5. Corneal Epi
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
101 Terms
What does the extracellular matrix regulate?
Proliferation
Migration
Differentiation
Angiogenesis
Immune functions
Autophagy
Tissue separation and shaping
What are the categories of ECM?
Periceullar matrix
Basement membrane of epithelia
Glycocalyx
Interstitial matrix
Cartilage/bone
Storms of cornea
Whar is ECM?
Dynamic 3D network of macromolecules that provide structural support for cells and tissues
What are the major components of the extracellular matrix?
Proteoglycans
Collagnes
Matrix Metalloproteinases (MMPs)
Elastic Fibers
Lysyl oxidase
Laminin
Tenascin
Fibronectin
What are proteoglycans composed of?
A protein core + glycosaminoglycans
Why are proteoglycans attracted to water?
Their negative charge binds to water
How thick is the basement membrane?
20-50 nm
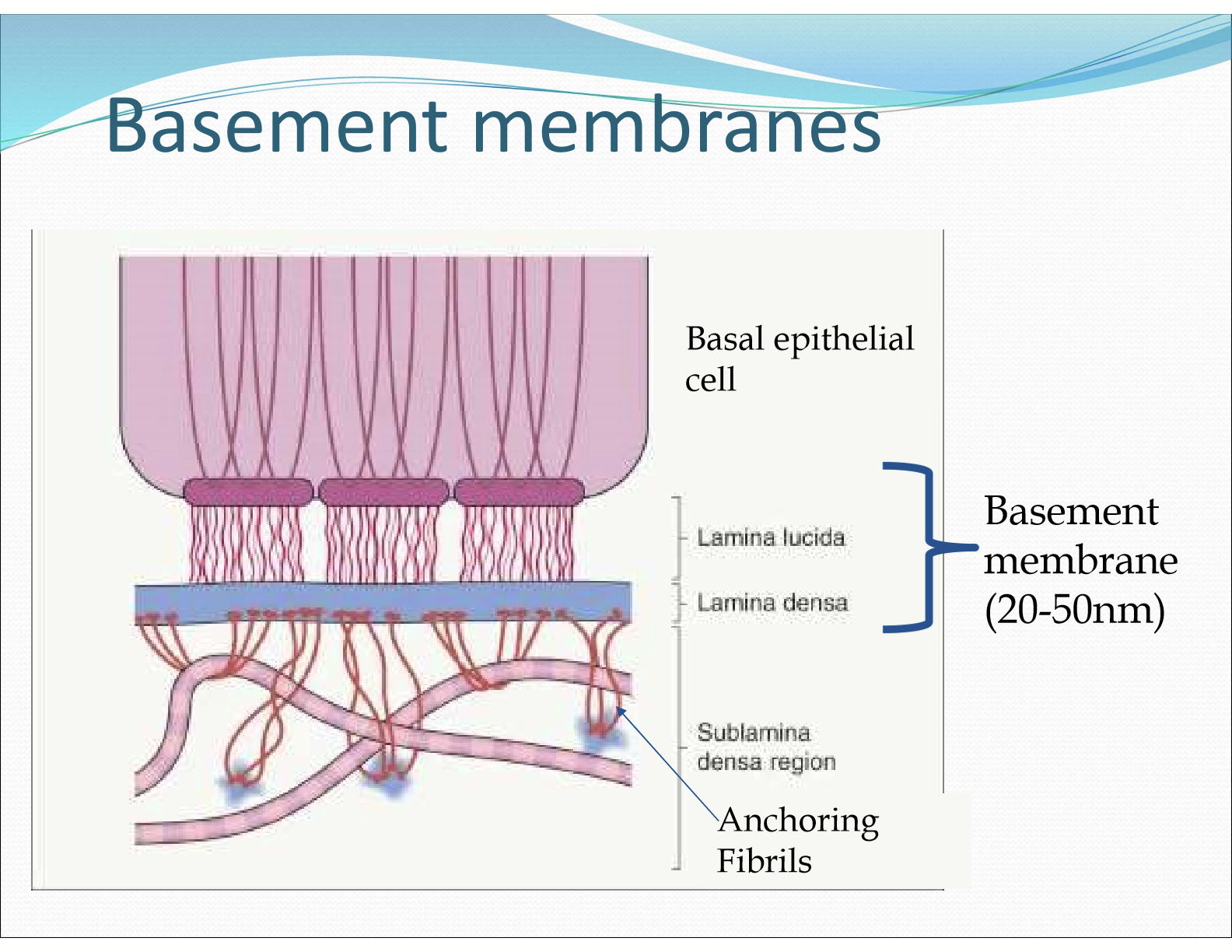
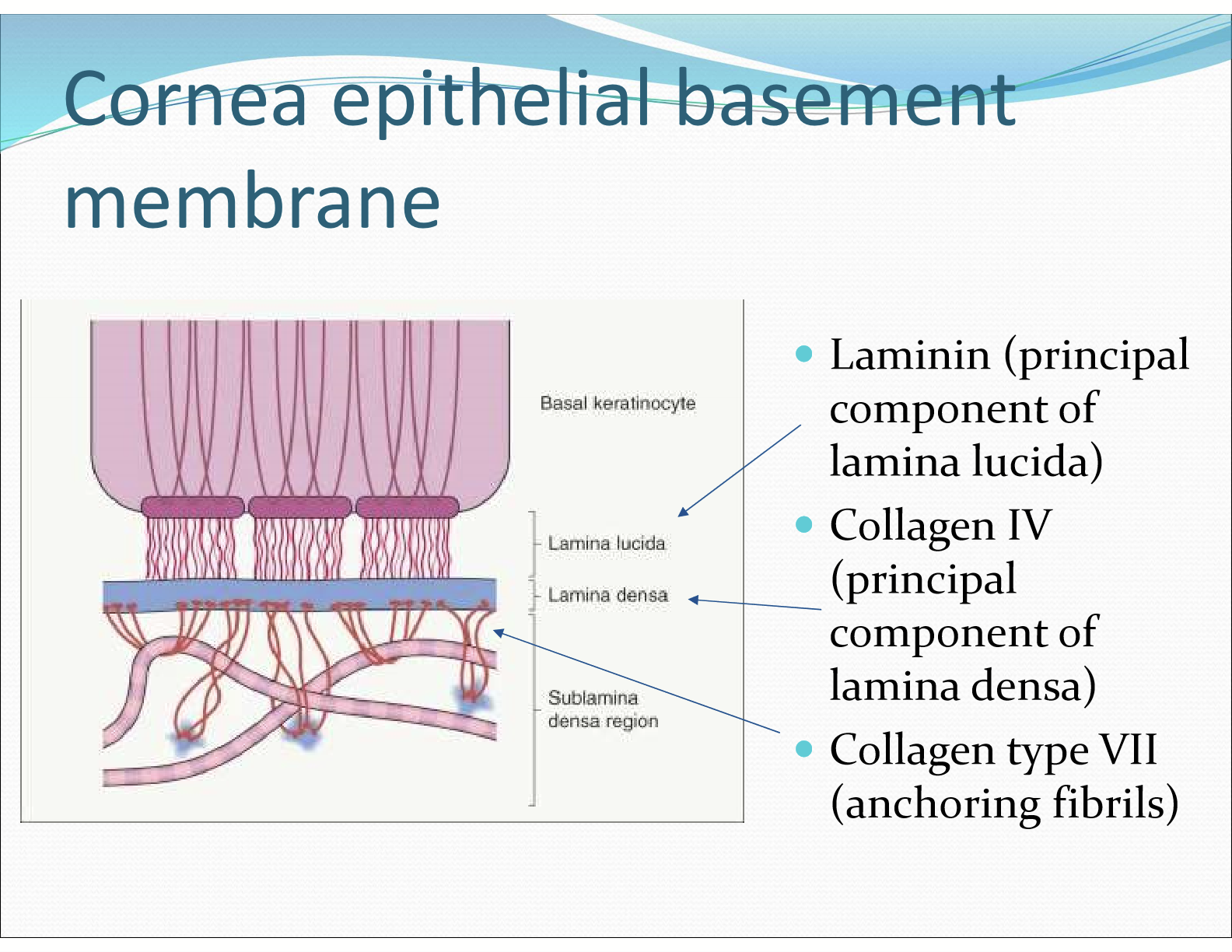
What is the cornea epithelial basement membrane composed of?
Laminin (princippal component of lamina lucida)
Collagen IV (principal component of lamina densa)
Collagen type VII (anchoring fibrils)
Where are hemidesmosomes found?
In the basal membrane of corneal epithelial cells
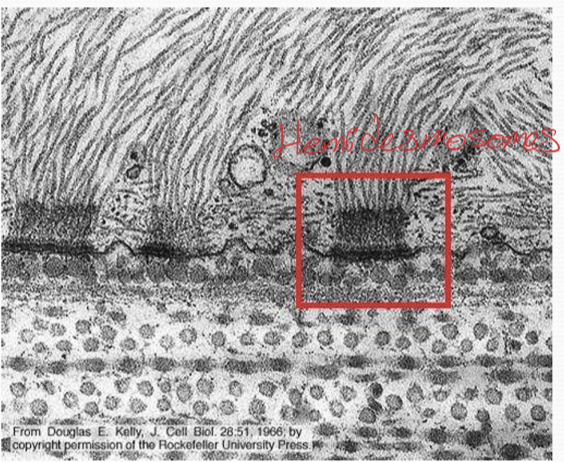
What role does hemidesmosomes play?
Adheres basement membrane to cells
What is the composition of hemidesmosomes?
intermediate filaments
plectin
integrins
What role does intermediate filaments do?
They are the structural cytoskeletal component and strengthens hemidesmosomes.
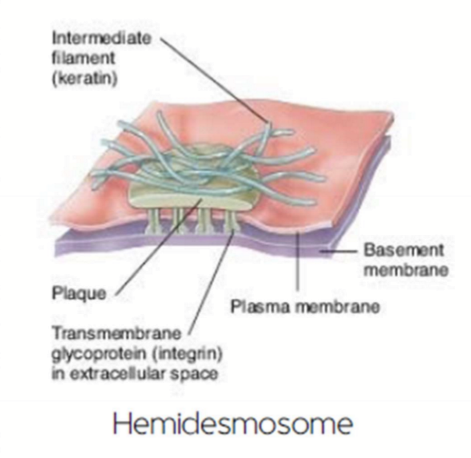
What roles do plectin play in hemidesmosomes?
They form intracellular plaque, bind to intermediate filament cytoskeleton, and bind to integrins
What do integrins do in a hemidesmosome?
They are transmembrane proteins that bind to laminin and plectin
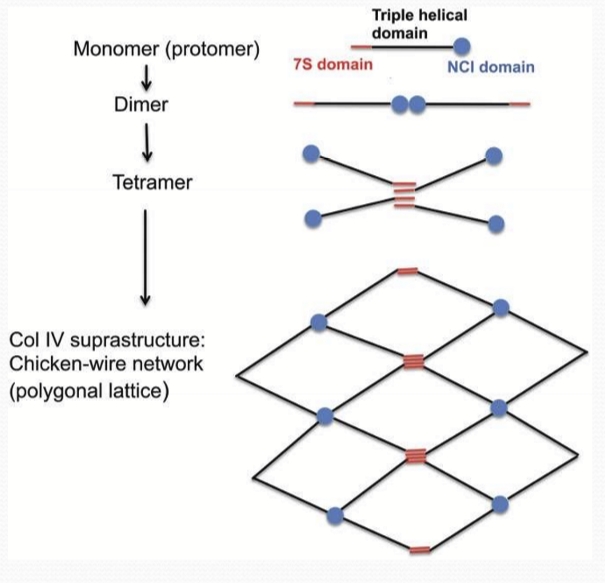
What is the structure of collagen IV?
It is composed of 4 proteins to make a molecular subunit. It is shaped like “chicken wire” and interconnects many proteins to provide strength
What happens during a cornea erosion?
Patient experiences pain due to exposed nerve endings
What causes cornea erosion?
