Carbon Dioxide
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
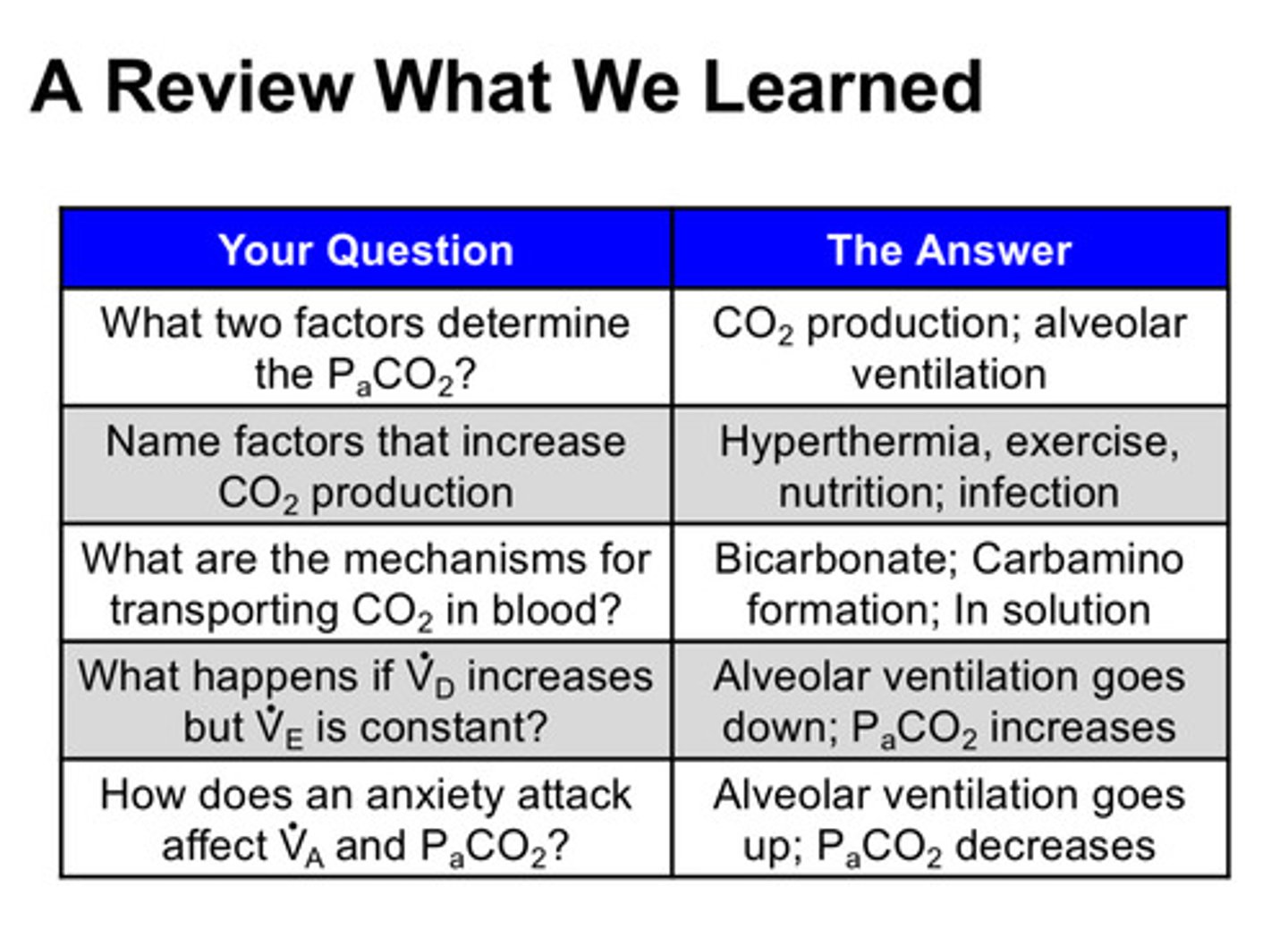
getting rid of high CO2 is so important to the body, that it is a bigger driver of respiration than?
low O2
ventilation is synonymous with what?
