Complex Exam II
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
Serum creatinine levels
Males: 0.6-1.2
Females: 0.5-1.1
Higher creatinine levels = higher kidney damage
Blood urea nitrogen
blood test that measures the amount of urea in the blood; should be 10-20 mg/dl
AKI
Over 50% increase in serum creatinine; can be prerenal (hypoperfusion), intrarenal (physical injury such as trauma), or postrenal (obstruction of urine flow)
Acute tubular necrosis
damage to the renal tubules due to presence of toxins in the urine or to ischemia
caused by sepsis, prolonged hypotension, rhabdomyolysis
s/s: oliguria, anuria, brown urine, swelling, coma/delirium/drowsiness/confusion
dx: serum BUN and creatinine, UA, kidney biopsy
tx: treat cause, prevent fluid vol. overload and hyperkalemia
mx: fluid restriction, strict Is and Os, daily labs
normal urinary output
1000 to 2000 mL per 24 hours OR 30 ml/hr
AKI clinical manifestations
Oliguria or anuria; edema in legs/ankles/feet, fatigue, SOB, HTN, confusion, nausea, flank pain, chest pain, seizures
AKI nutrition
No more than 500-600 mL over the previous day's 24 hr UOP. Limit potassium and sodium.
AKI interventions
Avoid nephrotoxic meds, avoid hyperkalemia (kayexalate, insulin), avoid hyperphosphatemia, avoid severe metabolic acidosis, admin. diuretics
Most common causes of kidney disorders
Uncontrolled diabetes (high glucose levels damage glomeruli), uncontrolled HTN (causes hardening of renal arteries), heart disease/atherosclerosis (decreased blood flow to kidneys), obesity, smoking
Primary glomerular disease
Non-systemic damage and inflammation within the kidneys
Nephrotic syndrome
Proteinuria; increased glomerular permeability leads to protein leakage (will have low serum albumin and low serum protein)
dx: blood work for albumin, sCr/BUN/GFR, UA
mx: strict Is and Os (watch for oliguria), control BP through diuretics, ACEis etc., anticoagulant therapy since body's anticoags are dumped out into urine
Nephritic syndrome
Hematuria; inflammation of the glomeruli causes bleeding (will have high BP, oliguria, azotemia and edema)
dx: BMP (sCr will increase quickly), UA
tx: diuretics, ACEis, fluid and Na+ restrictions, abx if needed for underlying infection
Glomerulonephritis
Immune system attacks kidneys and injures glomeruli.
HAD STREP: HTN, a positive strep titer, decreased GFR, swelling in face/eyes, tea colored urine, recent strep infection, elevated BUN and sCr, proteinuria (mild)
dx: UA, CMP
mx: daily weights, watch for fluid overload
Chronic glomerulonephritis
condition in which the glomeruli suffer gradual, progressive, destructive changes, with resulting loss of kidney function; also called chronic nephritis. caused by repeat acute glomerulonephritis, HTN-related nephrosclerosis, hyperlipidemia. will have hyperkalemia, metabolic acidosis, hypoalbuminemia, anemia.
