Understanding Ultrasound in Therapeutic Applications
1/131
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
132 Terms
Ultrasound
Sound waves transmitting energy via compression and rarefaction.
Sound Frequency
Greater than 20,000 Hz, inaudible to humans.
Normal Hearing Range
Human audible sound frequency: 16 to 20,000 Hz.
Thermal Effects
Increase in tissue temperature due to ultrasound.
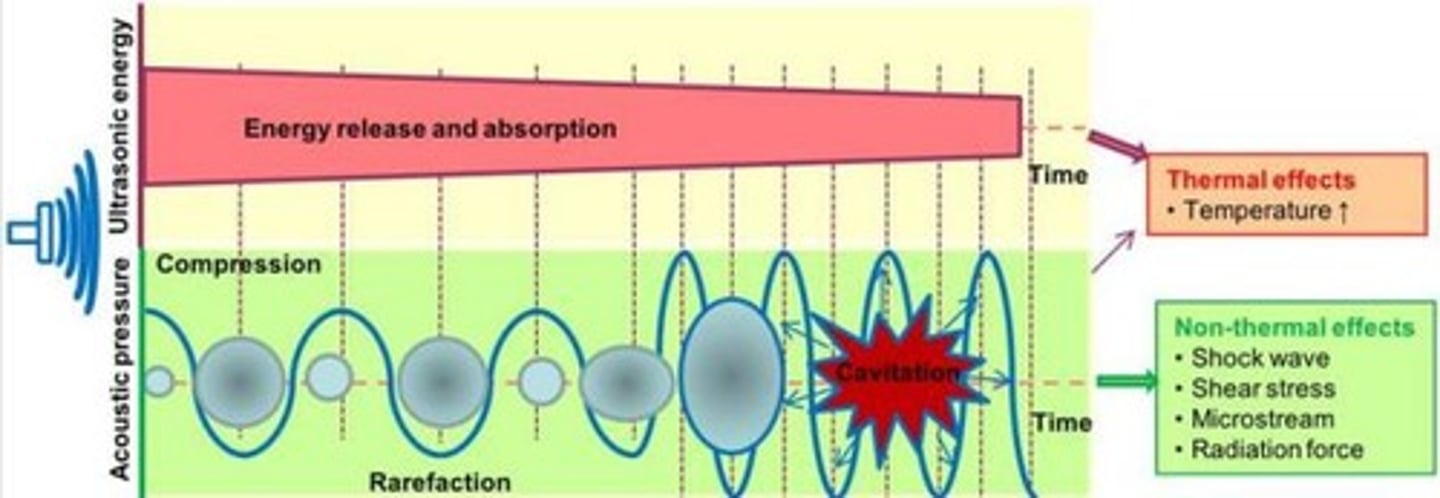
Nonthermal Effects
Include acoustic streaming, microstreaming, and cavitation.
Acoustic Streaming