getting rid of CO2 (good ventilation will lead to good oxygenation obviously)
what 6 factors increase CO2 production
1) exercise
2) fever
3) infection
4) feeding
5) hyperthyroidism
6) seizures
what 4 factors decrease CO2 production
1) hypothermia
2) antipyretic therapy (medications that reduce fever, ex: acetaminophen)
3) holding nutrition
4) neuromuscular blockade (medications that take away muscle function)
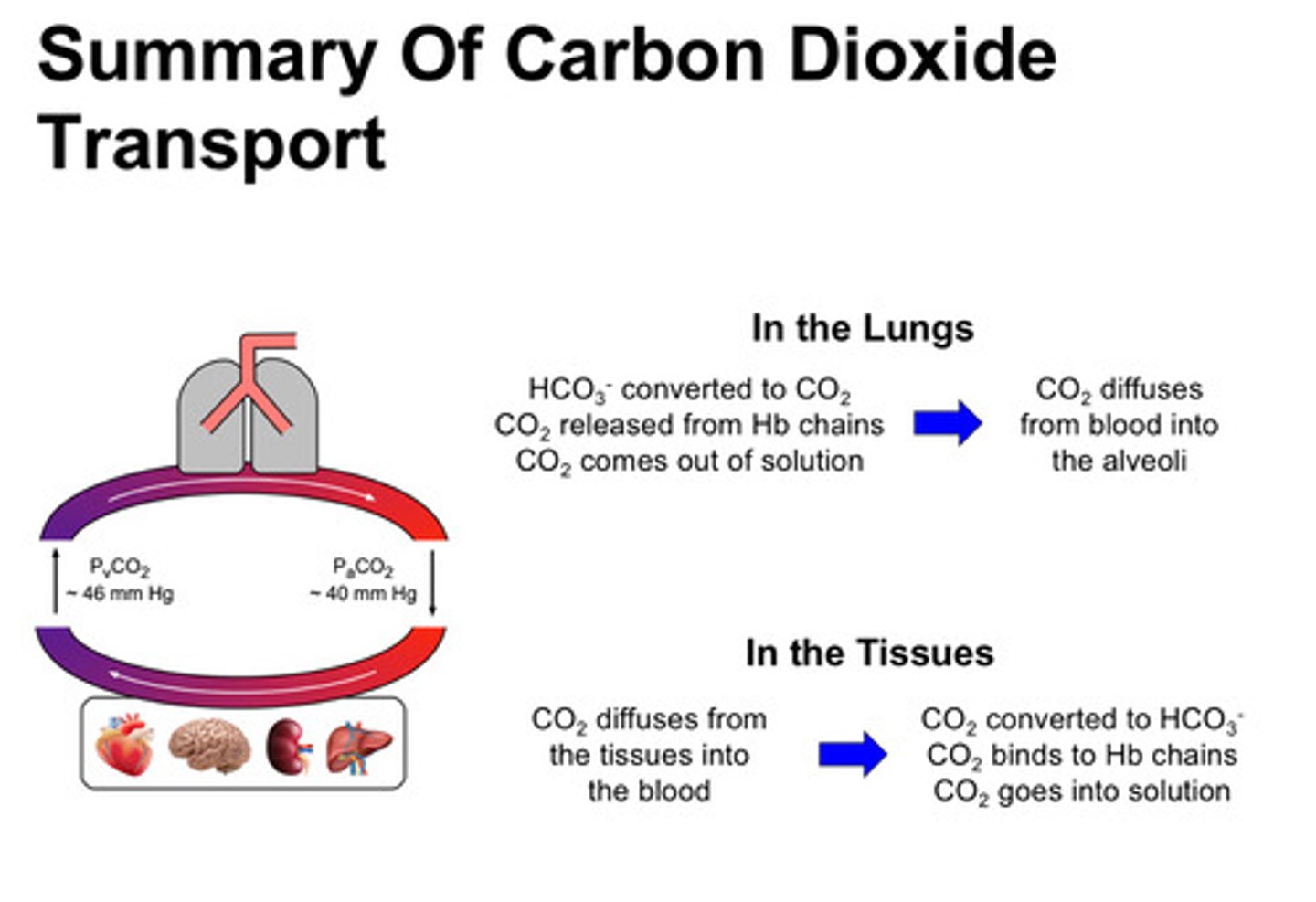
by what 3 means is CO2 carried in the blood?
1) dissolved in solution: 2.9 mL/100 mL blood (6% total CO2 transport)
2) bound to hemoglobin: 2.1 mL/100 mL blood (4% total CO2 transport)
3) conversion to bicarbonate: 42 mL/ 100 mL blood (90% total CO2 transport)
even though CO2 is much more soluble in blood than oxygen, you still cannot transport enough CO2 into solution alone for this to be the only transport tool; what percent of total CO2 transport is dissolved in the blood?
only 6%
when CO2 binds to hemoglobin, where does it bind to on the Hb?
