2. nutrition assessment and body composition
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
68 Terms
what is NCP?
A systematic, problem-solving method that registered dietitians use to critically assess and make decisions to address nutrition-related problems and provide safe and effective quality nutrition care
what is the most important part of the NCP
nutrition assessment
steps in nutrition assessment
Nutrition Assessment
Nutrition Diagnosis
Nutrition Intervention
Nutrition Monitoring and Evaluation
how does one initiate the nutrition assessment and why?
initiated by referral or screening
There can be many different reasons for referral
Under fueling, over fueling, post-surgery care, cramping
nutrition assessment
format
where information comes from
Face-to-face (in-person or virtual) with athlete
Additional info from athletic trainers, coaches, family
reasons for referral to sport dietitian
Lack of energy
Changes in body weight → both major and minor weight loss and gain
Persistent injuries (seen a lot with underfueling)
Abnormal biochemical data indicating possible nutrition etiology
Self-referral
This is totally different to the other referral types due to motivational differences
nutrition assessment components
ABCDE
Anthropometrics including weight history
Biochemical (blood and urine)
Clinical including nutrition-focused exam
Dietary assessment - most difficult but most important
Exercise/Energy Expenditure
what are biochem test
Measurement of nutrient and metabolite levels in the blood and urine
standard panel (biochem) includes what (4)
Complete blood count
Comprehensive metabolic panel with lipids
Endocrine markers
Urinary analysis
when should specific nutrients be assess
if deficiency is indicated
what are the potential deficiencies in athletes (3 main categories)
oxygen carrying nutrients
bone-building nutrients
hydration status
oxygen carrying nutrients of risk include what
iron, folic, vit b12
bone-building nutrients nutrients of risk
vit D and calcium
hydration status importance (like for biochem exams)
Can negatively impact performance
Can also alter the result of key biochemical tests
Include plasma osmolality, urine osmolality and urine specific gravity to ensure your athlete is not dehydrated during the testing
purpose of nutrition focused exam
To uncover any medical condition or physiological factor that may interfere with food intake, digestion, and metabolism
what issues can be found by nutrition focused exam
Recent or chronic illnesses, recent or persistent injuries
Anxiety and/or depression
GI issues
Physical signs of malnutrition
Muscle wasting, dry and brittle finger nails, bony protrusions, clubbed fingers
what is the most important skills for sport RDN to develop
dietary assessment
accurate dietary assessment allows the sports RDN to:
Accurately screen + diagnose nutrition-related issues
Highlight nutrient timing issues that hinder performance or recovery
Optimize fueling and hydration to fully address the issue and/or help the athlete achieve athletic goals
what are the dietary recall tools (4)
24-hour Dietary Recall
Food Frequency Questionnaire (FFQ)
Diet History (combo of 24-h recall + FFQ)
3-day Food Records or Diet Logs
what are important things to consider for nutrition assessment (6)
Weight history (how has weight changed)
Fluid and electrolytes (enough water, electrolytes?)
Dietary supplements and medications
Environment, access to food, cooking facilities and competency
Knowledge, beliefs, and attitudes
Eating behaviors
24 hour recall
what is it
who does it
The athlete is asked to describe all foods and beverages consumed during the previous 24 hours,
form is filled out by the dietitian
strengths (3) and limitations (3) of 24hr recall
Strengths: quick and easy, low burden
Limitations:
Memory and recall bias
Previous day may not be representative of typical diet or typical training day
Snacks and beverages, condiments, cooking oils + seasonings
24 hr tips to make it better (3)
Experience is key
Build rapport to improve accuracy of the information
Multiple Pass Method & Probing
Food preparation
Portion sizes
Snacks and beverages
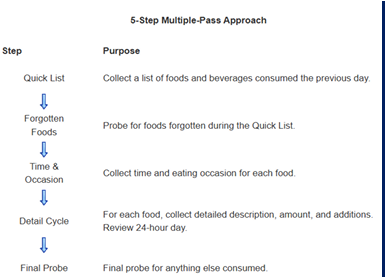
what is the multiple pass method
Research-based, multiple-pass technique employs 5 steps designed to enhance complete and accurate food recall and reduce respondent burden
5 STEP METHOD
Quick list
Forgotten foods
Time and occasion
Detail cycle
Final probe
food frequency questionnaire (FFQ)
what is
strengths and weaknesses
Commonly used for assessing intake of nutrients and specific foods in groups of people; Contain a predetermined food list with or without portion sizes; How frequently certain foods are consumed
Strengths: chronic intake of specific foods, screening tool, food preferences
Weaknesses: Recall bias, not suitable for usual energy intake and macros
diet history is a combination of what
24-hour recall + FFQ
diet history
usage
time
Preferred technique of choice by most dietitians in clinical practice
Fast (20 – 30 min)
diet history advantages (3)
Gives good insight on social, behavioral and cultural influences on food choices
gives you baseline of athlete nutrition and cooking literacy
Valuable for assessing nutrient timing before, during, and after exercise
diet history con
It is NOT accurate for quantitative assessment of total energy or macronutrient intake
what are 3-day records
Weighed or estimated records filled out by the athlete
Usually 3 – 7 days
strengths of 3-day records
Does not rely on memory, potential to provide detailed info, better reflection of
typical dietary intake
major limitations for diet records (5)
underestimation of energy and intake
underreporting (around 50%)
user error (portions, condiments, snacks, oils)
athlete with weight focuses underreport
reporting of socially desirable foods
how to make food records better (3)
give instructions!!!