Corneal injury disrupting the molecular connection between hemidesmosomes and the basement membrane
What genetic predispositions that lead to a weakened cornea?
Alport’s syndrome: mutation in Collagen IV, causing epithelial cell death and cataracts
Epidermolysis bullosa: disruptions in other hemidesmosomal/basement membrane genes
Why is the cornea more prone to injury during healing?
The hemidesmosome are the last structures to appear during the healing process, so the cornea is still weak and therefor susceptible to injury
What is epithelial basement membrane dystrophy (EBMD)?
It is an intrusion of the abnormally thickened basement membrane into more superficial layers of the cornea that forms geographic map-like lines in subepithelial microcysts.
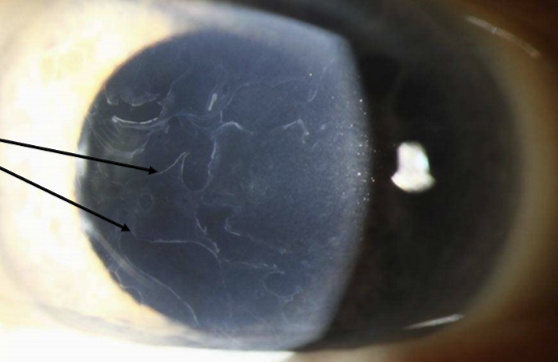
What are the other names of epithelial basement membrane dystrophy?
Also known as Cogan’s microcystic epithelial dystrophy or map-dot-fingerprint dystrophy.
Where are the subepithelial microcysts?
They are below the basement membrane surrounded by epithelial cells.

Why does EBMD weaken the cornea?
The cells below the basement membrane are not tightly bound and therefor are more likely to be damaged/ripped off. It is also biomechanically weaker.

What is the prevalence of EBMD?
~2% of the population has it, and has a genetic component.
What are some characteristics of EBMD?
Often asymptomatic
Often an underlying factor for corneal erosions (~30%)
Stem cells have 2 important characteristics, what are they?
Unspecialized/undifferentiated cells capable of renewing themselves through cell division
They have the potential to change into/differentiate into a specific cell type
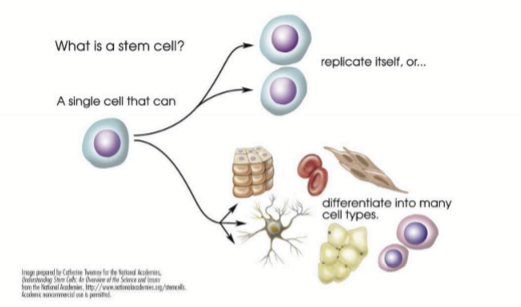
What are pluripotent cells?
Cells that can give rise to all tissue cell types
What are multipotent cells?
Cells that can give rise to multiple cell types
What are unipotent cells?
Cells that give rise to a single cell type
What are the two kinds of stem cells?
Embryonic stem cells (pluripotent/totipotent)
Somatic adult stem cells (multipotent)
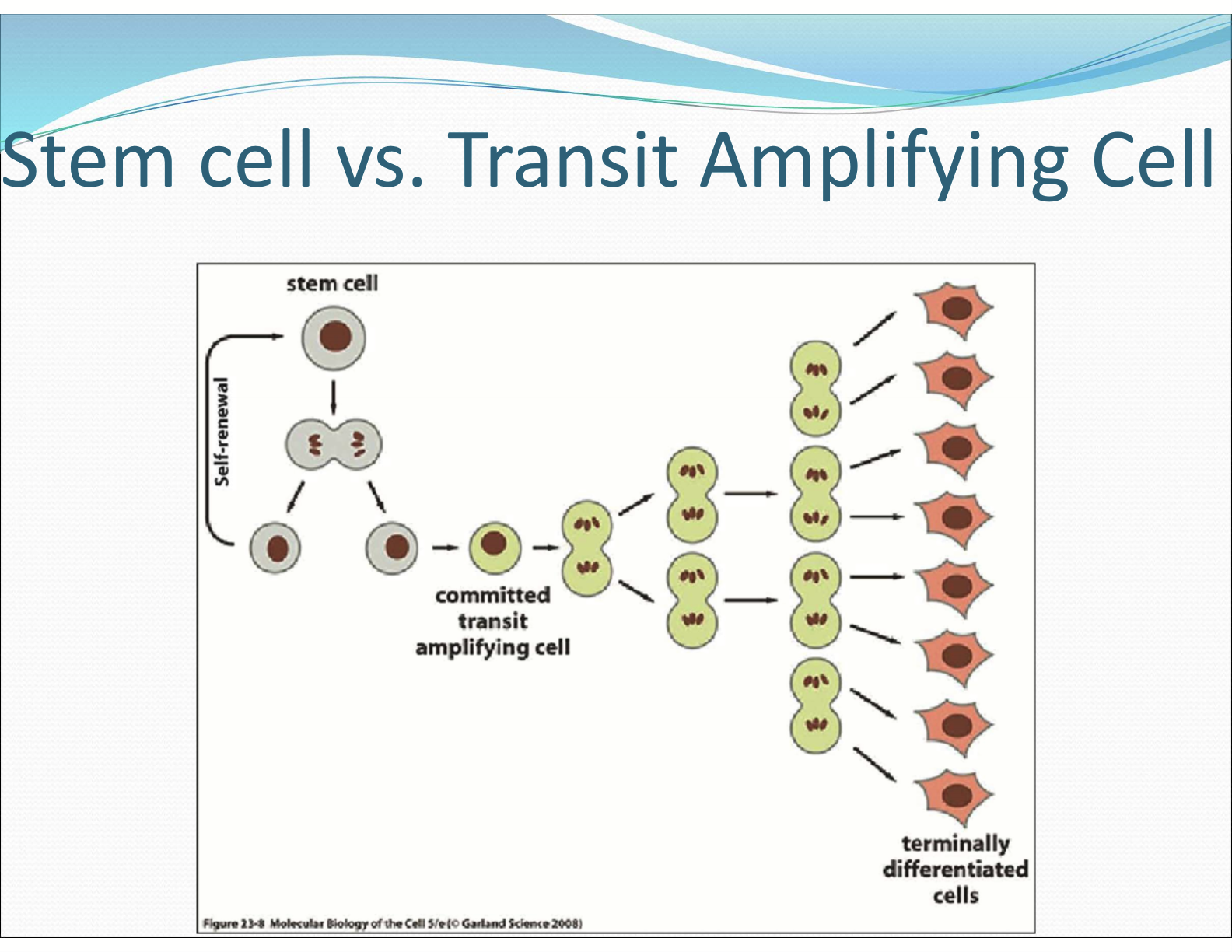
What is the difference between stem cell and transit amplifying cell (TAC)?
Stem cells are self-renewing and do not undergo differentiation. Transit amplifying cells are cells that are committed and are only able to amplify and terminally differentiate.
What are the corneal cells constantly doing?
Exfoliation and desquamation. Induced by blinking, minor abrasions, and eye rubbing
How far do the cells move?
The move centripetally 10-15 micrometers/day from growth pressure
How often is the entire corneal epithelium renewed?
9-12 months
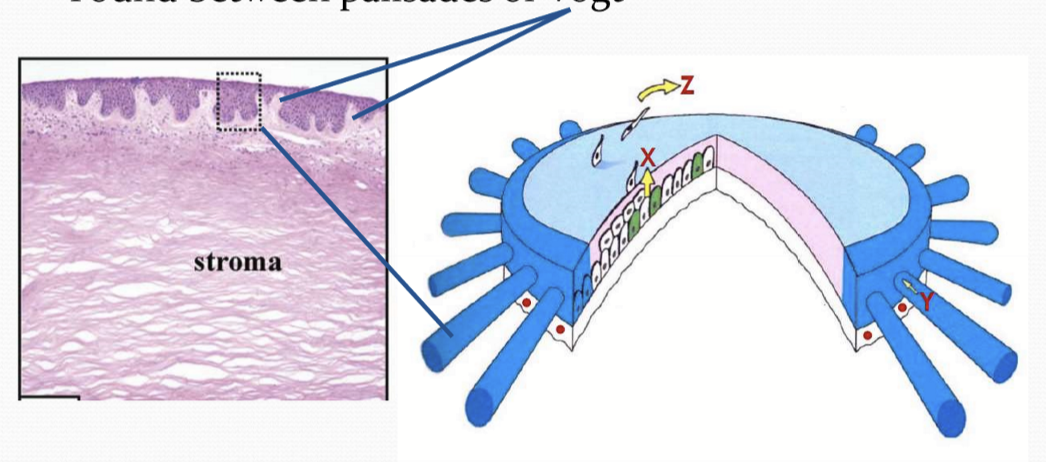
What is X+Y=Z
X= cell contribution due to basal cell proliferation
Y= cell contribution due to centripetal movement of cells
Z= Normal loss of cells from the corneal surface
What is LESC?
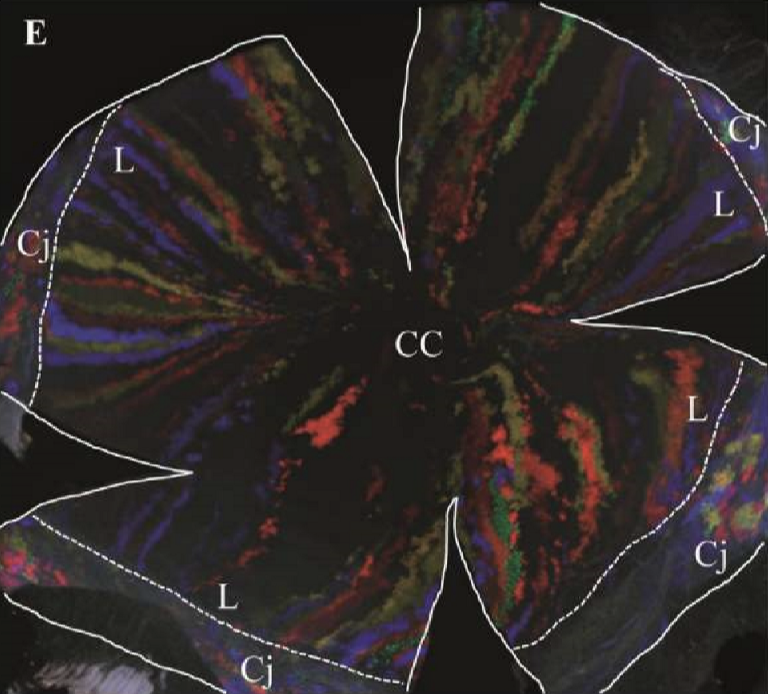
Limbal epithelial stem cell, where stem cells are found exclusively in the limbus. TAC’s move centripetally and refresh the corneal epithelium during homeostasis and injury.
What is CESC?
Corneal epithelial stem cell, where stem cells are found in the limbus and basal cornea epithelium. TAC’s move centrifugally, LESCs contribute only during injury, CESCs contribute during homeostasis and injury.
Where are the sources of epithelial cells located?
In the limbal region of the cornea, between the palisades of Vogt.
