Capillary Exchange: Microcirculation and Lymphatics
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
72 Terms
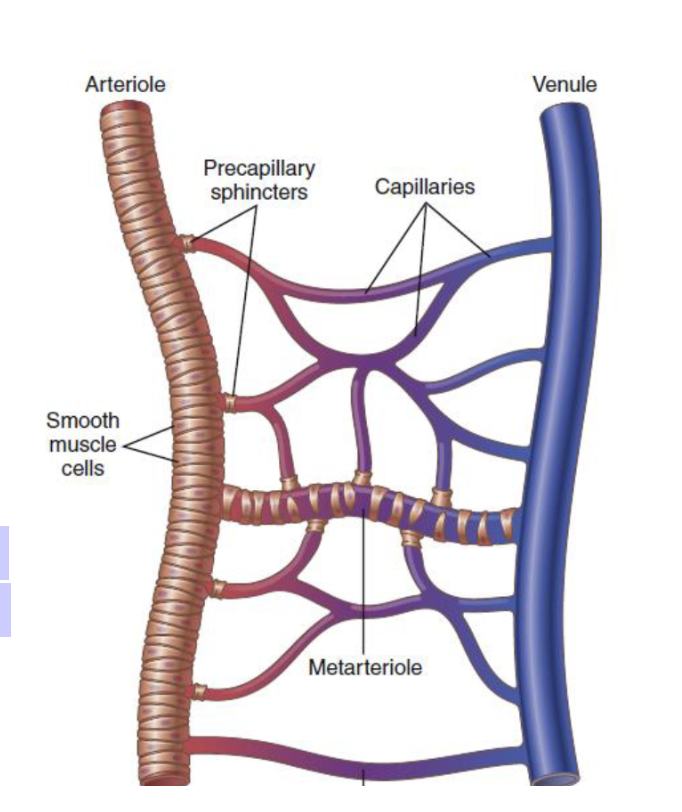
What is microcirculation?
to the functions of the smallest blood vessels, the capillaries, and the neighboring lymphatic vessels.
What structures are involved in microcirculation?
Capillaries and neighboring lymphatic vessels.
What is the main function of microcirculation?
The transport of nutrients to the tissues and the removal of cell excreta.
microcirculation
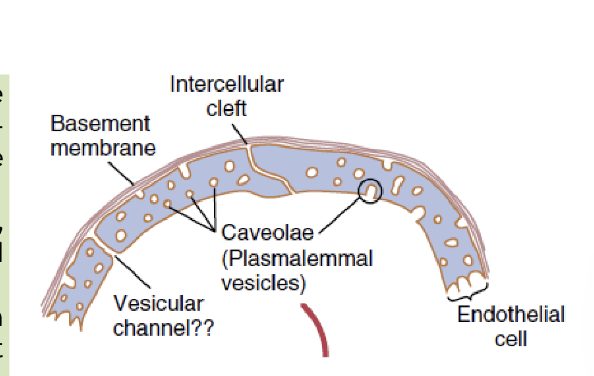
What are capillary walls made of?
A single layer of highly permeable endothelial cells.
Why are capillary walls highly permeable?
To allow quick and easy interchange of water, cell nutrients, and cell excreta.
What allows for the rapid exchange of substances in the capillaries?
Their thin walls made of a single layer of permeable endothelial cells.
How is microcirculation adapted in each organ?
It is organized to serve that organ’s specific needs.
structure of microcirculation
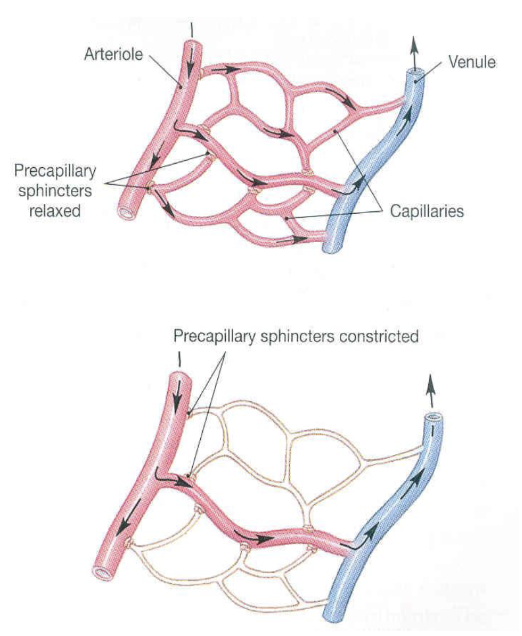
What is vasomotion?
The intermittent flow of blood in the capillaries, turning on and off every few seconds or minutes.
