The Inflammatory Response: Neutrophils & Macrophages
1/98
Earn XP
Description and Tags
Exam 1 - Lectures 2, 3, & 4
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
99 Terms
What are the 3 major way microbes can gain access to the body?
inhalation, ingestion, wounds
What is the general purpose of sentinel cells?
recognize invaders → signals generated → attract defensive cells to site of invasion
What are the sentinel cells?
dendritic cells, mast cells, eosinophils, neutrophils, macrophages, lymphocytes
What are the major 3 sentinel cells that possess the ability to recognize and phagocytize pathogens?
dendritic cells, mast cells, macrophages
What are the 2 possible stimuli that can result in an inflammatory response?
cellular damage
foreign antigenic substance (pathogen)
What does DAMP stand for?
damage associated molecular patterns
What are some of the possible causes of DAMP?
immunological rxn
nutritional imbalances
genetic defects
hypoxia
microorgansms
chemical agents
What does PAMP stand for?
pathogen associated molecular patterns
What are PAMPs?
unique components of microorgansms that are essential for their survival
T/F: PAMPs are found on normal host tissue.
FALSE - they are NOT found on host tissue
What are some examples of PAMPs?
unmethylated DNA, cell walls, bacterial flagella, etc
How does the host cell recognize the DAMP or PAMP?
toll-like receptors
What are toll-like receptors?
transmembrane proteins that mediate PAMP recognition
What happens when PAMPs bind to a toll-like receptor?
initiates intracellular signal transduction pathways that culminate in NF-kB
What is NF-kB?
major regulator of inflammatory gene transcription regulating the expression of chemokines, cytokines, etc
Chemokines and cytokines are examples of what?
proinflammatory genes
Toll-like receptors are found in high numbers on which cells?
dendritic cells, macrophages, & mast cells
T/F: Each TLR recognizes different components of PAMP.
TRUE - there are close to 13-15 TLR understood at this point
Sentinel cells mediate inflammation by way of what 3 things?
vasoactive molecules, cytokines, antibacterial molecules
What is considered the hallmark of acute inflammatory response?
vasodilation
What are sentinel cells?
circulating cell population that detects invaders or tissue damaged
What do sentinel cells do?
release cytokines and other substances that cause necessary vascular changes, and attract & activate phagocytic cells
Which cells are the first cells to arrive (primary effector) and deal with most if not all the invading organisms.
neutrophils
T/F: Sentinel cells are strategically located throughout the body to help mediate the inflammatory response.
TRUE
Hey this is important
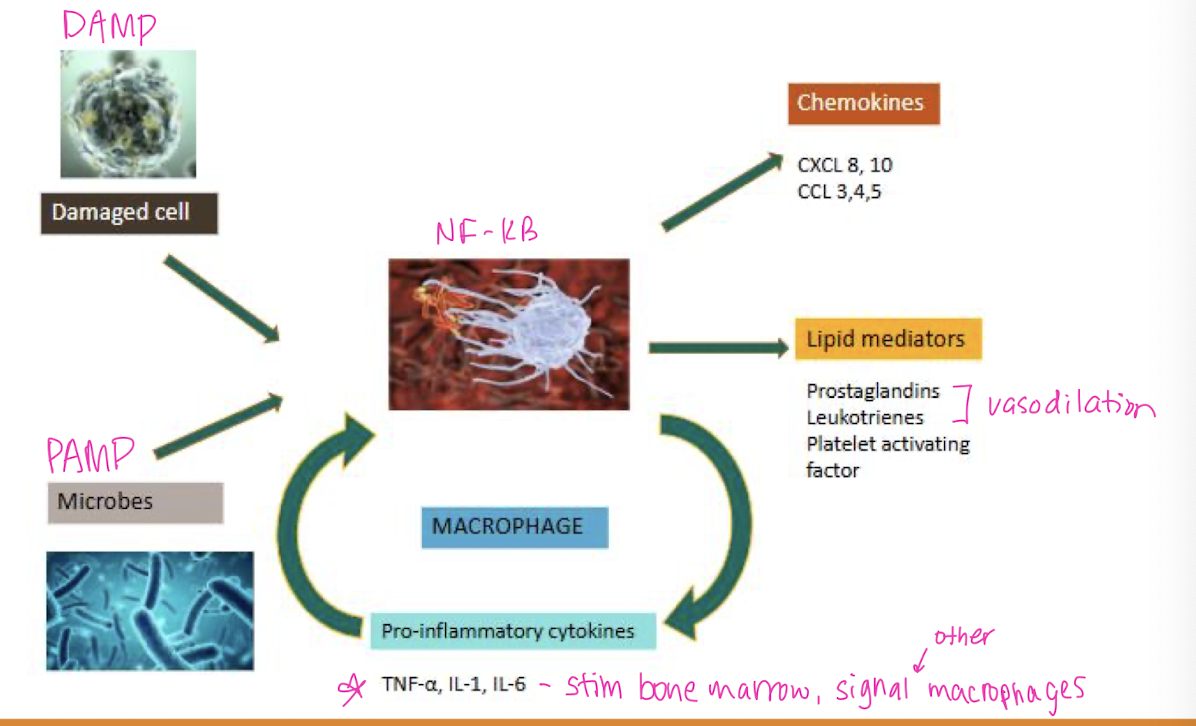
What is the key to mediating the immune response?