dx: UA/CMP/CBC, kidney US
mx: daily weights, high protein diet
polycystic kidney disease (PKD)
multiple fluid-filled sacs (cysts) within and on the kidney; will have hematuria, polyuria, and proteinuria; as well as HTN, renal calculi, flank pain, UTI, palpable cysts on exam
mx: no available tx so supportive mx with BP control, kidney transplant
CKD staging
G1: GFR > 90
G2: GFR = 60-89
G3a: GFR = 45-59
G3b: GFR = 30-44
G4: GFR = 15-29
G5: GFR < 15
CKD nutrition
low sodium (2-3 g a day)
low fluids
low phosphorus
increase protein only of 1.-1.5g per day when on dialysis
regulatory mechanisms in shock
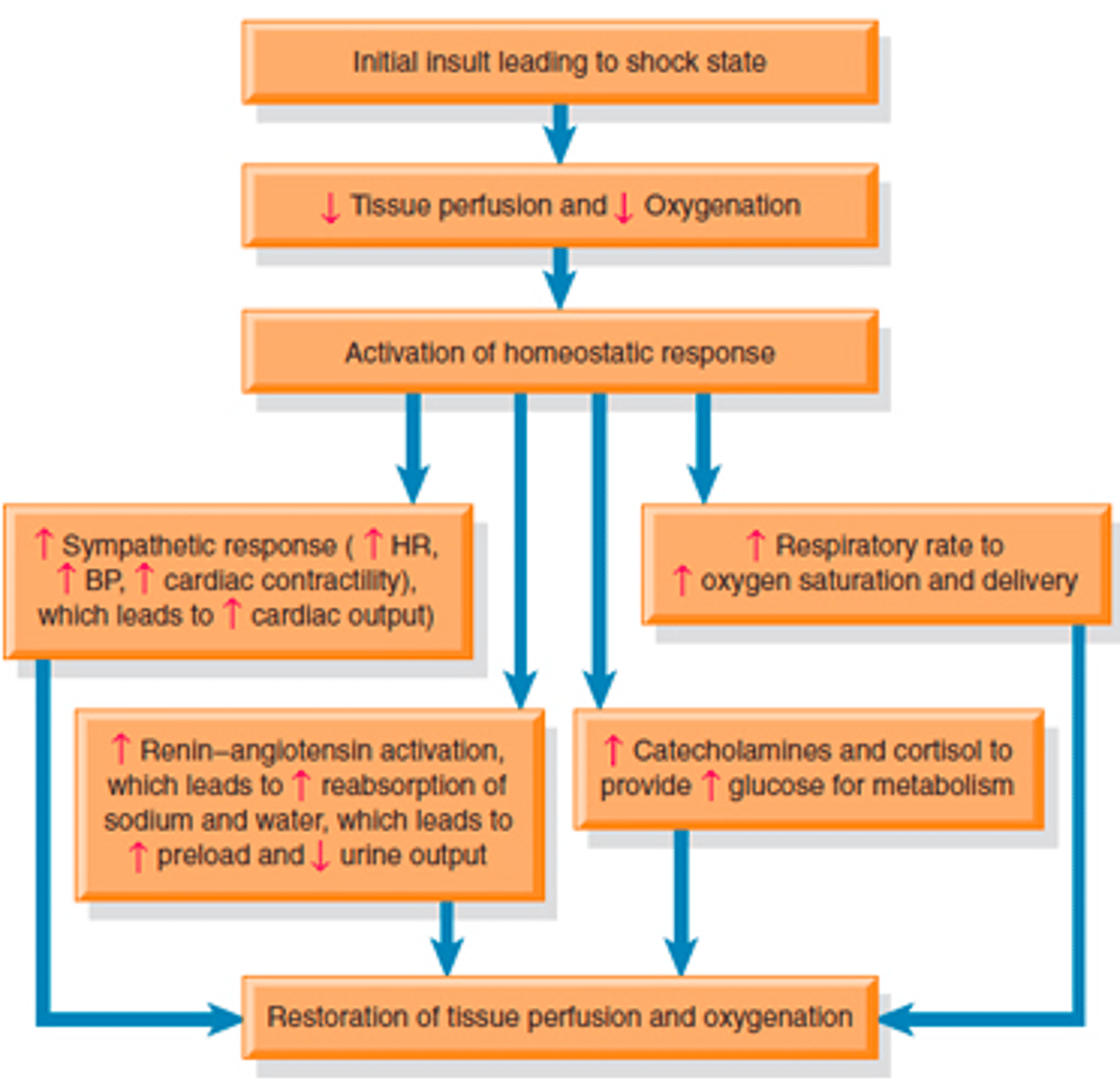
pathophysiology of shock
cells switch to anaerobic metabolism, creating lactic acid; cell function ceases and swells and membranes become more permeable, with electrolytes seeping out of cells. na/k pump and mitochondria fail and cell death and lysis begins to occur.