review the food record entries with the athletes
2 weekdays and 1 weekend
what are 4 challenges od dietary assessment of athletes (4) - think of their training
Periodized training cycles
Training days versus competition days
Major dietary changes (make weight or carb load)
Nutrient timing
which is the best assessment tool in practice
food records (3-7 days) but expect 20-50% innacuracy
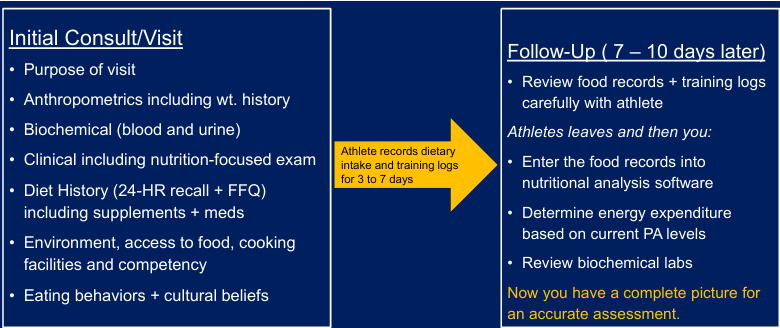
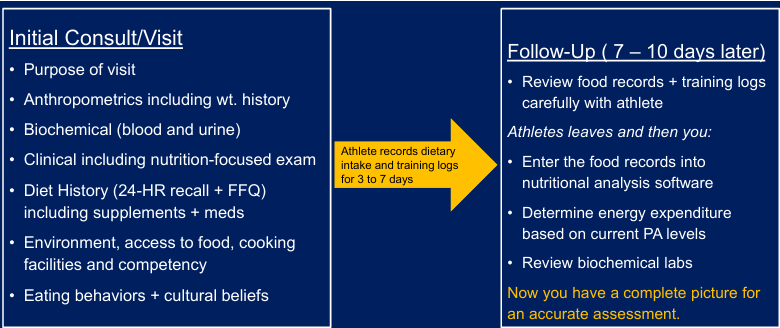
what would one usually do in practice (timeline)
baseline visit
follow-up
Baseline visit → Diet history (24-hour recall and FFQ) USOC Form
Give them a food record and ask them to keep track of diet for minimum of 3 days (7 is better). Keep a record of exercise training logs including intensity and duration during same timeline.
