Deck 1: Hepatobiliary, Urinary System, Pelvis
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
106 Terms
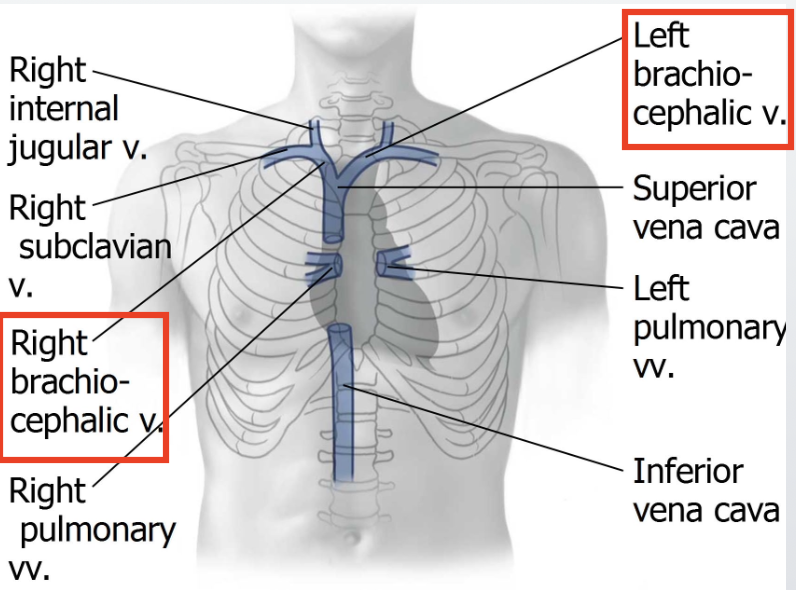
Where does the Superior Vena Cava drain from? List the 2 exceptions.
→ returns blood from all structures above the diaphragm
Exception: lungs and heart
Where and how does the superior vena cava form and descend? FIX
Forms on the right side, behind the costal cartilage of the 1st rib, at the junction of the brachiocephalic veins
Descends posterior and to the right of the aorta
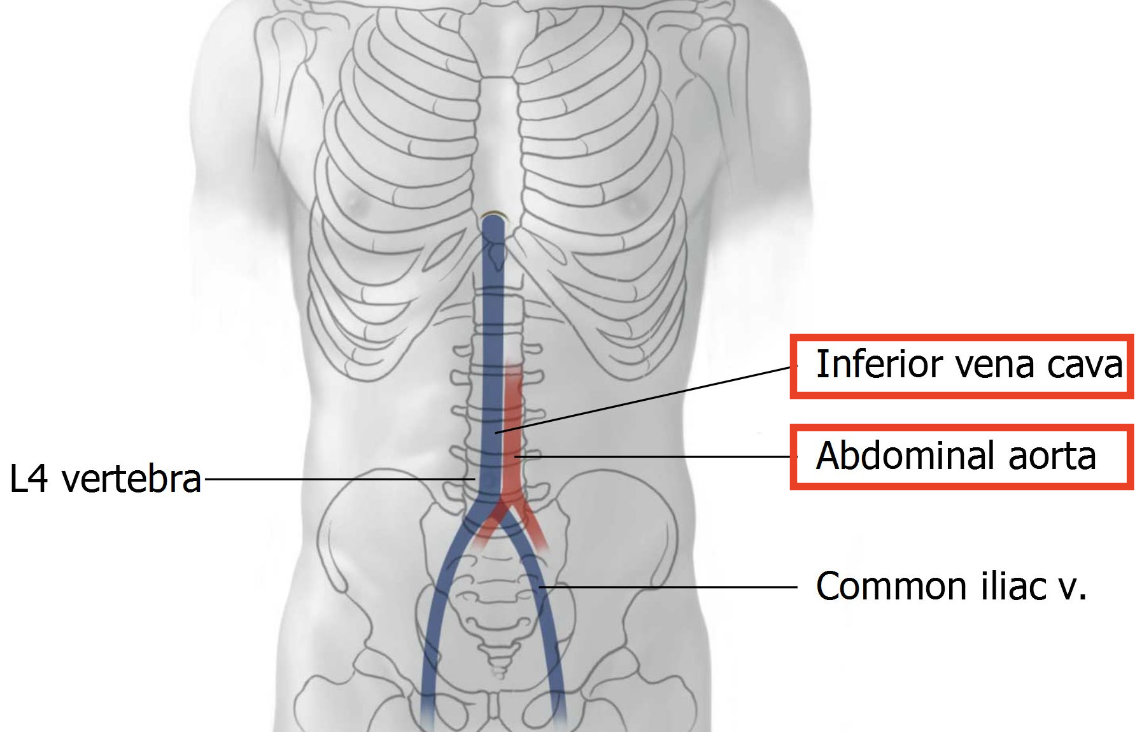
What are the 2 large vessels running down the posterior abdominal wall?
Abdominal aorta + its branches
Inferior vena cava + its tributaries
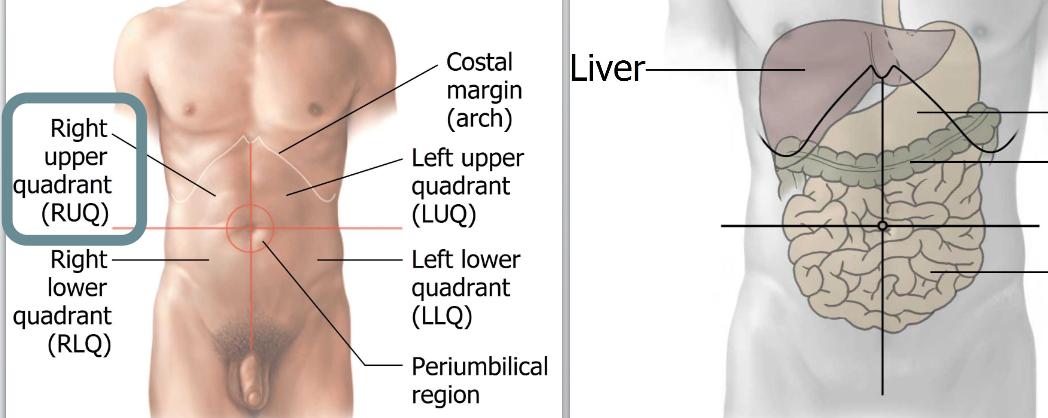
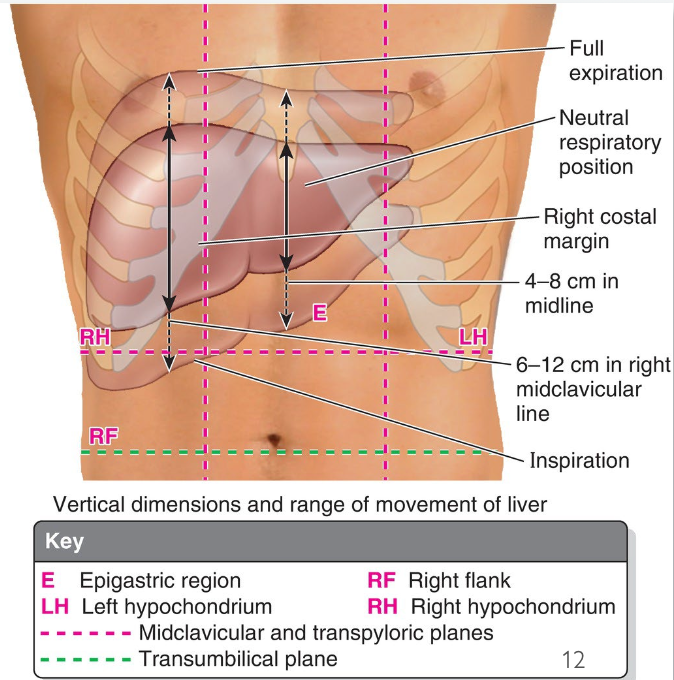
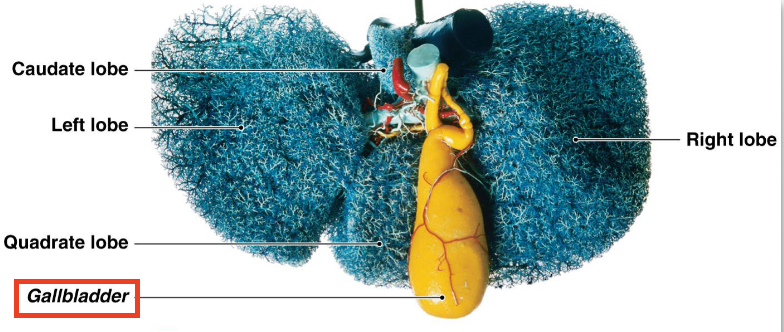
List the characteristics of the Liver.
2nd largest organ in the body
largest gland
largest blood reservoir
accounts for 2.5% of the adult body weight
located in the upper right quadrant (RUQ)
All nutrients absorbed from the GI tract are sent to the ____ via the _____ for filtration. (Exception: _____)
All nutrients absorbed from the GI tract are sent to the liver via the portal venous system for filtration (Exception: fat)
What is the role of the Liver?
Produces and secretes bile
Stores: glycogen, minerals & fat-soluble vitamins (A, D, E, K)
Why is the liver’s movement with the diaphragm clinically important?
liver moves with the diaphragm → this mobility helps facilitate palpation during a physical exam
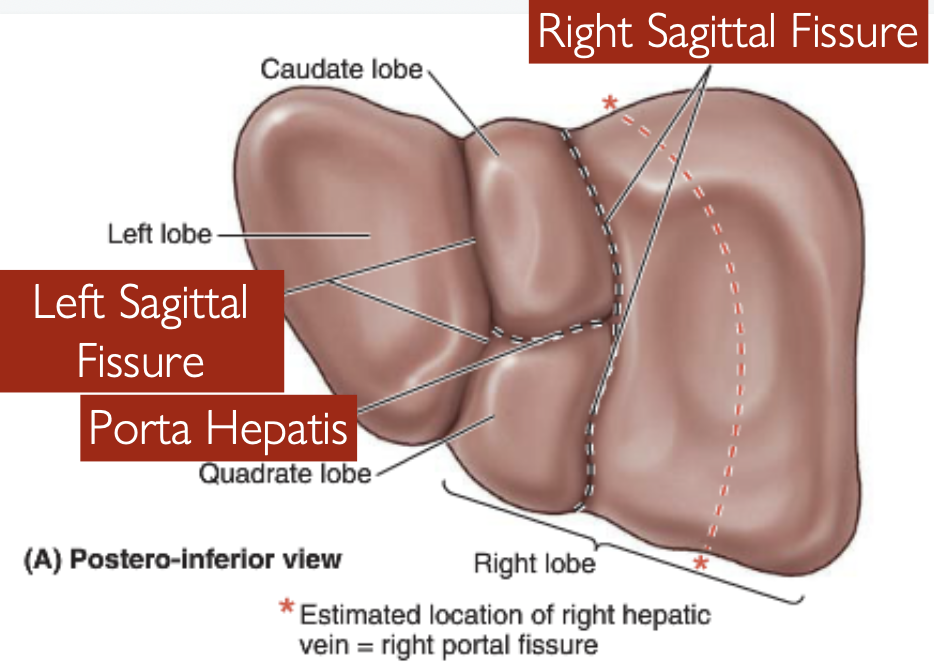
What are the external/visible lobes called?
Anatomical lobes
List the 2 main & 2 accessory lobes.
Main lobes: Right and left
Accessory lobes: Caudate and Quadrate
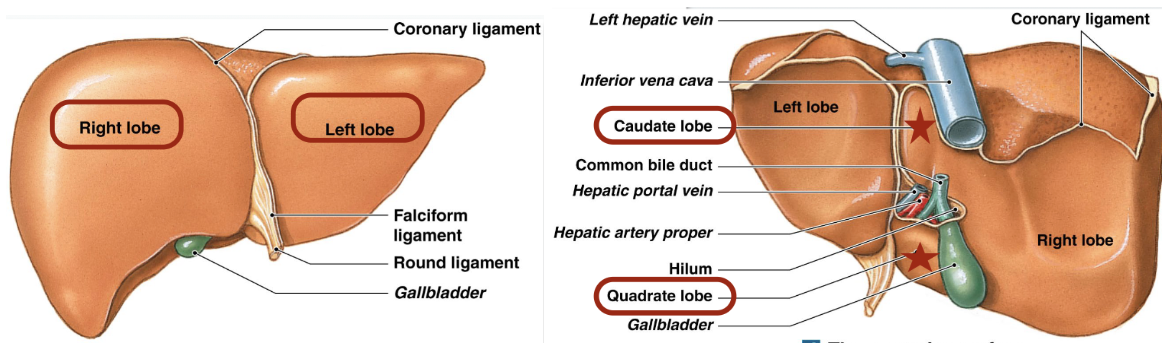
Which lobe has a “tail”? What this tail called?
Caudate has a tail called “caudate process”
What are the internal/functional lobes called? How many are there?
Segments - there’s 8
What are the Segments divided based on? What does this organization allow for?
→ Major subdivisions of the:
hepatic artery
portal vein
hepatic ducts
*This organization facilitates surgical removal of individual diseased segments
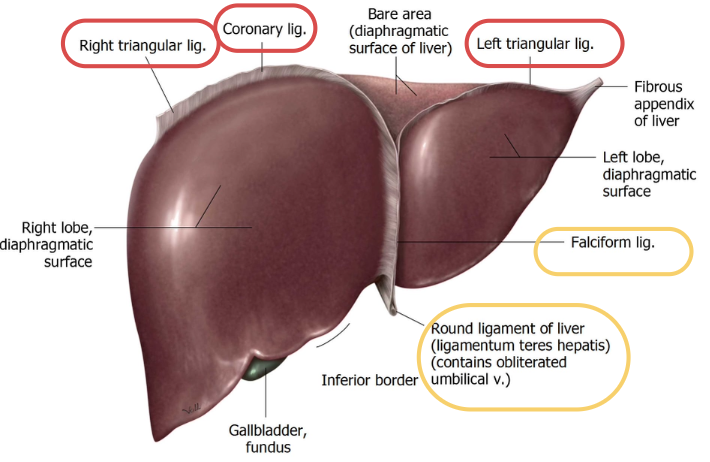
List the 2 surfaces.
Diaphragmatic Surface
Visceral Surface
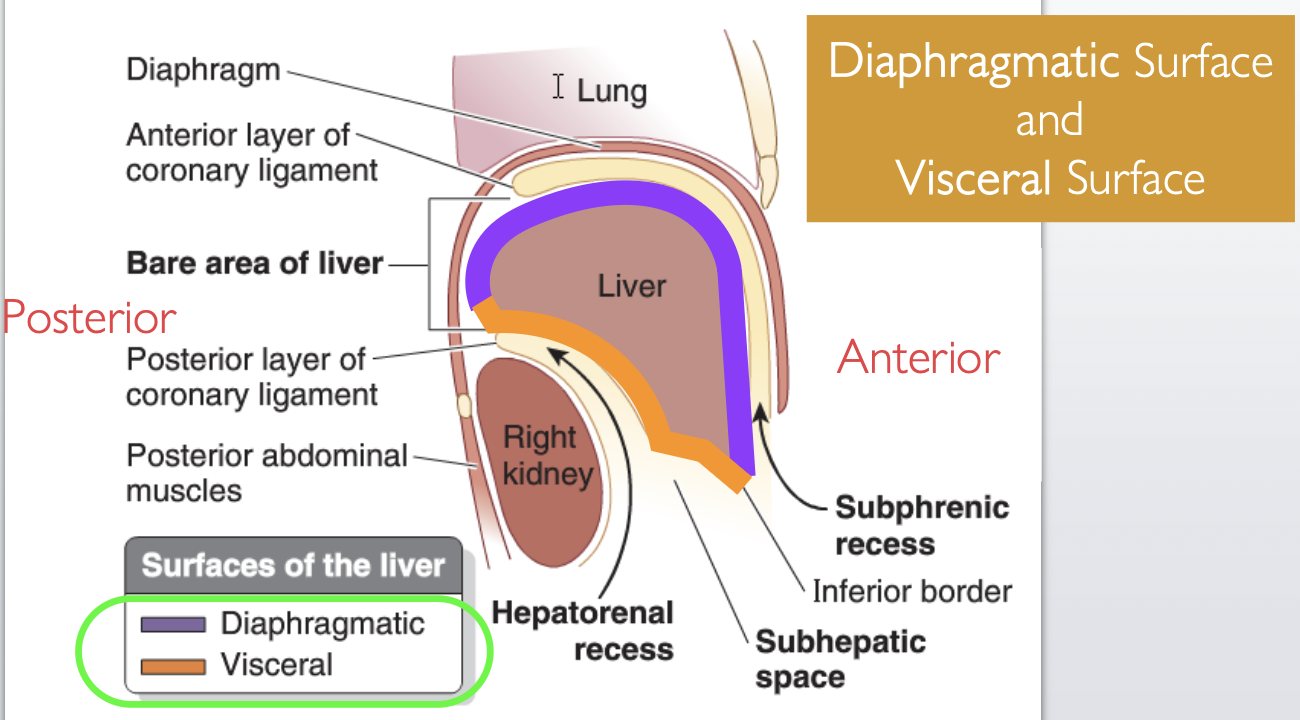
What is the diaphragmatic surface of the liver in contact with?
diaphragm
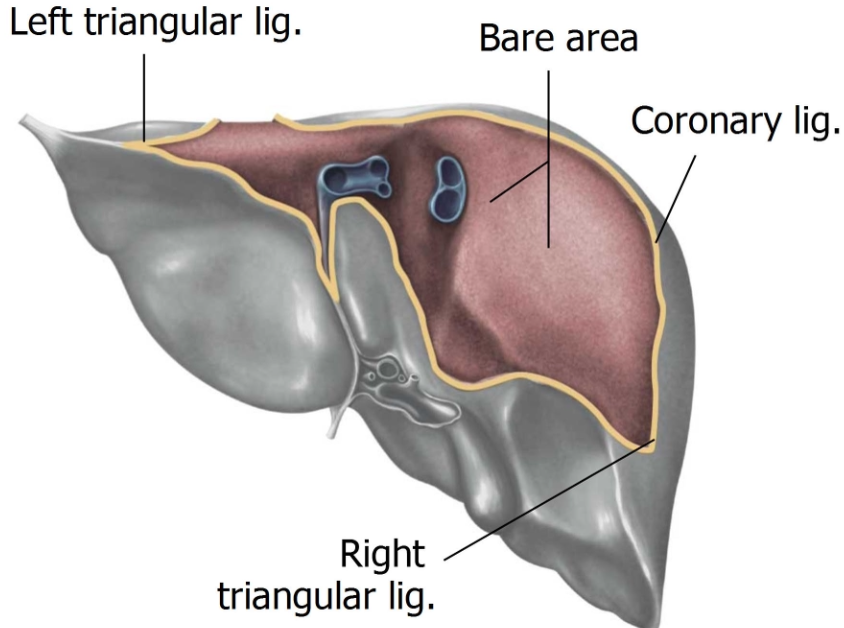
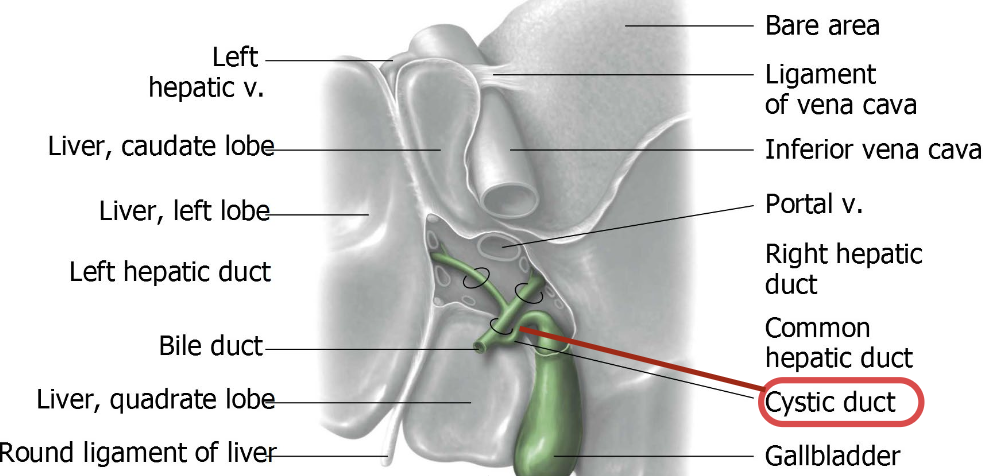
What is the bare area of the liver?