Steady circular flow of cellular fluids induced by ultrasound.
Microstreaming
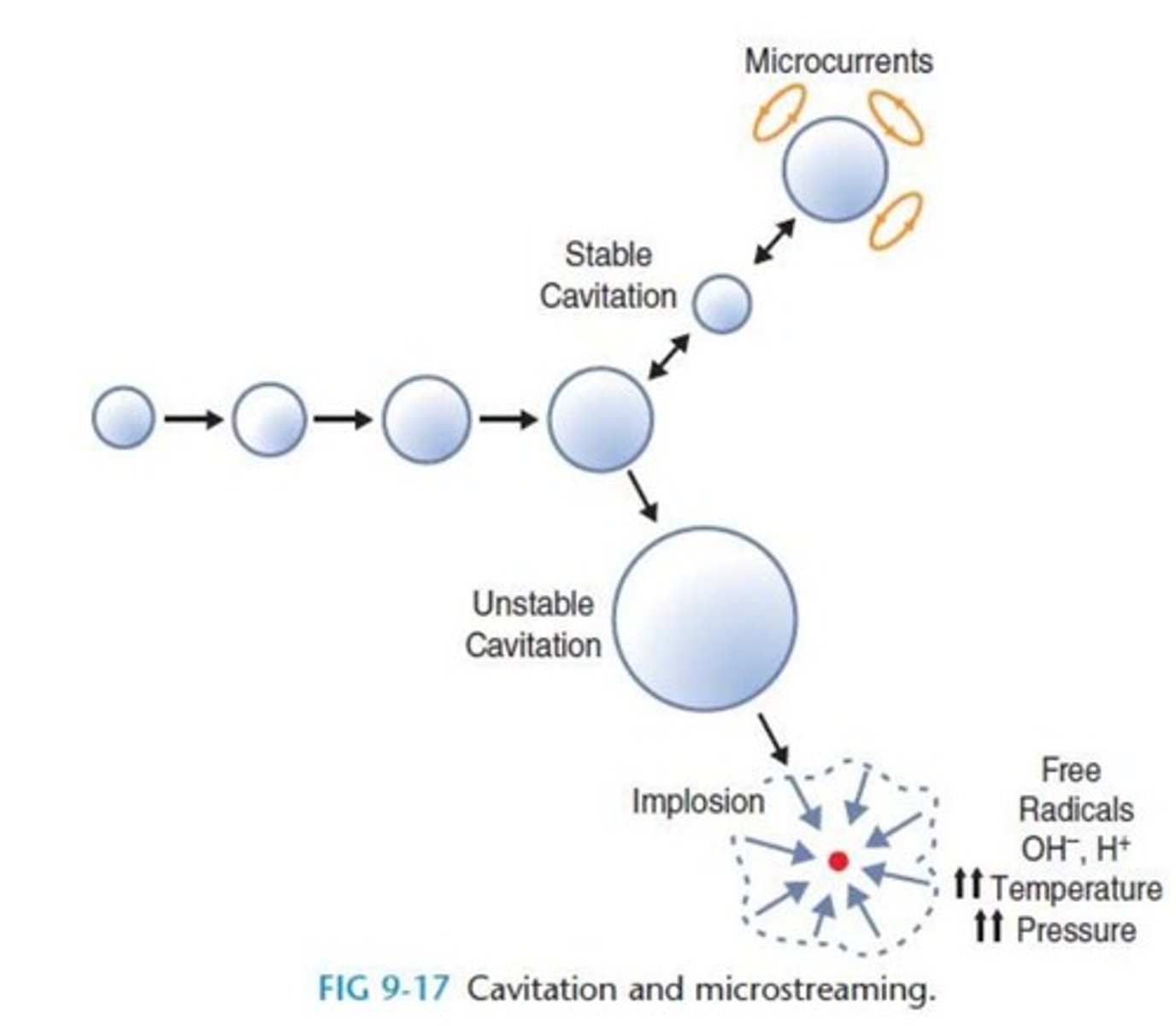
Microscale eddying near vibrating objects in ultrasound.
Cavitation
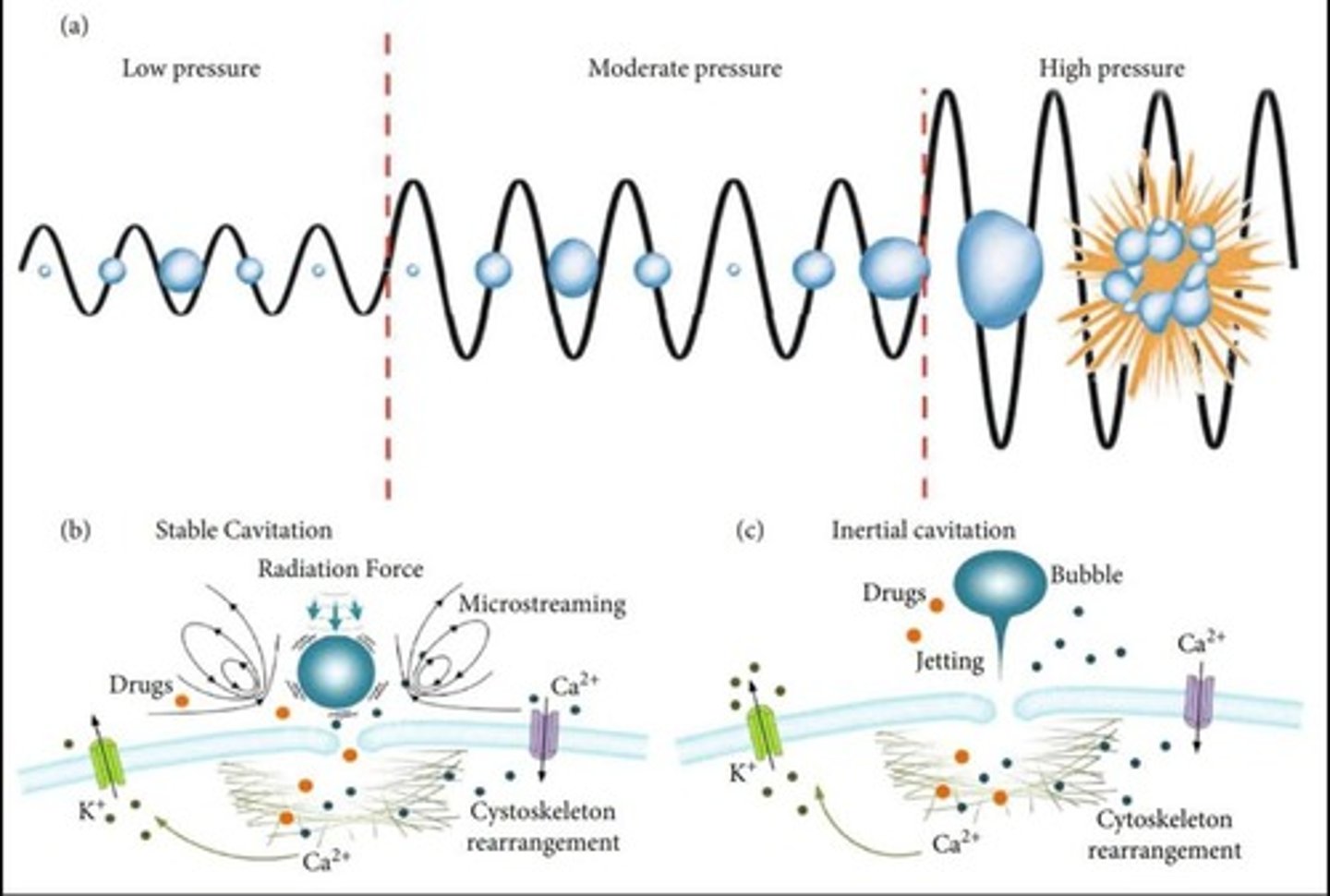
Formation and pulsation of gas bubbles caused by ultrasound.