does not bind to the heme moiety that oxygen binds to, but binds to the amine groups on the terminal ends of the hemoglobin chains —> these are referred to as carbamino groups
what is the primary mechanism that we transport CO2 to the lungs?
conversion to bicarbonate!
what is the ubiquitous enzyme that is used to get CO2 into a transportable form?
carbonic anhydrase; we convert CO2 + H2O —> carbonic acid —> bicarbonate ion
(reaction moves to the right in tissues and to the left in the lungs)
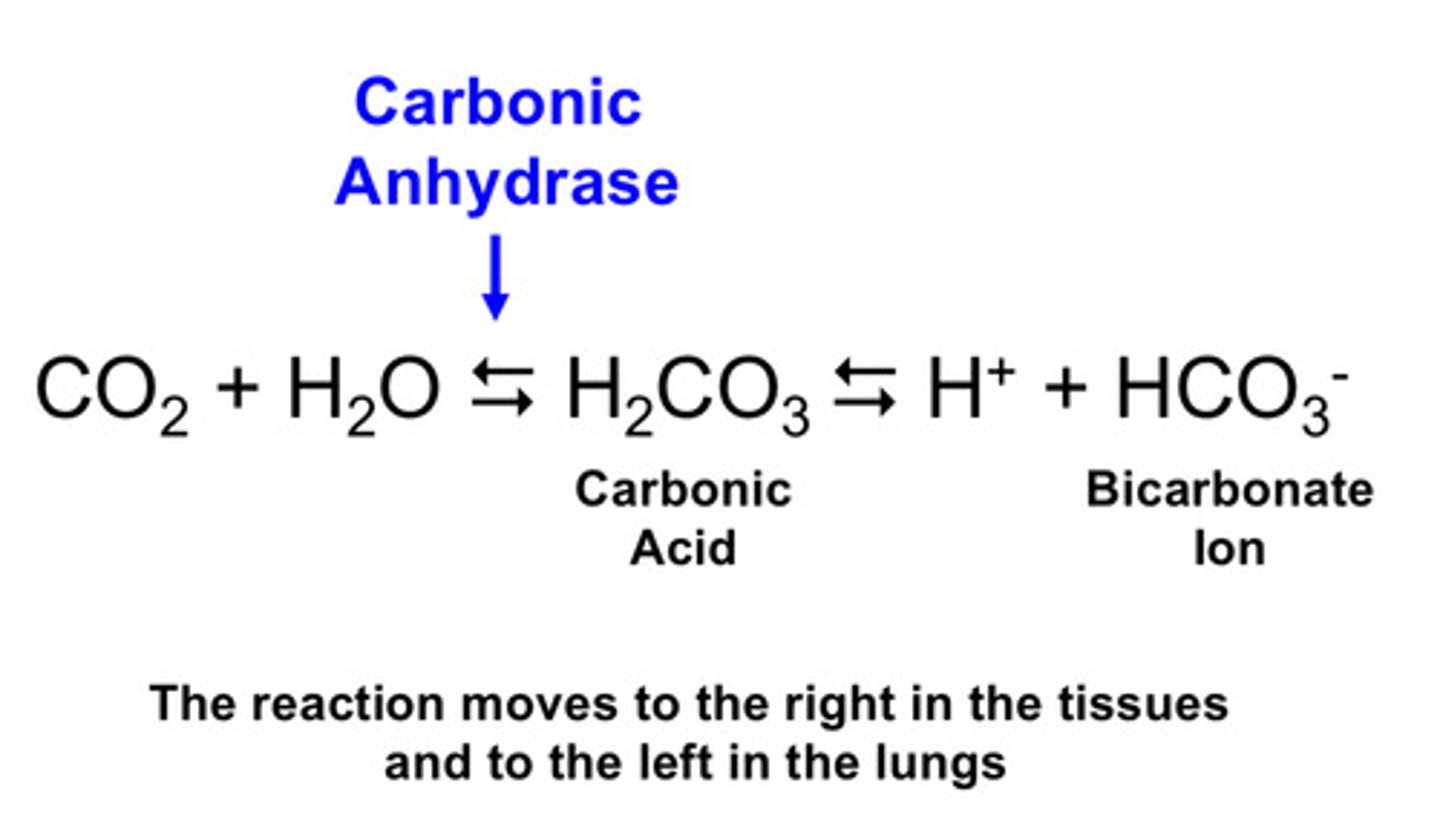
describe the conversion of CO2 into bicarbonate and how they travel to get to their appropriate places
1) CO2 is produced in the tissues, converted into bicarbonate, and is transported into the blood
2) in the lungs, bicarbonate is converted back to CO2, which then diffuses across the alveolar capillary barrier and leaves via ventilation
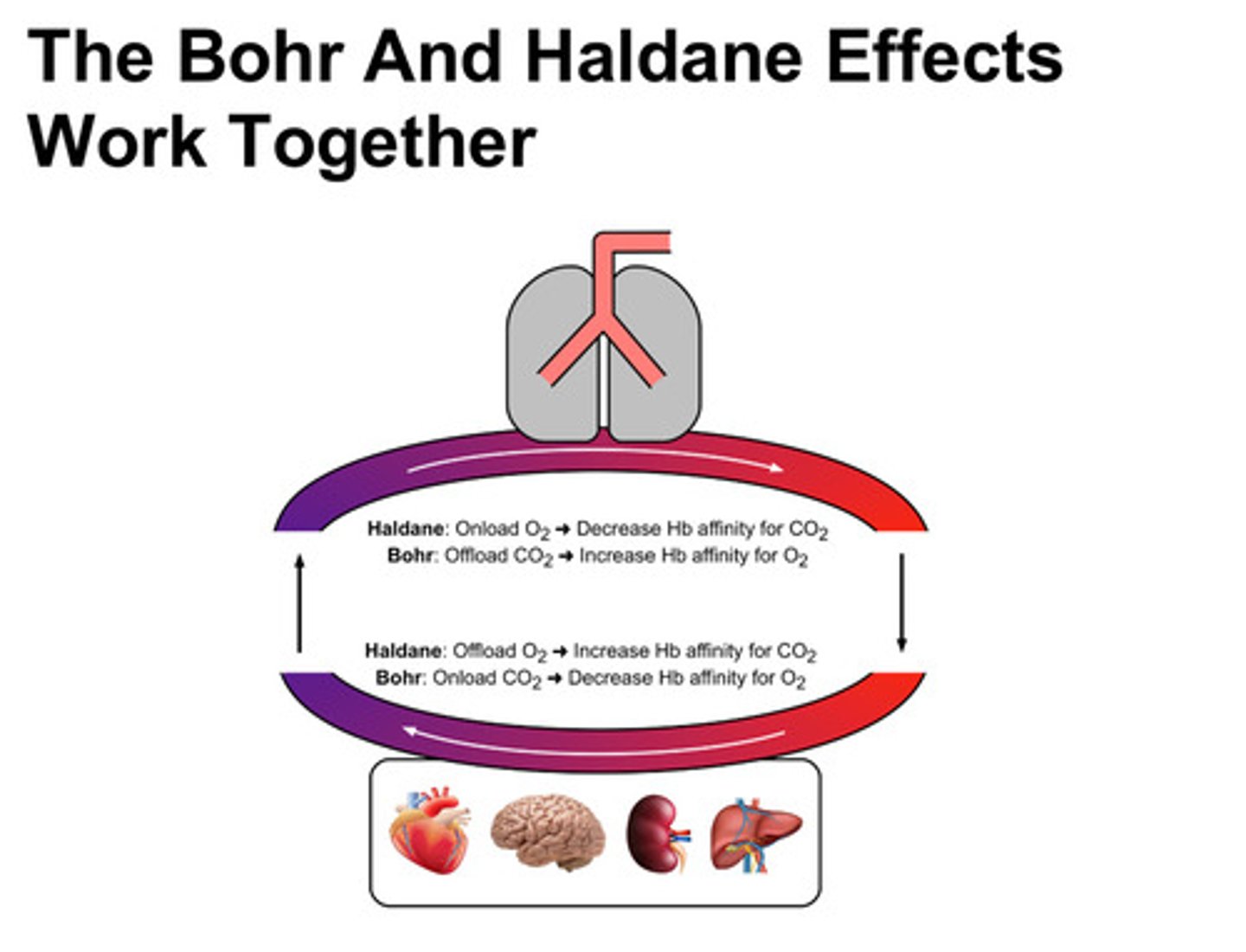
what is the haldane-bohr effect?