cytokine production
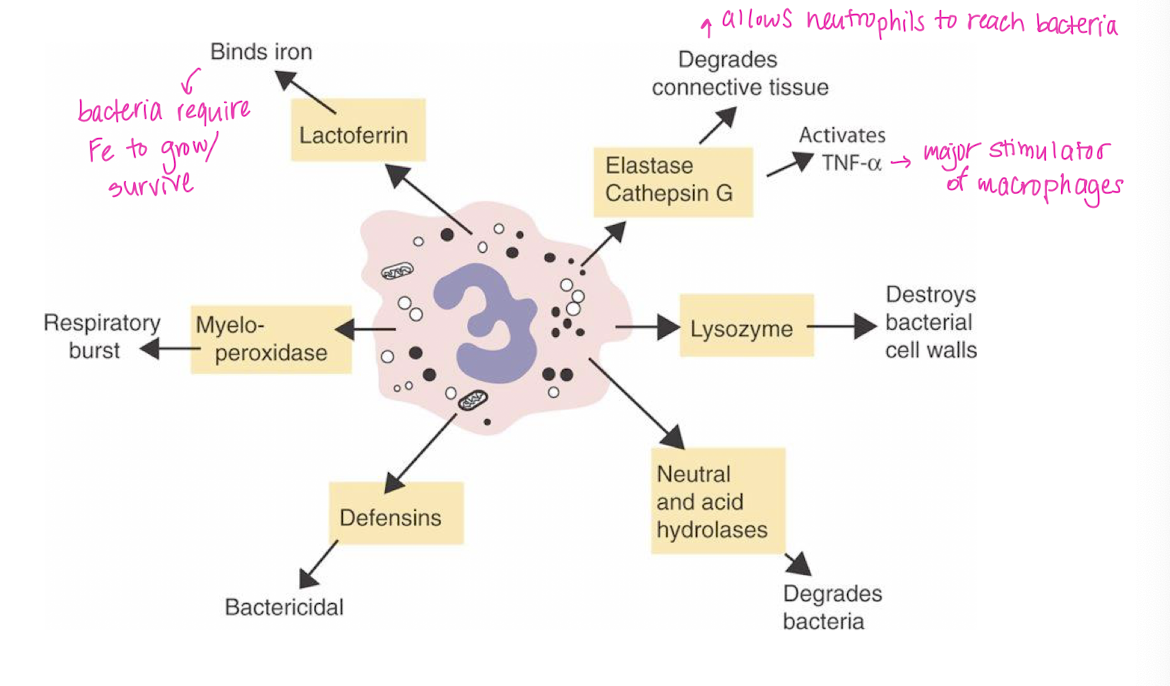
What are the 4 major cytokines we discussed?
Tumor necrosis factor α (TNFα)
Interleukin-1 (IL-1)
Interleukin-6 (IL-6)
Chemokines
What are the 2 major sources for the 4 cytokines discussed?
macrophages & endothelial cells
In addition to macrophages and endothelial cells, what other cells can produce TNFα?
NK cells, T cells
What are the main actions of TNFα and IL-1?
activates endothelial cells → vasodilation
What is the main action of IL-6?
acute phase protein synthesis by the liver
What is the main action of chemokines?
regulate cell movement
T/F: Inflammatory cytokines only have local effects.