→ part of the liver not covered by peritoneum
allows lymphatic drainage to easily pass to the diaphragm
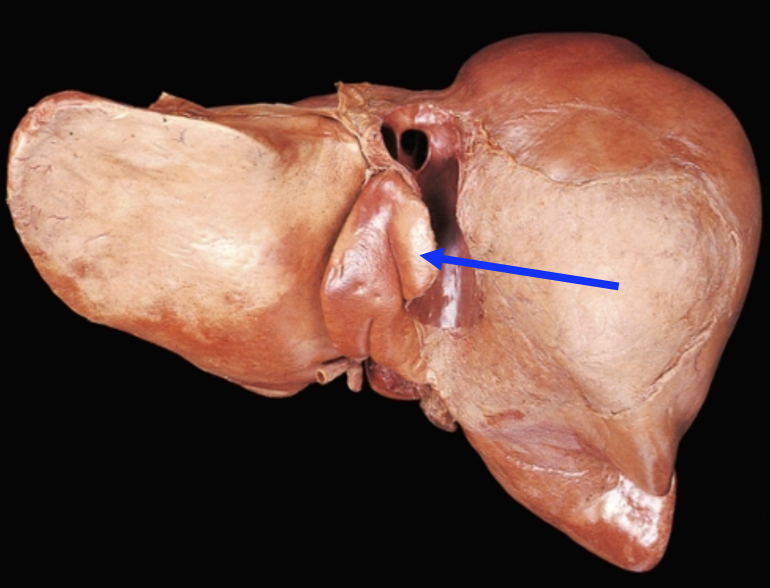
List the 3 fissures found on the Visceral Surface.
Left sagittal fissure
Right sagittal fissure
Porta hepatis (transverse fissure)
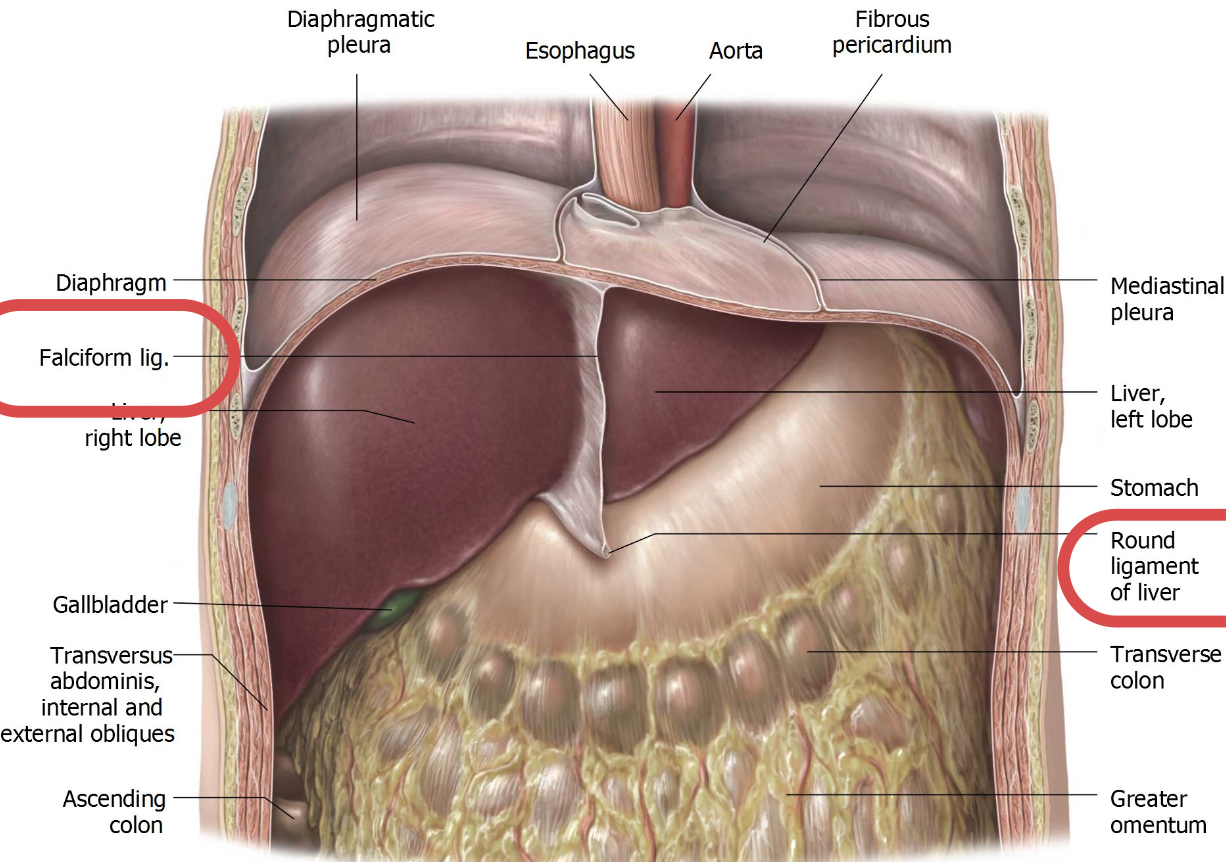
What structures hold the liver in place? List.
→ peritoneal reflections called ligaments:
Coronary and triangular ligaments
Falciform ligament
Round ligament
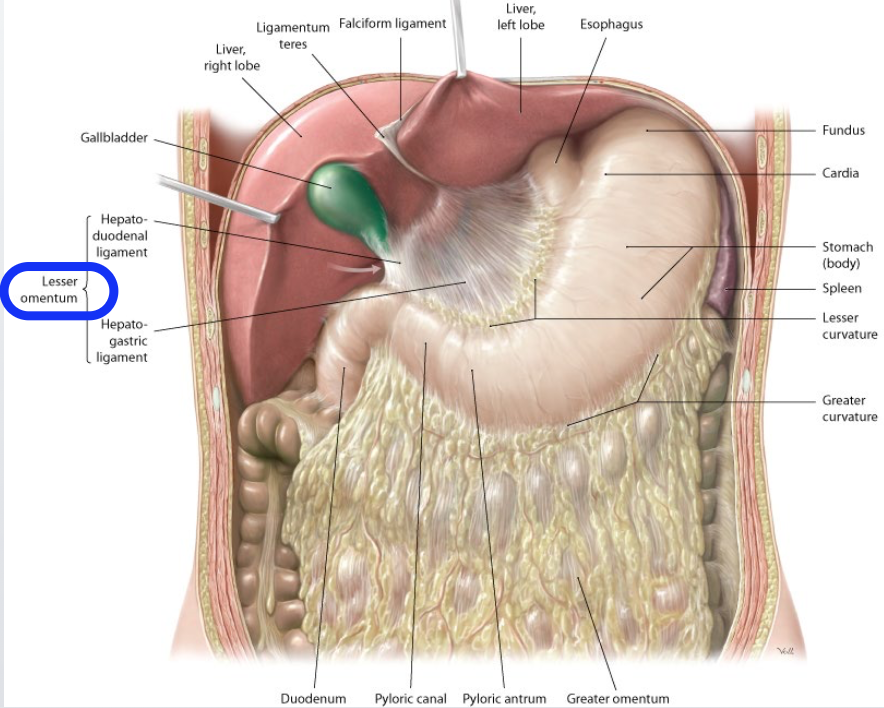
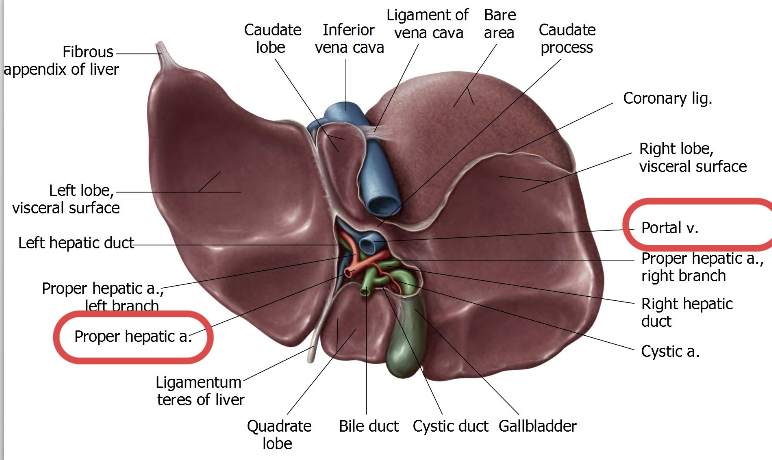
Where does the lesser omentum extend, and what does it enclose?
Lesser omentum extends from the liver to the lesser curvature of the stomach & the superior part of the duodenum
encloses the portal triad
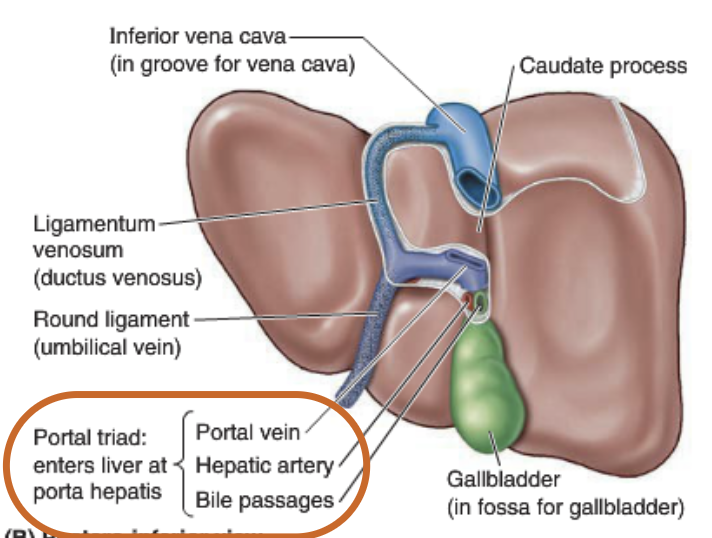
What does the portal triad consist of?
1) Proper hepatic artery (right & left hepatic arteries)
2) Hepatic portal vein
3) (Common) bile duct
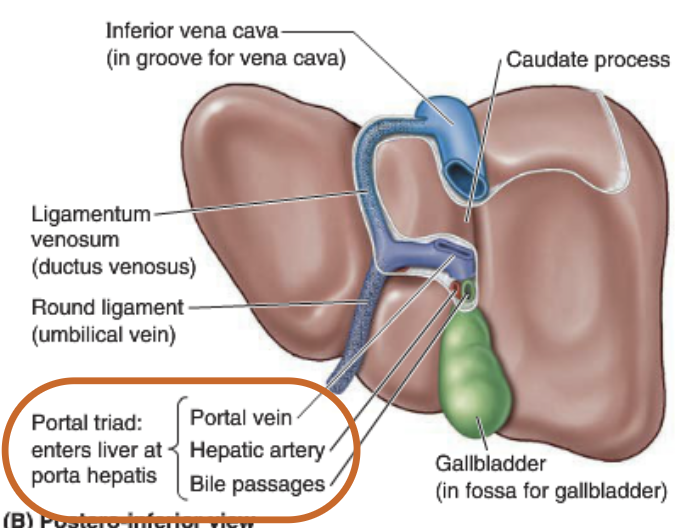
Where does the Portal triad enter and exit?
enter and exit at porta hepatis (deep, transverse fissure on the underside of the liver)
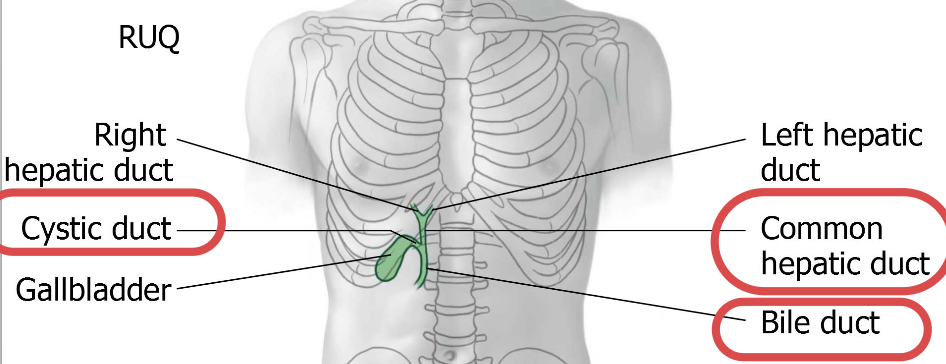
What structures make up the hepatic biliary system?
Right hepatic duct
Left hepatic duct
Common hepatic duct
Right & left hepatic duct join to make up the common hepatic duct
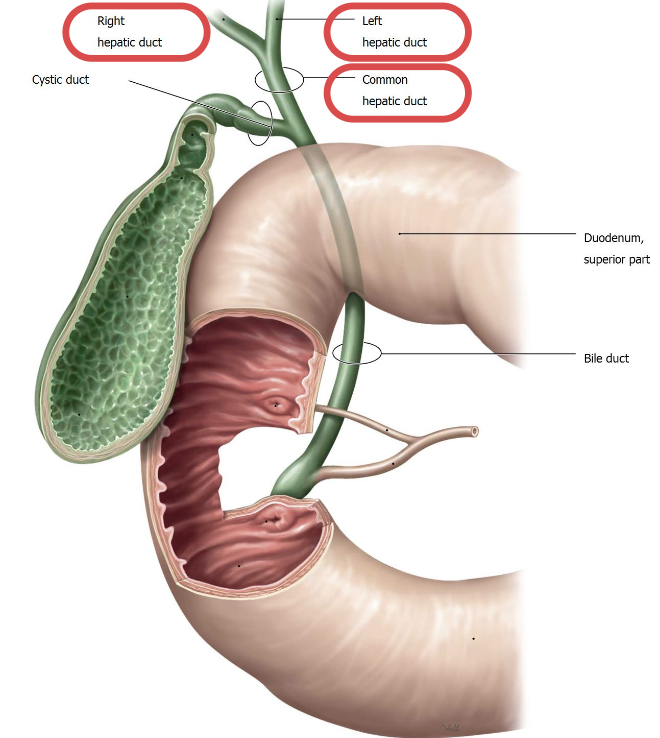
How does bile flow through the hepatic biliary system?
Bile flows either:
directly to the duodenum
indirectly via gallbladder through the extrahepatic biliary system
Where does the hepatic artery originate, and how is it divided? Draw the branching diagram.