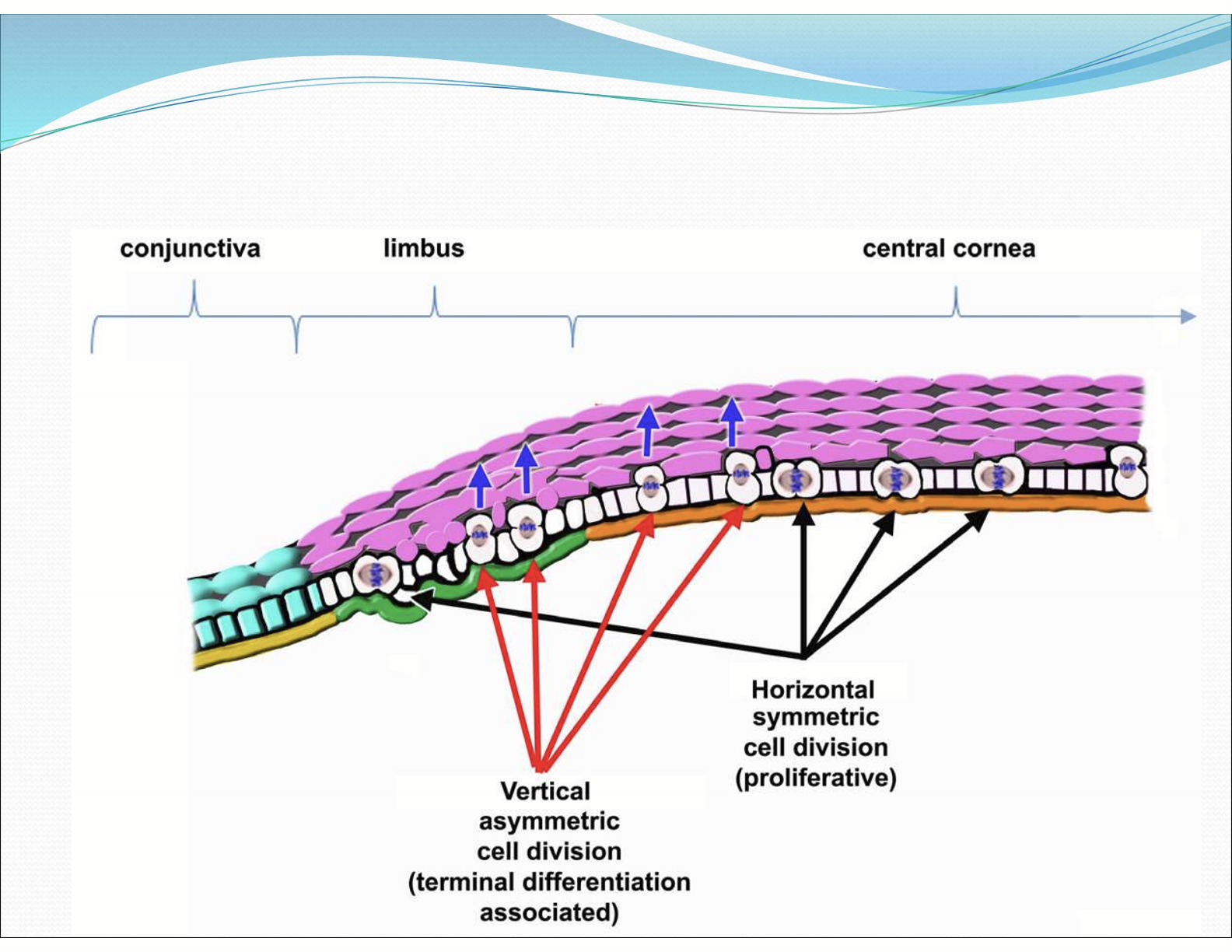
Where are vertical cell division typically located?
Towards the limbus
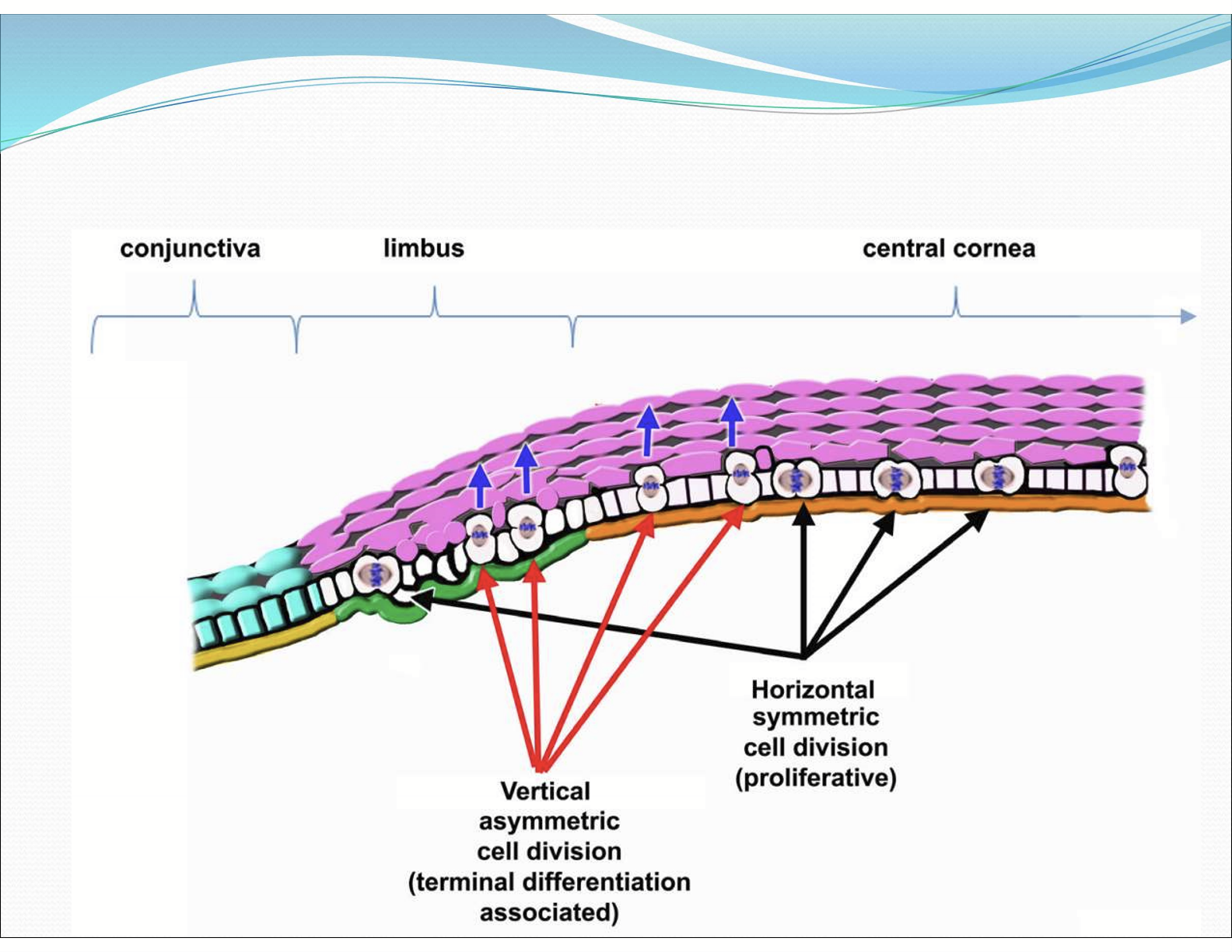
Where are horizontal cell division typically located?
Towards the central cornea
Where are limbal stem cells located?
In limbus, at the basal layer.
What are the characteristics of Limbal stem cells?
Low mitotic activity
Multipotent
Non-differentiated when in limbal epithelium
cornea-specific keratins absent
Long life span
Unlimited potential for cell division
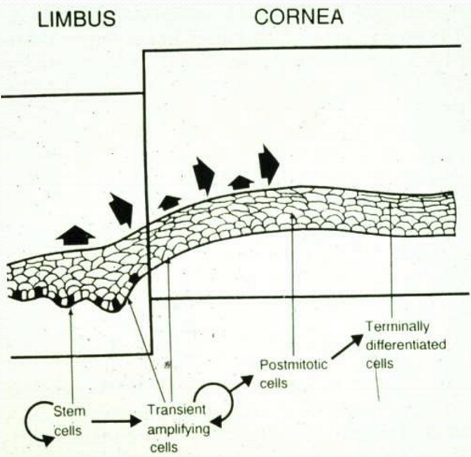
What happens during cell division of limbal stem cells?
2 cells are produced, with1 cell retaining multipotency and the other cells becomes a TAC in the basal layer
What happens to the mitosis rate of the TAC?
It rapidly increases upon asymmetric division
How do the TAC migrate?
Centripetally towards the central cornea and anteriorly becoming wing and superficial cells.
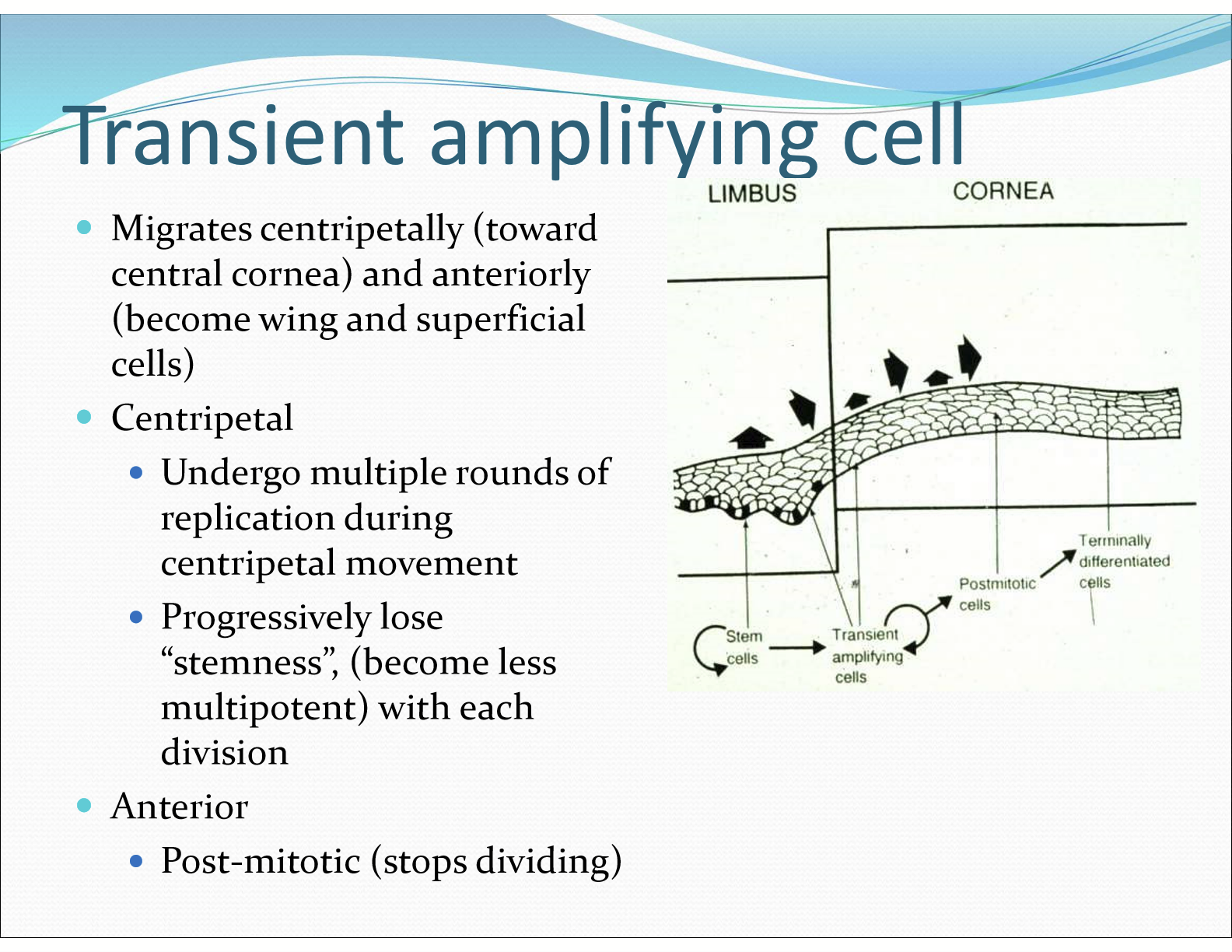
What happens to the TAC when it moves anteriorly?
It stops dividing
What is a stem cell niche?
A region that protects a stem cell population and helps maintain their multipotency. This is seen as epithelial thickenings in the limbus.