FALSE - systemic effects
What do inflammatory cytokines do?
stimulate hypothalamus to produce prostaglandins → fever (pyrogen)
stimulate liver to produce acute-phase proteins
A fever can be considered an _______ immune response.
innate
What do acute-phase proteins do?
cause “sickness behavior” → loss of appetite, lethargy, protein catabolism (muscle wasting)
Inflammatory cytokines are responsible for
clinical illness → septic shock, cachexia
What is the overall action of cytokines?
attract leukocytes to sites of infection
Cytokines trigger the formation of _________ on leukocytes.
lamellipodia → allows movement
Cytokines stimulate actin___________.
polymerization/ depolymerization
Cytokines increase expression of __________ on leukocytes.
adhesion molecules (β-integrins)
What are β-integrins?
receptor necessary for WBC to leave the vessels and enter the connective tissue
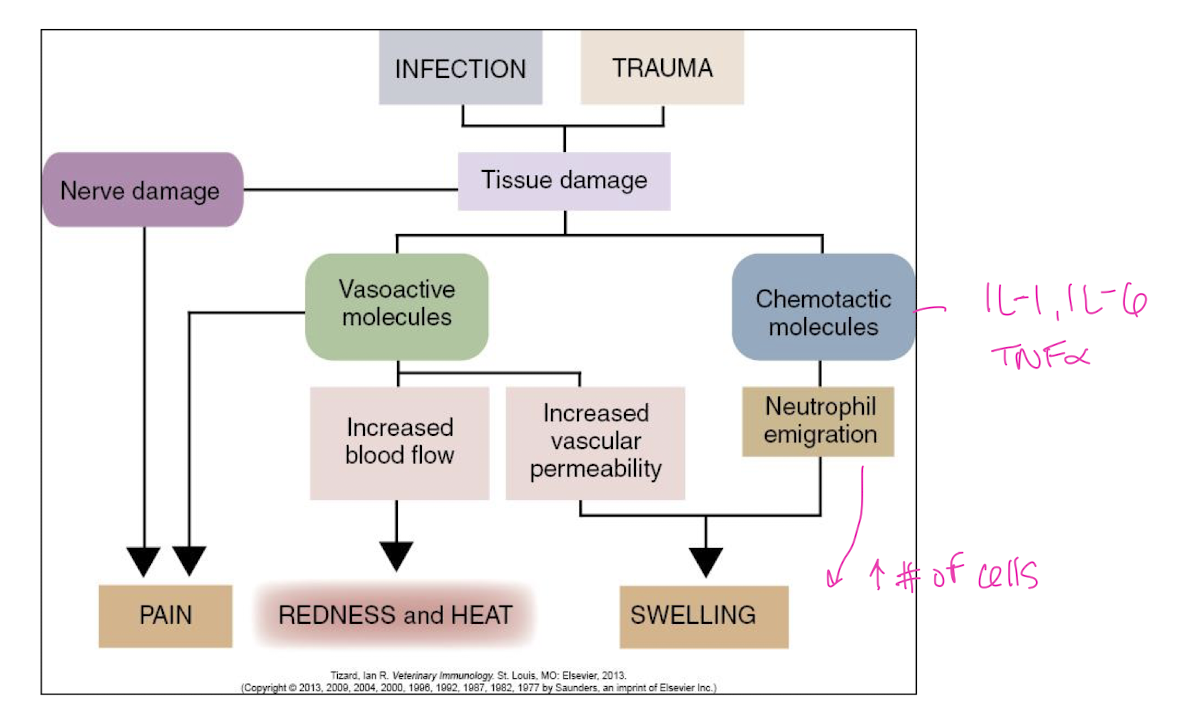
What are the 5 cardinal signs of inflammation?
Redness → increased blood flow to site of inflammation
Heat → increased blood flow to site of inflammation
Swelling → accumulation of fluid and cells
Pain → stimulation of sensory neurons by inflammatory mediators
Loss of function → tissue damage
Inflammation consists of how many changes in the small blood vessels in the area of infection?
3
What is the first change that occurs to the small blood vessels in the area of infection/ inflammation?
arterioles dilate → increased blood flow to affected area
What is the second change that occurs to the small blood vessels in the area of infection/ inflammation?
capillaries become more permeable → extra fluid + large serum proteins (antibody, complement) escape from blood
What is the term for the fluid containing large serum proteins that escapes from the blood during inflammation?
transudate → straw-colored yellow fluid, cloudy (protein rich)
What is the third change that occurs to the small blood vessels in the area of infection/ inflammation?
leukocytes migrate through venule walls into extravascular tissue
What is the term for WBCs when they migrate through venule walls into extravascular tissue during inflammation?
exudate
What is the hallmark of acute inflammation?
inflammation
T/F: There is a brief moment of transient vasoconstriction during the inital stages of inflammation.