Origin: branch of the celiac trunk
Hepatic artery divides into:
Common hepatic artery
Proper hepatic artery
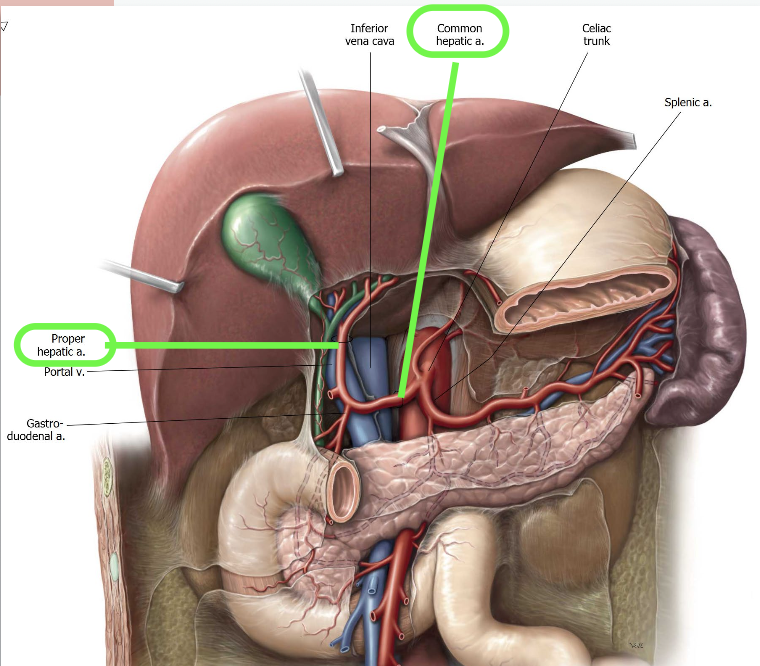

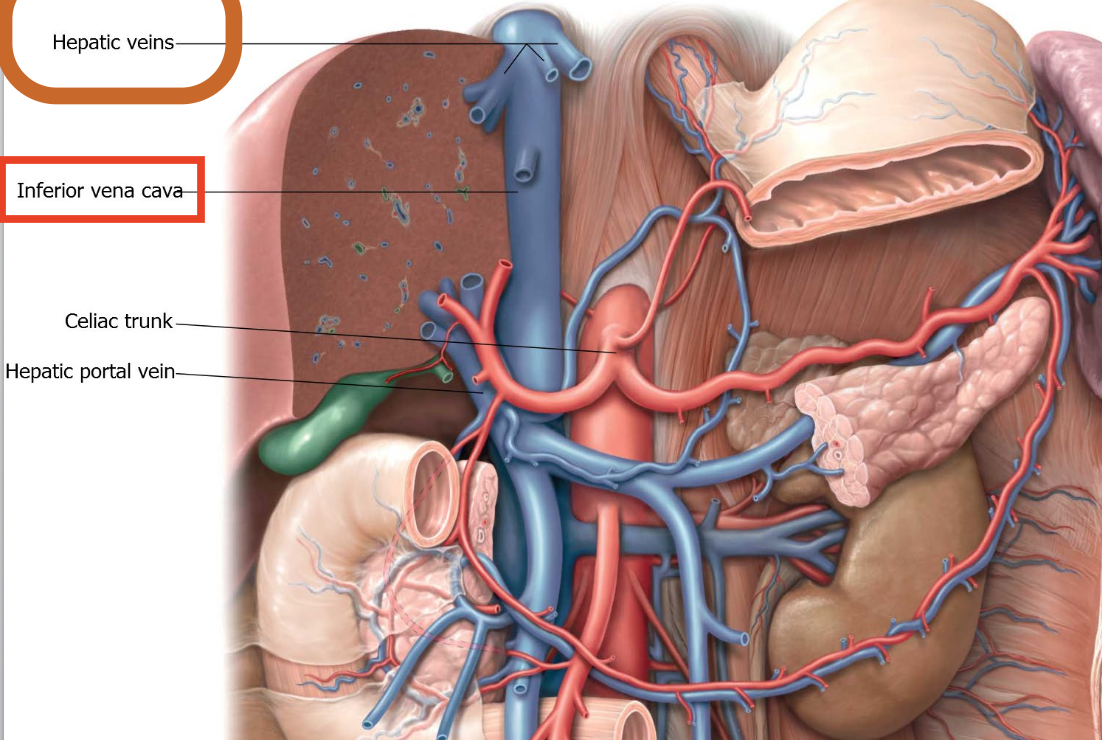
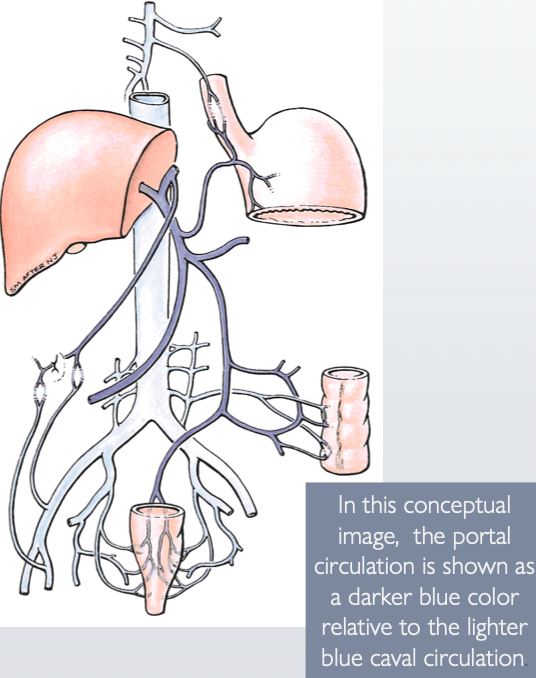
How does blood enter and leave the liver?
Enters via the portal vein & proper hepatic artery
Leaves the liver through the inferior vena cava
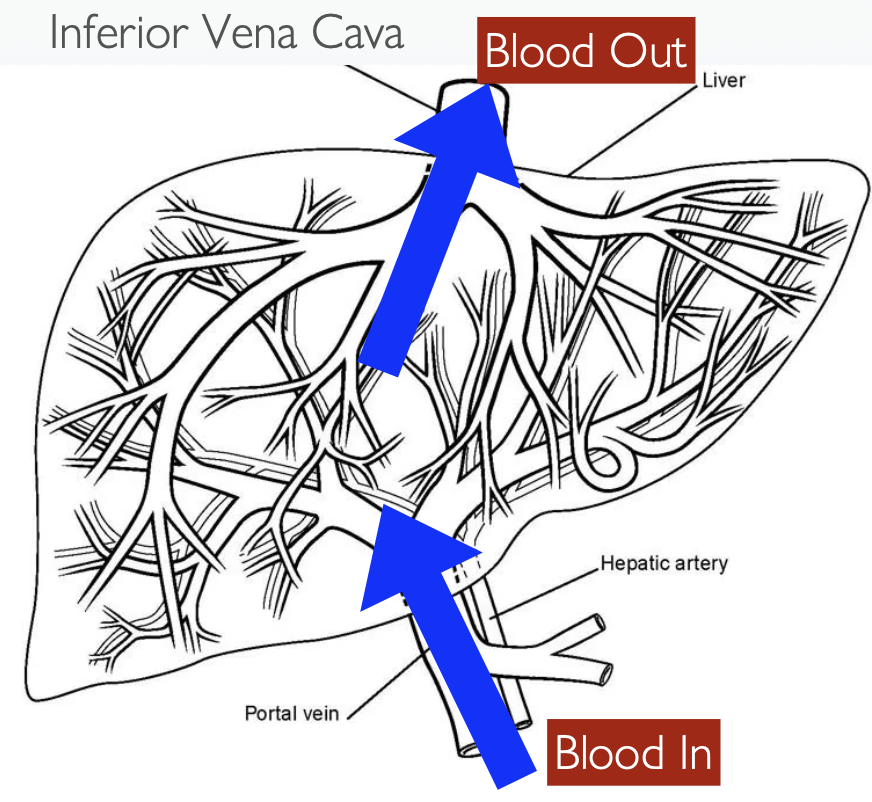
What kind of blood supply does the liver have?
Liver has a dual blood supply from:
Portal vein (dominant) – brings 75–80% of blood to the liver
Proper hepatic artery – brings 20–25% of blood to the liver
What happens to the portal vein and proper hepatic artery (e.g., blood supplies to the liver) at the porta hepatis?
Portal vein & proper hepatic artery terminate by dividing into:
Right hepatic branches → supplies right lobe
Left hepatic branches → supplies left lobe
Describe the characteristics of the Portal Vein.
→ drains blood from the entire GI system in the abdominopelvic area via contributions from the splenic and superior mesenteric veins
Short and wide
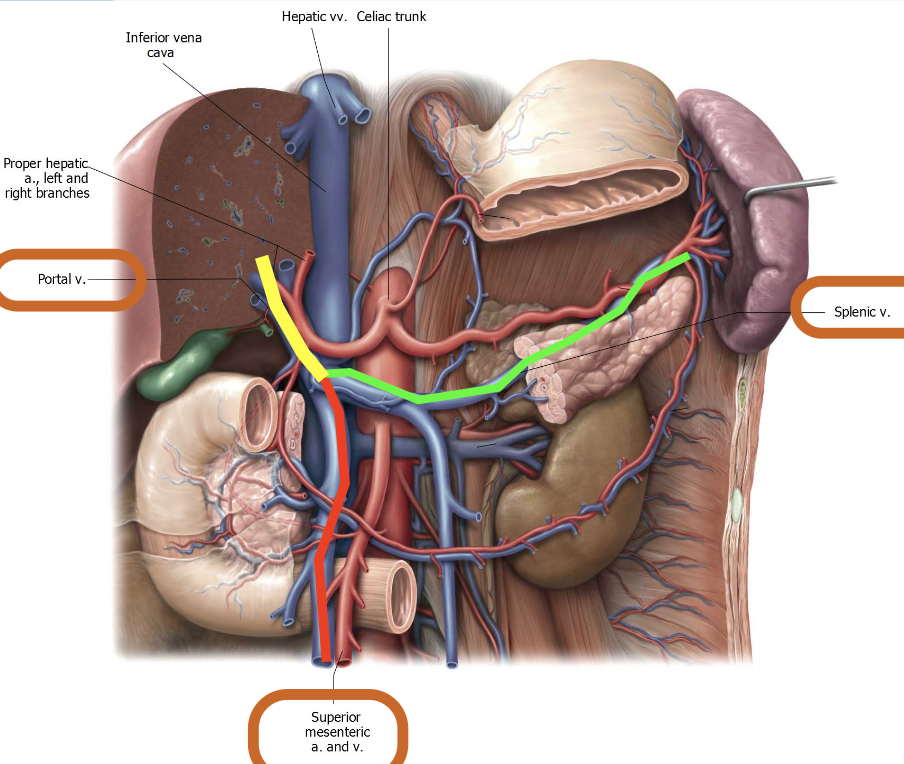
How does Venous drainage of the liver work?
Drains via the:
Right hepatic vein
Intermediate (middle) hepatic vein
Left hepatic veins
- these are intersegmental & open into the IVC within the liver
Intersegmental = run b/w anatomical segments
IVC helps hold the liver in place
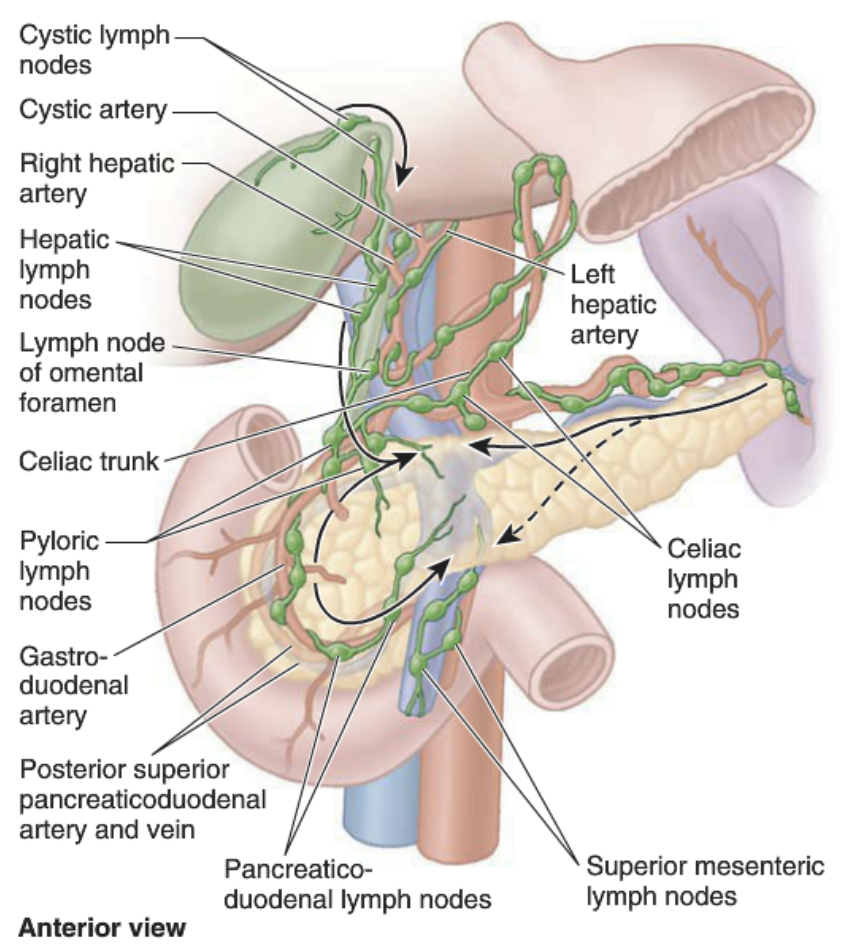
What is the liver’s role in lymph production?
→ major lymph-producing organ
25% to 50% of the lymph entering the thoracic duct comes from the liver
What are portocaval (portal-systemic) anastomoses?
→ act as relief valves, allowing blood from the portal vein to bypass the liver and return to the heart
not designed for high flow, so backup and complications occur
When blood flow through the liver is blocked, portal HTN occurs. What are the major complications of portal HTN in liver disease (e.g., cirrhosis)?
Esophageal Varicosities (Varices) - swollen veins in the esophagus
Hemorrhoids - swollen veins in the rectum or anus
Ascites - fluid in the abdomen
Caput Medussae - veins visible on the belly that look like snakes

What are the key features and functions of the gallbladder?
Hollow, pear-shaped, intraperitoneal organ
Fills by gravity; emptied by muscle contraction
Function: Stores and concentrates bile
What is the function of the extrahepatic biliary system?
transports bile from the liver to the duodenum and/or the gallbladder
What does the Extrahepatic biliary system consist of?
Common hepatic duct
Cystic duct
Bile duct
Extrahepatic biliary system
What is the role of the cystic duct?
→ connects with the common hepatic duct and fills/drains the gallbladder
spiral valve in the gallbladder neck keeps the cystic duct open, allowing bile to flow via gravity from the liver
Extrahepatic biliary system
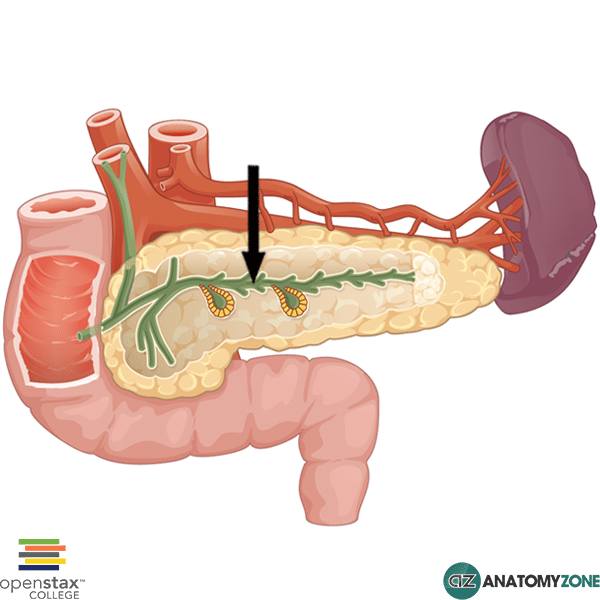
How is the bile duct created?
via the union of the Common hepatic duct & Cystic duct
Extrahepatic biliary system
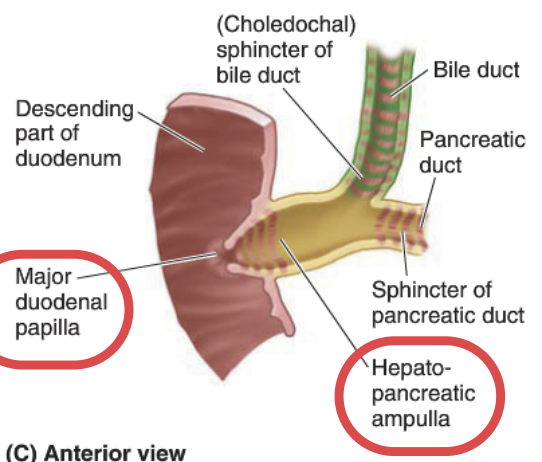
Describe the course and connection of the bile duct.
The bile duct:
Descends behind the 1st part of the duodenum & behind the pancreas head
Joins the main pancreatic duct at the hepatopancreatic ampulla (Ampulla of Vater)
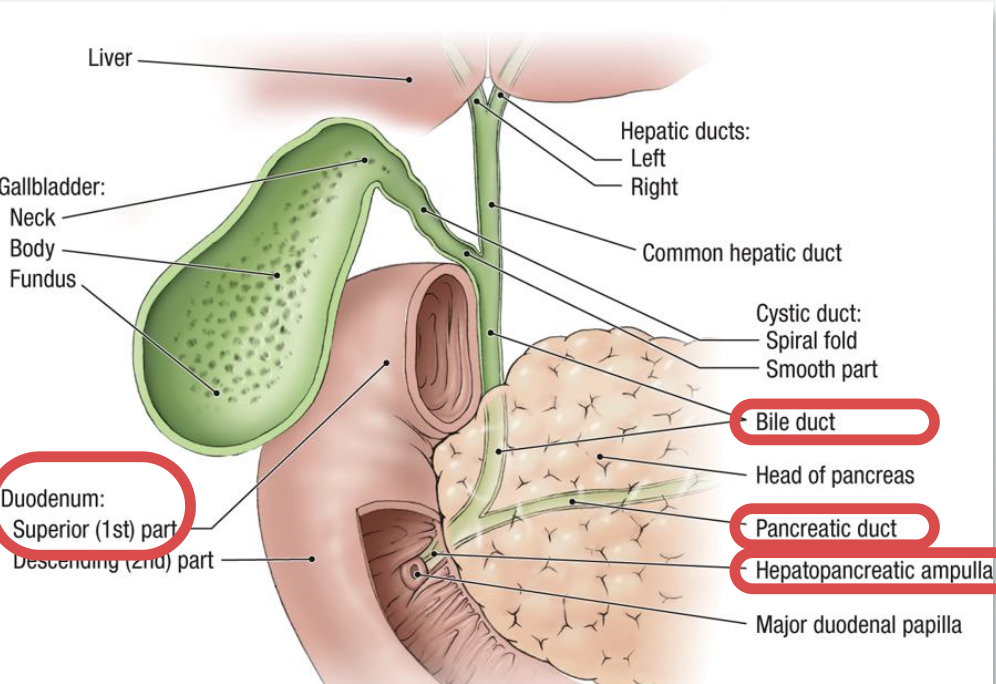
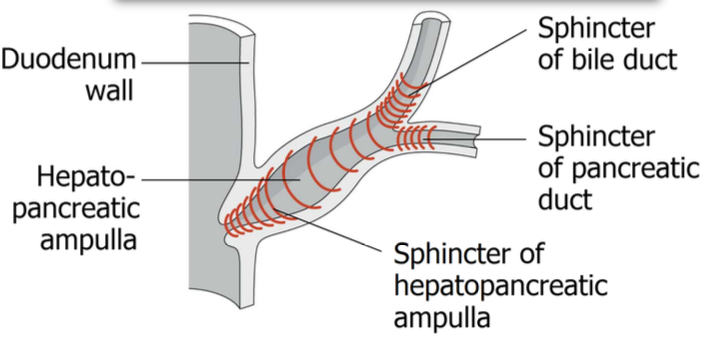
What is the hepatopancreatic ampulla, and how is bile flow regulated?