the haldane effect: oxygenation of Hb in the lungs decreases the ability of Hb to carry CO2 as carbamino groups
the bohr effect: increase of PCO2 in the tissues causes Hb to release more oxygen
these 2 effects work together to assist with the onloading and offloading of oxygen and carbon dioxide in the tissues and lungs
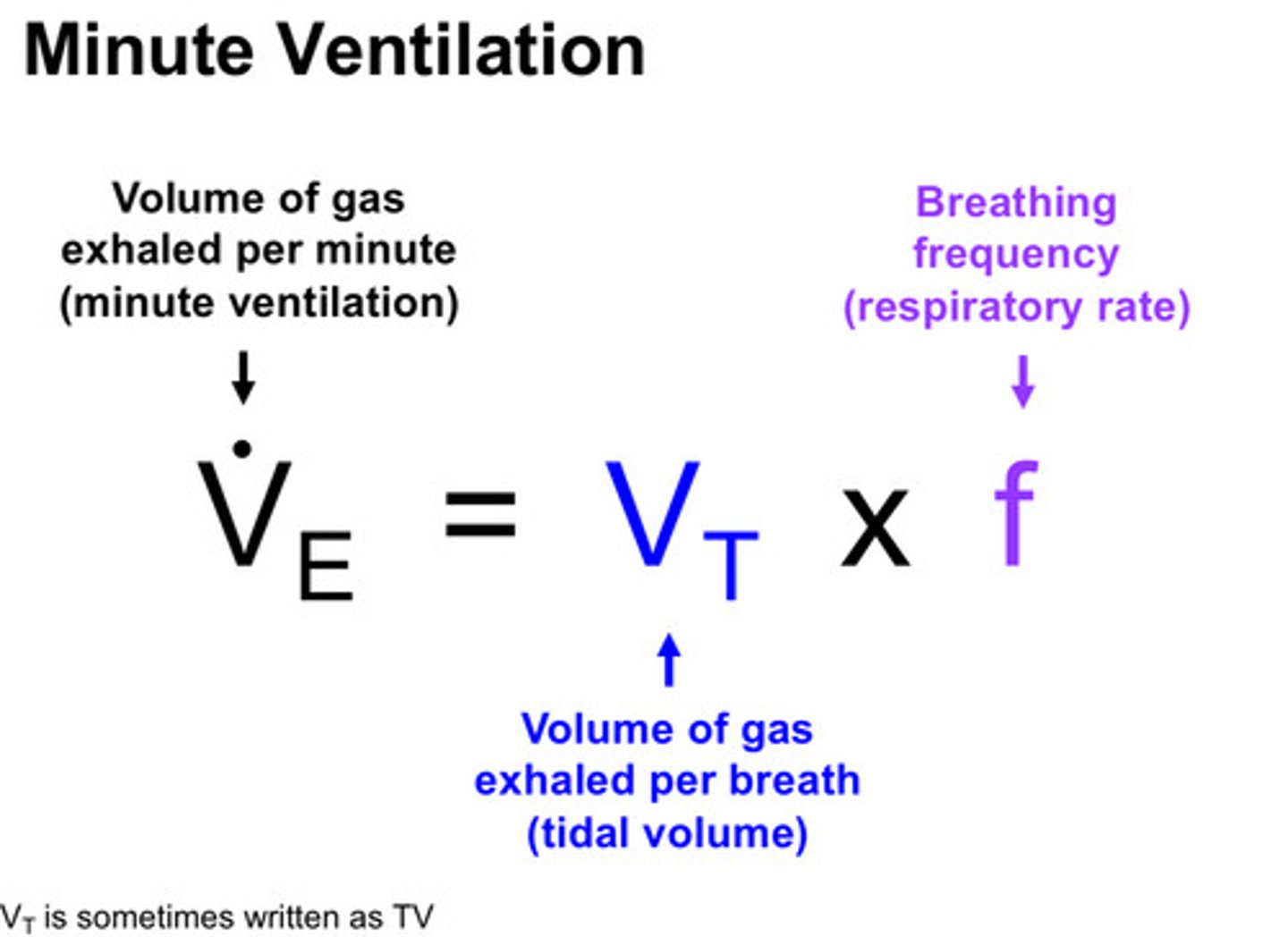
what is minute ventilation
the volume of air exhaled per minute; denoted as V.E (normal resting minute ventilation at sea level is ~5-6 L/min)
describe the bohr effect
1) as blood moves across pulmonary capillary bed, PCO2 is decreasing as the CO2 diffuses across the alveolar capillary barrier and leaves through ventilation
2) as CO2 comes off Hb, the Hb conformation changes in a way that its affinity for O2 increases; loads on more O2
3) out in the tissues, as blood moves across capillaries, PCO2 rises and more CO2 is bound to Hb
4) this changes the conformation of Hb such that it has less affinity for O2 and releases O2 so it can diffuse into the tissues to support metabolic activity
describe the haldane effect
1) as blood moves across pulmonary capillary bed, PO2 rises as oxygen diffuses in from the alveoli —> increases Hb oxygen saturation
2) as conformation of Hb changes, its affinity for CO2 goes down so Hb kicks off the CO2 from the terminal ends of the hemoglobin chains
3) this then frees CO2 to diffuse across the alveolar-capillary barrier
4) out at the tissues, as blood moves through the capillaries, the oxygen is offloaded from Hb; as Hb-O2 saturation goes down, Hb's affinity for CO2 increases —> more likely to pick up the CO2 produced by tissue metabolic activity so it can be transported to lungs

what are the variables that determine the minute ventilation?