TRUE → shock response of the nervous system that stimulates platelets
What does the leukocyte adhesion cascade (LAC) ensure?
that appropriate WBCs leave the appropriate vessel at the appropriate area of the body
ex: cut on finger → need WBCs to exit at the finger not a toe
What is the leukocyte adhesion cascade (LAC) mediated by?
cytokines
Explain the process of the LAC (vaguely)
macrophage releases cytokines → intravascuar WBC attracted to P & E-selectin on the endothelium membrane → binds in a “fast on - fast off” manor → acts as a speed bump to slow the WBC → WBC continues to roll down the endothelial membrane, binding and releasing from various receptors → as WBC rolls, it becomes more activated → WBC binds to integrins causing the it to stop → the binding changes cytoskeleton of WBC changing its shape (exit hole better) → more cytokines are activated → tell WBC that has just exited the vessel to travel to the recruiting WBC
Take a gander at this chart
What are the main effects of cytokines on the hypothalamus?
fever, anorexia, sleepiness, depression
What are the main effects of cytokines on the liver?
increased synthesis of acute-phase proteins, iron sequestration (keep from bacteria)
What is the main effect of cytokines on bone marrow?
increased WBC production (neutrophilia)
The liver produces increased amounts of _________ in response to proinflammatory cytokines.
acute phase proteins
What are the 5 main acute phase proteins that are produced by the liver in response to proinflammatory cytokines?
SAA (serum analoid A)
Fibrinogen
CRP (C reactive protein)
Ceruloplasmin
AGP (Alpha-1-glycoprotein)
What does SAA do?
role in WBC chemotaxis and induction of enzymes that degrade extracellular matrix
What does fibrinogen do?
plays a crucial role in hemostasis
What does CRP do?
assists in complement binding to antigenic or damaged cells
What does ceruloplasmin do?
oxidizes iron, facilitating for ferritin, inhibiting microbe iron uptake
What does AGP do?
increases with sepsis → exact function unclear
Increased serum electrophoresis of which protein fractions are features of inflammation?
α1, α2, β
Antibodies are found in which protein fraction?
γ (gamma)
In the context of innate immunity, acute phase proteins assist in the
recognition of microbial moieties (functional group/ subunit) and damaged cells or tissues
The major blood leukocyte is the
neutrophil
Which cell follows the neutrophil (primary effector cell) and deals with the remaining invaders while also cleaning up the mess?
macrophages
In order for the neutrophil to perform a specific action, the ________ must first be triggered.
correct receptor
ex: antibody receptor vs complement receptor, vs cell adhesion molecules
Once the correct neutrophil receptor is engaged, the activated neutrophil releases a ______.
net
What does the neutrophil net do?
directs neutrophil granules and contents toward the inflammatory stimulus
What are the 3 main steps of releasing the neutrophil net?
Nuclear envelope ruptures
Proteolytic breakup of chromatin
Plasma membrane ruptures and releases the net
What is the neutrophil net directed toward?
bacteria, PAMPs, and cytokines
In addition to casting the neutrophil net, the neutrophil undergoes
respiratory burst
What is respiratory burst?
a process by which numerous antimicrobial compounds and radicals are produced that can neutralize or eliminate pathogens
What are the key steps in respiratory burst in neutrophils?
NADPH oxidation & superoxide production
Superoxide conversion to hydrogen peroxide
Further conversion of hydrogen peroxide to other ROS (reactive O2 species) like hypochlorous acid
Simultaneous neutralization of ROS
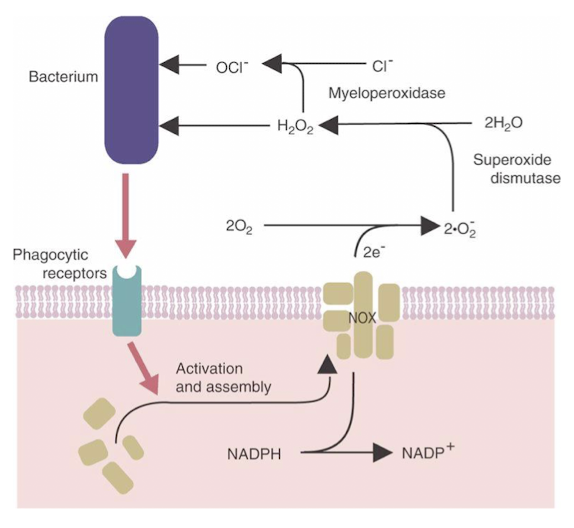
What are the contents of the primary granules of neutrophils?
