Congenital Heart Defects
1/5
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
6 Terms
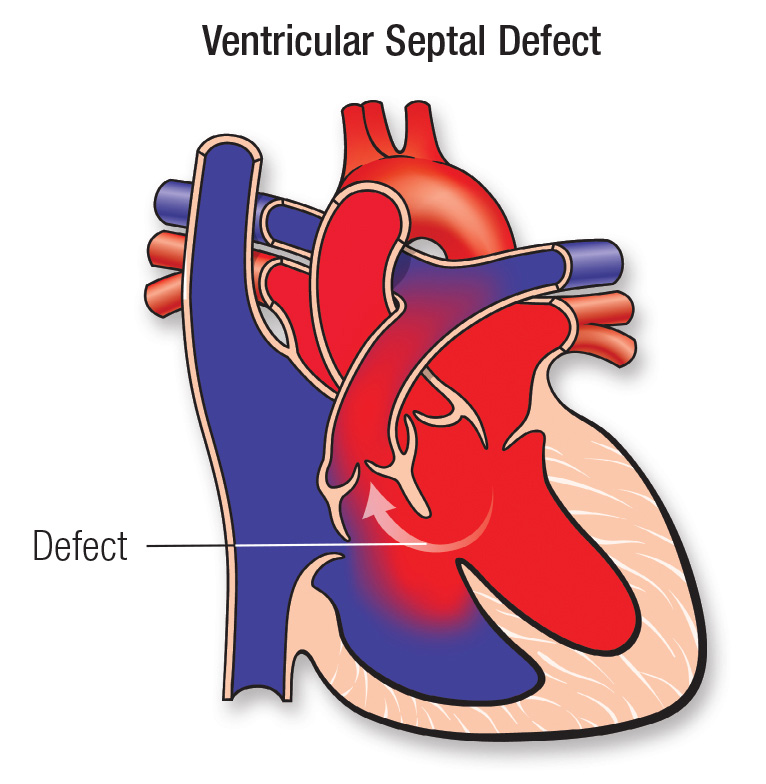
Ventricular Septal defect
Can be small or large
Assessment Data:
HF
Feeding and Failure to Thrive
Additional Diagnostics
Cath, ECHO, Chest X Ray, 12 Lead, Blood Gas,
Cardiac Cath: Why?
Evaluate the extent of flow being pumped to the pulmonary circulation and to evaluate hemodynamic pressures/stability
Nursing interventions:
Informed Consent
NPO
VS + Pre Op and Post Op Assessment
Check Pedal Pulses and Mark with a Marker
Allergies
Labs: Renal, CBC, CMP
Same considerations post cath for adult (i.e. BP frequently, lie flat, Tele, Immobilization, Assessments, etc)
Child will need to keep extremities straight for 4-6 hours with no movement and will be positioned on their back
Pulse and CMST checks above and below cath sites
I&Os; contrast can have a diuretic effect → think about hydration
Monitor tele for arrhythmias
Assessments, VS
Client Education:
Keep site dry for 3 days
Temperature and Elevated Temp call
Rest for 3 days
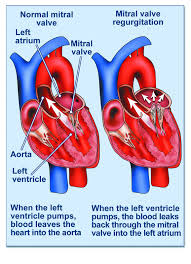
Mitral Regurgitation
Doesn’t close properly causing backflow
The mitral valve separates the left atrium and left ventricle (think tri before you buy (bicuspid = mitral)
Oxygenated blood is returned to the left atrium from the lungs and pumped into the left ventricle where the oxygenated blood is then pumped into systemic circulation
Surgical Planning:
Repair: Balloon Valvuloplasty Most Common
Replace: valve replacement - requires open heart surgery
Mechanical Valve: last 20-30 years, increased risk for thromboembolism; require lifelong anticoagulants, clicking noise drives patients crazy