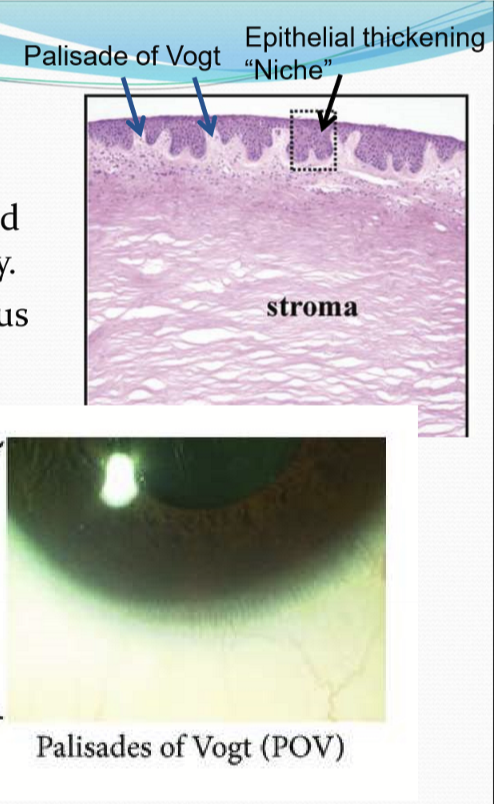
What are factors that aid multipotency in the stem cell niche?
Thickness of epithelium
Rich in melanin pigments
Different array of BM proteins than central cornea with different ECM promoting stemness or differentiation and proliferation
Presence of nearby BV to provide O2, growth factors, and antioxidants
Where are the stromal stem cells located?
They are subjacent to limbal basal cells
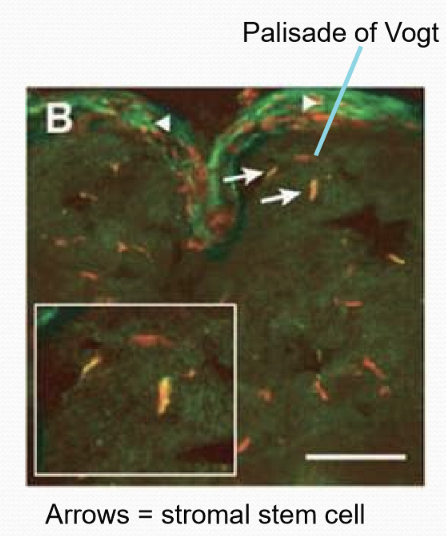
What supports and nurtures stroma stem cells?
Limbal stem cell niche
What do stromal stem cells differentiate into?
Keratocytes
Where are Conj stem cells?
Location is unknown, but believed to be concentrated in fornical conj or spread throughout conjunctiva
What potential do conj stem cells have?
Multipotent, able to differentiate into both epithelial and goblet cells, but do not differentiate into cells that express corneal specific proteins
What are some symptoms of limbal stem cell dificiency?
Patients will complain of blurry vision, foreign body sensation, photophobia, tearing, and pain. Patients will have an obvious loss of limbal palisades of Vogt observed with slit-lamp and cornea epithelium thinning.
What causes limbal stem cell deficiency?
Autoimmune disorders
Chemical/thermal injury
CL wear
Surgical damage
Infections
Often seen in congenital malformations
What are Ocular Surface Squamous Neoplasia (OSSN)?
It is a spectrum of precancerous and cancerous epithelial lesions affecting the conjunctiva and cornea. It ranges from mild dysplasia (conjunctival intraepithelial neoplasia, CIN) to invasive squamous cell carcinoma (SCC). OSSN is the most common non-pigmented malignancy of the ocular surface.
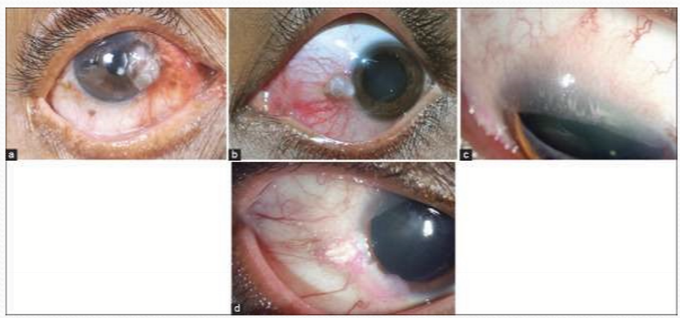
What areas does OSSN affect?
The cornea and/or conjunctiva, with the conj of limbus region particularly susceptible.
How does OSSN appear?
Zigzag vessel patterns with surface keratinization
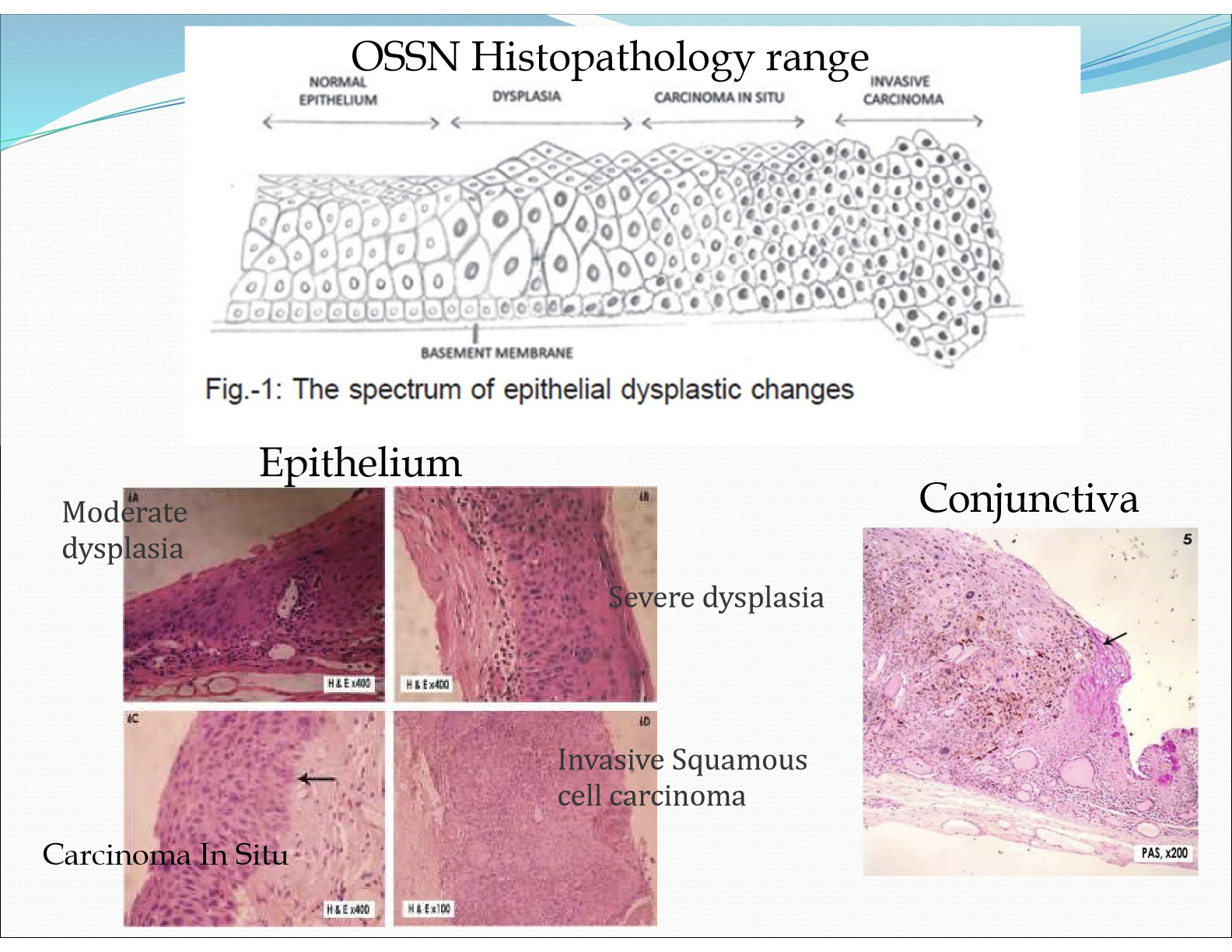
What are the risk factors for OSSN?
UV exposure
HIV
HPV
What is Pterygium?
The encroachment of subepithelial conj fibroblastic tissue onto the cornea involving the degradation of bowman’s layer
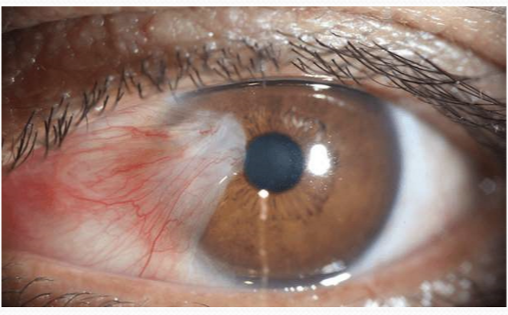
What is the etiology for pterygium?
Mutation of limbal stem/epithelial cells causing them to inappropriately proliferate into conj cells
Destruction of limbal stem/epithelial cells which normally act as a physical barrier to conj proliferation and encroachment into the cornea
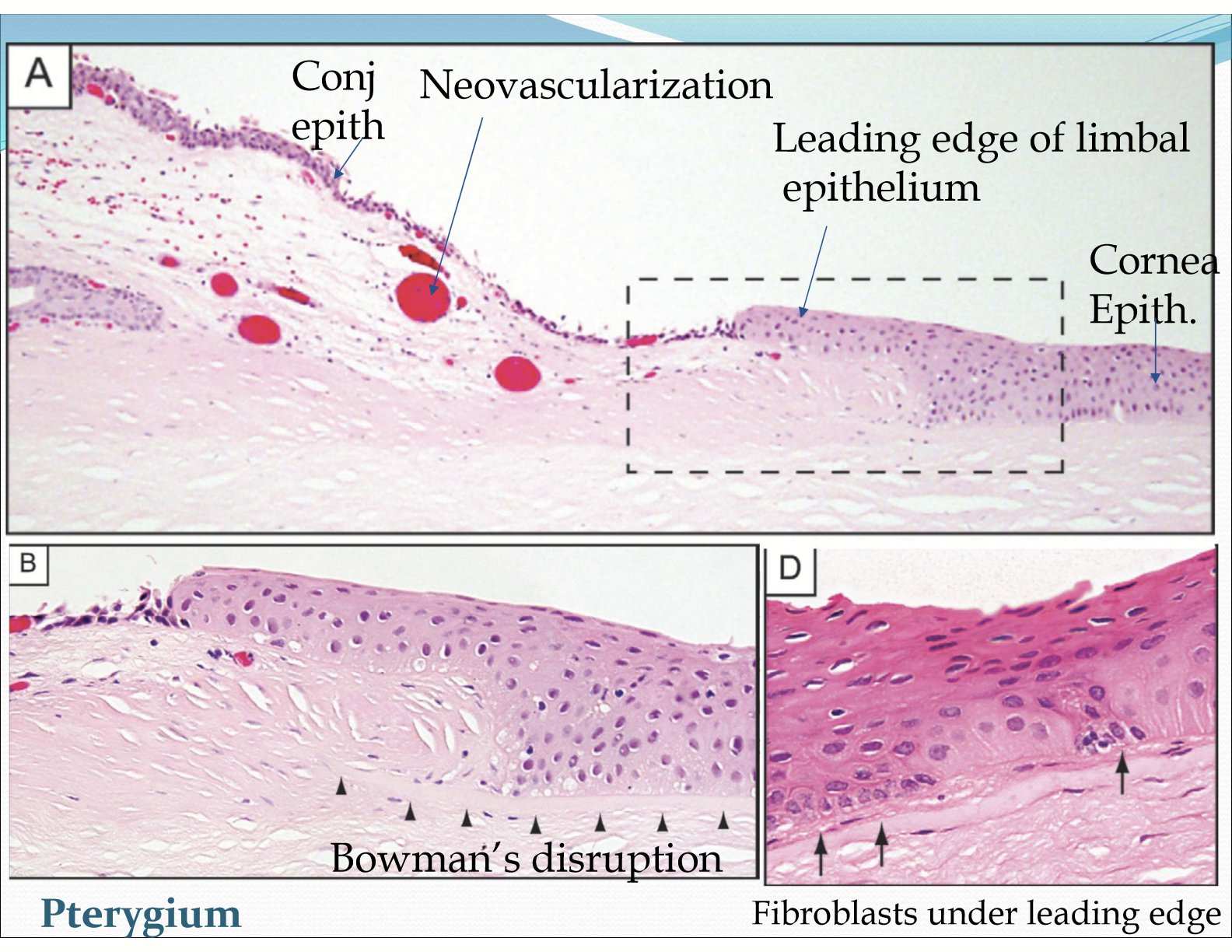
What are some characteristics of pterygium?
