + visual far/noise. (close=within 3 feet from speaker, far = 15 feet from speaker)
Determining how a person may need additional help in different settings, ex: home, classroom
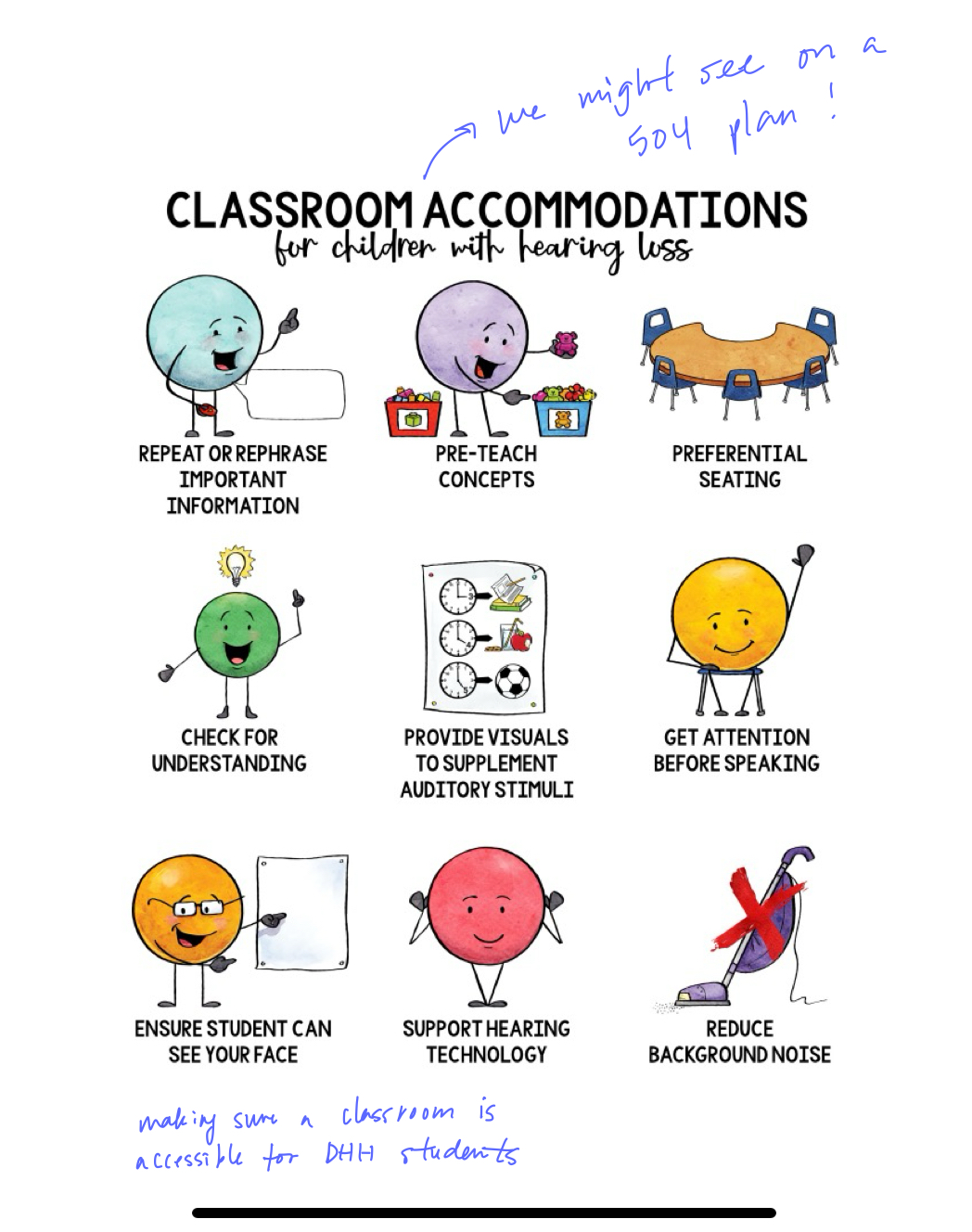
What are some of the typical accommodations recommended for school-aged DHH children to maximize access to instruction?
Repeat or rephrase important information
Pre-tech concepts
Preferential seating
Check for understanding
Provide visuals to supplement auditory stimuli
Get attention before speaking
Ensure student can see your face
Support hearing technology
Reduce background noise
How do we typically test children 6 mo–2 yrs?
Otoacoustic emissions (OAE) - measure of cochlear outer hair cell function (usually higher refer rate than AABR)
Automated Auditory Brainstem Response (AABR) - measure of electrophysiologic response from auditory pathways through brainstem; this procedure is mandated for infants with NICU stay due to the risk of auditory neuropathy, either can be used with Well Baby population
How do we typically test children 3-5 (sometimes 2) yrs old?
Conditioned play audiometry (CPA) - audiologists start using this method around 2–3 yrs of age, most can do it by 2 ½ if practiced
When we can’t measure or monitor unaided behavioral hearing thresholds, what test can audiologists perform?