→ hepatopancreatic ampulla opens into the duodenum as the “Major duodenal papilla”
its surrounded by the hepatopancreatic sphincter (Sphincter of Oddi)
When this sphincter is closed, bile backs up into the cystic duct and enters the gallbladder
How is bile excreted?
Hormonal or neural stimulation triggers bile release into extrahepatic bile ducts
Bile ducts carry bile from liver → gallbladder → duodenum
Where is bile produced, stored, and excreted?
Produced: Liver
Stored: Gallbladder (where it can solidify into stones)
Concentrated: Gallbladder
Excreted into: Lumen of the descending (2nd) part of the duodenum
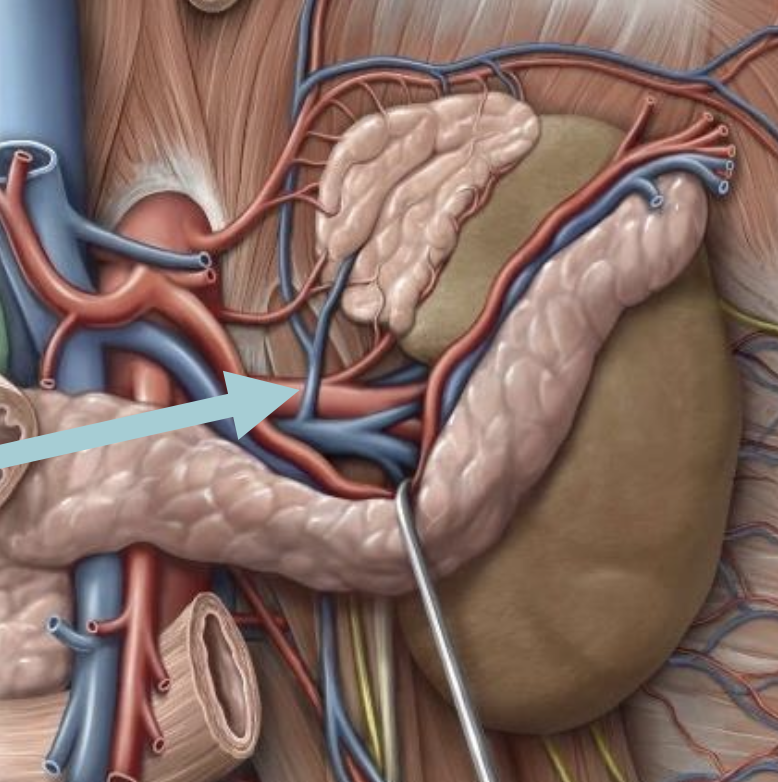
What are the characteristics of the Pancreas?
retroperitoneal accessory gland
transversely crosses L1 and L2 vertebra
Endocrine and exocrine gland
Exocrine secretion - enters the duodenum via the main and accessory pancreatic ducts → neutralize acidity
Endocrine secretions - enters the blood → produces hormones that regulate carb metabolism
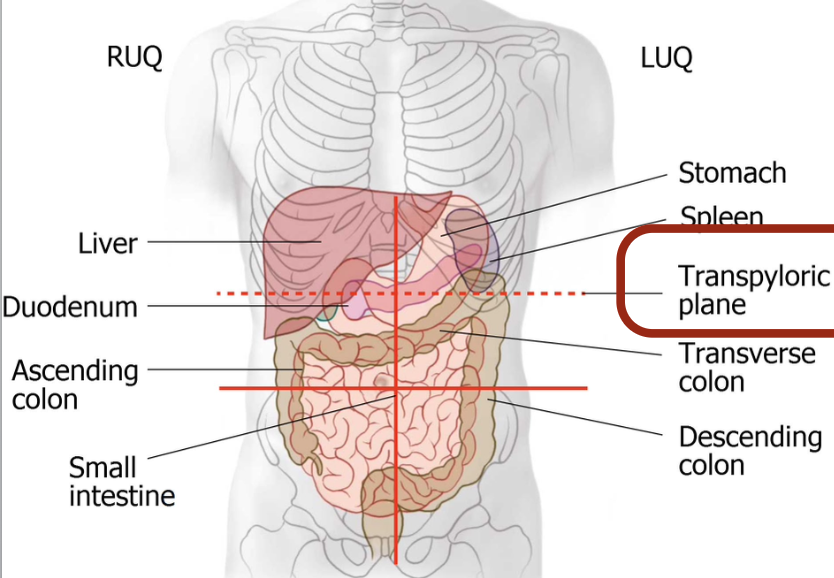
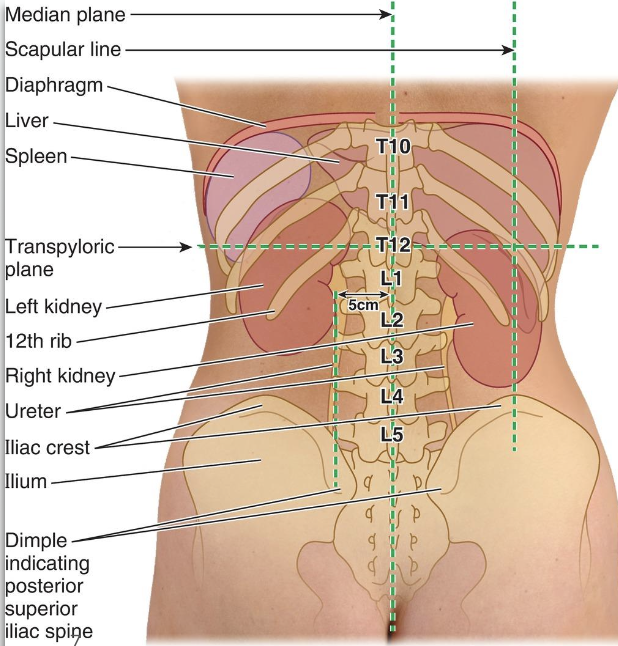
What is the Transpyloric plane?
intersects L1
Found midway b/w the jugular notch of the sternum & upper border of the pubic symphysis
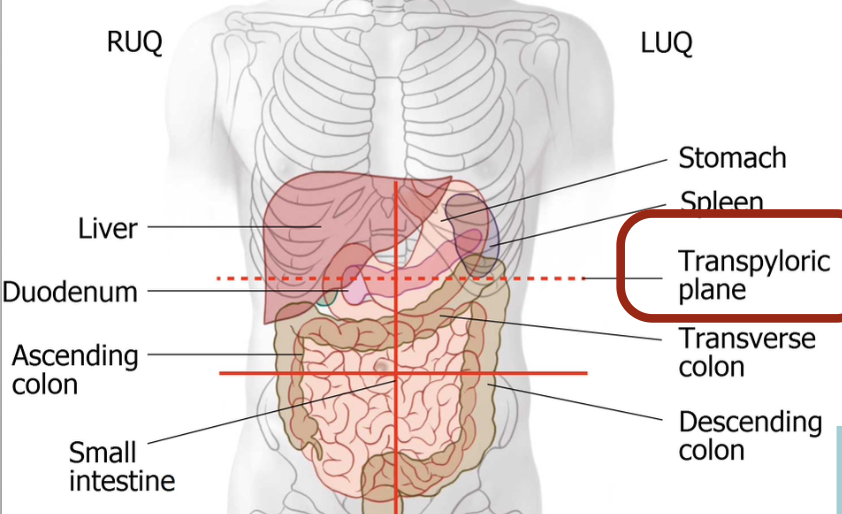
List the structures within the Transpyloric plane.
Superior mesenteric artery, portal vein, renal arteries (origin)
Gallbladder fundus
Duodenojejunal flexure
Left kidney hilum
Spinal cord termination
Pylorus (sometimes)
Name the parts of the Pancreas.
Head
Uncinate process
Neck
Body
Tail
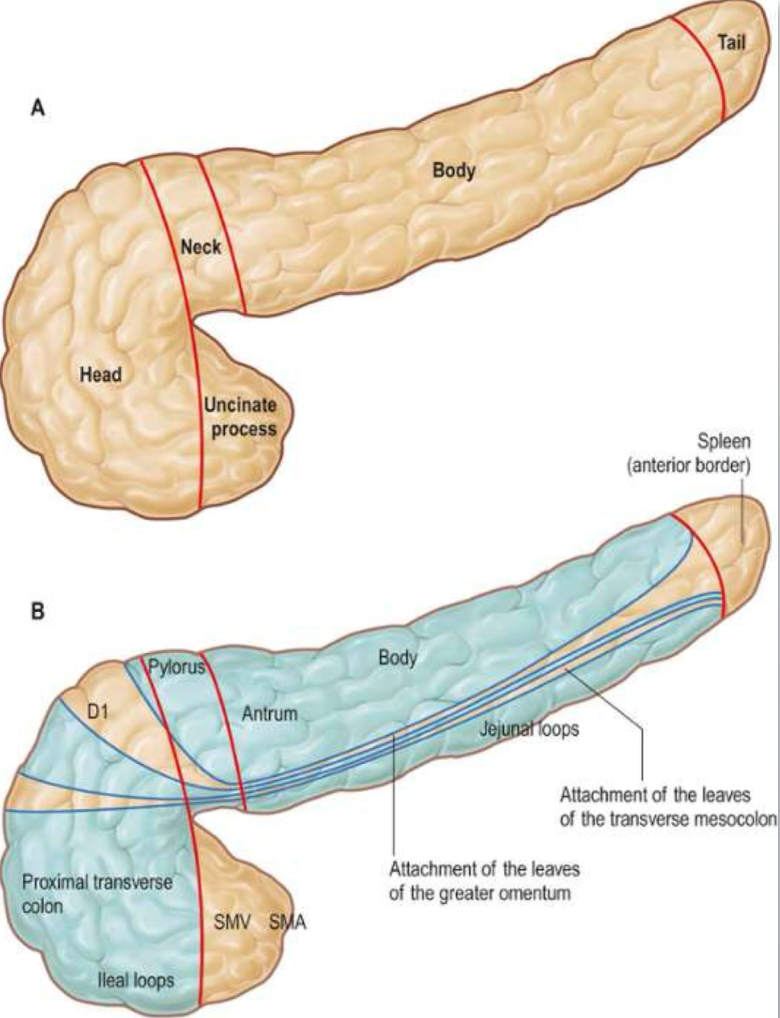
Why can tumours spread so easily in the pancreas?
b/c they have no capsule so tumors spread easily
Where does the pancreatic duct begin, and how does it course through the pancreas?
pancreatic duct begins in the tail and runs through the pancreatic parenchyma (has the cells that produce digestive enzymes and hormone)
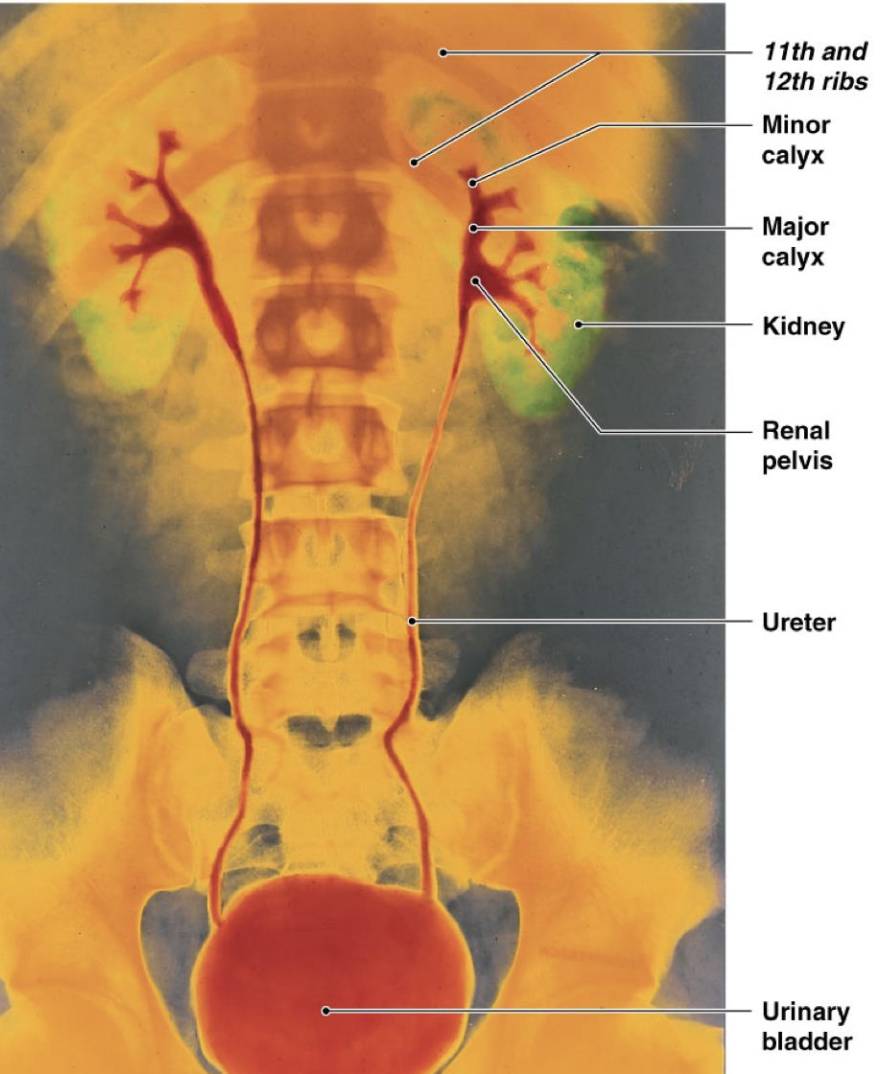
List the primary tissues of the Urinary System. Highlight the Retroperitoneal and Subperitoneal regions.
Suprarenal glands
Kidneys
Ureters
Bladder
Urethra
Differentiate the kidney placement.
Right kidney it positioned lower b/c the liver is on top
What are both kidneys capped by?
Suprarenal glands
What are the posterior relations of the kidneys?
Right kidney: Related to the 12th rib
Left kidney: Related to the 11th & 12th ribs
How does the appearance of the kidney differ in infants and adults?
Infant kidney: lobulated surface (like an adult cow’s kidney).
Adult kidney: smooth surface (about 11–12 cm long, 5–7 cm wide & 2.5–3 cm thick)

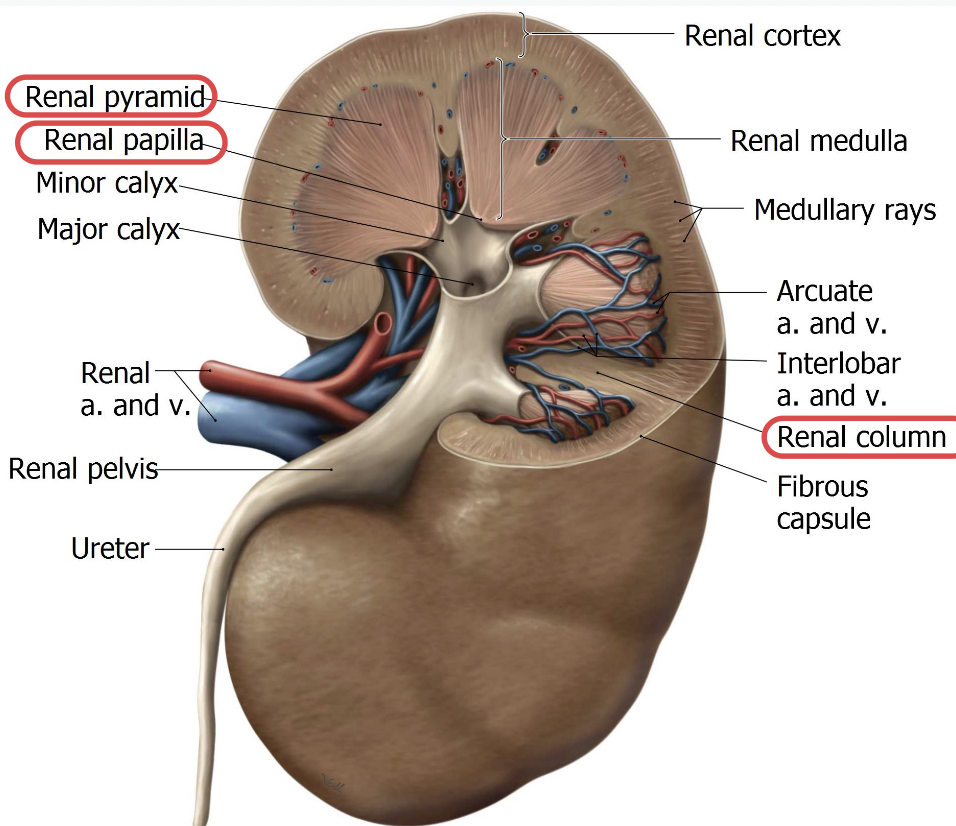
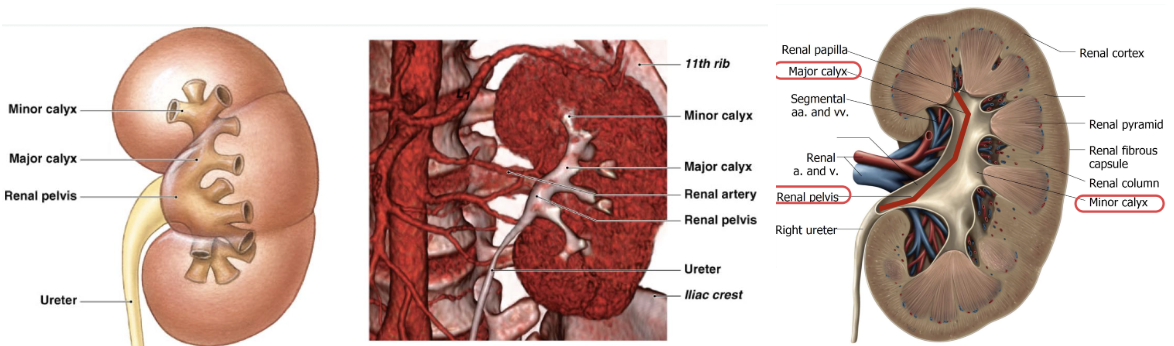
What structures are found at the hilum of the kidney?