stages of shock
Initial insult
Compensatory
Progressive
Irreversible
progressive stage of shock
when compensatory mechanisms fail and organ functions begin to deteriorate
clinical manifestations of shock (compensatory)
Tachypnea, tachycardia, diaphoresis, cool or clammy skin, decreased UOP, increased serum glucose, hypoactive bowel sounds, decreased PaCO2
clinical manifestations of shock (progressive)
hypotension (late sign), pulmonary edema w/ crackles, multiple organ dysfunction syndrome (MODS), altered mental status, AKI (oliguria, anuria), GI ischemia (bloody diarrhea, ulcers), abnormal hemostasis (increased clotting times, bruises, petechiae), tachycardia/tachypnea
multiple organ dysfunction score
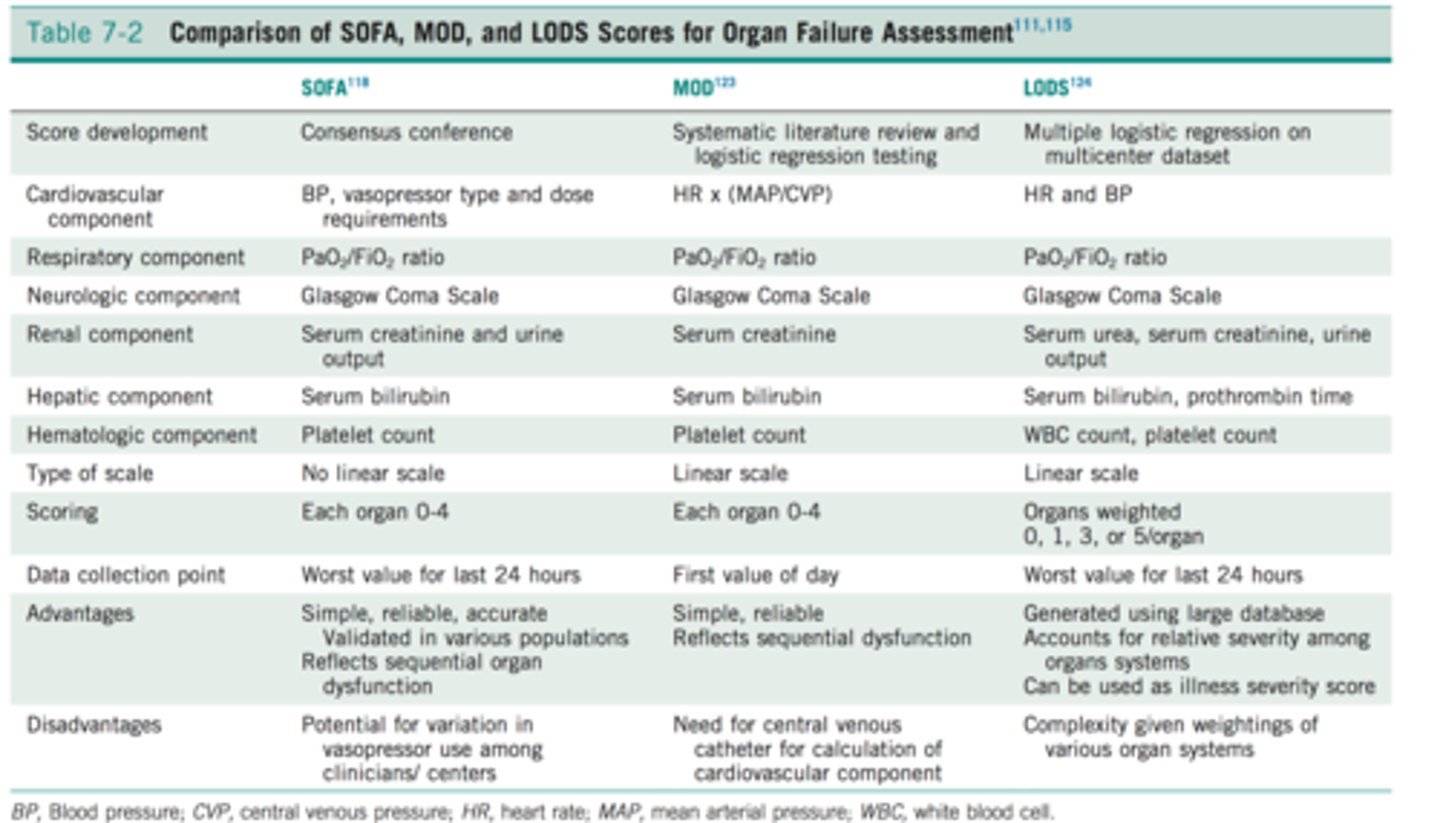
signs of MODS
respiratory P/F ratio <250 w/o pneumonia, or <200 w/ pneumonia (PaO2 to FiO2 ratio)
MAP <65 mmHg; SBP <90 or SBP decreases >40 from baseline
creatinine > 2 mg/dl
urine output <0.5 mL/kg/hr in 6 hours or <400 mL in 24 hours
bilirubin > 2 mg/dl
platelets <100,000/mm3
INR > 1.5 or aPTT > 60 secs
lactate > 2 mmol/L
clinical manifestations of shock (irreversible)
significantly diminished cardiac output, pale/cyanotic/yellowish skin, anuria, disseminated intravascular coagulation (widespread clot formation, clotting factors get used up and patient develops uncontrollable bleeding)
hypovolemic shock: causes
blood loss, dehydration, burns, diarrhea/vomiting, diabetes insipidus, diuresis (such as hemodialysis)
hypovolemic shock: clinical manifestations
poor skin turgor, thirst, oliguria, low systemic and pulmonary preloads, rapid heart rates
hypovolemic shock: management
Find the source and stop it!
Replace lost intravascular volume
Redistribute fluid volume
hypovolemic shock: tx
surgical intervention to control bleeding, IV fluid resuscitation (isotonic), blood transfusion (usually if Hgb < 7 g/dL)
1 unit of PRBCs should raise Hgb by what?
1 g/dL
cardiogenic shock: causes
MI (most common), HF, dysrhythmias, CAD, cardiomegaly, myocarditis, valvular disorders, drug toxicity
cardiogenic shock: clinical manifestations
crackles in lungs, chest pain, weak and thready pulses, hypoxemia, fatigue, diaphoresis
cardiogenic shock: management
restore tissue perfusion, improve cardiac contractility, manage other organ dysfunction
cardiogenic shock: tx
Thrombolytics, PCI, stents; meds (dysrhythmias, electrolyte imbalance correction), mechanical assistive devices (IABP, impella, LVAD); use fluids with extreme caution. major purpose of tx is to correct underlying cause
obstructive shock: causes