Biologic Valves: made of pig/cow, last 8-20 years, no long-term anticoagulant unless there is a history of atrial fibrillation (3 months anticoagulated)
All valve replacements will require prophylaxis antibiotics
Post-Valve Replacement Interventions:
Assessments: Respiratory, Circulatory, Neuro
Intensive care for 24-72 hours
Transfer to telemetry stepdown unit
Client Teaching:
Coumadin (Warfarin) requires ongoing blood test ptINR
Desired INR when on warfarin 2.0-3.0
Biological Valves require only 3 months of anticoagulants
Prophylactic Antibiotics treatment before and after the following:
Dental procedures, GI surgeries, Cesarean deliveries, Surgeries for implanting a device, such as a pacemaker or defibrillator
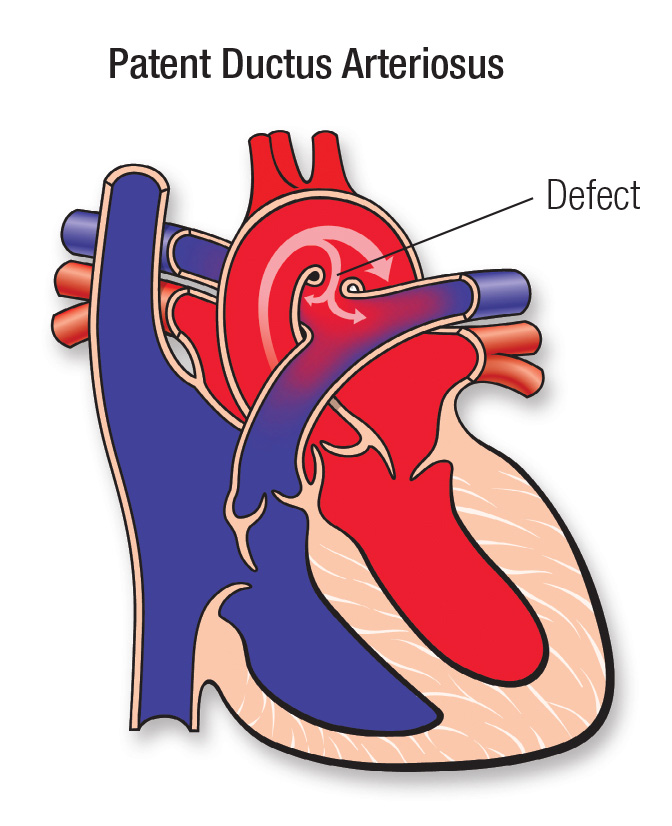
Patent Ductus Arteriosus (PDA)
Second most common congenital heart defects
Initially a PDA may produce no clinical effects, but with age may precipitate pulmonary vascular disease, typically causing symptoms by age 40
Right ventricular pressure increases in an attempt to overcome the increase in pulmonary pressure. The prolonged increase iN RV pressure creates right ventricular hypertrophy
Risk factors:
Non-modifiable:
Genetics, Age, Gender
Modifiable:
German measles during pregnancy
Uncontrolled diabetes
Drug/Alcohol Use
Presence of other congenital heart defects
In a child with a large left to right shunt, oxygen will decrease pulmonary vascular resistance while increasing the systemic vascular resistance, which leads to increased left to right shunting. Monitor the child carefully and use oxygen only as prescribed
Over oxygenation can lead to blindness due to increase pressure
Physical Exam:
Tachycardia
Tachypnea
Bounding Pulses
Widened Pulse Pressures (Systolic and diastolic pressures far apart)
Diastolic BP low
Harsh, Continuous, Machine Like Murmur
Loudest under the left clavicle at the first and second intercostal spaces
Fixes:
Pharmacological Management:
Indomethacin
NSAID
Given in 3 doses, 12 hours apart
Closed by coil embolization or device via cardiac catheterization
May also be surgically ligated
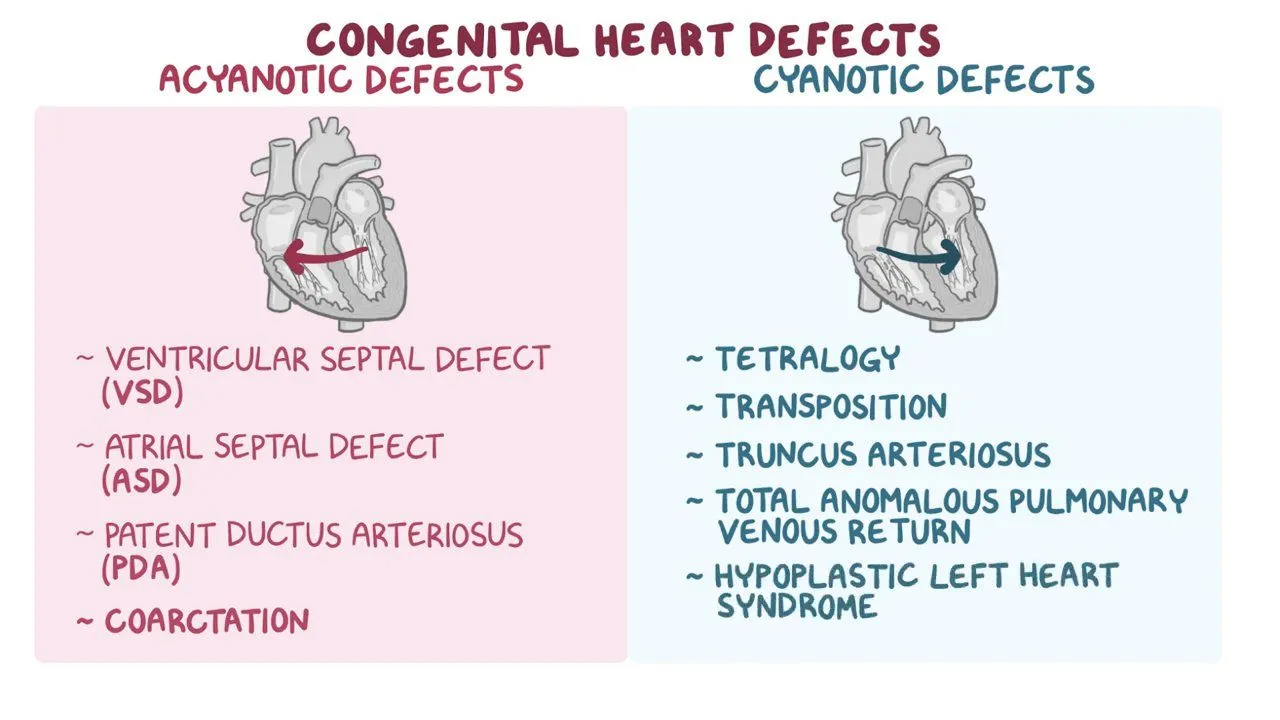
Cyanotic congenital heart defects
** usually start with T
Decreased Pulmonary Flow:
Tetralogy of Fallot: 4 defects
Pulmonary Stenosis, VSD, Overriding Aorta, Right Ventricular Hypertrophy
Tricuspid Atresia: 3 tricuspid valve
Mixed Disorders:
Truncus Arteriosus: Vessels join to make 1
Hypoplastic Left heart Syndrome
Transposition of the Great VesselsL 2 major vessels switched
Nursing Priority:
Infants and children less than 2 years with CHD should receive a monthly RSV vaccination during RSV season
Nursing Assessments:
Cyanosis, Cooling, Clamminess of skin
RR and work of breathing
SpO2 via pulse oximeter
Retractions, SOB, noisy breathing
Changes in skin color with Positional Changes (fetal position/Knee bending)
Loud, Harsh Murmur on auscultation of the heart (TOF)
Adventitious sounds on auscultation of the lungs
Clubbing of fingers
Irritability
Labs for polycythemia (when hemoglobin and hematocrit are raised to try to compensate)
Prepare infant and family for ECHO, EKG, and cardiac cath
Nursing Assessment continued:
Note color changes with activity, crying and feeding
Hypercyanosis develops suddenly → increased cyanosis, Hypoxia, dyspnea, agitation
Usually 60-80% at baseline