Renal Artery
Renal Vein
Renal Pelvis
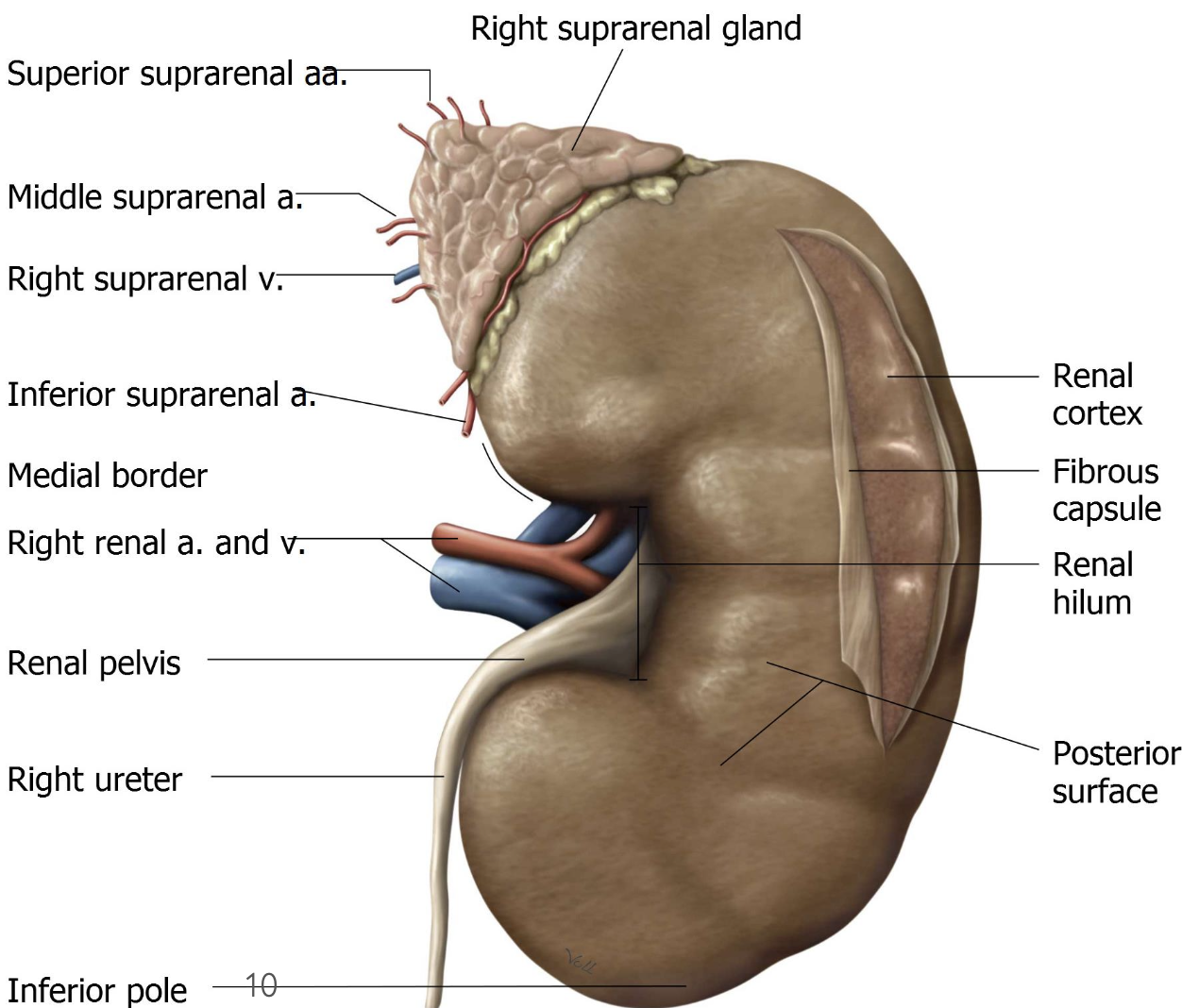
The kidney is enclosed by a fibrous capsule with 2 layers.
Outer layer: Protective and tough
Inner layer: Stuck closely to the kidney surface
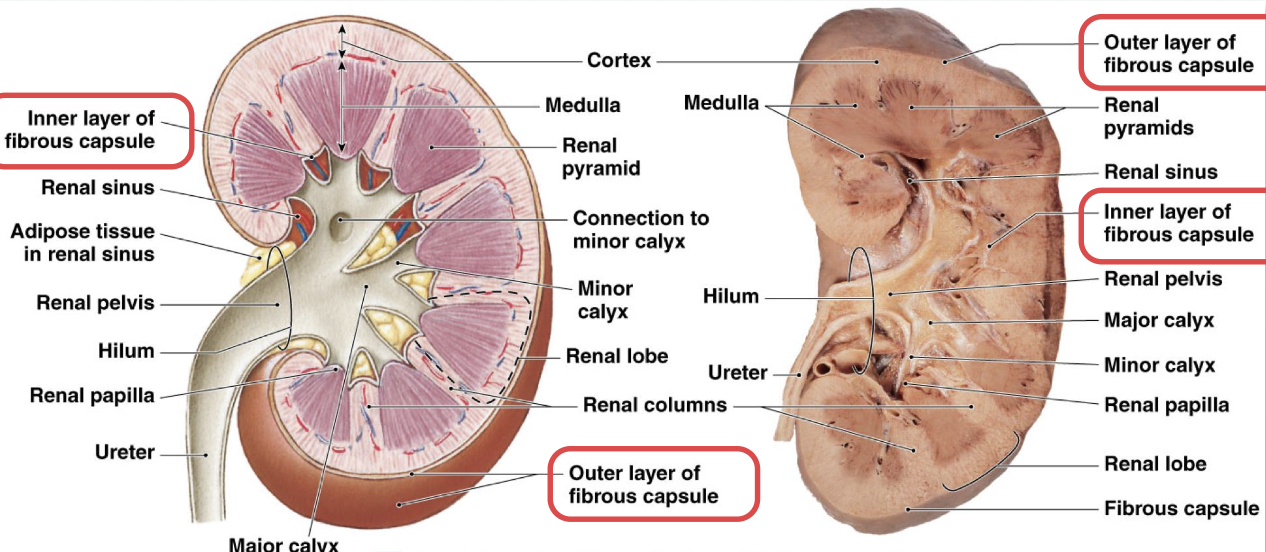
What does the Renal Medulla consist of?
Renal pyramids
Renal papillae
Renal columns
What does the Renal Sinus consist of?
Minor calyx
Major calyx
Renal pelvis
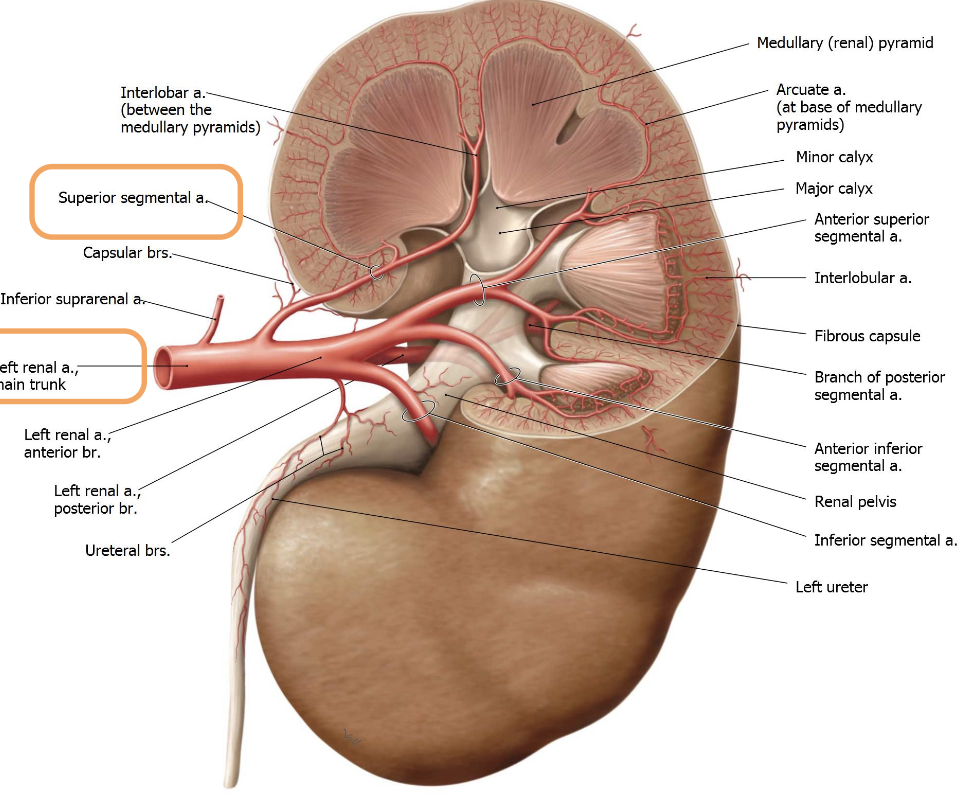
Describe the Renal Arteries.
→ originate directly from the aorta.
branch into segmental arteries and smaller vessels within the kidney
are “end arteries” — has no significant collateral circulation, so if one is blocked, that kidney segment dies
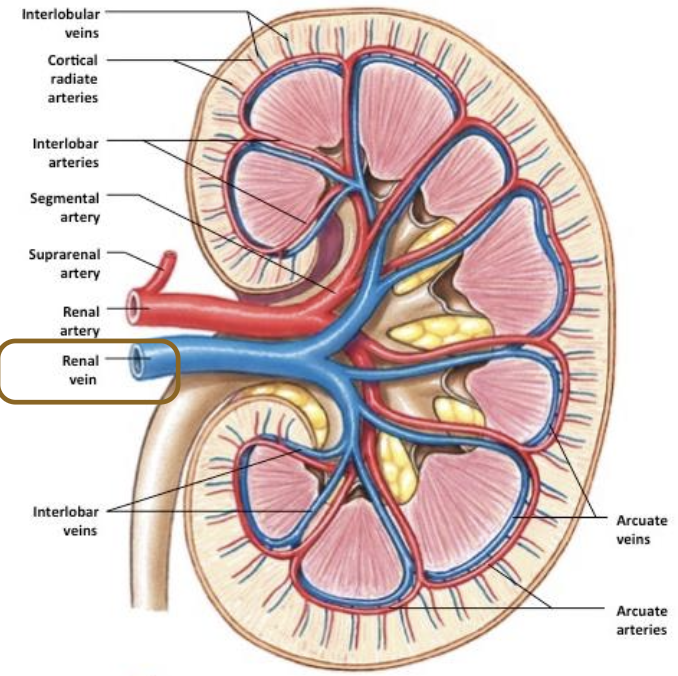
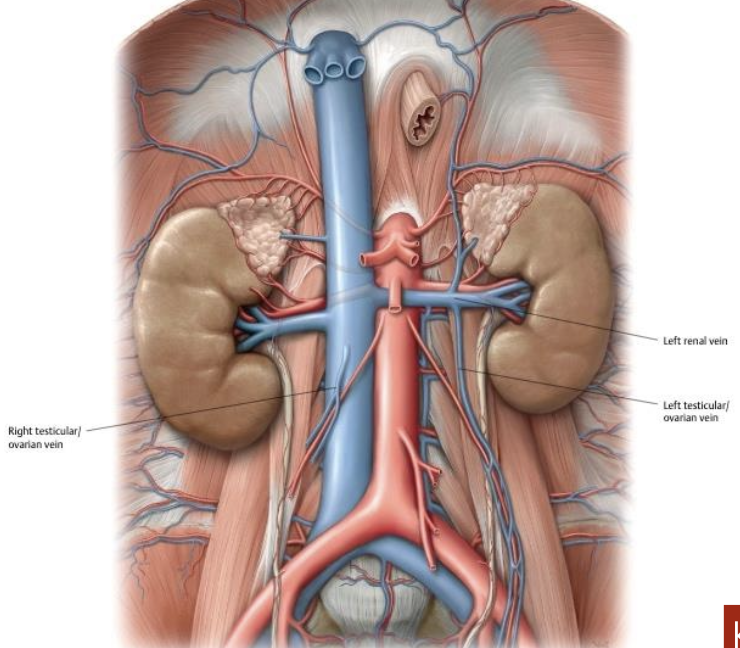
What is the function of the Renal veins? Outline venous drainage.
→ drain blood from kidneys into the inferior vena cava
Blood flows from interlobular veins → arcuate veins → interlobar veins → segmental veins → renal vein → IVC
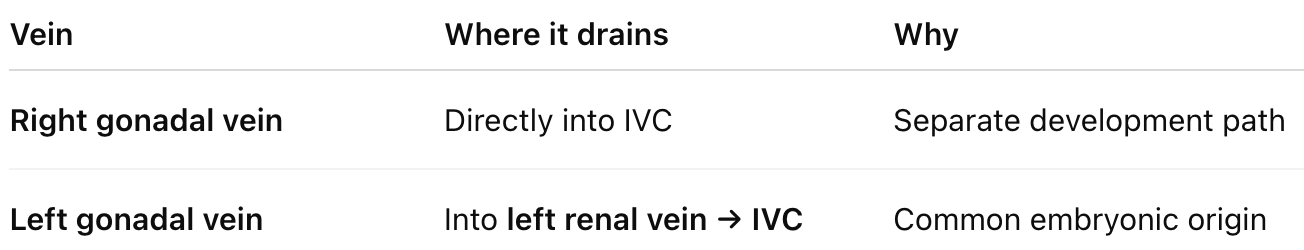
What special vein connection does the left renal vein have?
During development (embryology), the left gonadal (testicular or ovarian) vein & left renal vein come from the same embryonic vein
Left renal vein is longer
Right renal vein is shorter
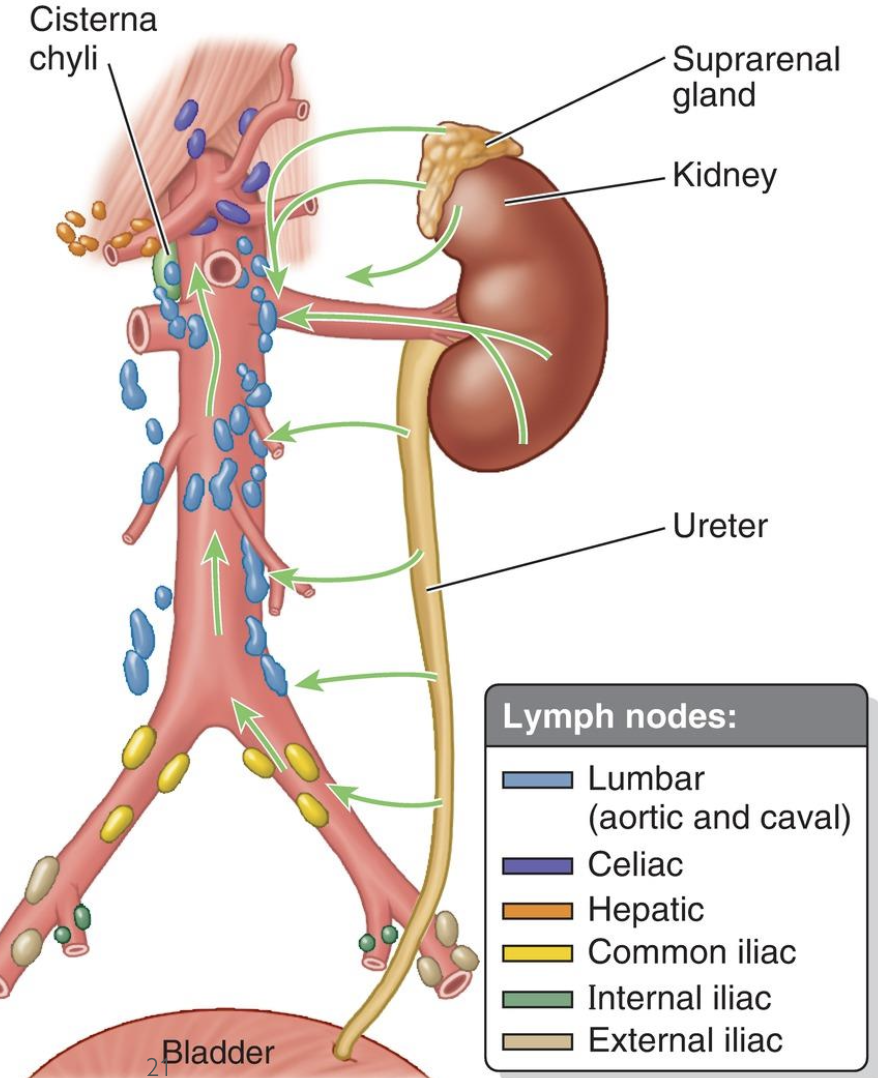
Describe renal lymphatic drainage.
Lymphatics follow the renal veins
Drain into the right and left lumbar (aortic) lymph nodes
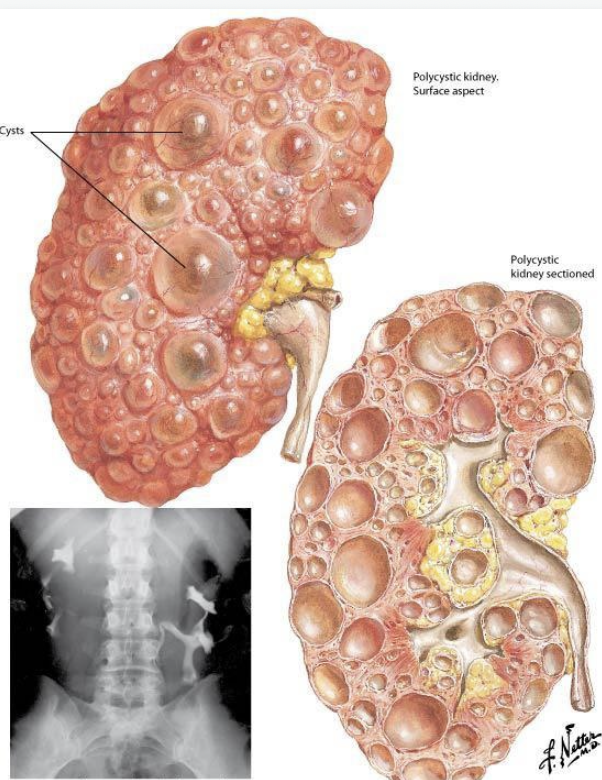
List some examples of anatomical variances you’ll see in kidneys.
Renal cysts
Variations in vasculature
List the Renal Functions.