What causes the intermittent flow of blood in capillaries?
Intermittent contraction of the metarterioles and precapillary sphincters.
What regulates vasomotion?
The concentration of oxygen in the tissues.
What structures control the opening and closing of capillary blood flow?
Metarterioles and precapillary sphincters.
flow of blood in the capillaries
What are the three main types of capillaries classified by permeability?
Continuous, Fenestrated, and Sinusoidal.
What type of capillary is found in skeletal muscle, lungs, and brain?
Continuous capillaries
What special feature do continuous capillaries in the brain have?
Tight junctions (part of the blood-brain barrier)
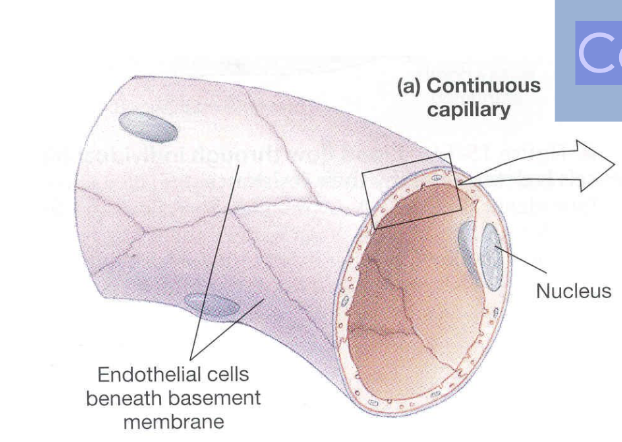
continuous capillary
Where are fenestrated capillaries commonly found?
In the renal glomerulus and intestines.
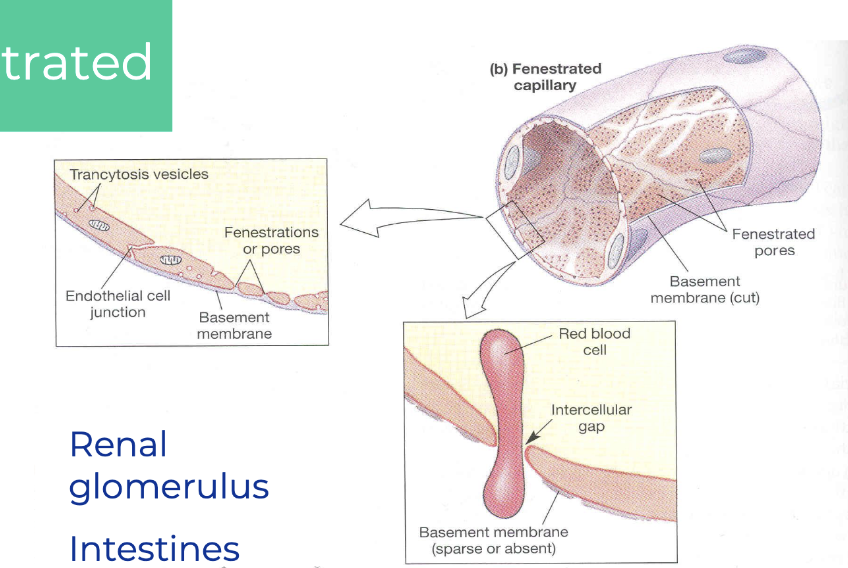
fenestrated capillaries
Where are sinusoidal capillaries found?
In the liver (microvilli of hepatocytes), spleen, lymph nodes, and bone marrow.