4mL/kg/hr is okay for IV fluids (dextrose or saline)
As the child gets older they may compensate for hypercyanotic spells
Specific postures such as bending the knees, assuming the fetal position, squatting
These positions improve pulmonary flow by increasing systemic vascular resistance
**Tet spell = hypercyanotic
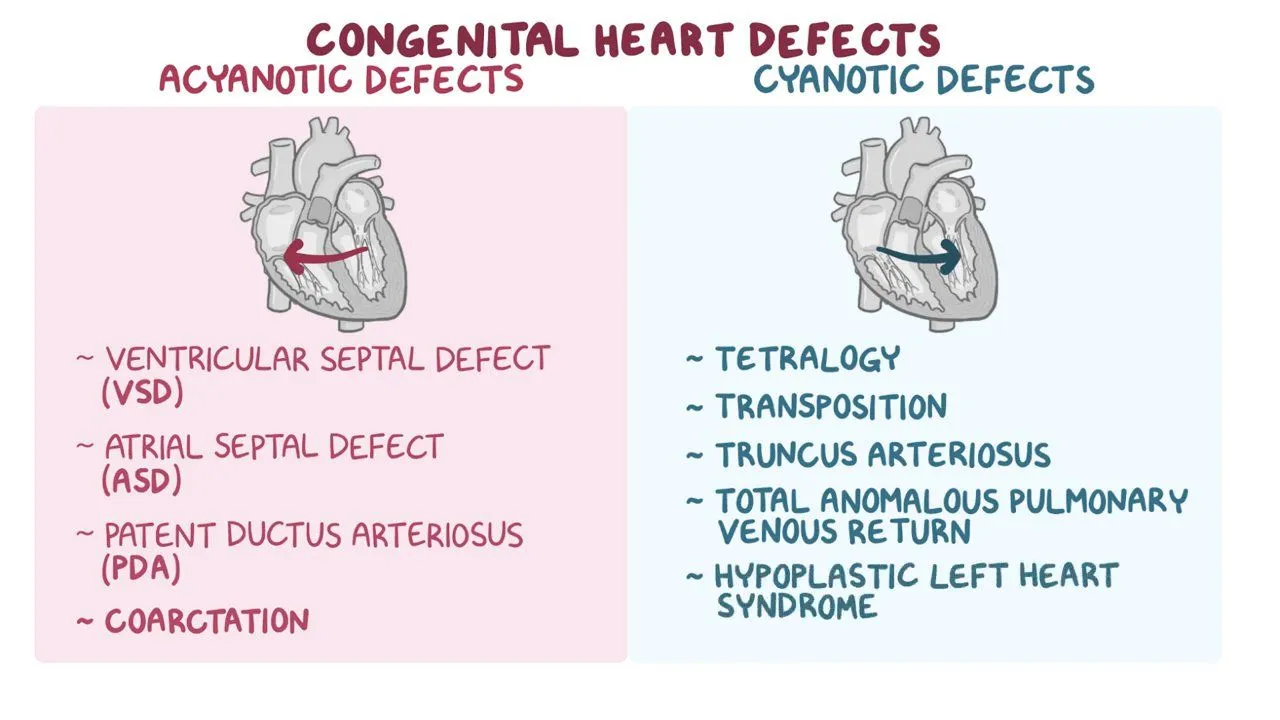
Acyanotic Congential defects
Obstructive Disorders:
Coarctation of the aorta
Aortic Stenosis
Pulmonary Stenosis
Increased Pulmonary Blood flow (Left to right shunts)
Patent ductus arteriosus (PDA)
Atrial Septal Defect (ASD)
Ventricular Septal Defect (VSD)
Tetralogy of Fallot
TOF Interventions:
Avoiding activity in extreme weather
Providing small feeding volumes → high calorie no more than 20 min
The need for prophylaxis antibiotics for dental care
Oxygen 100% in the face mask
Report any temperature elevation greater than 100.4F
For tet spells position fetally
Good hydration → bc of polycythemia causing thick blood
Gavage feeding: promotes less metabolic demand for feeding
RSV Vaccinations
TOF Fixes:
4-12 months for corrective surgical fixes
Initially palliation with systemic to pulmonary anastomosis:
Blalock-Taussig Shunt: an end to side anastomosis of the subclavian artery and the pulmonary artery
Avoid BP measurements and venipunctures in the affected arm, pulse will not be palpable in that arm because of the use of the subclavian artery for the shunt
Monitor for ventricular arrhythmias following a corrective repair
Waterston Shunt: an anastomosis of the descending aorta and the pulmonary artery
Definitive correction involves patch closure of the VSD and repair of the pulmonary valve and the right ventricular outflow tract