Neovascularization with straight vessel patterns
ECM remodeling
Inflammation
Leading edge of altered limbal epithelial cells
Goblet cell hyperplasia
What is Pinguecula?
A common, benign, yellowish or whitish growth on the bulbar conjunctiva and limbus
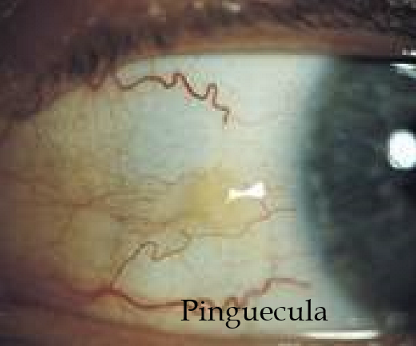
What causes pinguecula?
UV damage of fibroblasts beneath the epithelium, causing inappropriate production of ECM proteins (elastin) and can lead to an increase in fibroblast cell number
How does pinguecula appear?
As a creamy-coloured, chalky growth on conj surface
What happens in the later stages of pinguecula?
p53 mutation can occur and the pinguecula can become a pterygium
How fast can a corneal injury heal?
If it is a small superficial abrasion (<4mm), it can heal within 24-48 hours. If it is a deeper stromal injury, it can take up to 2 years to fully heal.
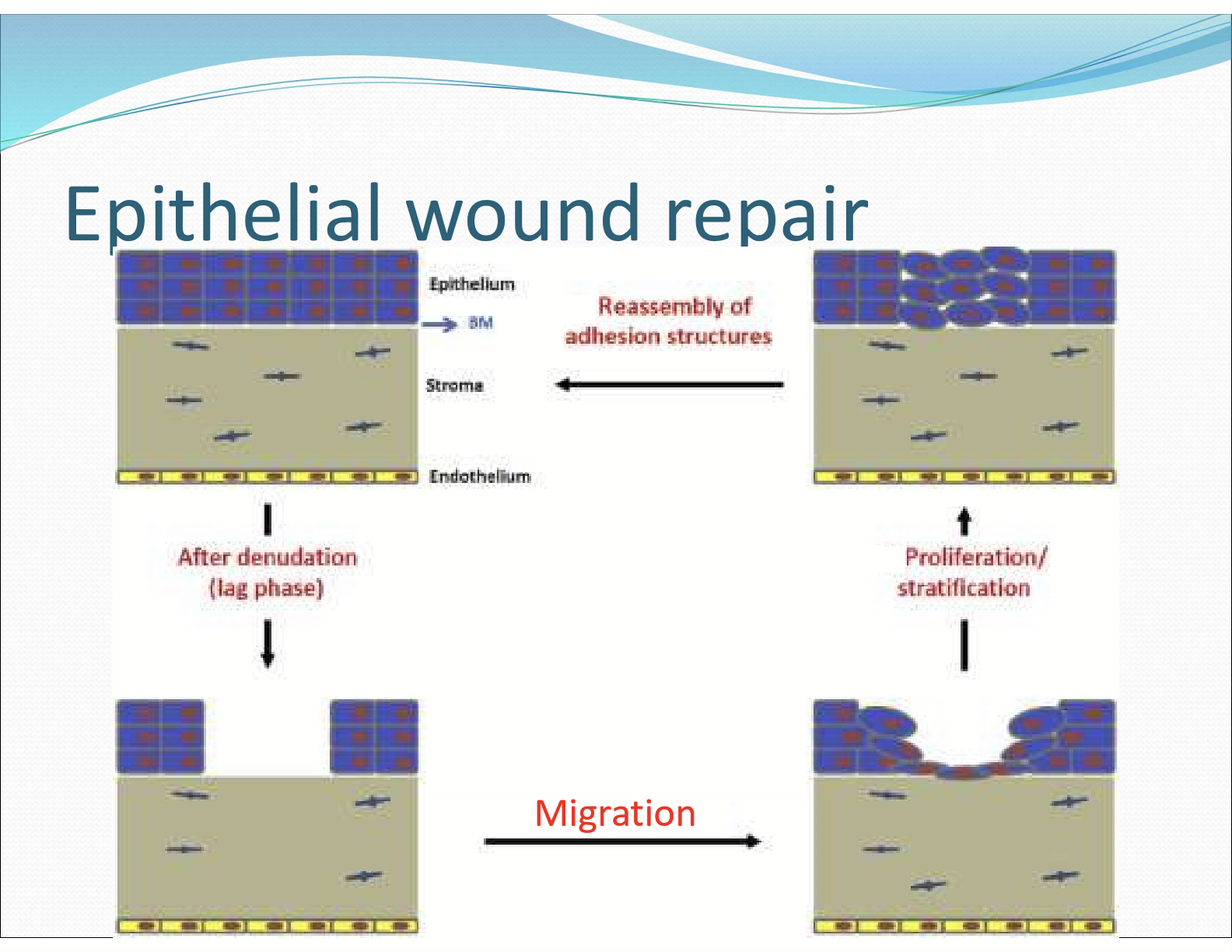
What are the stages of epithelial wound repair?
Stage 1: latent phase (4-6 hours after wound)
Stage 2: cell migration
Stage 3: epithelial mitosis
Stage 4: reassembly of adhesive contacts
What chemicals/substances are released by the epithelium during stage 1 repair?
Chemotaxis/Signaling:
Cellular Stress with Calcium and H2O2 released
Nerve damage causing cytokines and Substance P (neuropeptide) to be released
What happens to the basement membrane during stage I latent phase?
Hemidesmosomal attachments between basement membrane and basal cells disappear outward from wound facilitated by PMN/neutrophils
Damaged cells are removed via tear flush, leukocyte phagocytic activity, and apoptosis of damaged cells
Mitosis is inhibited
What is the role of PMN and neutrophils in stage 1 repair?
They enter the tears from lymphoid follicles and corneal stroma from limbal BV’s to faciliate the events of latent phase.
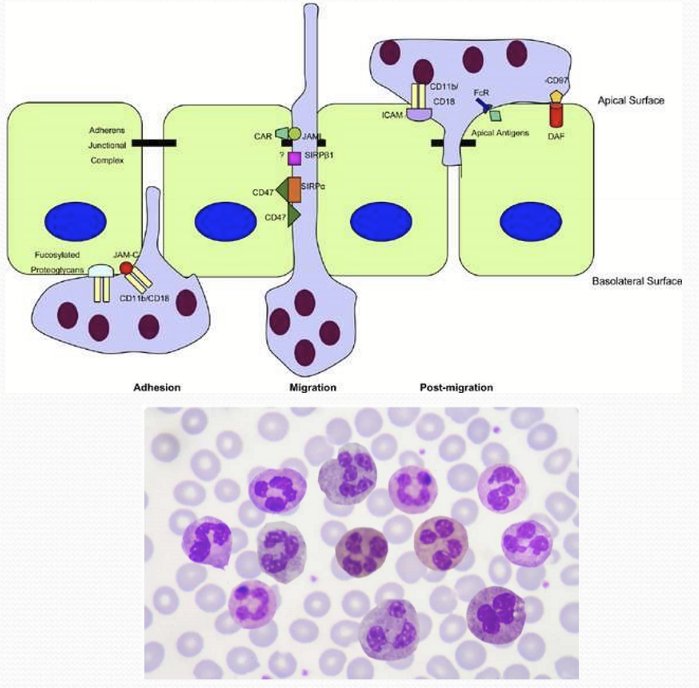
What happens during stage II: cell migration?
The leading edge of migrating cells is 1 cell thick with 3-6 sheets of eptihelium migrate together. The sheets move at 60-80 micrometers/hour and move centripetally.
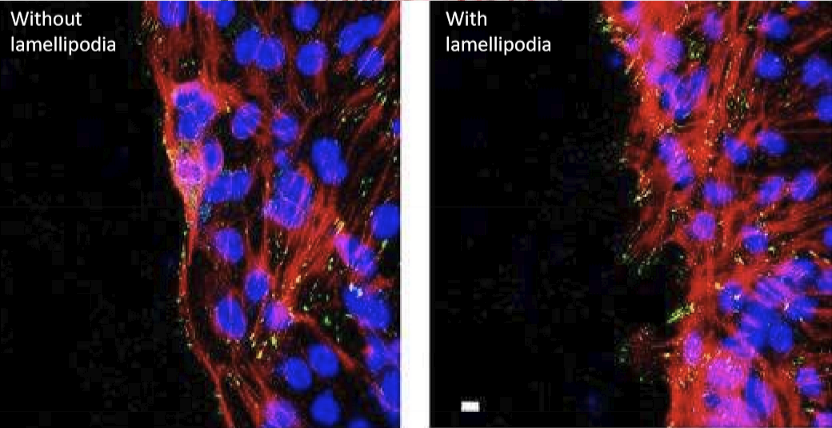
What are the cells doing during the cell migration stage?
The cells produce lamellipodia (broad) and filopodia (narrow) that extend from margin of epithelial wound. It composed of actin and myosin.
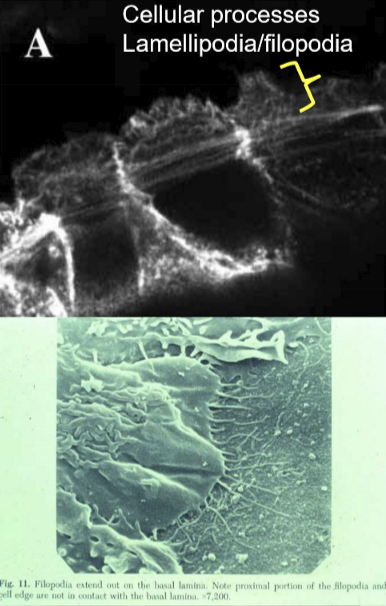
What is the purpose of the lamellipodia and filopodia?