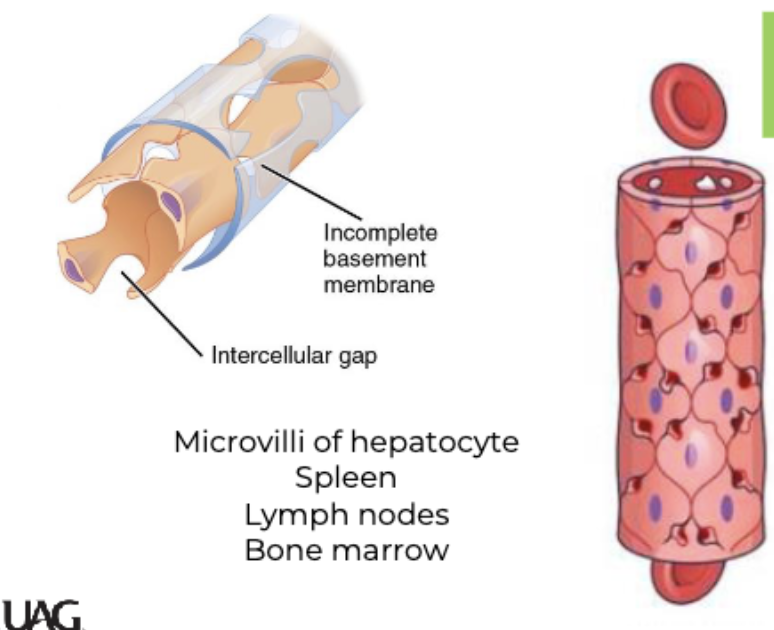
sinusoidal
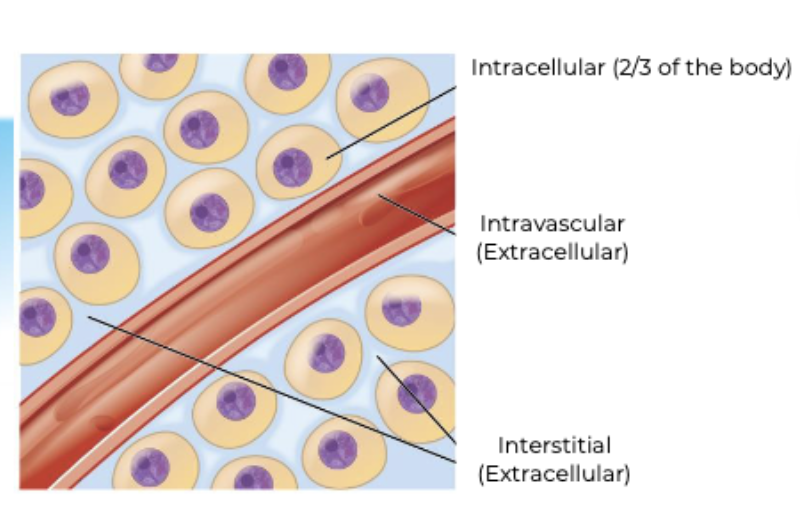
Where is most of the water in the human body located?
Inside the cells — Intracellular fluid (ICF), which makes up about 2/3 of total body water.
What are the two main components of extracellular fluid (ECF)?
Intravascular fluid (within blood vessels/plasma) and interstitial fluid (between cells).
What is the primary function of the lymphatic system?
It serves as an accessory route for fluid to flow from the interstitial spaces into the blood.
What is lymph?
Lymph is fluid derived from interstitial fluid that enters the lymphatic vessels.
How does the composition of lymph compare to interstitial fluid?
When lymph first enters the terminal lymphatics, it has almost the same composition as interstitial fluid.
Where does lymph originate?
From the interstitial fluid surrounding the tissues.
Through what structures does interstitial fluid become lymph?
Through the terminal lymphatics.
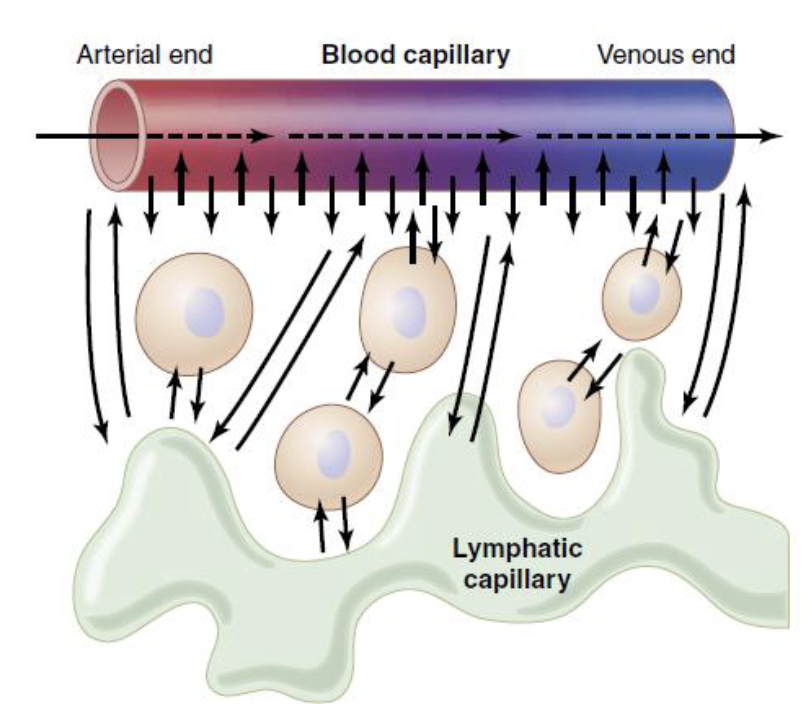
What is hydrostatic pressure?