Auditory brainstem response (ABR) is a type of auditory evoked potential (AEP) testing that is often used with babies and older children who are unable to participate in behavioral testing
What type of testing is used for infants referred to audiology after failing (refer) on newborn hearing screening?
OAE, ABR, frequency-specific tone bursts, air & bone conduction, sedation capability (only needed for some infants)
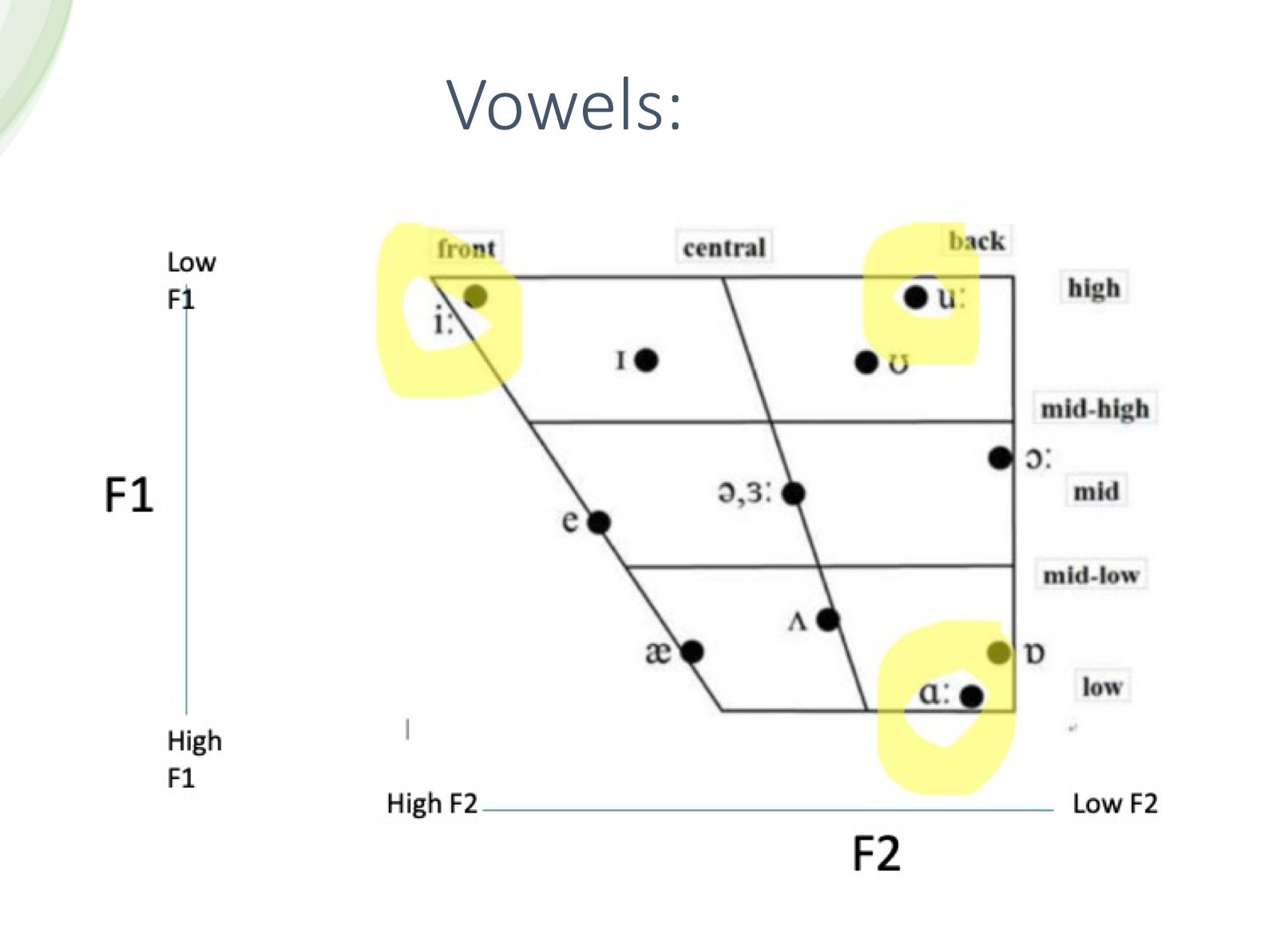
Know the ling vowels and identify the first and second formants (F1 and F2) on an audiogram
[i] - F1= 270 Hz, F2= 2290 Hz
[a] - F1=730 Hz, F2= 1090 Hz
[u] - F1= 300 Hz, F2= 870 Hz
Explain significance of relative difference in relation to vowel formants
Discrimination/identification of vowels is dependent upon the relative positions or relative difference of F1 and F2
Consonants - where are they located frequency/amplitude on an audiogram
See image
When given a vowel chart, be able to identity ling vowels and whether they have a high or low frequency F1 and F2 and what is happening with the articulators
Front-central-back (where constriction is): location of the narrowing or constriction in the mouth, determines F2
High-mid-low (tongue height): position of the tongue itself, which determines F1. The lower the tongue, the higher the F1
Why is it important to understand speech acoustic when working with DHH children?
