Meiosis, Further Cell Theory
1/17
Earn XP
Description and Tags
Meiosis and further cell theory explained in one loooong flashcard.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
Apoptosis
Programmed cell death, a controlled process that removes damaged, unnecessary, or harmful cells without causing inflammation.
Overview of Apoptosis
Trigger: G2 phase cell unable to repair DNA → Apoptosis signal received (internal/external) → Caspase cascade activated
Process:
Caspases cleave DNA, nuclear proteins, plasma membrane
Structural breakdown – Membrane, cytoskeleton degrade → Cell shrinks & blebs → Apoptotic bodies form
Removal: Macrophages signal → Apoptotic bodies removed via endocytosis
Cell Cycle Checkpoints in Apoptosis
Malfunctions in apoptosis can occur during cell cycle checkpoints at G1, G2, and M phases.
G1: Checks nutrients, growth factors, and DNA damage, cell size.
G2: Checks DNA damage and cell size.
M: Checks chromosome spindle attachment.
These checkpoints ensure appropriate resources for the next phase and prevent progression with damaged DNA.
Cell Reparation and Apoptosis
DNA damage can occur:
During DNA replication.
Due to environmental factors (mutagens, UV radiation, viruses, etc.).
If the damage cannot be repaired, the cell undergoes apoptosis. If apoptosis does not occur, cancer can form.
Malfunctions in Apoptosis
Underactive Apoptosis: Can lead to conditions like syndactyly (in embryonic development), tumors, cancer, and autoimmune diseases (e.g., rheumatoid arthritis).
Overactive Apoptosis: Can lead to neurodegenerative disorders such as Alzheimer's disease and Parkinson's disease.
Caspases
Enzymes activated in apoptosis (intrinsic/extrinsic). They:
Chop DNA into fragments
Break down nuclear, cytoplasmic, and membrane proteins
Dismantle the cytoskeleton
Shrink the cell and form blebs
Active Caspases Pathway
🔹 Intrinsic (mitochondrial): Triggered by internal damage (e.g., radiation, DNA damage, infection). Releases apoptosis factors→ activates caspases→ controlled cell breakdown.
🔹 Extrinsic (Death Receptor): Triggered by external signals (e.g., cytokines, cytotoxic drugs, immune cells, hormones, pathogens). Death receptor activation → caspases → cell disassembly.
Stem cells
Unspecialized cells with the ability to divide and differentiate into specialized cell types.
(Or are partially differentiated)
Stages of Stem Cells (Embryonic Development)
Zygote (A): Single-cell stage after fertilization.
2-cell stage (B): Initial division.
Morula (C): Solid ball of cells.
Early Blastula / Cavitating Morula (D): Transition stage where the morula starts forming a fluid-filled cavity (blastocoel).
Blastula/Blastocyst (E): Hollow ball of cells where embryonic stem cells are collected.
Gastrula (F): Stage where differentiation begins (Adult Stem Cells include gastrula).
Further Stages of Human Development: Embryo & Fetus
Embryo: Development stage from the end of gastrulation to ~8 weeks; major organs and body structures begin forming.
Fetus: From ~9 weeks to birth; organs develop further, and the body takes a more recognizable human form.
Type of stem cell potency
Totipotent:
Source: Zygote or early-stage embryo (Morula).
Potential: Can form all cell types, including embryonic and extra-embryonic tissues (e.g., placenta).
Pluripotent:
Source: Inner cell mass of the blastocyst.
Potential: Can form all body cells but not extra-embryonic tissues.
Multipotent:
Source: Adult stem cells (e.g., bone marrow, brain), Gastrula.
Potential: Can form related cell types within a specific tissue or organ system.
Unipotent:
Source: Found in specific tissues (e.g., muscle, skin).
Potential: Can only differentiate into one specific cell type but can self-renew.
Potency: The ability of stem cells to differentiate into different cell types.
Cells with greatest potency can generate more cell types than low potency.
Embryonic and Adult Stem Cells
Embryonic Stem Cells:
Source: Collected at the inner mass of the blastocyst and zygote stage (3-5 days after fertilization).
Potency: Pluripotent (can develop into nearly any cell type).
Issues: Ethical concerns and potential allergic reactions.
Adult Stem Cells:
Source: Collected at the gastrula stage; found in tissues like bone marrow, liver, small intestine.
Potency: Multipotent (can develop into related cell types, e.g., blood cells).
Issues: Lower potency, fewer ethical concerns.
Induced Pluripotent Stem Cells (iPSCs):
Source: Adult somatic cells reprogrammed to become pluripotent using specific chemical hormones.
Potency: Pluripotent (similar to embryonic stem cells).
Advantages: No ethical concerns, can be derived from the patient's own cells.
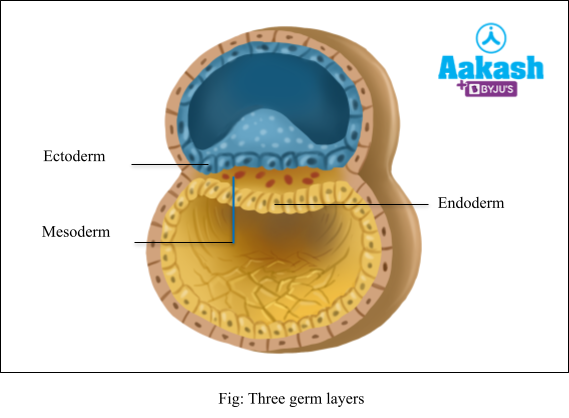
Stem Cell (Gastrula) Diagram
Ectoderm → Forms skin, brain, and nervous system.
Mesoderm → Develops into muscles, bones, blood, and heart.
Endoderm → Becomes the digestive system, lungs, and liver.
Necrosis
Uncontrolled cell death that releases substances causing inflammation, leading to damage of surrounding tissues.
Cell Cycle Misregulation
DNA mutations in cells that are not destroyed by apoptosis can lead to uncontrolled cell division and accumulation of mutations, resulting in cancerous cells. These mutations are often caused by disruptions in cell cycle checkpoints, causing the cycle to become unregulated.
Causes of DNA Damage
DNA damage can be caused by:
Mutagens: Factors that cause damage to DNA.
Environmental factors, mutagens, and inherited genes can contribute to genetic changes.
Types of Mutagens
Chemical Mutagens: Tobacco smoke, air pollutants, chemicals in processed food.
Physical Mutagens: Radiation, UV radiation.
Biological Mutagens: Certain viruses infect cells responsible for regulating cell division and can damage DNA.
Cancer and Cancerous Cell Growth
Cancer is caused by the overgrowth of cells, resulting in tumors due to increased cell division or suppression of apoptosis.
Characteristics of Cancer Cells:
Immortal and divide rapidly.
Not destroyed by apoptosis.
Irregular size and shape, larger than normal cells.
Disorganized arrangement.
Encourage the growth of blood vessels to increase blood supply.
No longer carry out normal cellular functions.