1) size of each breath which we call the tidal volume (VT)
2) respiratory rate, or breathing frequency (f)
what is the equation of minute ventilation
VT x f = V.E
tidal volume x respiratory rate = minute ventilation
(you can breathe at a very high RR, but if tidal volumes are very low, then minute ventilation may actually be low and vice versa)
what 6 things can increase minute ventilation
1) anxiety
2) pain
3) hypoxemia
4) pregnancy
5) liver disease
6) metabolic acidosis
what 4 things can decrease minute ventilation
1) opiate pain medications
2) altered mental status (not a universal finding)
3) neuromuscular weakness
4) metabolic alkalosis
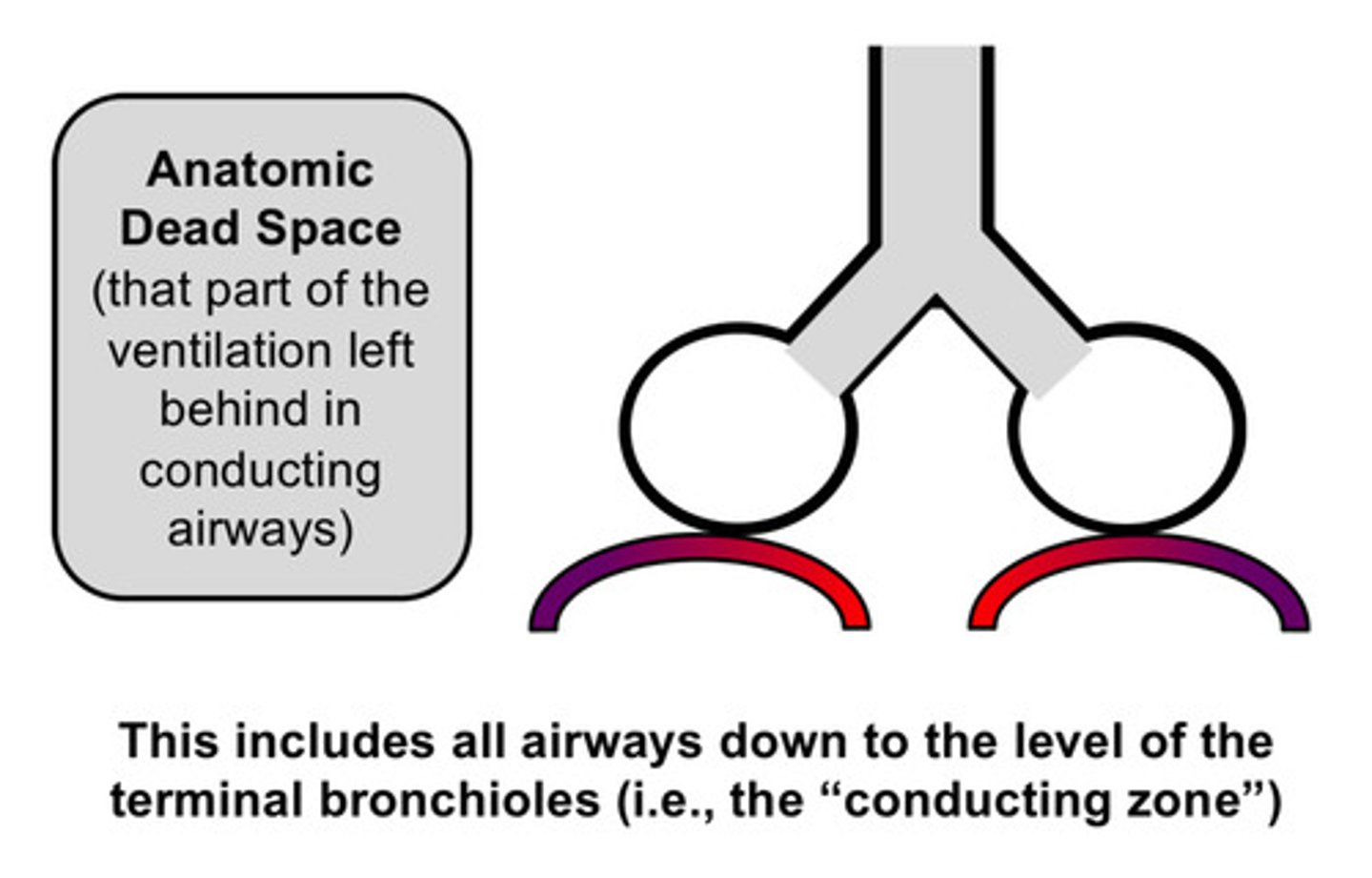
describe what dead space is
at first glance, you might expect all of the minute ventilation to go to the alveoli and be devoted to gas exchange BUT the reality is that not