The fluid pressure that pushes water out of the capillaries into the interstitial space.
What is colloid osmotic (oncotic) pressure?
The pressure exerted by solutes, mainly proteins, that pulls water into the capillaries from the interstitial space.
What are Starling forces?
The competing forces between hydrostatic pressure and oncotic pressure that determine the movement of fluid across capillary membranes.
What happens when hydrostatic pressure is greater than oncotic pressure?
Fluid moves out of the capillaries (filtration).
What happens when oncotic pressure is greater than hydrostatic pressure?
Fluid moves into the capillaries (reabsorption)
What does the Starling equation calculate?
Net fluid movement (Jv) across capillary membranes.
What is the Starling equation?
Jv = Kf [(Pc − Pi) − (πc − πi)]
In the Starling equation, what does Jv represent?
Jv = fluid movement (positive = filtration, negative = absorption).
What does Kf represent in the Starling equation?
Hydraulic conductance (a measure of membrane permeability).
What does Pc represent in the Starling equation?
Capillary hydrostatic pressure
What does Pi represent in the Starling equation?
Interstitial hydrostatic pressure
What does πc (pic) represent in the Starling equation?
Capillary oncotic pressure (due to plasma proteins)
What does πi (pii) represent in the Starling equation?
Interstitial oncotic pressure
What happens when Jv is positive?
Net filtration – fluid moves out of the capillary.
What happens when Jv is negative?
Net absorption – fluid moves into the capillary.
What does Pc stand for in capillary dynamics?
Capillary pressure - the pressure exerted by blood against the capillary walls, promoting filtration out of the capillary.
What is the function of capillary pressure Pc?
It drives fluid out of the capillaries into the interstitial space.
What does Pif stand for?
interstitial fluid pressure - the pressure exerted by the interstitial fluid on the outside of the capillary wall
What effect does Pif usually have on fluid movement?
it opposses filtration by pushing fluid back into the capillariesw
what does np represent?
Plasma colloid osmotic pressure - the osmotic pull exerted by plasma proteins to draw water into the capillaries.
What is the role of np in fluid exchange?
it promotes reabsorption of the fluid into the capullaries.
what does nif stand for?
interstitial fluid colloid osmotic pressure- the osmotic pull exerted by proteins in the interstitial fluid
how does nif affect fluid movement?
it promotes movement of fluid out of the capillaries into the interstitial space.
what is the starling equation used to determine?
the net movement of fluid across capillary membranes (filtration or reabsorption)
At the arterial end of the capillary, what is the net filtration pressure?
13 mmHg out
At the venous end of the capillary, what is the net reabsorption pressure?
7 mmHg in
What is the blood hydrostatic pressure at the arterial end?
30 mmHg out
What is the interstitial hydrostatic pressure at both ends of the capillary?
+3 mmHg out
What is the net hydrostatic pressure at both ends?
33 mmHg out (arterial) ; 13 mmHg out (venous)
What is the colloid osmotic pressure of blood at both ends?
28 mmHg in
What is the colloid osmotic pressure of tissue fluid (interstitial) at both ends?
8 mmHg out
What is the net oncotic pressure at both ends?
20 mmHg in
according to the Starling forces, what happens at the arterial end of the capillary?
Net filtration occurs (fluid leaves the capillary)
what occurs at the venous end of the capillary according to the Starling forces?
net reabsorption occurs (fluid enters the capillary)
What is the formula used to calculate net filtration pressure (NFP)?
NFP = (Pc + πi) - (Pi + πp)
Where:
Pc = Capillary hydrostatic pressure
πi = Tissue oncotic pressure
Pi = Tissue hydrostatic pressure
πp = Plasma oncotic pressure
Given Pc = 32 mmHg, πi = 0 mmHg, Pi = -2 mmHg, and πp = 29 mmHg, what is the net filtration pressure?
NFP = (32 + 0) - (-2 + 29) = 32 - 27 = 5 mmHg outward
What does a positive net filtration pressure indicate?
It indicates filtration, meaning fluid is moving out of the capillaries into the interstitial space.
What does a negative net filtration pressure indicate?
It indicates reabsorption, meaning fluid is moving into the capillaries from the interstitial space.
Which pressures promote fluid movement out of the capillaries?
Capillary hydrostatic pressure (Pc) and tissue oncotic pressure (πi)
Which pressures promote fluid movement into the capillaries?
Plasma oncotic pressure (πp) and tissue hydrostatic pressure (Pi)
What is the effect of a tissue hydrostatic pressure (Pi) that is negative (e.g., -2 mmHg)?
It increases outward movement of fluid (promotes filtration).