Approach to patient with Afib
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
What is afib?
Electrophysiological changes in the atrial myocardium result in unsynchronized beating of the heart.
Atria may beat or quiver at a rate of 300 to 400 beats per minute
In atrial fibrillation, for reasons that are unclear, atrial electrical pathways become aberrant and chaotic, and the majority of impulses are unable to pass through the AV node.
If the atria are beating at 400 bpm and only a third of the impulses pass to the ventricles, that can lead to a rapid ventricular rate (RVR) of over 140 bpm, which is unstable and can lead to cardiogenic shock and/or MI
What are complications of Afib?
Embolic stroke from the left atrium that travels up the MCA
Afib w/ RVR can lead to cardiogenic shock and MI
What is the most common diagnosed arrhythmia?
Afib
What are the different classifications of Afib?
Paroxysmal (ie, self-terminating or intermittent) AF – AF that terminates spontaneously or with intervention within seven days of onset. Episodes may recur with variable frequency.
Persistent AF – AF that fails to self-terminate within seven days. Episodes often require pharmacologic or electrical cardioversion to restore sinus rhythm. While a patient who has had persistent AF can have later episodes of paroxysmal AF, AF is generally considered a progressive disease.
Long-standing persistent AF – AF that has lasted for more than 12 months.
Permanent AF – A joint decision by the patient and clinician has been made to no longer pursue a rhythm control strategy. Acceptance of persistent AF may change as symptoms, therapeutic options, and patient and clinician preferences evolve.
While AF typically progresses from paroxysmal to persistent states, patients can present with both types throughout their lives.
What is the clinical presentation of Afib?
Patients with AF may or may not have associated symptoms, and the spectrum of symptoms is broad.
Typical symptoms include palpitations, tachycardia, fatigue, weakness, dizziness, lightheadedness, reduced exercise capacity, increased urination, or mild dyspnea.
More severe symptoms include dyspnea at rest, angina, presyncope, or syncope.
Some patients present with stroke or other systemic embolic event or heart failure
Precipitants of AF may include exercise, emotion, or alcohol.
How is Afib diagnosed?
Clinical exam
EKG
Stroke or embolism that was found to be caused by Afib
What are some causes of Afib?
Electrolyte disturbance (hypokalemia, hypomagnesemia)
Thyrotoxicosis
Drugs (e.g. sympathomimetics—amphetamine, high doses of caffeine, cocaine)
Alcohol
Pulmonary embolus
Pericardial disease
Acid-base disturbance
Pre-excitation syndromes
Cardiomyopathies: dilated, hypertrophic.
Pheochromocytoma
Sick Sinus Syndrome
What are some PE findings with Afib?
Irregularly irregular pulse
No S4
No JV A waves
Apical and radial pulse mismatch
Variation in BP
What would you see on EKG with Afib?
Electrocardiogram — There are no discrete P waves but rapid, low-amplitude, continuously varying fibrillatory (f) waves are seen. The ventricular rhythm is generally irregularly irregular (lacking a repetitive pattern), although AF is uncommonly associated with a regular ventricular rate.
There are a number of potential pitfalls in the ECG diagnosis of AF. Errors in the diagnosis of AF are especially common with computerized ECG interpretation and in patients who are continuously or intermittently paced. It is important that the automated ECG interpretation provided by the machine is confirmed by a skilled reader.
What is additional testing that can be done for AFib?
Stress Test — A stress test is reasonable for patients with signs or symptoms of ischemic heart disease In addition, stress testing may be helpful in gauging adequacy of heart rate control in AF during exercise.
Ambulatory cardiac monitoring-- event recorders, adhesive extended time event monitors, or insertable cardiac monitors (also sometimes referred to as implantable cardiac monitor or implantable loop recorder) can be used to identify the arrhythmia if it is intermittent and not captured on routine ECG. Twenty-four- to 48-hour Holter monitoring can also be used.