all of the air we inhale participates in gas exchange! instead, some of that air is going to get left behind in what is referred to as the "dead space" and only a portion of it gets down to the alveoli for gas exchange
describe what dead space ventilation is
refers to the areas of the lung that receive ventilation (air flow) but do not receive any perfusion (blood flow)
what is the anatomic dead space
normal and present in all individuals; this refers to the conducting airways where no gas exchange occurs (nasopharynx down to end of terminal bronchioles)
what is the alveolar dead space
areas of the respiratory zone (particularly the alveoli) that receive ventilation but for some PATHOLOGIC reason, do not receive any perfusion (ex: pulmonary embolism)
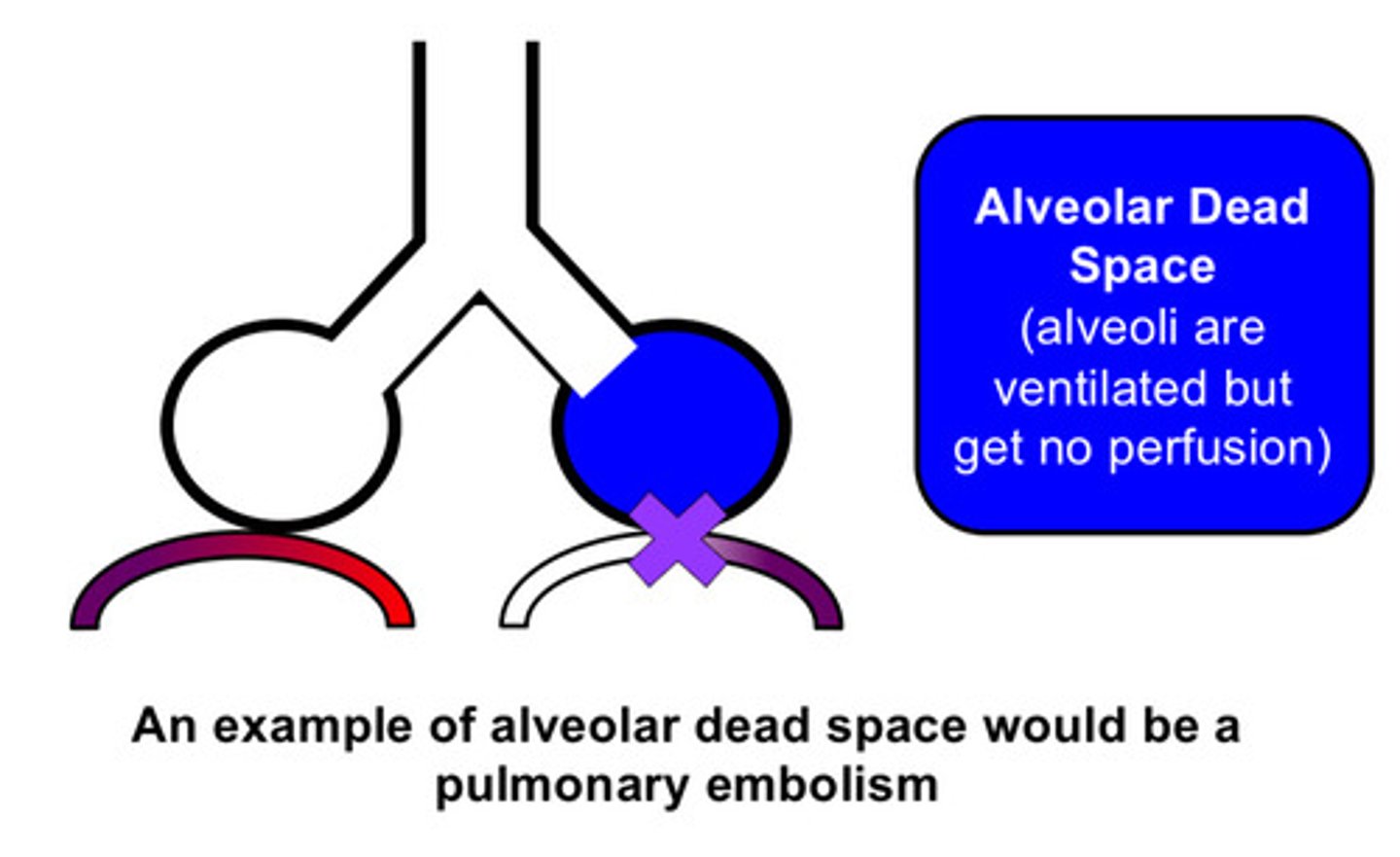
in alveolar dead space, do the alveoli get air into them?