It assists the cell migrating across the wound area to cover the region of cell loss
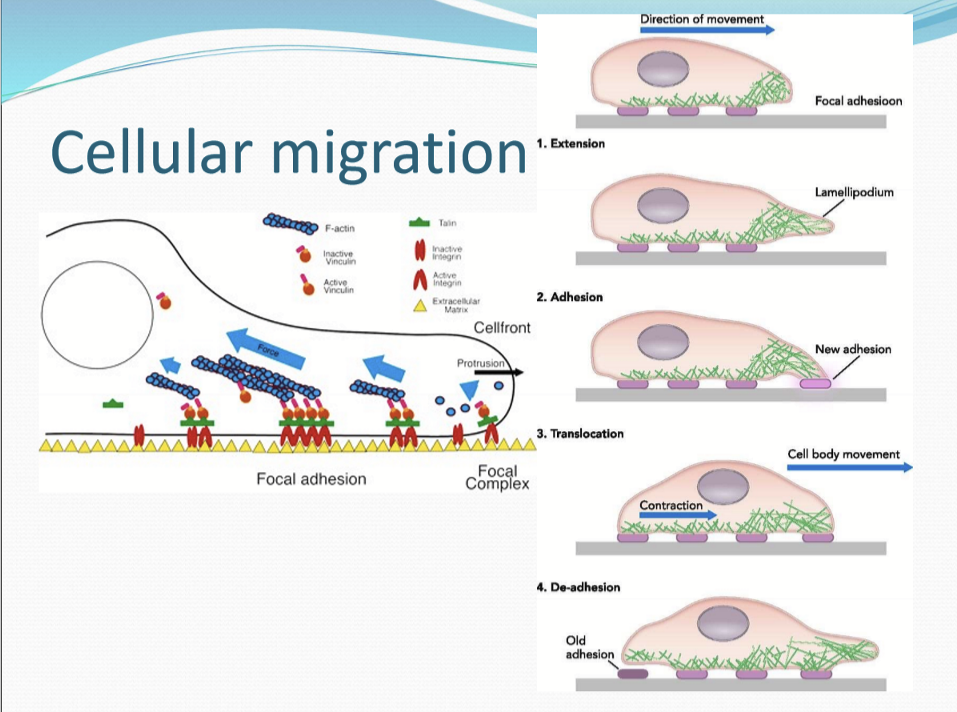
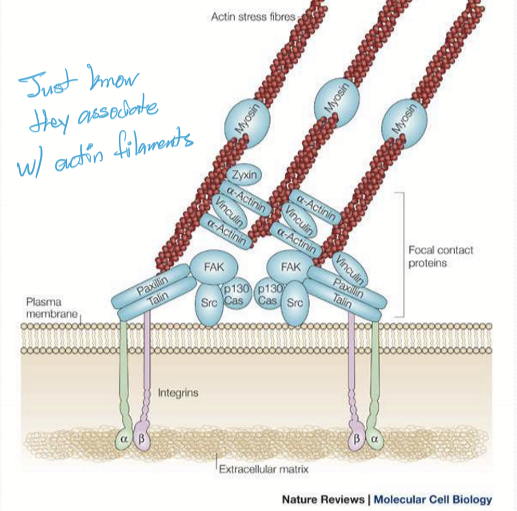
What do cells use attach to the basement membrane during the cell migration?
Focal adhesion attached to actin filaments
What are the focal adhesions composed of?
Protein complex using transmembrane integrins and actomyosin to connect the intracellular cytoskeleton with the extracellular matrix
What happens during Stage III: Epithelial cell proliferation?
Mitosis and differentiation of transit amplifying cells (TACs) resumes and continues until full thickness is restored
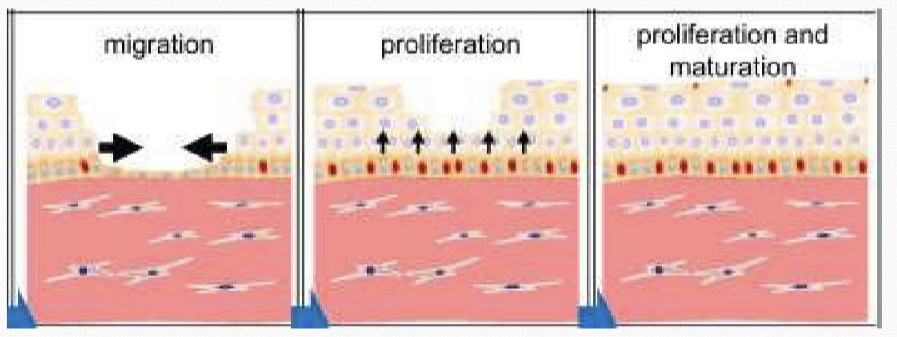
What happens during Stage IV: Reassembly of adhesive structures?
The tight junctions on the superficial side is re-established to act as a barrier and the synthesis of hemidesmosomes and anchoring filaments to anchor cell
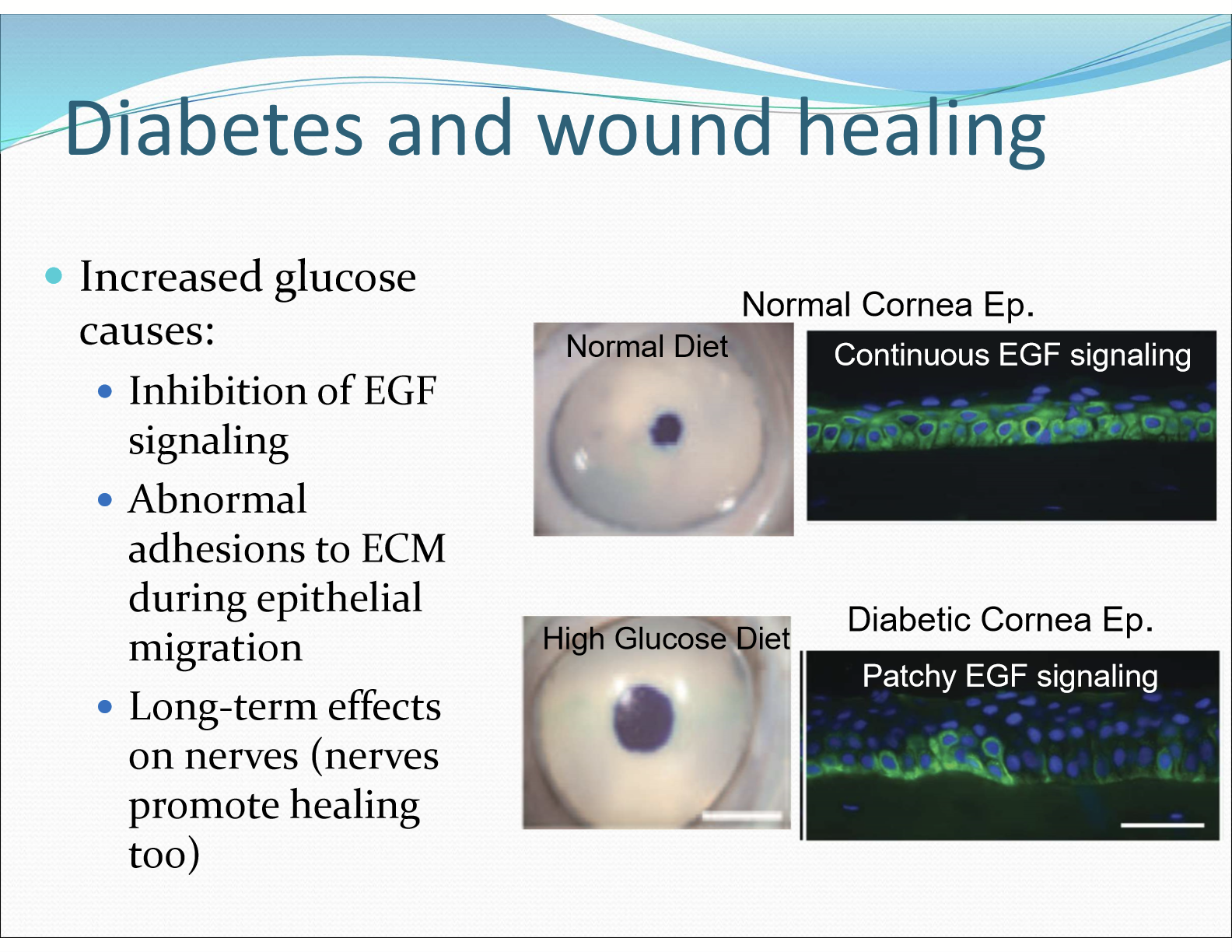
How does diabetic keratopathy affect wound healing?
It decreases wound healing, can cause corneal edema, and alter the epithelial basement membrane
Why does an increase in glucose cause poor corneal wound healing?
Increase glucose causes inhibition of EFG signaling, causing abnormal adhesions to ECM during epithelial migration. Excess glucose also leads to excess sorbitol preventing healing of corneal epithelium.
How does excess glucose cause edema?
NKA is inhibited, decrease in pump function, morphological abnormalities of endothelial cells, and sorbitol’s high negative charge may also contribute to influx water
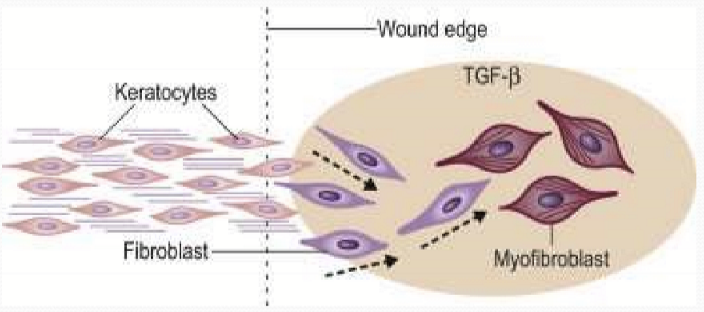
When keratocytes in the stroma are damaged, what happens?
They undergo apoptosis, facilitated by PMNs, and cleared by macrophages
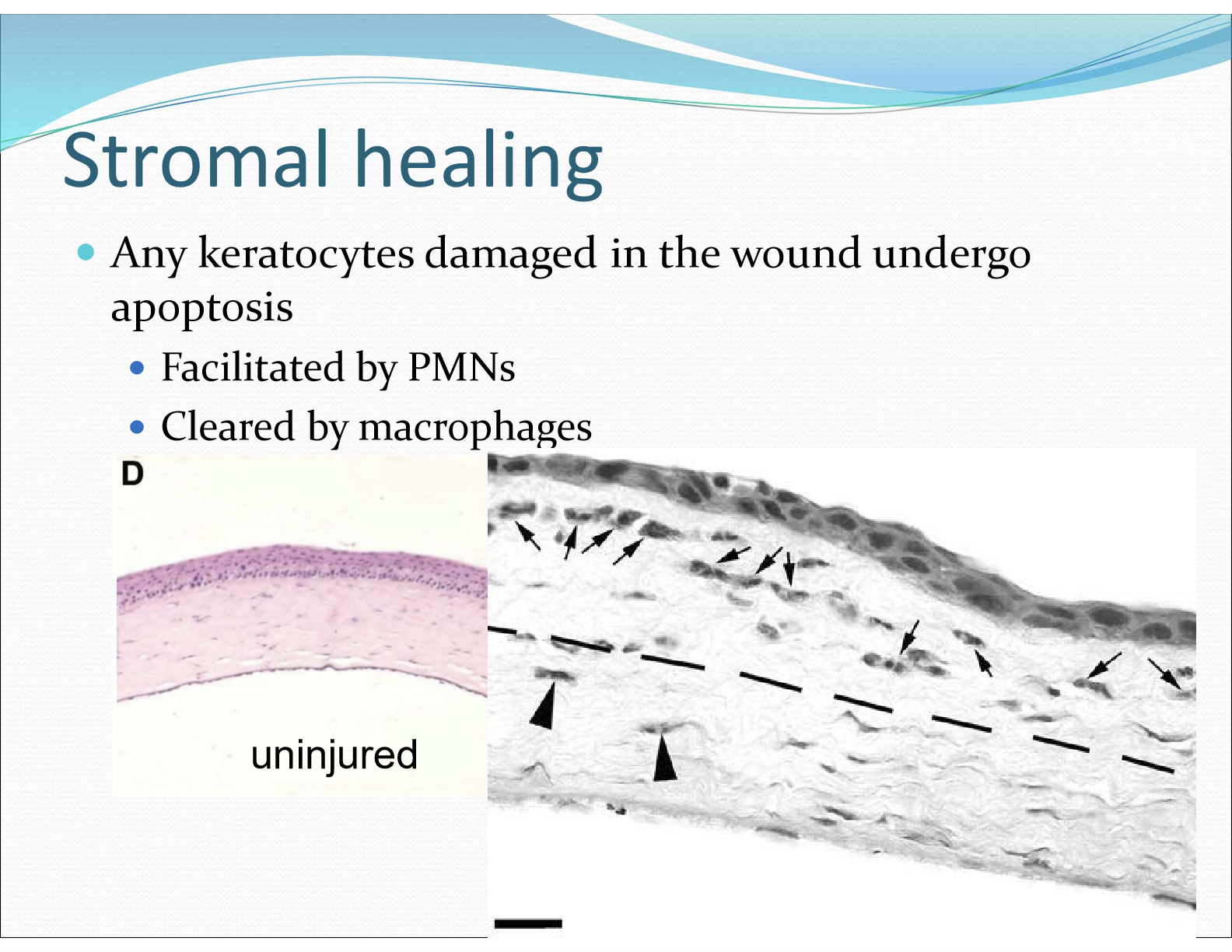
What do keratocytes nearby the stromal wound differentiate into?
hypercellular myofibroblasts
What do hypercellular myofibroblasts do in stromal healing?