Defensins → bactericidal
Myeloperoxidase → respiratory burst (provide Cl for hypochlorous acid)
Neutral & acid hydrolases → degrade bacteria
Lysozyme → destroys bacterial cell walls
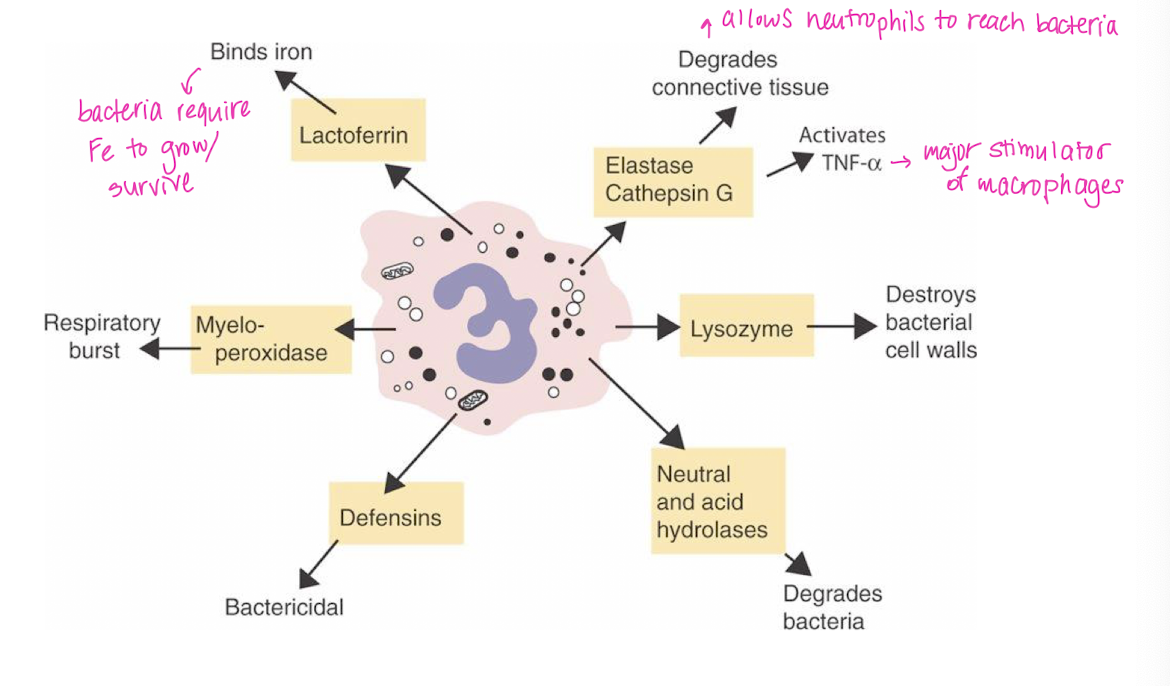
What are the contents of the secondary granules of neutrophils?
Lactoferrin → binds iron
Collagenase → degrades connective tissue
Lysozyme → destroys bacterial cell walls
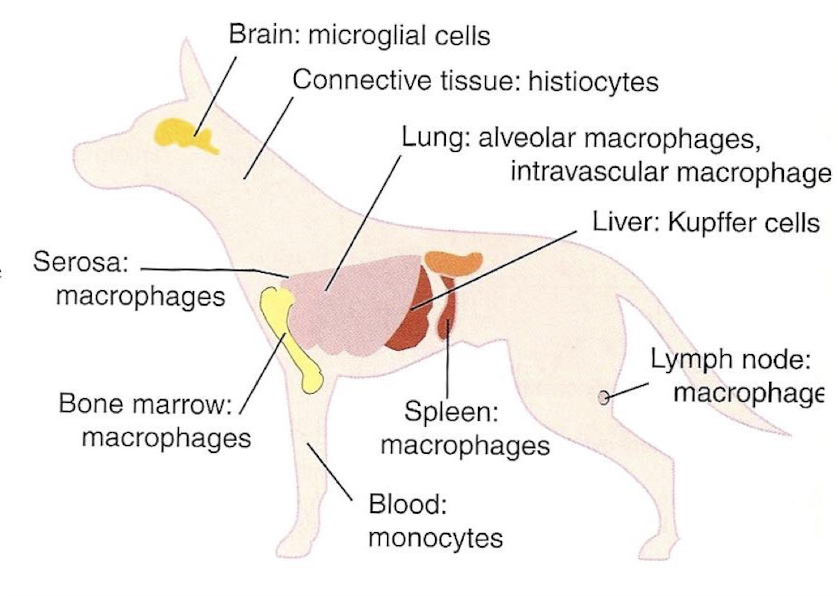
Macrophages arise from a ________.