these alveolar units may still get air into them but they do not receive any blood flow
what are the 2 compartments that add up to the minute ventilation
the dead space and the alveoli
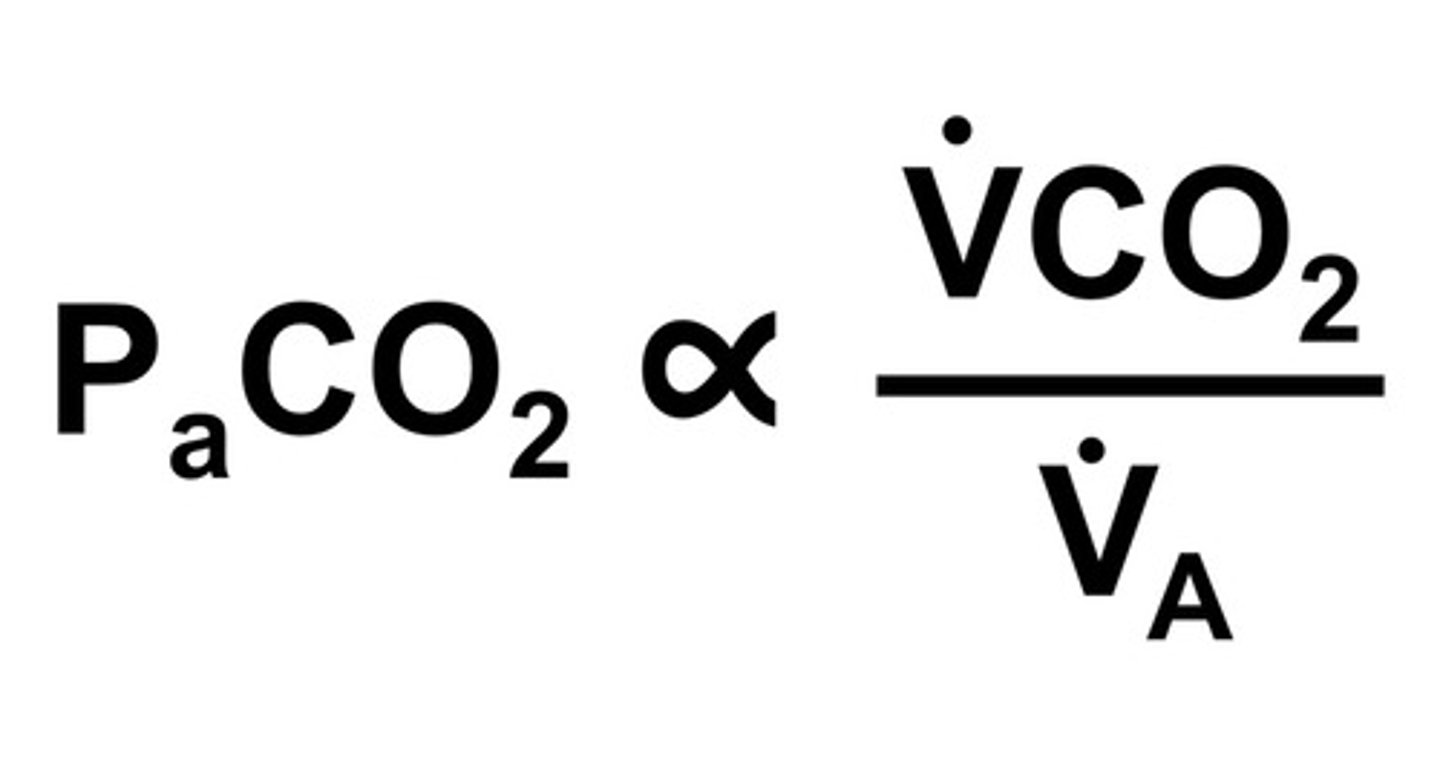
if minute ventilation = alveolar ventilation + dead space ventilation, how can we calculate alveolar ventilation?
simple PEMDAS: alveolar ventilation = minute ventilation - dead space ventilation
1) if dead space ventilation increases, alveolar ventilation decreases
2) if minute ventilation increases, alveolar ventilation increases
case 1: 35 year old person found in bathroom at pike place with empty fentanyl syringe on the ground; pt has a RR of 6 and is taking shallow breaths
can you explain how the PaCO2 would change?
1) pt has low RR and most likely low tidal volumes due to shallow breaths —> these cause a decreased minute ventilation value
2) decreased minute ventilation in the (V.A = V.E - V.D) equation means decreased alveolar ventilation
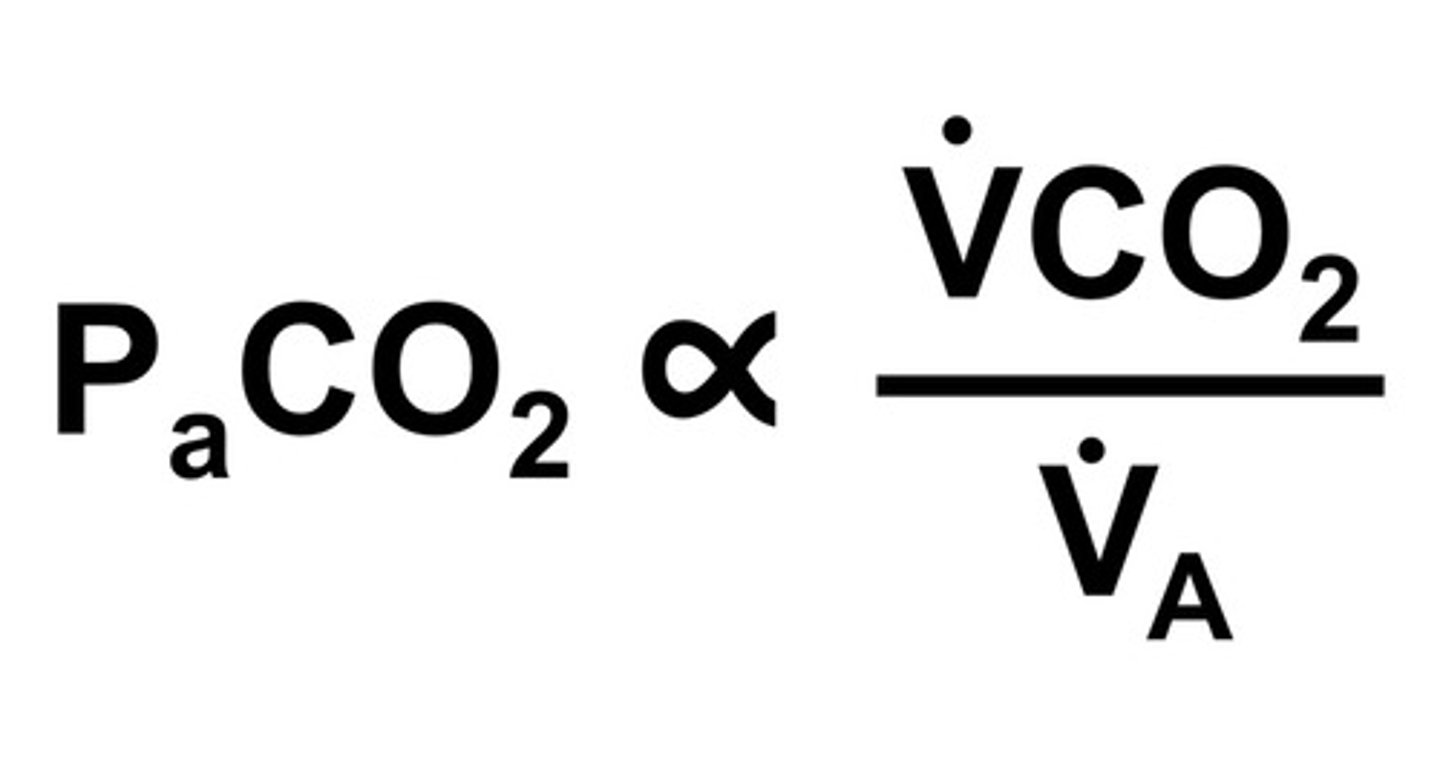
3) we know that PaCO2 is proportional to V.CO2/V.A
4) if V.A is decreased, PaCO2 increases
case 2: 27 year old person comes into ED complaining of chest pain, appearing nervous and diaphoretic and breathing deeply at RR of 20
can you explain how the PaCO2 would change?