pneumothorax, cardiac tamponade, PE, aortic dissection, pulmonary hypertension, restrictive cardiomyopathy
obstructive shock: clinical manifestations
chest or abd. pain, distended jugular veins, muffled heart sounds (in cardiac tamponade), unequal peripheral pulses (in aortic dissection)
obstructive shock: management
remove the obstruction
obstructive shock: tx
Fibrinolytics and DOACs (for PE)
Surgical intervention (for PE, tumors, aortic dissection, or
splenic sequestration)
Needle decompression/chest tube (for pneumothorax)
Pericardiocentesis (for cardiac tamponade)
Medications (HTN meds for restricted cardiomyopathy or PH)
Use fluids with extreme caution
distributive shock: causes
anaphylaxis, sepsis, spinal cord injury
distributive shock: clinical manifestations
warm or flushed skin due to widespread vasodilation (blood sits in blood vessels for longer than normal), other systems dependent on type of distributive shock
distributive shock: management
main goals are restoring sympathetic tone, reversing cause, supporting BP/pulse/respirations
distributive shock: tx
if neurogenic: spinal stabilization or surgery; atropine for parasympathetic induced bradycardia, DVT/VTE prophylaxis; if anaphylactic: IM epinephrine
distributive shock: neurogenic
interruption of sympathetic nervous system impulse transmission caused by injury to brain or spine; causes include meningitis, spinal anesthesia, stroke
*parasympathetic nervous system takes over, promoting bradycardia and worsening cardiac output
distributive shock: anaphylactic
major release of histamine leads to widespread hypotension and vasodilation
distributive shock: septic
an infection causes an exaggerated inflammatory response by the body, causing widespread vasodilation, hypotension, and organ damage
general treatment for shock
early identification (ABCs, vitals, lab trends, subtle changes including LOC, UOP, skin tone, cap refill), establishing adequate tissue perfusion (restoring intravascular volume and vasomotor tone to increase CO, adequate oxygenation), restoring normal cell function (restore acid-base balance, provide nutritional support, prevent GI injury), monitor labs (lactate levels, ABGs, signs of MODS, CMP, CBC), monitor BP and MAP, provide psychosocial support and advanced supportive care prn (ventilation, dialysis, etc.)
general fluid replacement for shock
fluid challenge (one time): 500-1000 mL bolus of isotonic fluids
aggressive fluid resuscitation (long-term): 30 mL/kg using ideal body weight of isotonic fluids