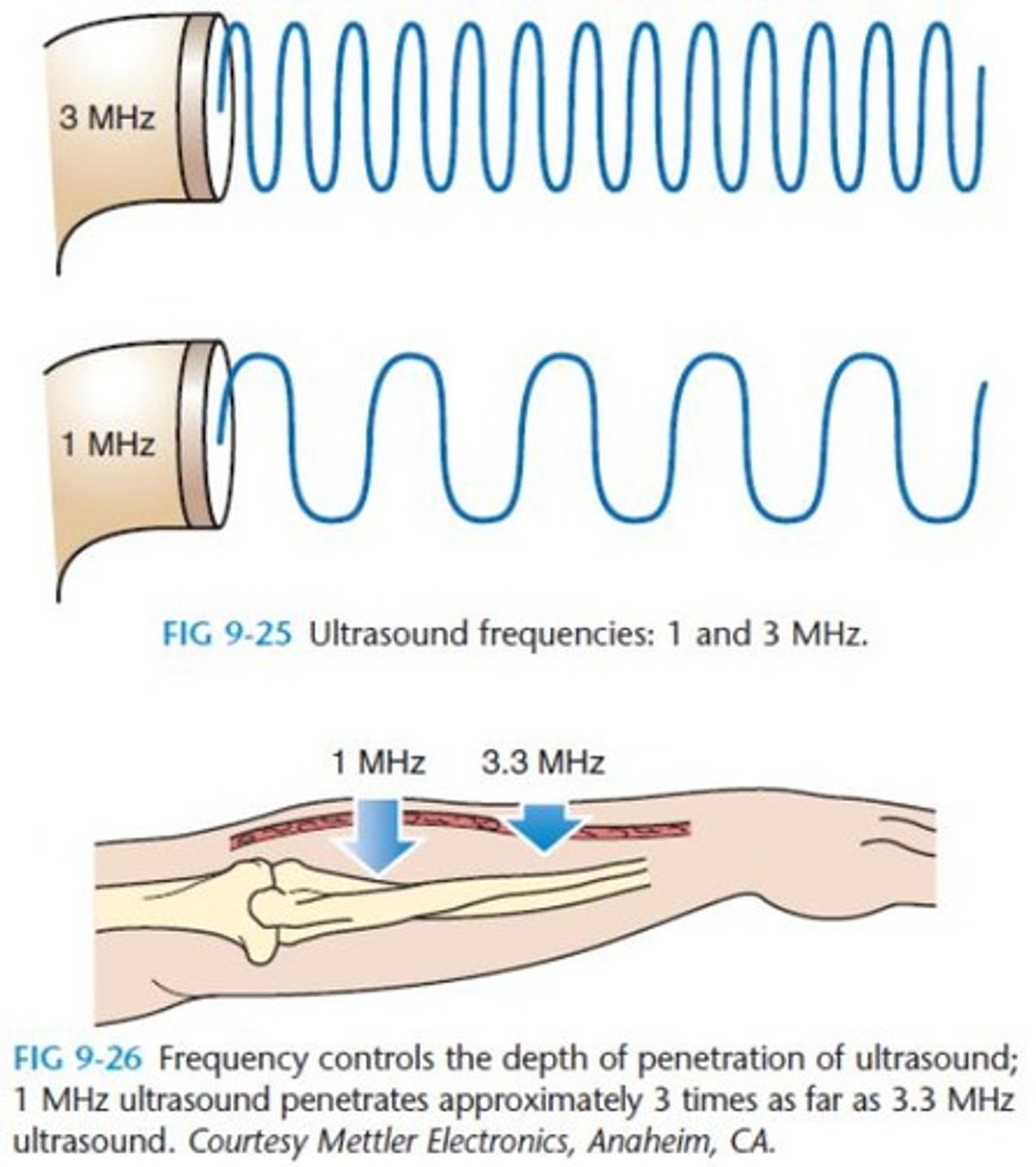
Therapeutic Ultrasound Frequency
Ranges from 0.7 to 3.3 megahertz (mHz).
Energy Absorption Depth
Maximized at 2-5 cm in soft tissue.
Attenuation
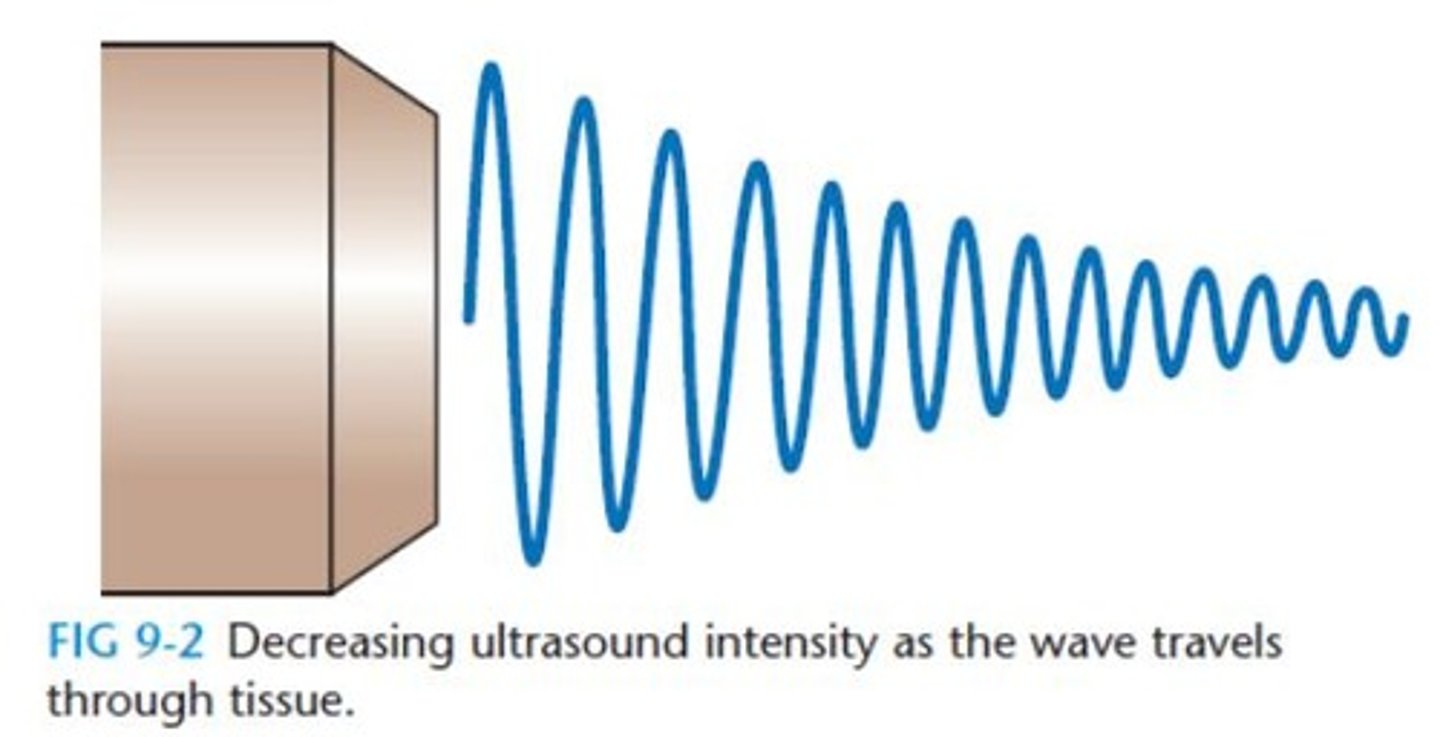
Decrease in ultrasound intensity as it travels through tissue.