Baseline laboratory testing — Clinical or subclinical hyperthyroidism is present in almost 5 percent of patients with AF. A thyroid-stimulating hormone and free T4 levels should be obtained in all patients with a first episode of AF, or in those who develop an increase in AF. Other important baseline tests include a complete blood count, a serum creatinine, and a test for diabetes mellitus
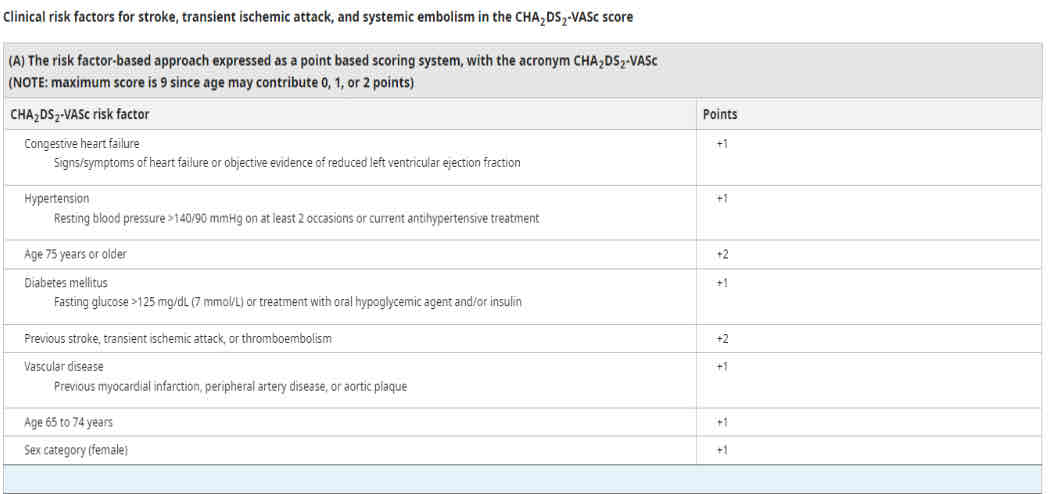
What is the CHADSVASC score?
What are the most common underlying chronic disorders associated with Afib?
HTN (most common), CAD, and CHD
What are risk factors for Afib?
HF, hypertrophic cardiomyopathy, valvular disease (MS, MR, TR), RHD, CongHD, Venous thromboembolic disease, OSA, obesity, DM, metabolic syndrome
What is the approach to treating Afib?
Anticoagulant
Better symptom management
CV and Comorbid risk assessment
What is the most important management considerations with Afib?
Prevention of stroke
What should be involved with symptom management of Afib?
Rate control, then rhythm, then treating comorbid factors or underlying disease (treat this first if it’s causing the Afib)
What are the steps to management of Afib?
Diagnosis of atrial fibrillation
Assessment of duration
Assessment for anticoagulation
Rate or rhythm control and is cardioversion indicated?
Treatment of underlying / associated diseases
What are the two acute methods to treating Afib?
Acute control of the heart rate, usually with a beta blocker (cardioselective like carvedilol or metoprolol) or calcium channel blocker (verapamil or diltiazem).
Unless AF reverts spontaneously, a decision is made whether, when, and how cardioversion will be performed. Management of thromboembolic risk is a key consideration when cardioversion is considered.
For patients with AF with acute hypotension caused by AF with rapid ventricular response, electrical cardioversion is required if there is no quick response to medications!
What are some examples of rate control medications for Afib?
B-Blockers for RATE control are used most commonly. Generally, cardiac medications for rhythm control are not used unless the patient’s HR is persistently above 100 bpm.
Metoprolol
Nebivolol
Bisoprolol
Atenolol
Betaxolol (this is also in optic drops for glaucoma or ocular hypertension)
Carvedilol
Nadolol
Timolol (also used in optic drops for glaucoma or ocular hypertension)
Calcium channel blockers. These medications have multiple effects on the heart. They are used to slow the heart rate in patients with Afib. Examples of calcium channel blockers include:
Diltiazem
Verapamil
Digoxin. This medication slows the rate at which electrical currents are conducted from the atria to the ventricle. (Not used often because of the risk of digoxin toxicity, but is used to help manage the patient with long-standing atrial fibrillation who also has heart failure, who is usually of advanced age.)
What are examples of anticoagulants used in Afib?
Anticoagulants used for atrial fibrillation are apixaban (Eliquis), edoxaban (Lixiana), rivaroxaban (Xarelto), dabigatran (Pradaxa), and warfarin.
What are some examples of medications used for rhythm control of Afib?
Sodium channel blockers help the heart's rhythm by slowing its ability to conduct electricity. Examples may include:
Flecainide (Tambocor)
Propafenone (Rythmol)
Quinidine (Various)
Potassium channel blockers help the heart’s rhythm by slowing down the electrical signals that cause AFib. Examples may include:
Amiodarone (Cordarone or Pacerone)
Sotalol (Betapace)
Dofetilide
Dronedarone (Multaq)
If you have an unstable patient presenting with Afib what should you do? ( low bp, low pulse ox, high hr, not responsive) And what is this patient at risk of going into?
Cardioversion and Cardiogenic Shock
What is crossover therapy with Afib?
Give low molecular weight heparin injections (such as enoxaparin or fondaparinux) combined with warfarin, until the PT/INR reaches 2.0. Then the low molecular weight heparin is discontinued and the dose of warfarin is adjusted. This is called crossover therapy.
What is PIRATES in regard to underlying Afib?
P-pulmonary causes (PE, OSA, COPD, Pneumonia)
I-ischemia/cardiac infarction/hypertension
R-rheumatic heart disease (i.e., valvular disease)
A-alcohol/anemia
T-thyrotoxicosis/toxins (i.e., amphetamines, stimulants)
E-electrolyte imbalance/endocarditis
S-Sepsis