Myeloid stem cell
Macrophages mature into _______ in the blood.
monocytes
T/F: Once macrophages mature into monocytes in the blood, they remain only in circulation.
FALSE → they populate many organs in the body
Nomenclature of macrophages is based on what?
the organ in which they reside

Similar to neutrophils, in order for a macrophage to perform a specific action, the __________ must first be triggered.
correct receptor
T/F: Many macrophage cell surface receptors are grouped, meaning they have similar functions.
TRUE
What are the important cytokines produced by macrophages?
IL-1, IL-23, TNFα, IL-18, IL-12, IL-6
Macrophages are very efficient ________ cells.
phagocytic
What are the other phagocytic cell types?
neutrophils, monocytes, & dendritic cells
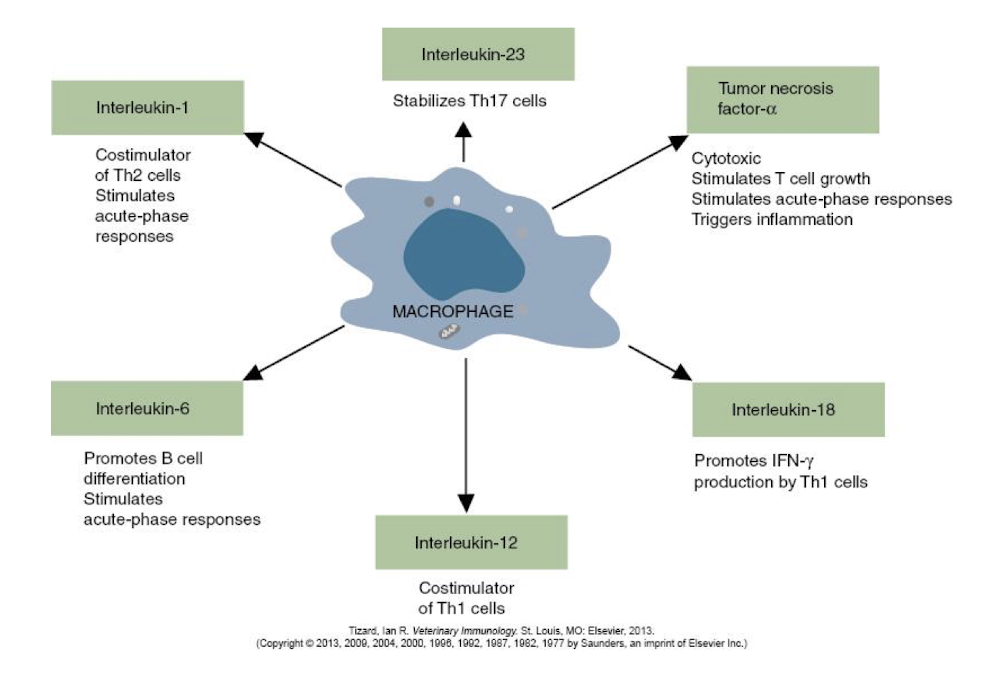
What are the 4 key steps of phagocytosis?
Chemotaxis → migration to the offending agent via chemotactic gradient
Adherence → mediated by cell surface receptors
Ingestion → the macrophage engulfs the particle
Digestion → breakdown of the particle effectively neutralized or kills the agent
How is phagocytosis triggered?
by the binding of a pathogen to receptors on the surface of the phagocyte (macrophage, neutrophil, etc)
Each step in phagocytosis is mediated by specific __________ interactions.
receptor-ligand
T/F: Only one receptor must be triggered in order to initiate and complete the phagocytic response.
FALSE → more than one
What is one of the main mechanisms by which macrophages recognize pathogens?
opsonization
What is opsonization?
process by which molecules (antibodies & complement) bind to the surface of a pathogen making that pathogen more susceptible to phagocytosis and destruction
The molecules that bind to the surface of a pathogen to induce phagocytosis are called ______.
opsonins
What is an essential function for cellular activation and deactivation?
crosstalk via cytokine network (i.e. macrophage & neutrophil crosstalk)
Different species clear particles from the blood in different areas of the body. Which sites are the most common among dogs, rabbits, guinea pigs, rats, and mice?
liver and spleen
Different species clear particles from the blood in different areas of the body. Which site is the most common among calf, sheep, and cats?
lungs