1) pt has high RR and most likely high tidal volumes due to deep breaths —> increased V.E
2) increased V.E means increased V.A
3) PaCO2 is proportional to V.CO2/V.A
4) increased V.A means decreased PaCO2
what part of the brain is the center for respiration and is driven by PaCO2 and not by PaO2?
the brainstem (it is the part of the brain that keeps us alive!)
define hypoventilation as it relates to PCO2
hypoventilation refers to a level of alveolar ventilation that is insufficient for metabolic needs. the hallmark of this is an increase in the alveolar and arterial PCO2. if the PaCO2 is high (>45mmHg), the person has, by definition, hypoventilation
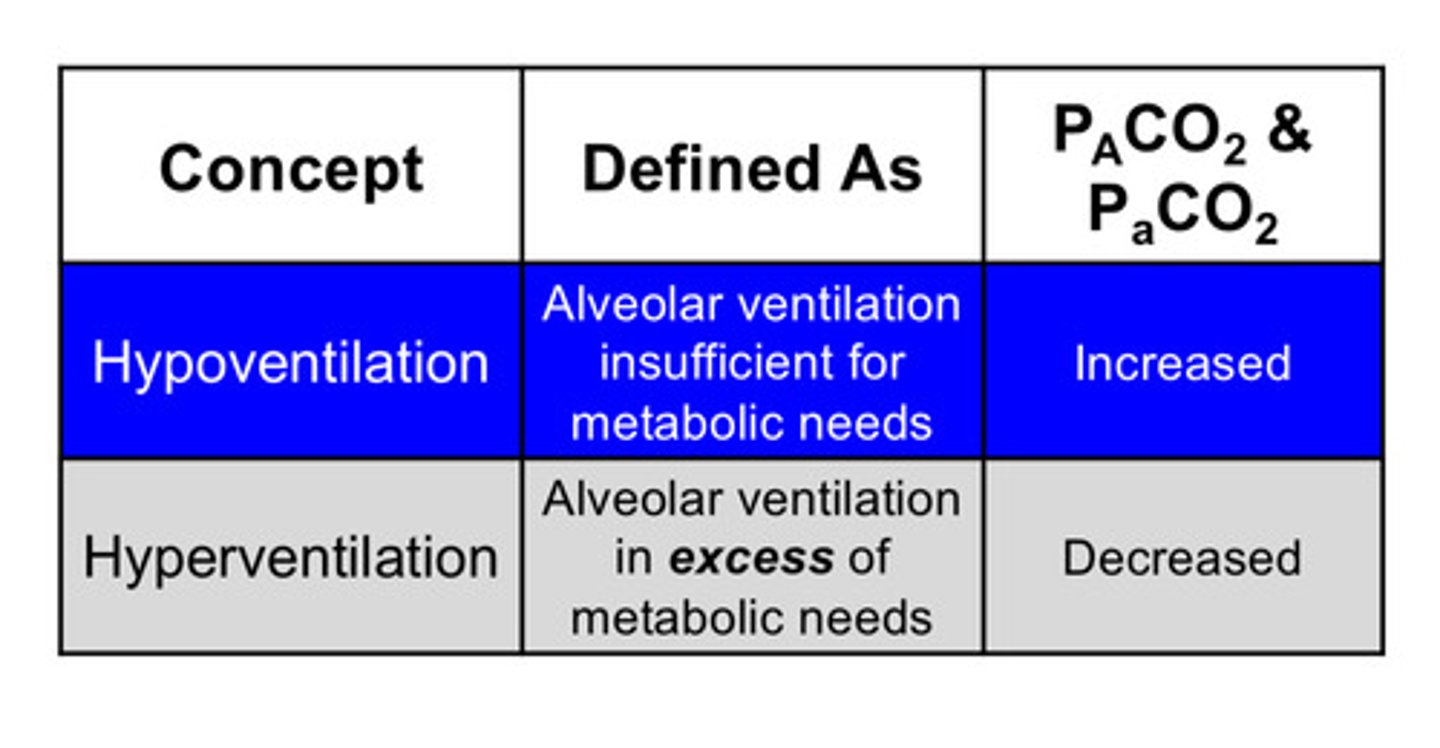
define hyperventilation as it relates to PCO2
hyperventilation refers to alveolar ventilation that is in excess of metabolic needs. the hallmark of this is a low arterial and alveolar PCO2. if PaCO2 is low (<35 mmHg), the person has, by definition, hyperventilation
key points