1) Excretory - removes extra or harmful water-soluble substances in urine — especially toxic nitrogen wastes like ammonia and urea
2) Regulatory - maintains stable fluid volume & ion composition
regulates pH in conjunction with the lungs
3) Endocrine - produces and releases 3 hormones
What are the main features of the suprarenal (adrenal) glands?
aka adrenal glands
retroperitoneal
sits on the superior pole of each kidney, in front of the crura of the diaphragm
Shape
Right gland - pyramidal shape
Left gland - crescent shape
“2 in 1” glands – cortex and medulla have different functions and embryologic origins
Cortex: Mesoderm
Medulla: Neural crest cells
Function: neuroendocrine glands that respond to stress
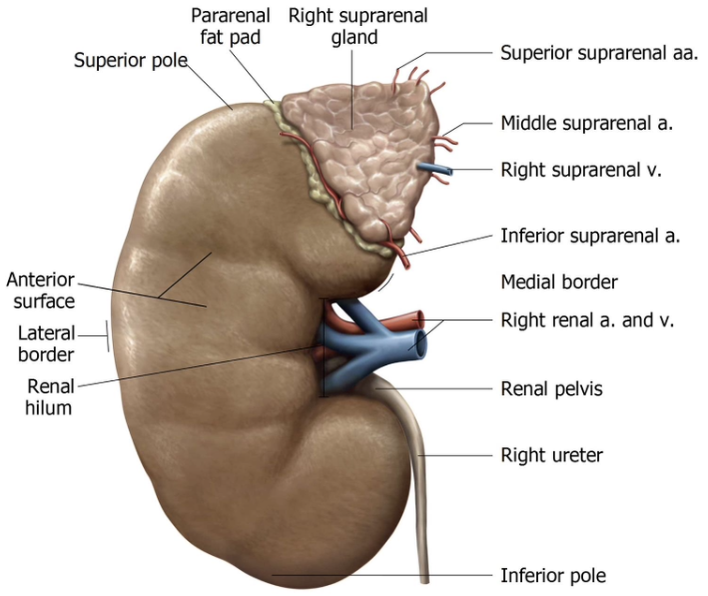
What are the key features of suprarenal (adrenal) gland vasculature?
Highly vascularized b/c hormones enter the venous bloodstream to reach targets
Suprarenal veins mainly drain into the renal veins
sometimes drain directly into the IVC
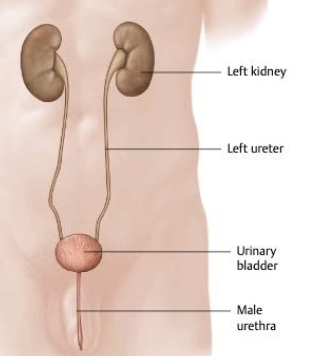
What are the characteristics of the Ureters?
Retroperitoneal organs
firmly attached to the posterior abdominal wall
pass through both the abdominal and pelvic regions
Exit the kidney at the hilum and extend to the urinary bladder
Urine moves through the ureters by peristalsis
What is the significance of ureter constrictions?
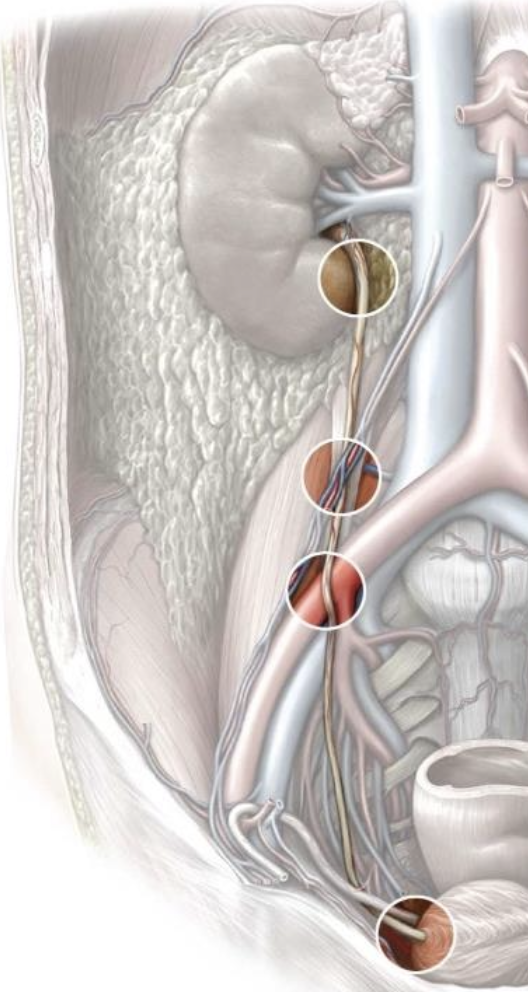
Common sites for obstruction (e.g., kidney stones)
BUT act as pseudovalves to slow urinary reflux
How is the 2nd constriction site of the ureter identified on imaging?
2nd constriction at the pelvic brim corresponds to the sacral promontory

What is an Intravenous Pyelogram (IVP) and how does it work?
uses iodine-based dye that’s injected intravenously
Dye is cleared by the kidneys, tracing the urinary pathway
Hazard: Possible reaction to iodine-based dye

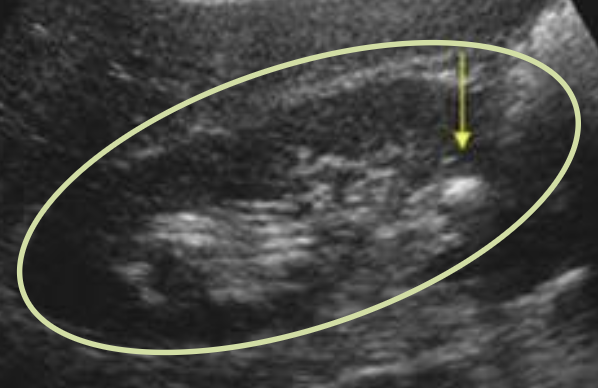
Why is ultrasonography used in urinary imaging?
Safer alternative to IVP for detecting urinary obstructions
can visualize kidneys and renal pelvis stones
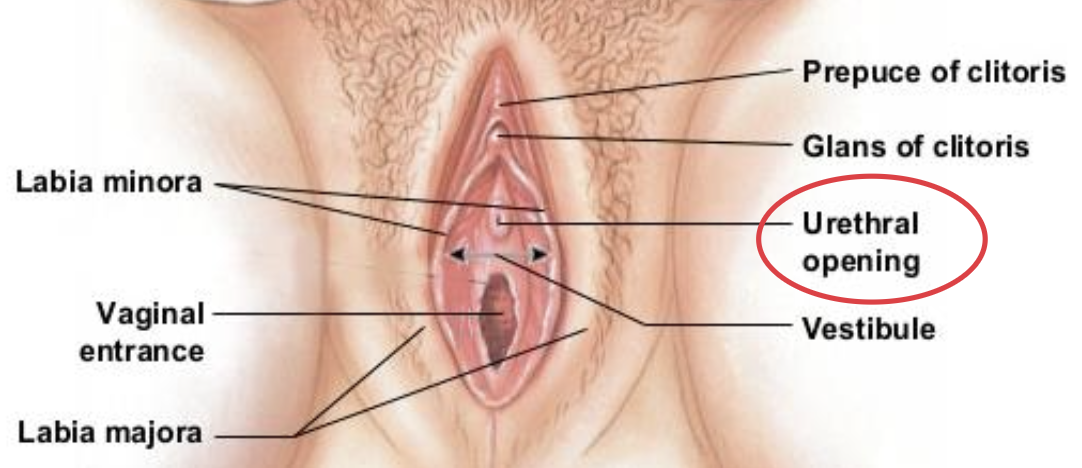
What are the characteristics of the female urethra?
Short & has no named parts
Short length makes UTIs more common in females b/c bacteria can reach the bladder more easily

Where is the opening of the female urethra located?
In the vestibule of the vulva (space between labia minora), above the vaginal opening
What are the characteristics of the male urethra?
→ Dual purpose: transmits urine & semen
18-22cm long (b/c it has a dual purpose) — extending from internal urethral orifice at bladder to glands of penis
Muscular conduit (uretha is part muscle to push fluid out actively)

List the 4 parts to the male urethra.
Preprostatic
Prostati
Membranous
Spongy
Parts of Male Urethra
What is the preprostatic urethra and what is its function?
Location: Neck of the bladder
Contains: Internal urethral orifice and internal urethral sphincter
Function:
SNS innervation closes sphincter during ejaculation
prevents backflow of semen into the bladder
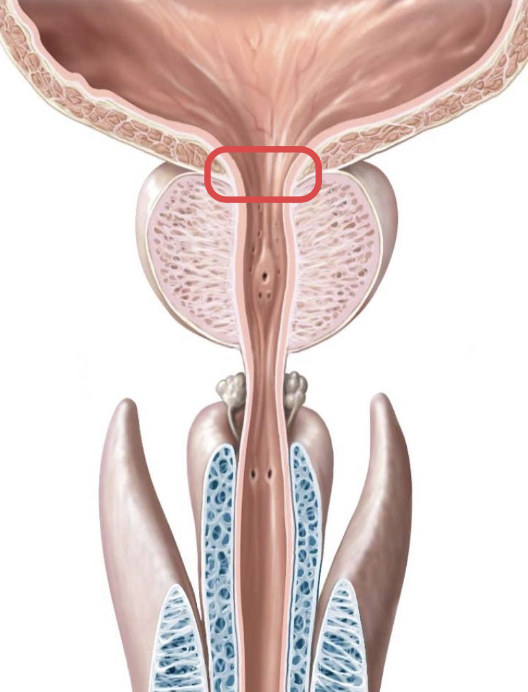
Parts of Male Urethra
Where is the prostatic urethra located?
Surrounded by prostate tissue, which contributes secretions to semen
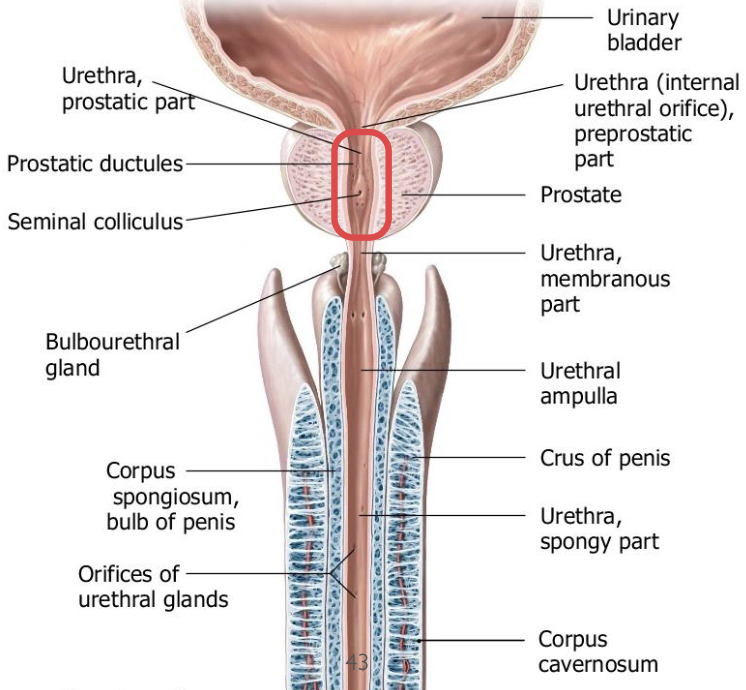
Parts of Male Urethra
What is the membranous urethra?
Shortest section of the male urethra
passes through the perineal membrane in the urogenital triangle
surrounded by the external urethral sphincter which allows for voluntary urine control
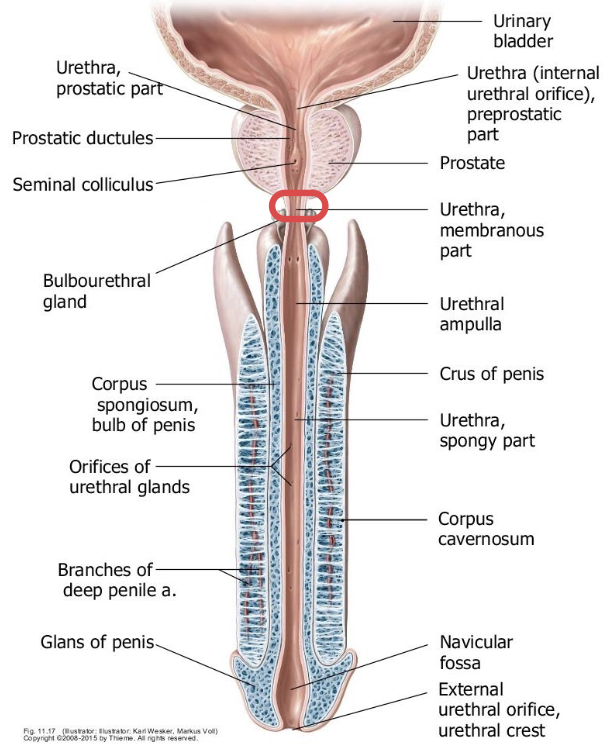
Parts of Male Urethra
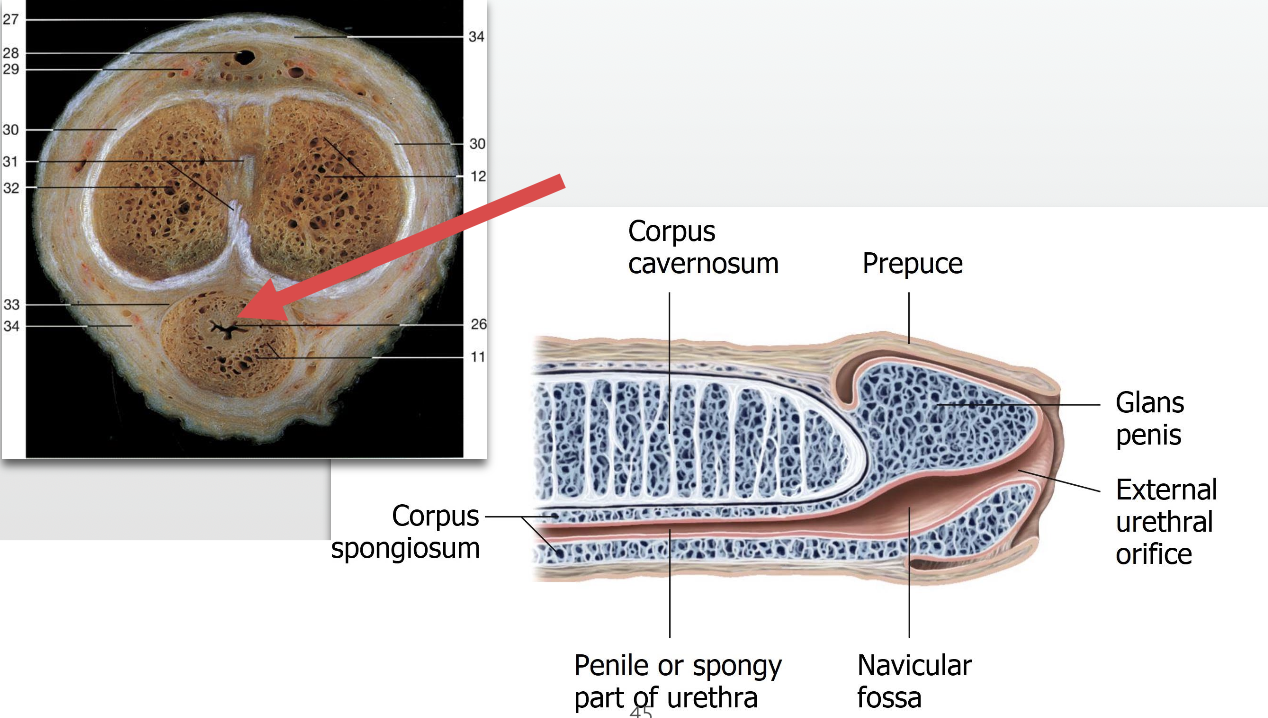
What is the spongy urethra?
aka: penile urethra
passes through the corpus spongiosum of the penis
Ends at the glans penis (external urethral meatus)
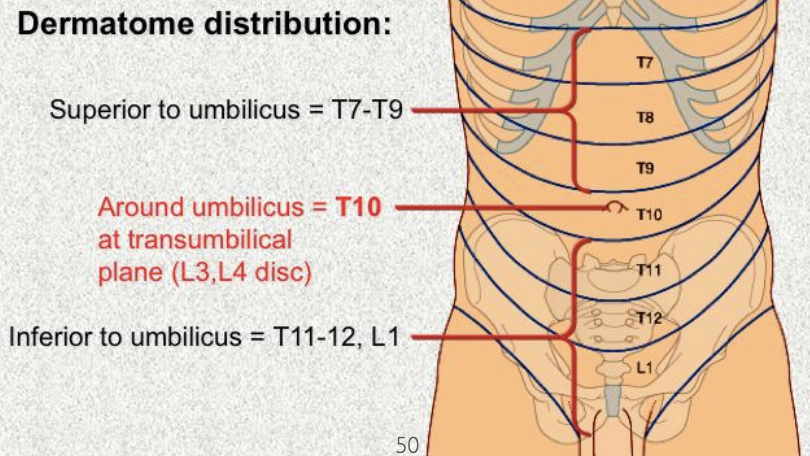
What is important to know about abdominal dermatomes vs spinal levels?
Ribs tilt downward anteriorly, so dermatomes don’t line up exactly with spinal levels
Ex: T10 dermatome at the umbilicus corresponds to the L3–L4 intervertebral disc
What is referred pain and why does it occur?
→ Pain from one organ is perceived in a different location
Causes:
shared neural pathways and ganglia
convergence of visceral & somatic afferent nerves in the spinal cord
only happens with organs that are supplied by autonomic (visceral) nerves
How is the peritoneum innervated and how does this affect pain?