The proliferate and form a region of hypercellularity between recently migrated epithelium and remaining stroma, produce sparse ECM with some GAGs, produce alpha-smooth muscle actin, and is not transparent
How does the corneal stroma become transparent again?
The opaque collagen ECM and myofibroblast is replaced with normal collagen ECM and wound fibroblast
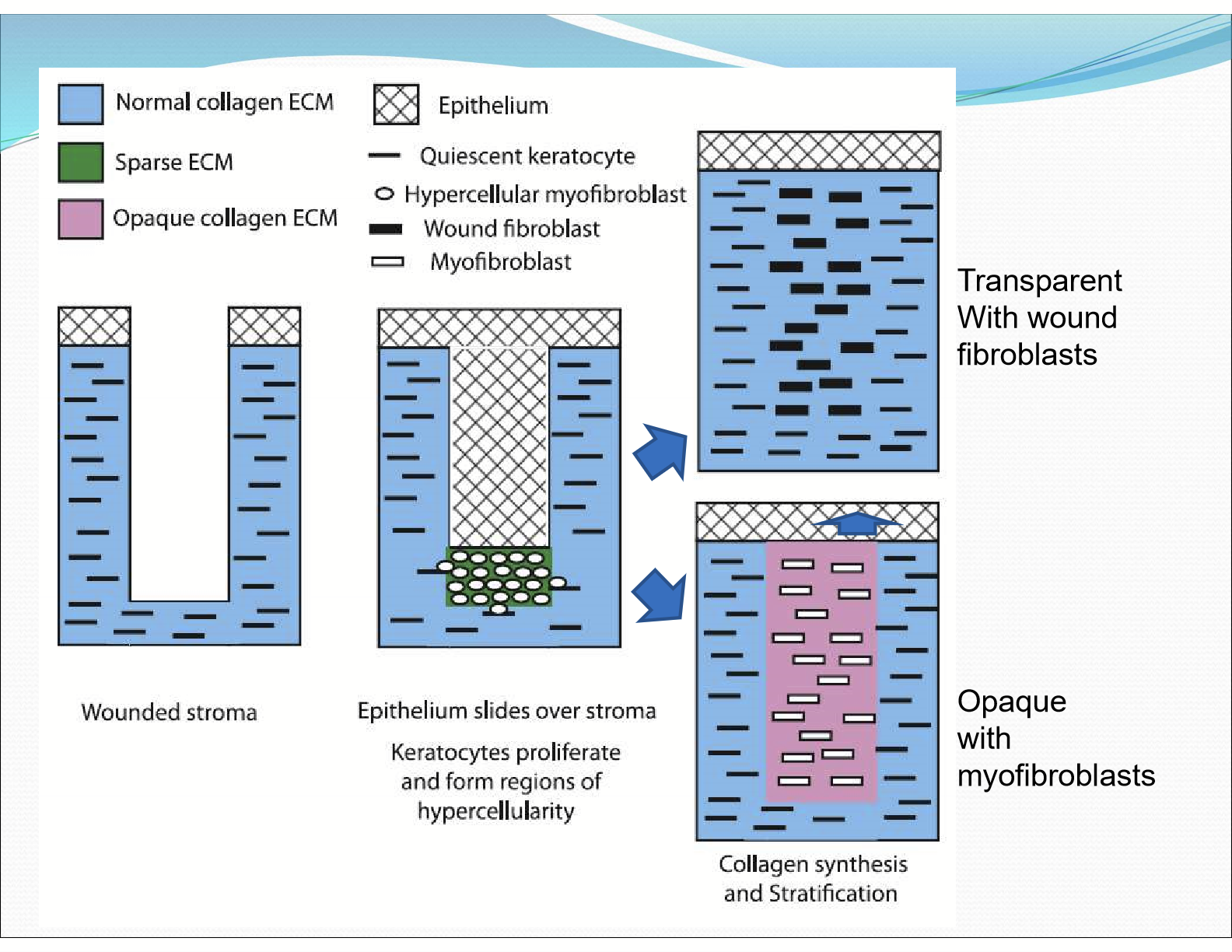
What do the hypercellular myofibroblast differentiate into?
myofibroblasts: produce alpha-smooth muscle actin and high levels of collagen & hyaluronan but low levels of mature stromal GAGs (opaque)
wound fibroblasts: produce high levels of collagen and mature stromal GAGs to form highly organized fibril structure to facilitate transparency
What do myofibrolasts able to do?
They are able to convert to wound fibroblasts to restore transparency over time
What happens to bowman’s layer when damaged?
It does not heal and its absence is permanent
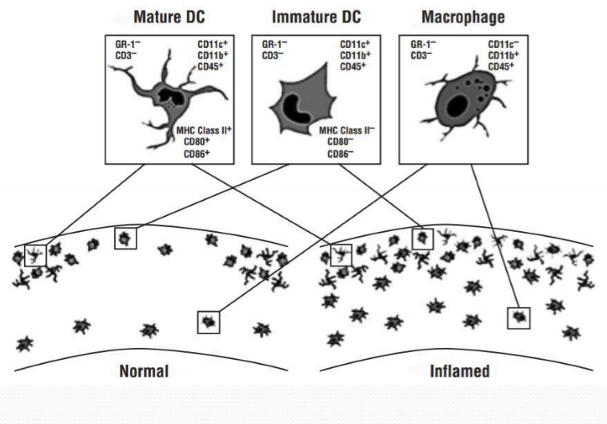
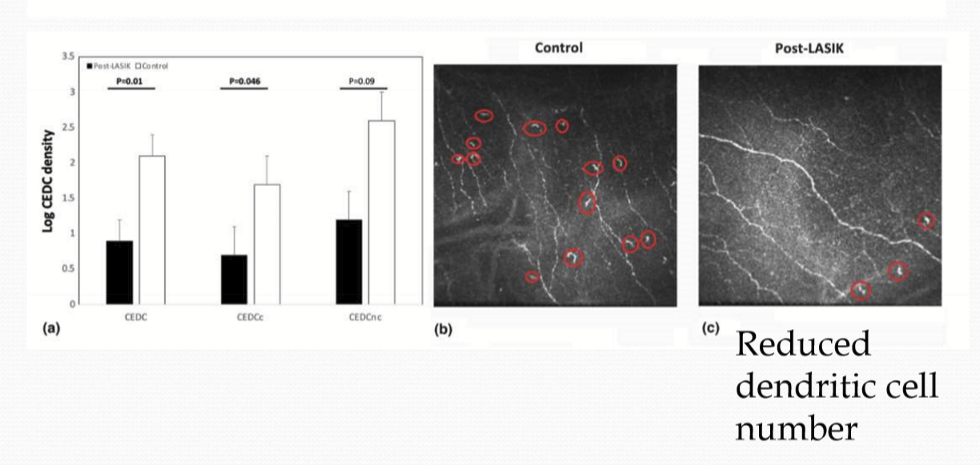
What role do corneal dendritic cells do?
They are antigen presenting cells that phagocytose pathogens and display foreign antigens to T-cells
Where are the corneal dendritic cells made?
They come from myeloid (mone-marrow) and lymphoid lineages
Where are the corneal dendritic cells found in the cornea?
They are found in the basal epithelium and stroma. The are more numerous peripherally than centrally and are migratory.
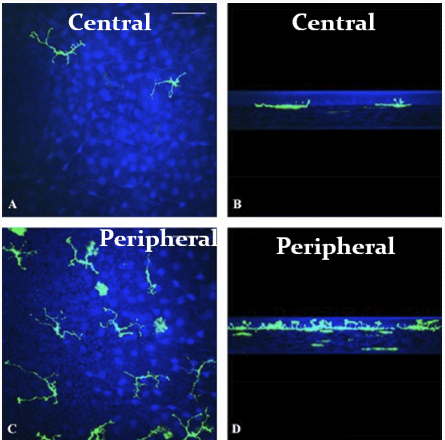
What increases in density due to a corneal inflammatory response?
Corneal dendritic cells and macrophages density increases upon inflammatory response from injury or infection
Is the corneal healing process perfect?
No, there are scar tissues from healing, clearly seen from surgeries
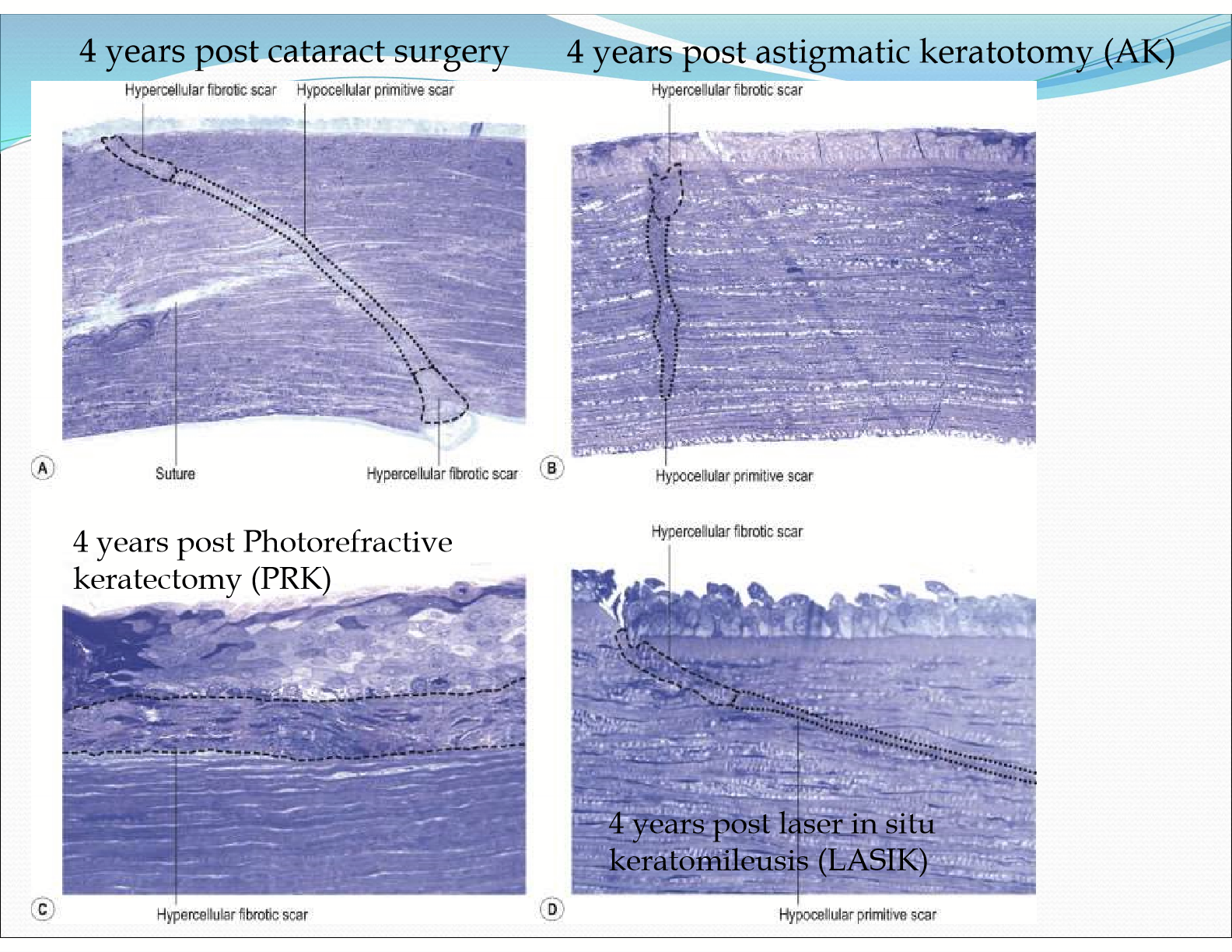
Why can corneal haze develop after photorefractive keratectomy (PRK)
The keratocytes transform into myofibroblasts, which are highly reflective cells that disrupt corneal transparency.