Follow-up visit → review food records and training logs with athlete
what must you do after your athlete has done their 3-day food record
Enter all of those foods and drinks into a nutrient analysis database
nutrient analysis potential error (6)
Actual food composition are just estimates of nutrient composition
Missing foods from the database
No serving size given
Serving sizes are difficult to standardize
Different countries of origin
Nutrition facts label
detailed nutrition assessment timeline
initial visit (what to determine, look for- 7)
time between
follow up (when, what to do- 3)
why do we use anthropometrics (what do we determine)
body comp
height
weight
BMI
BMI issues
not a suitable assessment for body comp in athletes
what are better ways to assess body comp in athletes
direct
cadaver
what are better ways to assess body comp in athletes
indirect (5)
Skinfold thickness
Bioelectrical impedance analysis
Underwater weighing
BODPOD
Dual energy X-ray absorptiometry (DXA)
skinfold thickness
accuracy
strength
limitations
Within 3 – 4 % of underwater weighing when individual is trained
Strengths: cheap, fast, fairly accurate
Limitations: training required for precision, unsuitable for quantifying absolute fat
bioelectrical impedance analysis (BIA)
what is it
strength
weakness
Measures the resistance to flow of electrical current passing through the body; based upon the idea that fat is more resistance than lean mass
Strengths: cheap, fast, portable
Limitations: greatly influenced by hydration status, moderate-to-high error versus DXA
underwater weighing
what is it
strength
weakness
Historical gold standard for assessing body composition via body density in humans
Body density (fat and fat-free mass)
Strengths: Very precise
Weaknesses: Time insensitive, impractical, less accessible
air displacement plethysmography
what is it
accuracy
strength
weakness
Measures body volume by measuring the amount of air displaced
Comparable to underwater weighing (within 2 – 3%)
Strengths: good accuracy, fast
Limitations: claustrophobia, expensive

dual energy x-ray absorptiometry (DEXA)
what is it
what does it measure
strength
weakness
Considered practical gold standard
Measures 3 compartments: lean mass, fat mass, bone mass
Strengths: Very precise, regional measurements, subject comfort
Limitations: small amount of radiation, expensive, tall and broad athletes
body comp assessments ranking based on accuracy and practically
DXA
BODPOD
Underwater weighing
Skinfold thickness
BIA
body comp assessments based on cost and portability ranking (5)
Skinfold thickness
BIA
BODPOD
DXA
Underwater weighing
how often should one asses body comp
every 2-3 months
why do we want 2-3 month between body comp assessment
Main reason is variability of measurements (1-2 % error for body fat or fat-free mass)
Body composition changes typically take time
Too frequent measures can create bad dietary practices (fasting, etc.)
why do we measure body comp in athletes (3)
Address concerns about the health of an athlete
To determine contributions to performance
To best prepare an individual for a sport-specific performance
too high body fat and health risk (4)
increased risk of cardiovascular disease, diabetes, hypertension, and some cancers
too low body fat and health risk (2)
loss of menstrual cycles and impaired bone development which can lead to osteopenia and osteoporosis later in life
essential body fat in men
2-5%
essential fat in woman
10-13%
why would we track changes in muscle mass (2)
Loss of lean tissue over time can impair performance
when track changes in fat and muscle mass
during the season
why should one monitor the effectiveness of diet and exercise training programs (2)
Athlete on a specific diet (weight gain or weight loss) led to favorable changes
Athlete on a specific diet and they gained muscle and increased strength
sports that have strong relationship between physique and performance (6)
Swimming (limb length, low fat)
Track and field (depends on the event)
Rowing (low body fat %, greater total muscle mass)
Track cycling (leg muscle volume)
Gymnastics (low body %)
Diving (low body %)
sports with weight classes and cutoffs that greatly impact performance (5)
Boxing
Wrestling
Mixed martial arts
Horse jockeys
Formula one racing
sports that vary in desired body size/comp differing on position (6)
Baseball
Softball
Basketball
Football
Tennis
Golf
nutrition assessment timeline
when you have all information from assessment, what must one do
Provide a written plan to both athlete and coach detailing results, interpretation, follow-up, plan, and next steps
nutrition diagnosis for athletes
No standardized list of diagnoses for athletes
Use scientific literature to document diagnosis
Describe the cause and factors contributing to the nutritional problem in the athlete
Provide clinical signs and symptoms of the problem
Develop a diagnostic statement of the situation
nutrition intervention for athletes (overall)
Prioritize and provide nutrition diagnoses to athlete
Develop educational materials for athlete that are evidence-based
The plan → provide suggested meal plan, food monitoring system or log, educate athlete how to self-monitor and make appropriate food choices
nutrition monitoring and evaluation for athletes (what to focus on)
Compare before and after values to assess changes (good and bad)
Provide the athlete with written verbal feedback
Document progress towards goals
Do we need to reassess strategy if it’s not working?
Determine whether to continue or discontinue