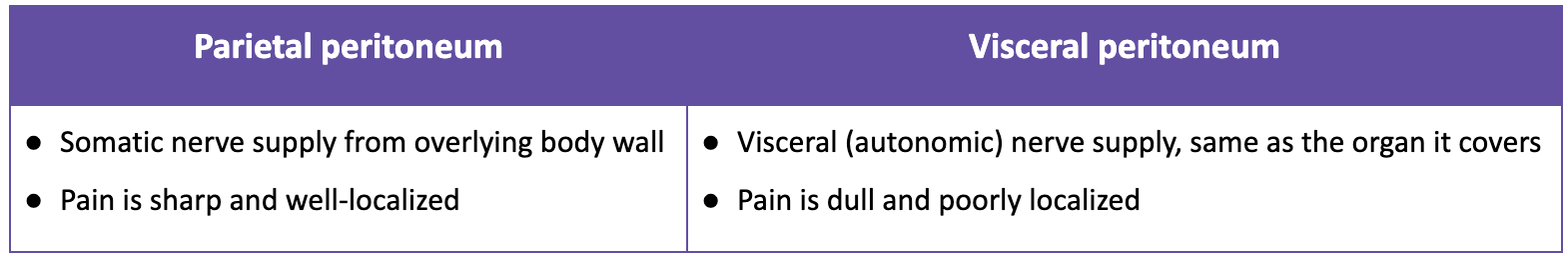
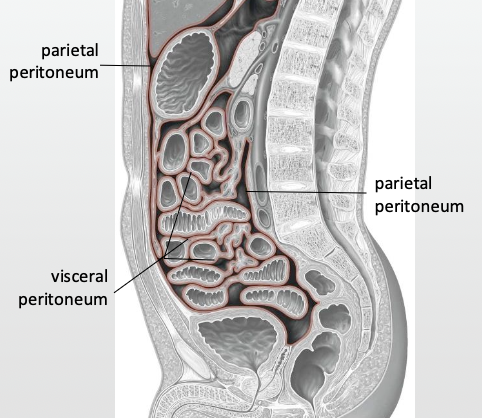
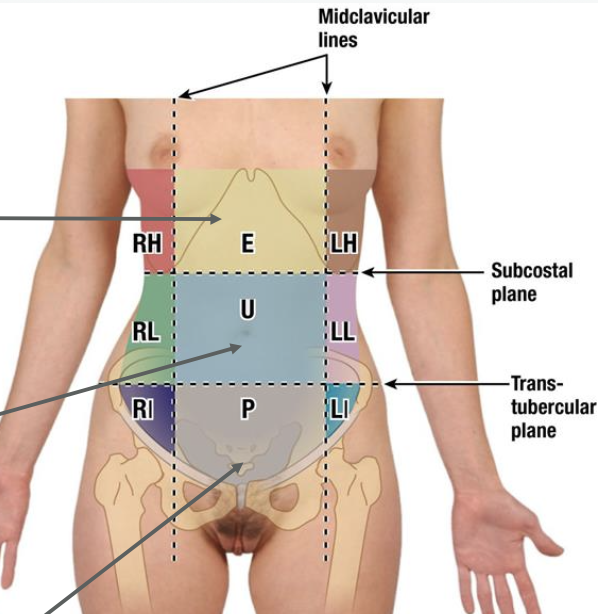
Where is abdominal visceral pain from different gut regions referred?
→ reffered to the middle line regions
Foregut: Epigastric region (upper midline)
Midgut: Umbilical region (midline)
Hindgut: Pubic/hypogastric region (lower midline)
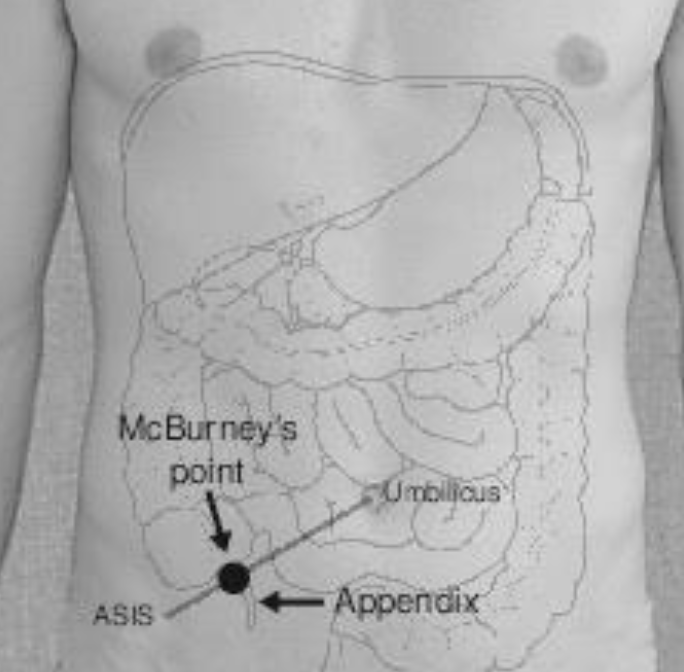
How does appendicitis cause pain, and why does it change location?
Origin: Inflammation of the appendix
Pain pattern:
Early: Periumbilical (visceral pain, T10 dermatome)
Later: Right lower quadrant at McBurney’s point (parietal peritoneum involvement)
Mechanism:
Visceral pain: Poorly localized, referred to midline (umbilicus)
Parietal pain: Somatic nerves activated → sharp, localized pain at actual site
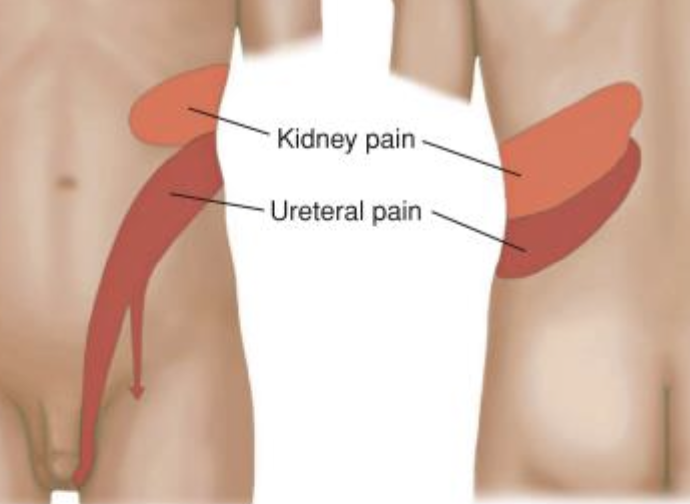
How does kidney stone pain present in the early stage and why? What dermatomes are involved?
→ Dull, aching pain in costovertebral angle (CVA) and flank
Caused by kidney distension from ureteral obstruction
Poorly localized b/c it’s visceral pain
Dermatomes: T10–L1

How does kidney stone pain present in the late stage and why? What dermatomes are involved?
→ Sharp, severe, colicky pain
Radiates along ureter: flank → lower abdomen → groin
Pain localizes as stone travels through ureter
Dermatomes: T11–L2
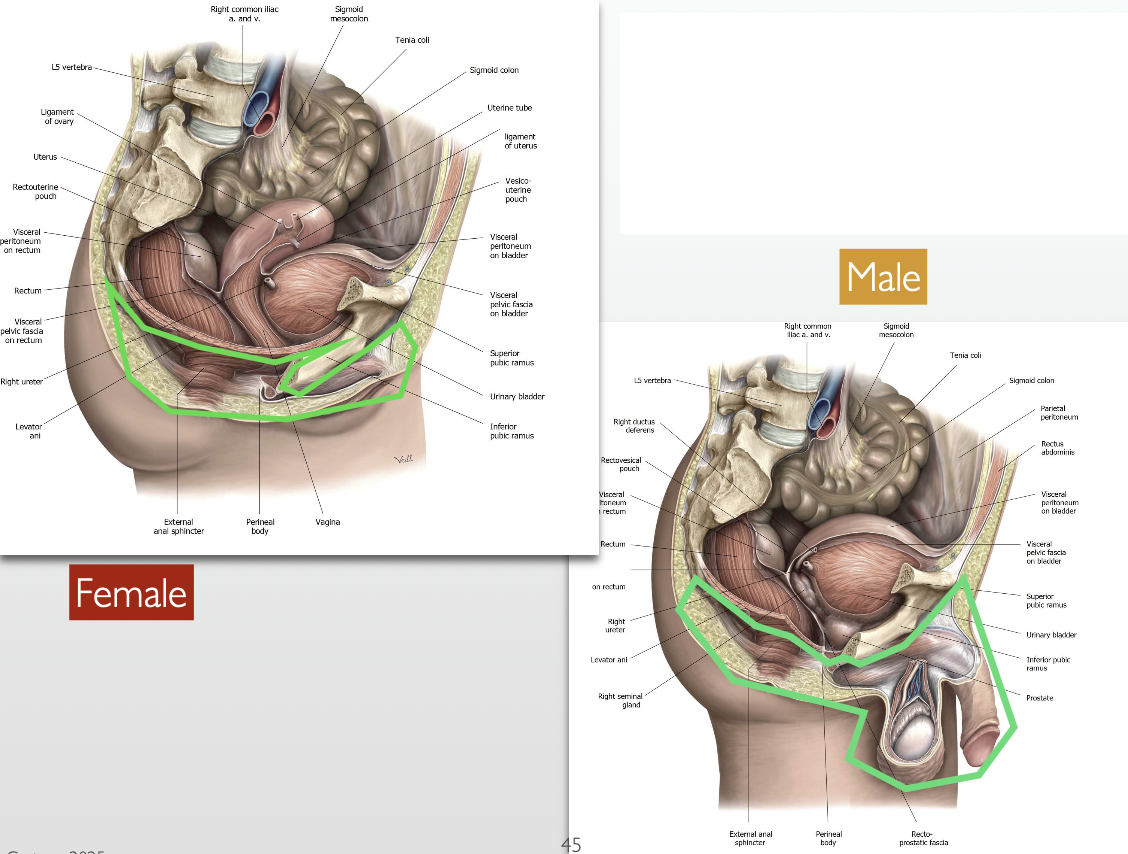
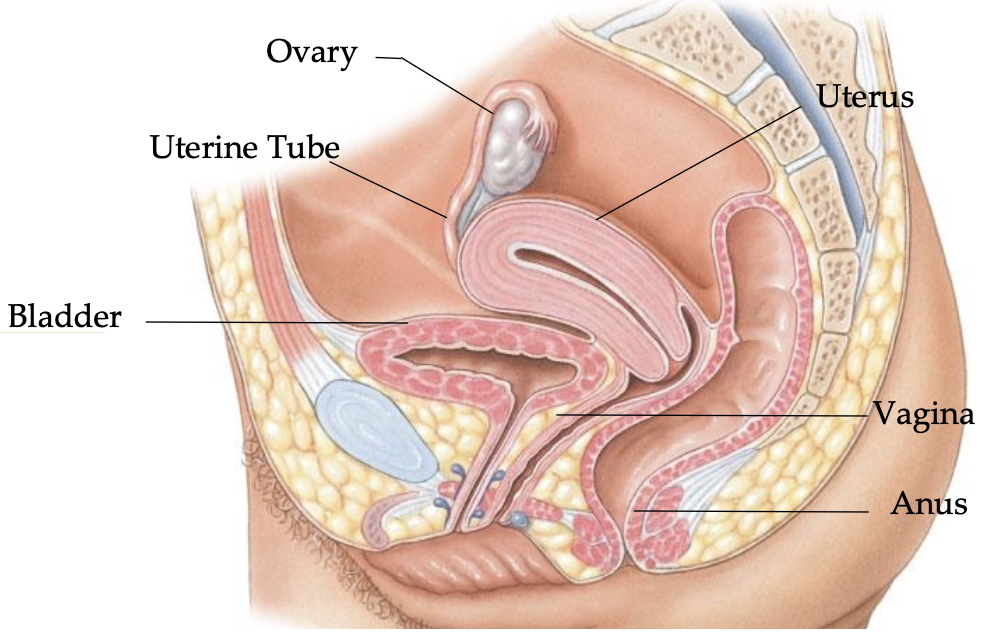
List the organs of the Pelvic Viscera.
Bladder (Urinary)
Ovary
Uterine Tube
Uterus
Vagina
Rectum
Anal Canal
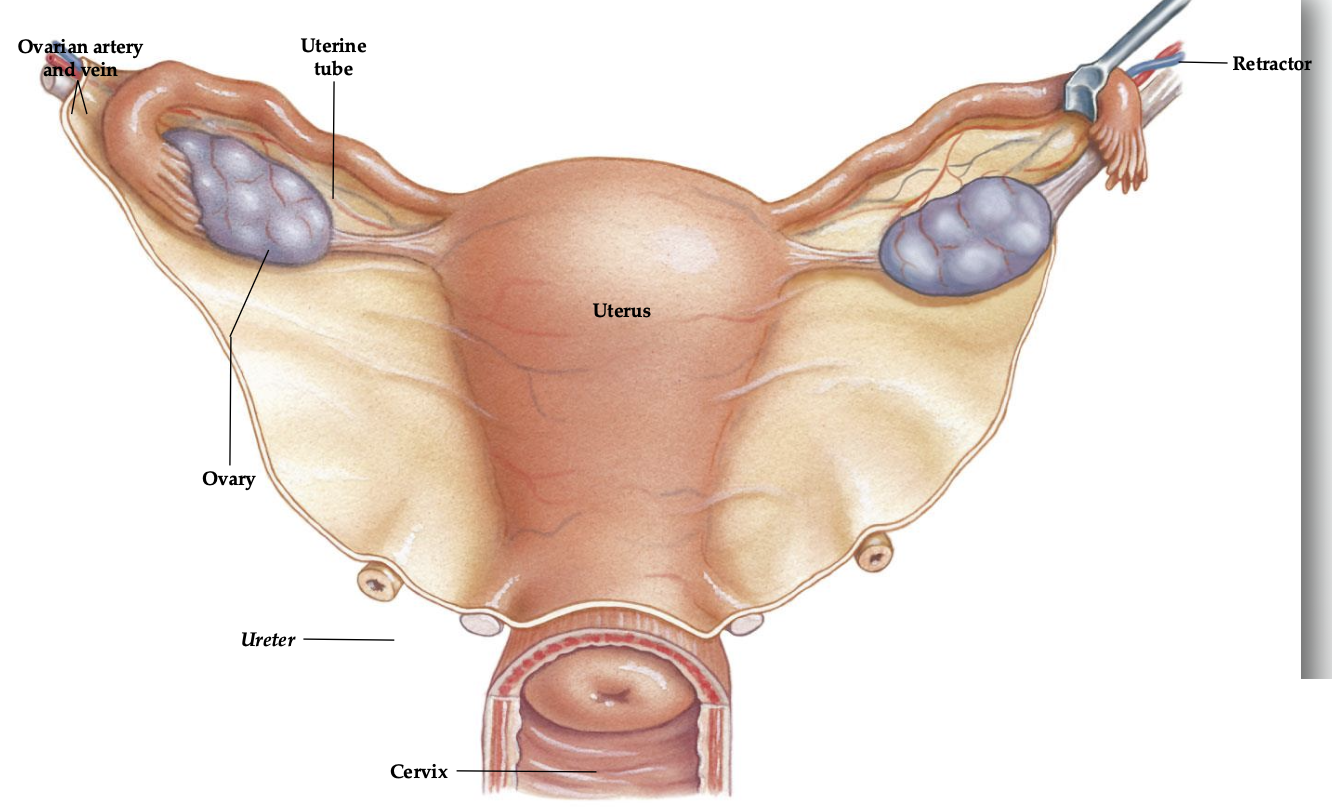
What do the ovaries produce and where does it go?
→ produce the ovum (egg) which travels through the uterine (fallopian) tube to the uterus
At ovulation, the fimbria swell to move closer to the ovary to optimize capture of the ovum

List the main pouches in the female pelvis.
Rectouterine pouch
Vesicouterine Pouch

What are the key features and functions of the Uterus?
Shape & size: Pear-shaped, ~7 cm long, 5 cm wide, 3 cm thick
Functions:
Protects the embryo
Provides nutritional support
Removes waste produced by the embryo
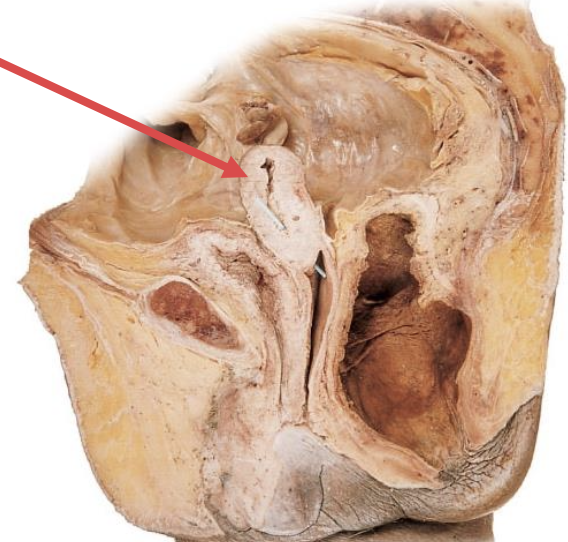
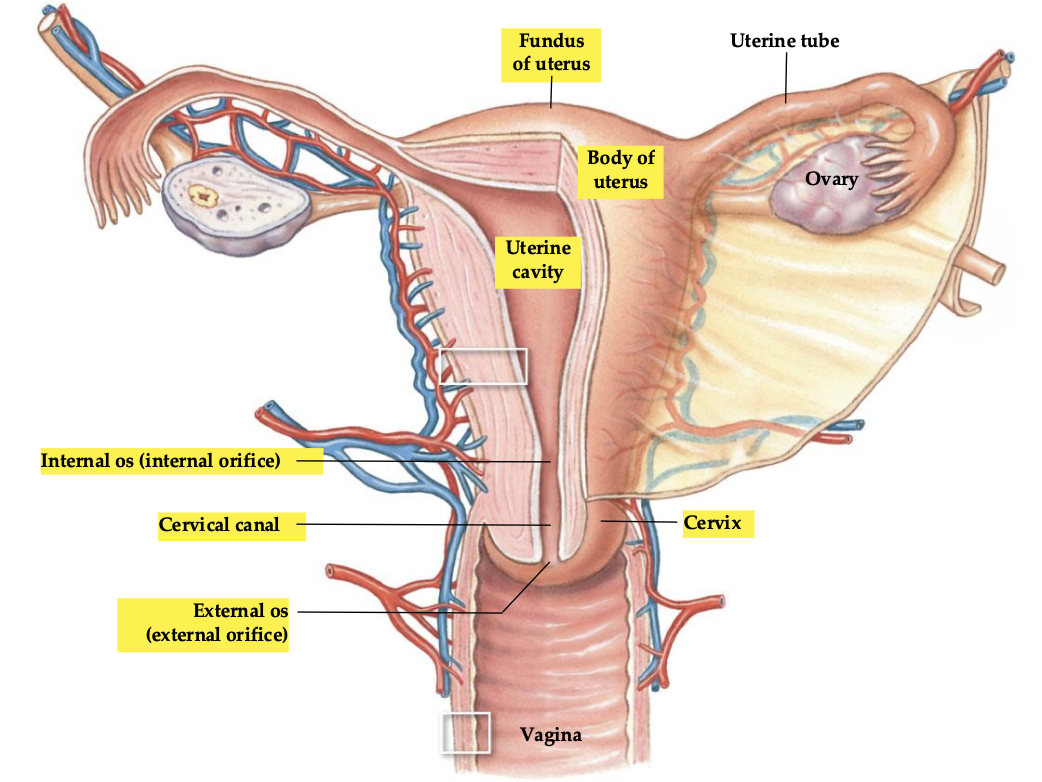
List the main anatomical landmarks of the uterus.