How long can the effects of LASIK affect they eye for?
12 months, affecting the corneal epithelial dendritic cells, tear neuropeptides, and corneal nerves
How do corneal nerves respond to injury?
They send impulses down the axon to the parent cell and also other non-stimulated branches (antidromically) and induces the release of neuropeptides (Substance P)
What is substance P?
A small neuropeptide found in most TG neurons that is released from nerve endings upon noxious stimuli
What does Substance P do?
It contributes to local inflammatory response through stimulation of cytokine production and epithelial mitosis and migration
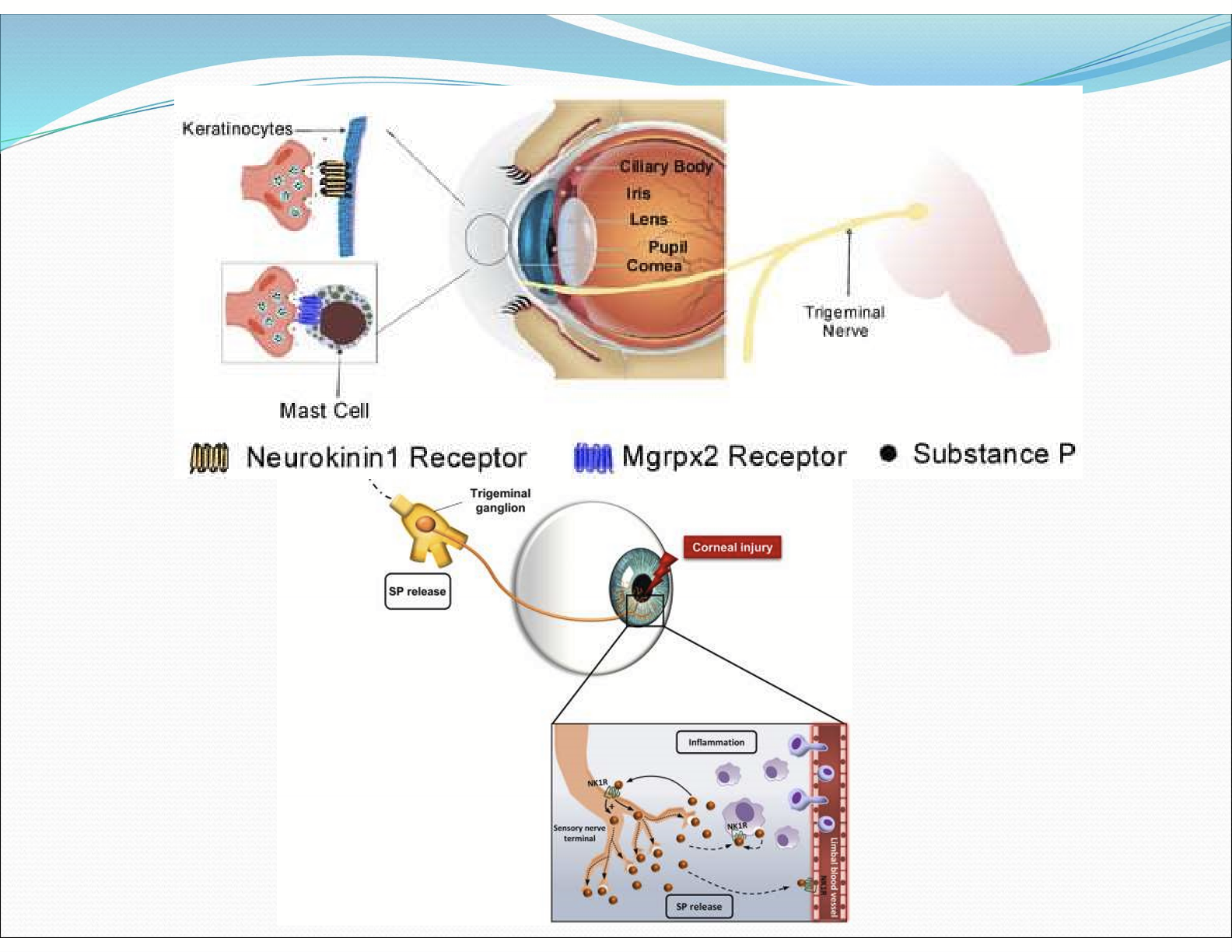
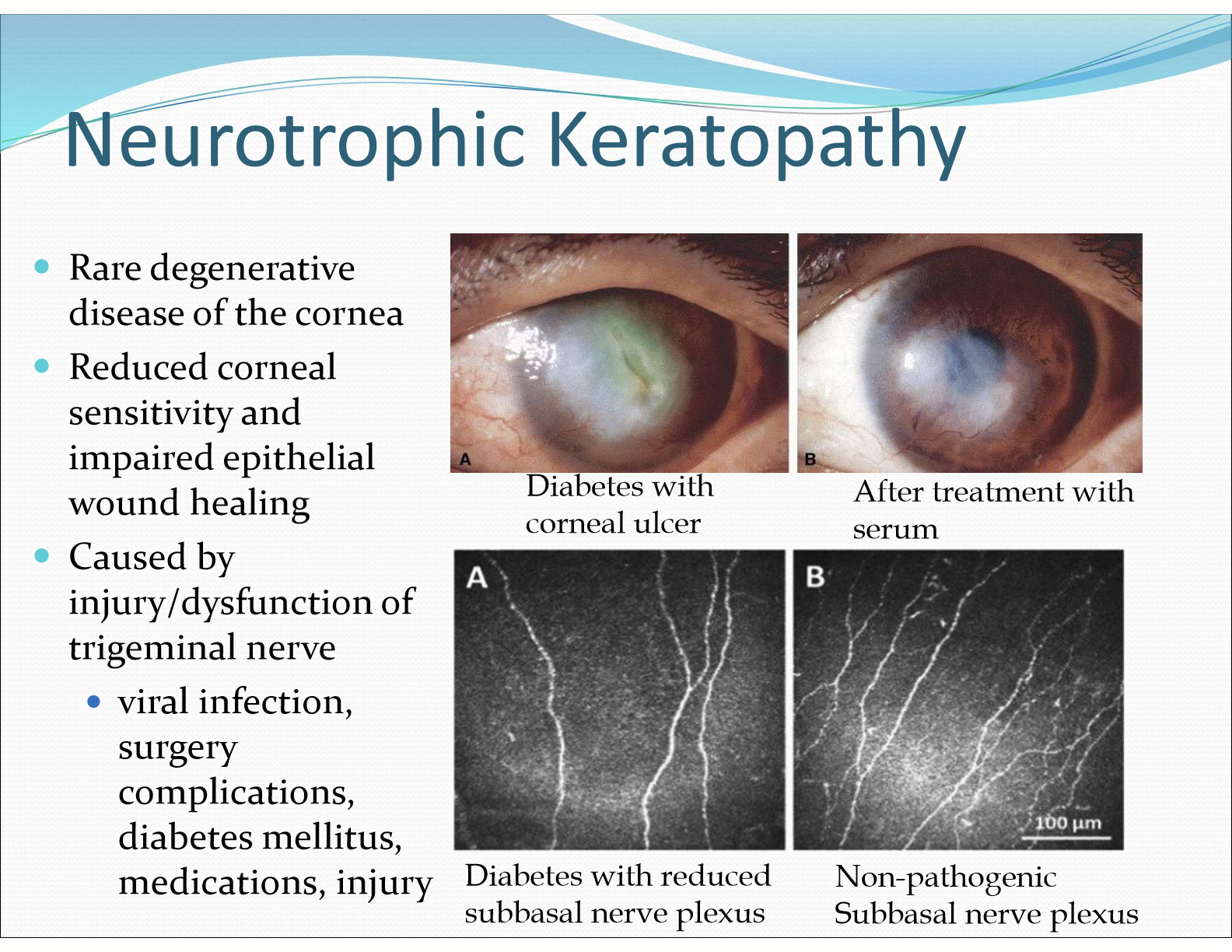
What is Neurotrophic Keratopathy?
A rare degenerative disease of the cornea due to reduced corneal sensitivity and impaired healing. It is caused by injury/dysfunction of the trigeminal nerve
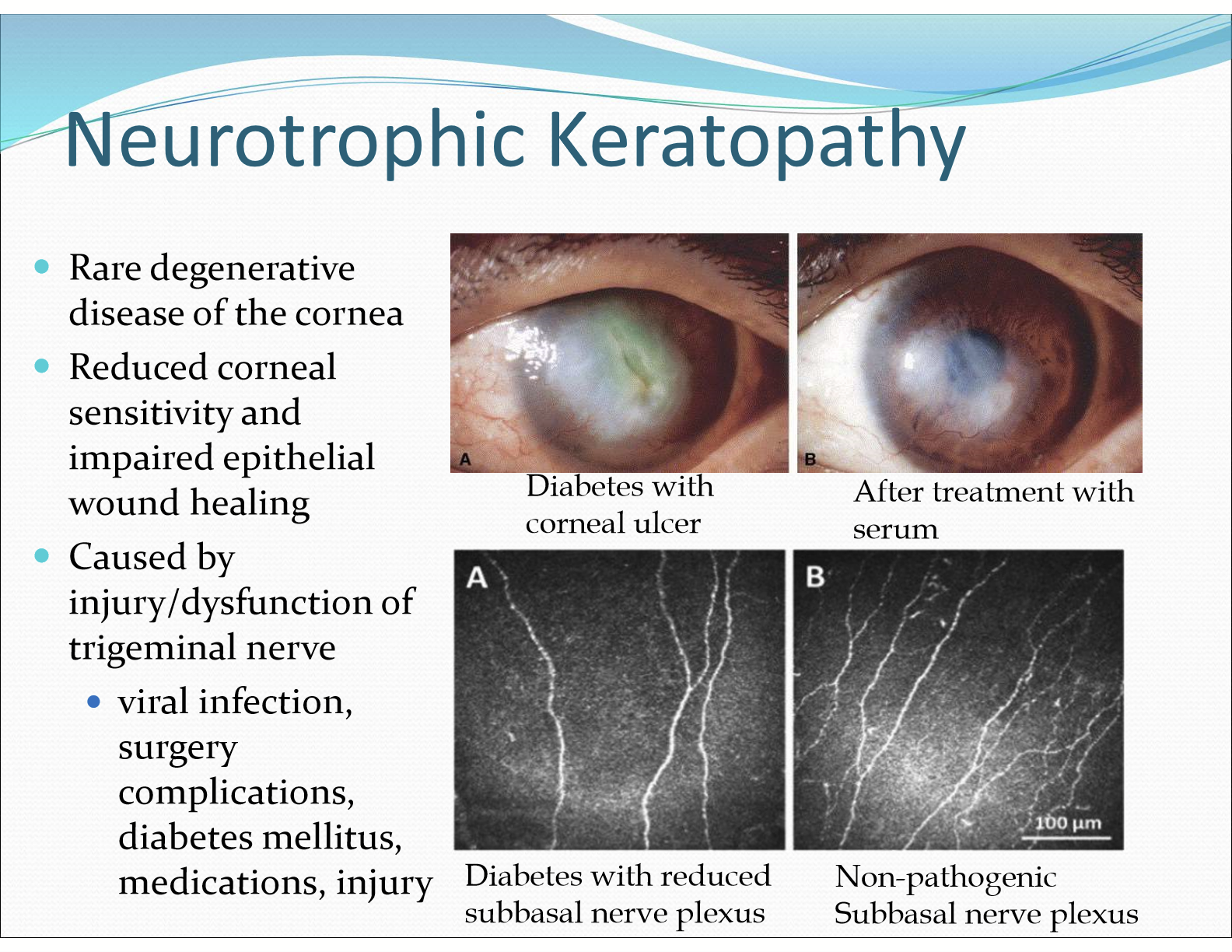
What are things that can damage the trigeminal nerve?
Viral infection, surgery complications, diabetes mellitius, medications, injuries