Children sound like what they hear
ex: if they can’t hear high frequencies, they may not produce sounds like /s/
Selecting appropriate therapy targets
Modifying technology
Setting appropriate expectations
Underscoring the critical nature of HAT systems
Passing the LSL exam (previously AVT)
Understand (4) basic stages of listening/auditory skill hierarchy
Awareness/ Detection: Is sound present? Does a child orient to sound?
Discrimination (Pattern perception) of sound: are sound the same or different? Even if sounds do not yet have meaning, can a child tell them apart?
Identification of sound (segmental identification): objects have names, and names have auditory representation. Can a child associate an auditory label with the object it refers to
Comprehension: can a child understand the meaning of a spoken message? Can a child listen to a short story and answer questions, sequence of events, etc.? Can a child comprehend speech in quiet and in noise?
What are listening therapy/auditory training techniques to consider?
Auditory Verbal Therapy (AVT)
Listening & Spoken Language (LSL)
Should be both analytic and synthetic activities
Angel sounds - all levels, environmental sounds to minimal pairs
Hear builder
Formal (highly structured, especially for monitoring skill development) and informal activities such as playing BINGO
Maximal contrasts to minimal contrasts (fish, king, mop vs. face, vase, lace)
Closed set vs Open set
Closed: word bingo (only words on card)
Open: play a game like Candyland, read the card aloud that contains the directions for the next move
If a child cannot understand a word of a phrase with hearing alone, add another cue, then take the visual cue away and try again
Get the most bang for your buck - use a child’s classroom curriculum for content for your activities or get vocabulary words for upcoming units —> listening and reviewing or front-loading vocab
Common LSL strategies
auditory bombardment - focused auditory stimulation, from the moment the child wakes up, narrating all actions
auditory closure - pause and prompt
acoustic highlighting - therapist/parent emphasizes keywords, pauses just before important words, sing - all techniques to draw a child in and make them want to listen, because listening is so exciting!
auditory sandwich - auditory first, listening sandwich, say it (w/o visual cues), show it, say it again
expansion - adding on to what the child says
expectant look - looking at child and waiting for a response with wide eyes
joint attention - focus on what they are focused on and provide the language communication about that
model language & speech - model clear speech with more vocal interest
caregiverese (motherese) - made up words, real speech with a singsong voice and facial expressions to go along with the voice
ask “what did you hear?”
open-ended questions
optimal positioning - sit close to the child during interactions, get on their level
parallel talk - adults talks to child about what they are doing
prompt
repetition
sabotage - create unexpected situations
self-talk - narrating what a child is doing
take turns - serve and return
wait time - wait longer than you think is necessary while giving an expectant look
whisper - an element of acoustic highlighting
Hands & Voices
A parent-led, professionally-collaborative organization infused with the life experiences of adults who are Deaf or Hard of Hearing, that is dedicated to serving families with children who are D/HH without a bias around communication modes or methodology
John Tracy Clinic in LA
Mission is to provide parent-centered services locally and globally to children with hearing loss, offering families hope, guidance, and encouragement.
Hearing First
Hearing First supports families and professionals to help children with hearing loss have the opportunity to take advantage of access to sound – a critical building block for future success. Hearing powers language, literacy, dreams, opportunities, and lifetime success. In short, hearing powers a child's potential
Language First
Language First aims to educate and raise awareness about American Sign Language (ASL)/English bilingualism and the importance of a strong first language foundation for Deaf and hard of hearing (DHH) children. Browse resources, handouts, events, and intervention activities to make your work as evidence-based as it can be.
How are we able to correctly identify vowel sounds, given the known differences in the speaker’s voice (i.e. male v. female v. child)?
Men’s average FF: 125 Hz
Women’s average FF: 250 Hz
Children’s average FF: 325 Hz
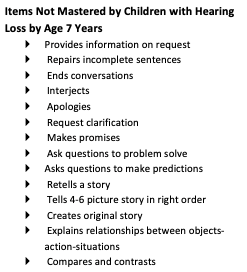
What are areas/items of pragmatic language for children with hearing loss not mastered by 7 years of age (compared to their normal hearing peers)?
See image
Understand difference of intelligibility and reading level between those with limited access to sound and those with early and good access to spoken language (via CI or hearing aids)
Intelligibility - may plateau, not a lot of progress
Children with CI: most have considerably higher overall intelligibility than 20%
Reading level - On average, adults with profound deafness do not have an English vocabulary or English reading ability above 4th grade level
Describe the difference between these 2 terms: Language Exposure & Language Access. Why is it important to know and understand language exposure and access when working with DHH young children?
Language exposure is about the input that is given to a child, while language access is relative to one’s environment and how the child takes in that input and processes it. To acquire a language, this is dependent on one’s language access.
For hearing children, the events of language exposure and access typically are one and the same, while for DHH children they are not. Parents can provide lots of language exposure to their child; however, there is still a possibility that the child won’t have access to that input, thus making language acquisition difficult. This is a form of language deprivation that is based on one’s environment.