Fundus
Body
Uterine cavity
Cervix
External orifice
Cervical canal
Internal orifice
How does pregnancy affect vision and why?
Caused by hormonal changes (estrogen, progesterone, relaxin) → leads to ↑ corneal thickness & curvature
resolves 6–8 weeks postpartum
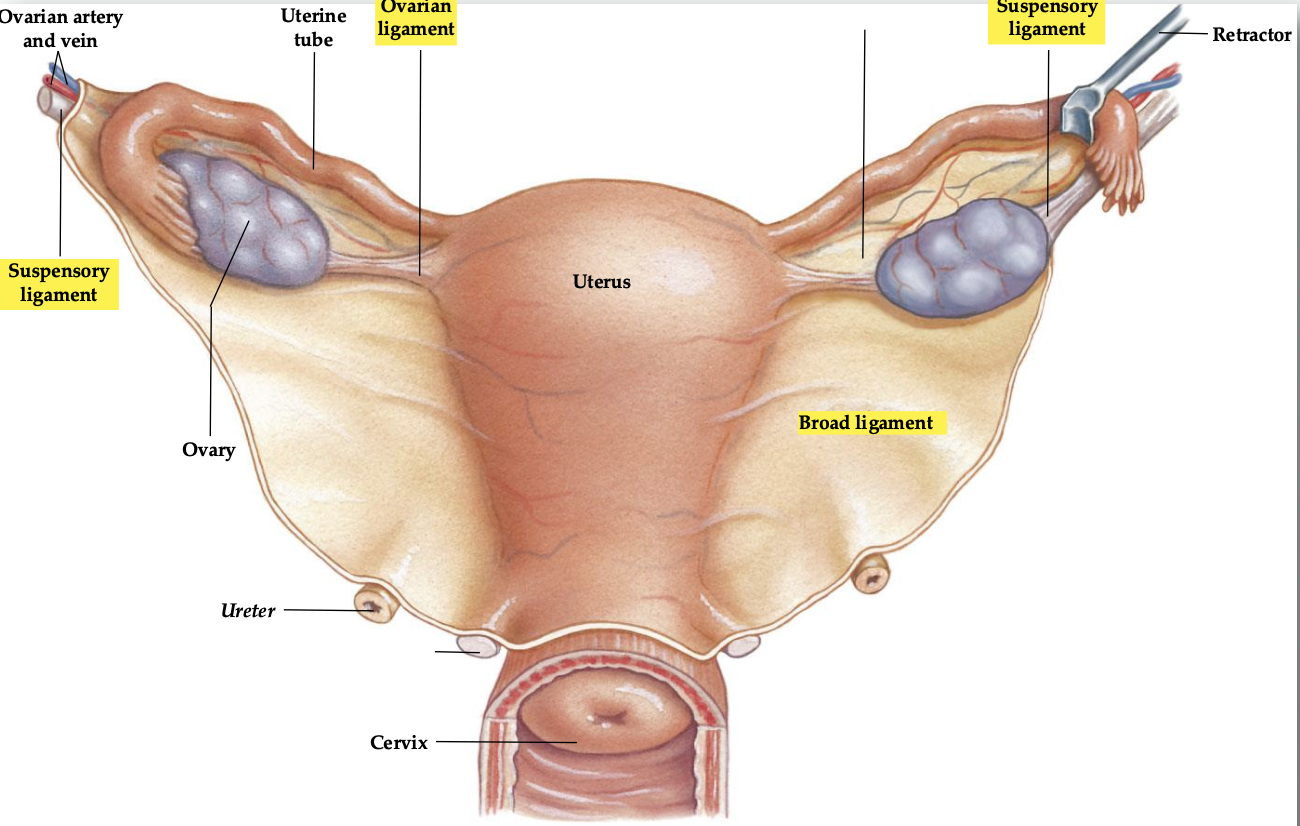
List the major ligaments that support pelvic organs and their functions.
Broad ligament: sheet-like, provides major support to pelvic organs
Ovarian ligament: stabilizes the ovary
Suspensory ligament: supports the ovary and vessels
Round ligament: restricts posterior movement of the uterus
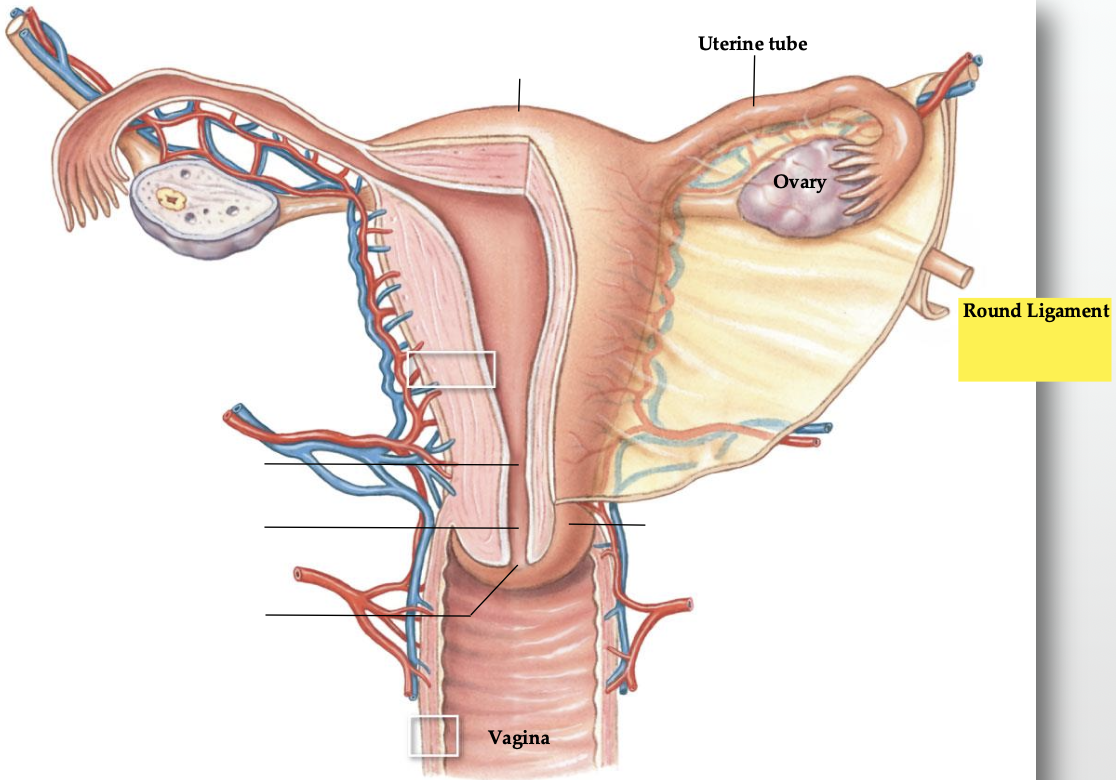
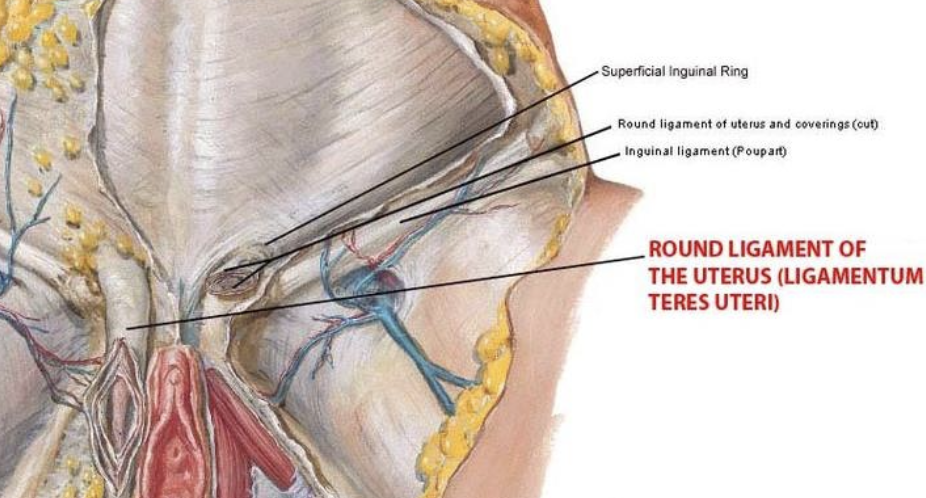
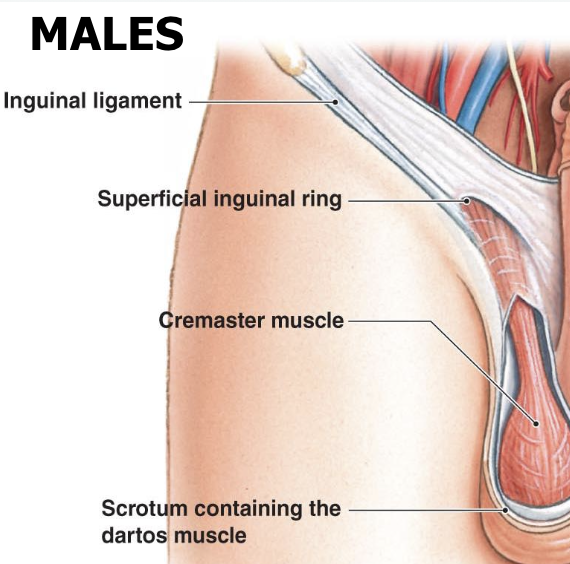
What is the female inguinal canal and its significance?
Passes the round ligament of the uterus (female analogue of spermatic cord)
Anchors into the abdominal wall
Clinical note: Smaller opening → less likely to develop hernia (ratio ~8:1 compared to males)
List the major organs of the Pelvic viscera of males.
Testes
Prostate & accessory glands
Ductus deferens
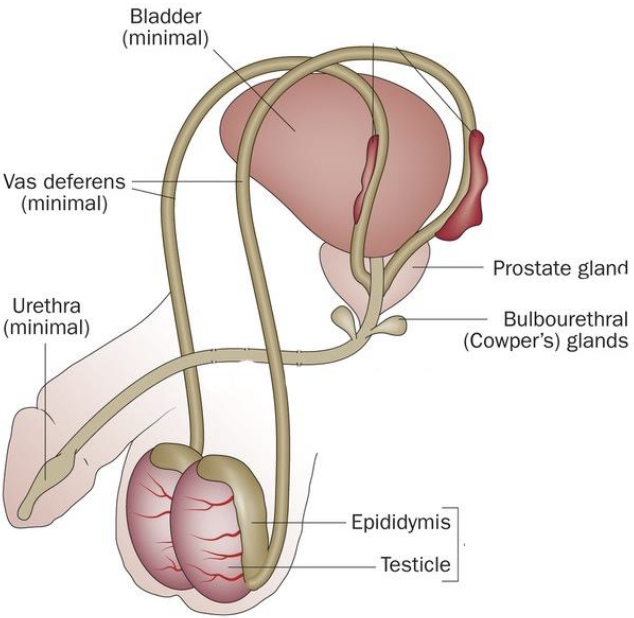
How does sperm travel through the male urogenital system?
Testes
Ductus (Vas) deferens
Ejaculatory duct (formed by ductus deferens and seminal vesicle duct)
Prostatic urethra (within the prostate) + cowper’s glands
Membranous urethra (through pelvic floor)
Spongy/penile urethra
Navicular fossa
External urethral orifice
List the main pouches in the male pelvis.
Rectovesical pouch
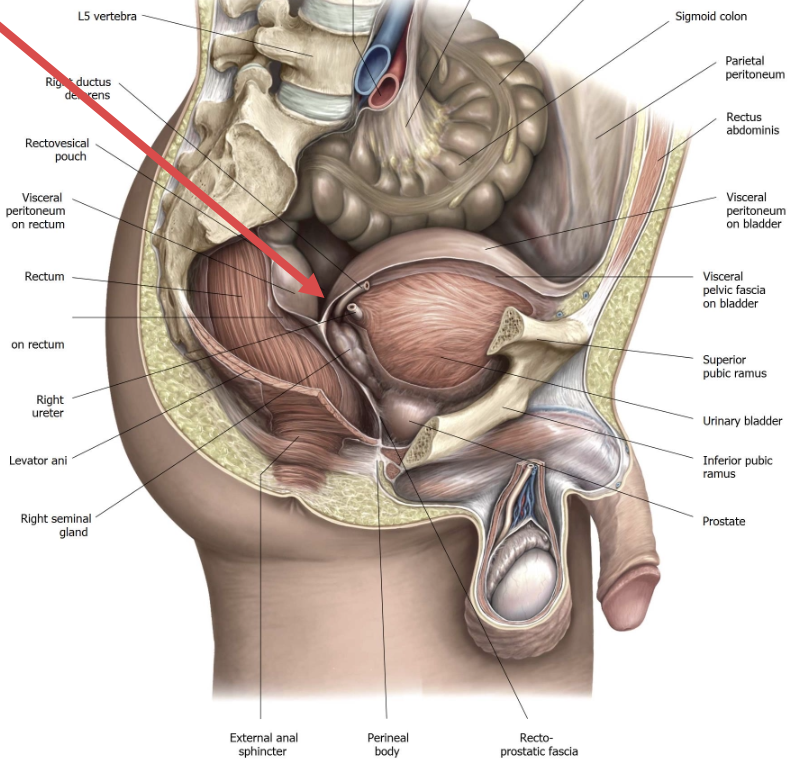
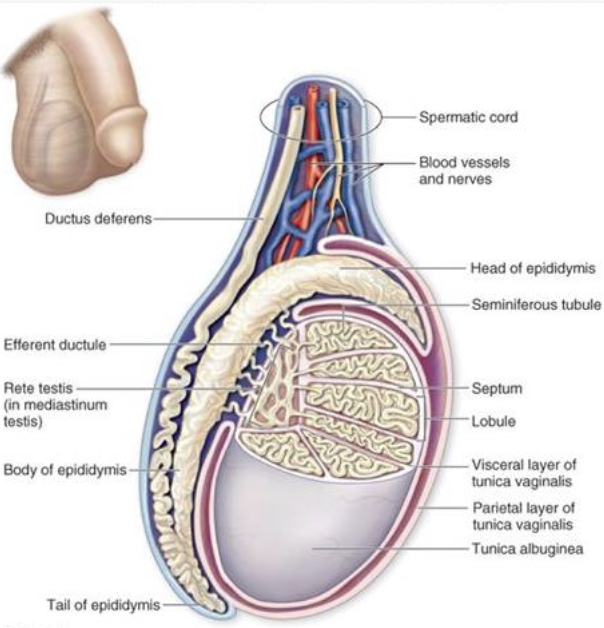
Where is sperm produced? How does it travel from the testes?
Production: seminiferous tubules of the testes
Efferent ductules
Epididymis
Ductus deferens through abdominal wall
Note: Epididymis feels like an elongated lump; normal on self-exam
What is the ductus deferens and what was its former name?
→ Fibromuscular tube carrying sperm from testes to prostate
Former name: Vas deferens
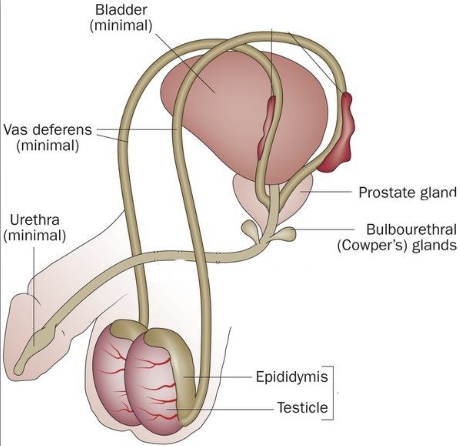
What is the largest accessory reproductive glands? Describe it
Prostate
has a fibromuscular capsule
surrounds the prostatic urethra
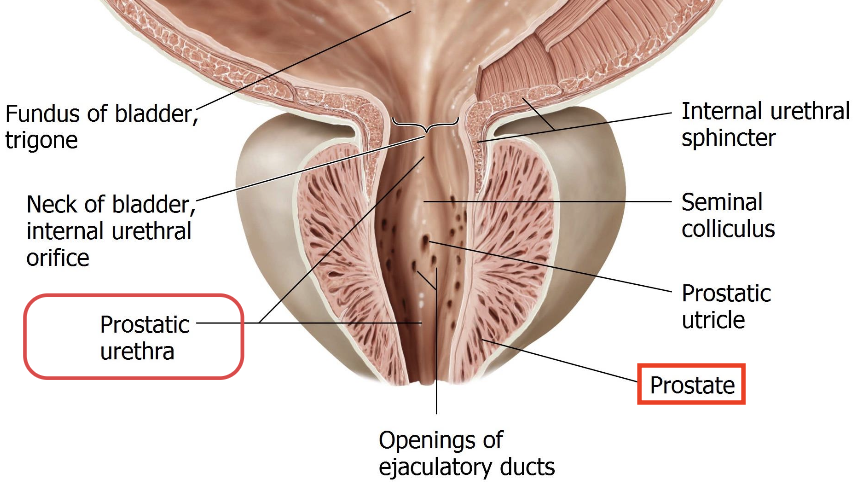
What is benign prostatic hyperplasia (BPH) and how is it treated?
→ age-related enlargement (hyperplasia) of the prostate
constricts urethra → urinary retention + constant urge to pee
Treatment: Alpha-blockers (e.g., Flomax® / tamsulosin)
How does Alpha-blockers affect the eyes?
Causes Intraoperative Floppy Iris Syndrome (IFIS)
reduces effective pupil dilation before and during cataract surgery
e.g., cause the pupil to suddenly constrict during surgery
Note: Stopping medication before cataract surgery may not prevent IFIS

What is the Perineum?
shallow compartment inferior to the pelvic floor