fluids used include lactated ringer's, 0.9% NS
complications of fluid replacement
if insufficient: higher incidence of morbidity and mortality due to lack of tissue perfusion
if excessive: higher incidence of morbidity/mortality due to multiple side effects, including acute lung injury, abd. compartment syndrome, MODS, hypothermia, acidosis
nutritional therapy for shock
caloric intake starts low and then increases, protein starts high and then decreases.
Narrow pulse pressures can be an indicator of shock from ______________ ______ or _______________ ________
decreased CO, increased SVR (systolic vascular resistance
MAP formula
(SBP + 2DBP)/3; normal range 70-100 mmHg
ScvO2 normal range
70-80%
PaCO2 normal range
35-45 mmHg
CVP (central venous pressure) normal range and significance
8-12 mmHg; used to estimate right atrial pressure and overall fluid status
PAP (pulmonary artery pressure) normal range and significance
12-20 mmHg mPAP; used to estimate right ventricular function and assess for pulmonary HTN
PAWP (pulmonary artery wedge pressure) normal range and significance
6-12 mmHg mPAWP; used to estimate left atrial pressure. low in hypovolemic and distributive shock, and can be either high or low in obstructive shock depending on cause
Systemic inflammatory response syndrome (SIRS)
a syndrome resulting from a clinical insult that initiates an inflammatory response that is systemic, rather than localized to the site of the insult
SIRS criteria
2 or more of the criteria must be met:
HR greater than 90
RR greater than 20
Temp greater than 100.9 or less than 96.8
WBC greater than 12,000/mm3 or less than 4000/mm3 or > 10% bands
glucose greater than 140 mg/dl in absence of diabetes
______________ levels are used to guide sepsis resuscitation efforts.
lactate
Sepsis 1 hour bundle
1. Measure lactate level. Remeasure if initial lactate elevated (>2).
2. Obtain blood cultures x2 prior to administering antibiotics.
3. Begin rapid administration of 30ml/kg crystalloid.
4. Administer broad spectrum antibiotics.
5. Administer vasopressors if needed.
persistent hypotension and vasopressor indications
B/P is measured every 15 minutes post-fluids. Two consecutive low B/P readings indicates persistent hypotension, and vasopressors should be started without delay.
Additional sepsis medications
volume expanders (albumin) to increase intravascular volume and improve BP; corticosteroids (hydrocortisone) to reduce inflammatory response and limit vasodilation; PPIs (pantoprazole) to protect the gut from stress ulcers or bleeding; antipyretics, insulin, etc.