Effective Radiating Area (ERA)
Area from which ultrasound energy radiates.
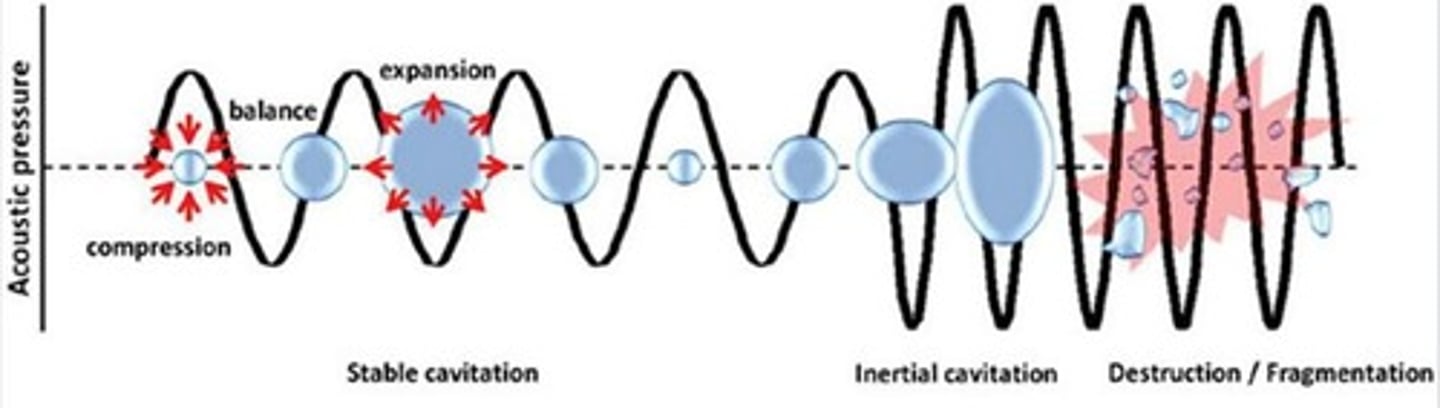
Stable Cavitation
Bubbles oscillate without bursting during ultrasound cycles.
Unstable Cavitation
Bubbles grow and implode, causing pressure and temperature spikes.
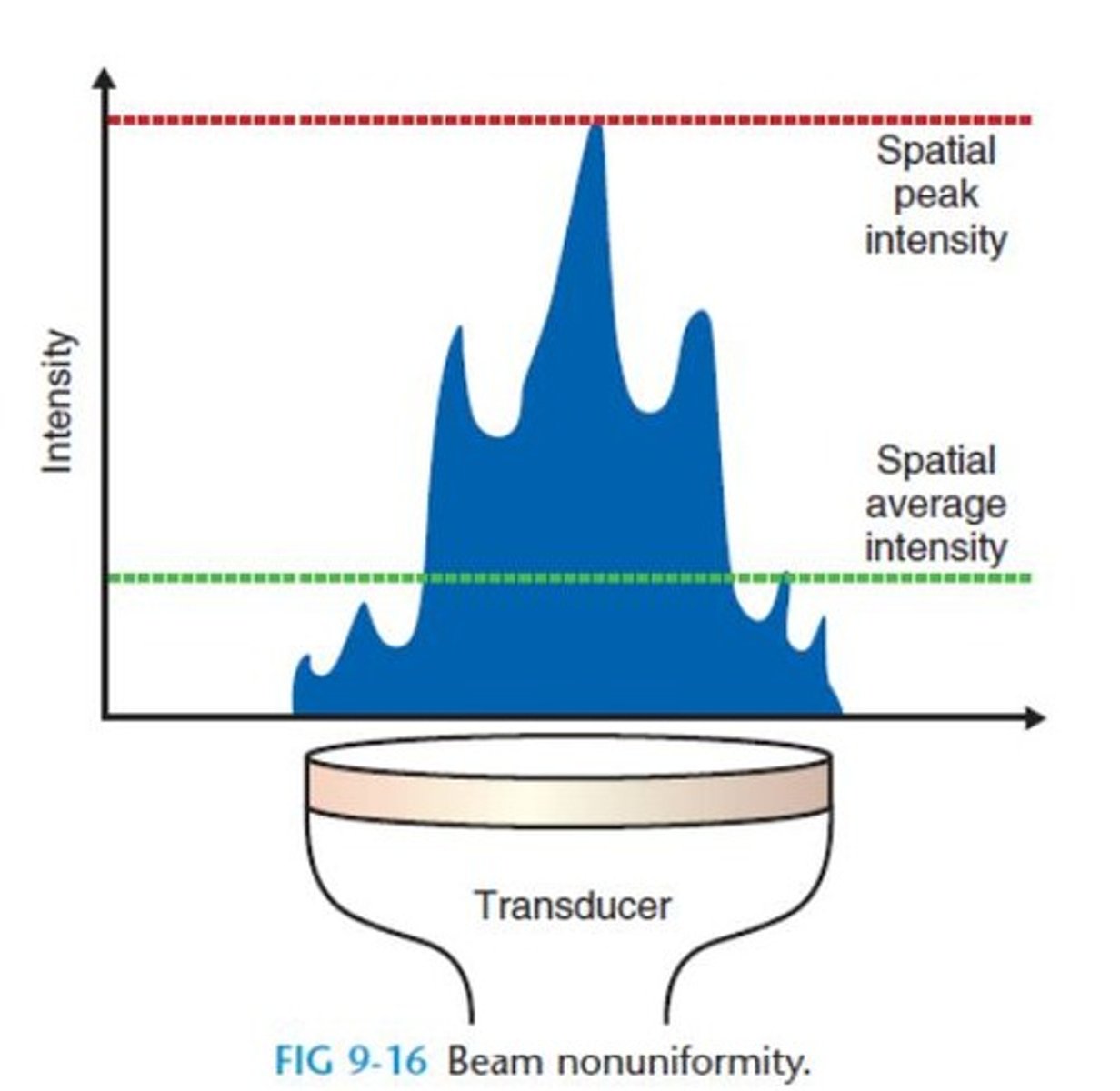
Beam Nonuniformity Ratio (BNR)
Ratio of spatial peak intensity to spatial average intensity.
Typical BNR Values
Usually between 5:1 and 6:1 for ultrasound units.
FDA BNR Requirement
Maximum BNR must be specified on ultrasound devices.
Intensity
Power per unit area of ultrasound, measured in W/cm².
Duty Cycle
Ratio of on-time to total time in ultrasound application.
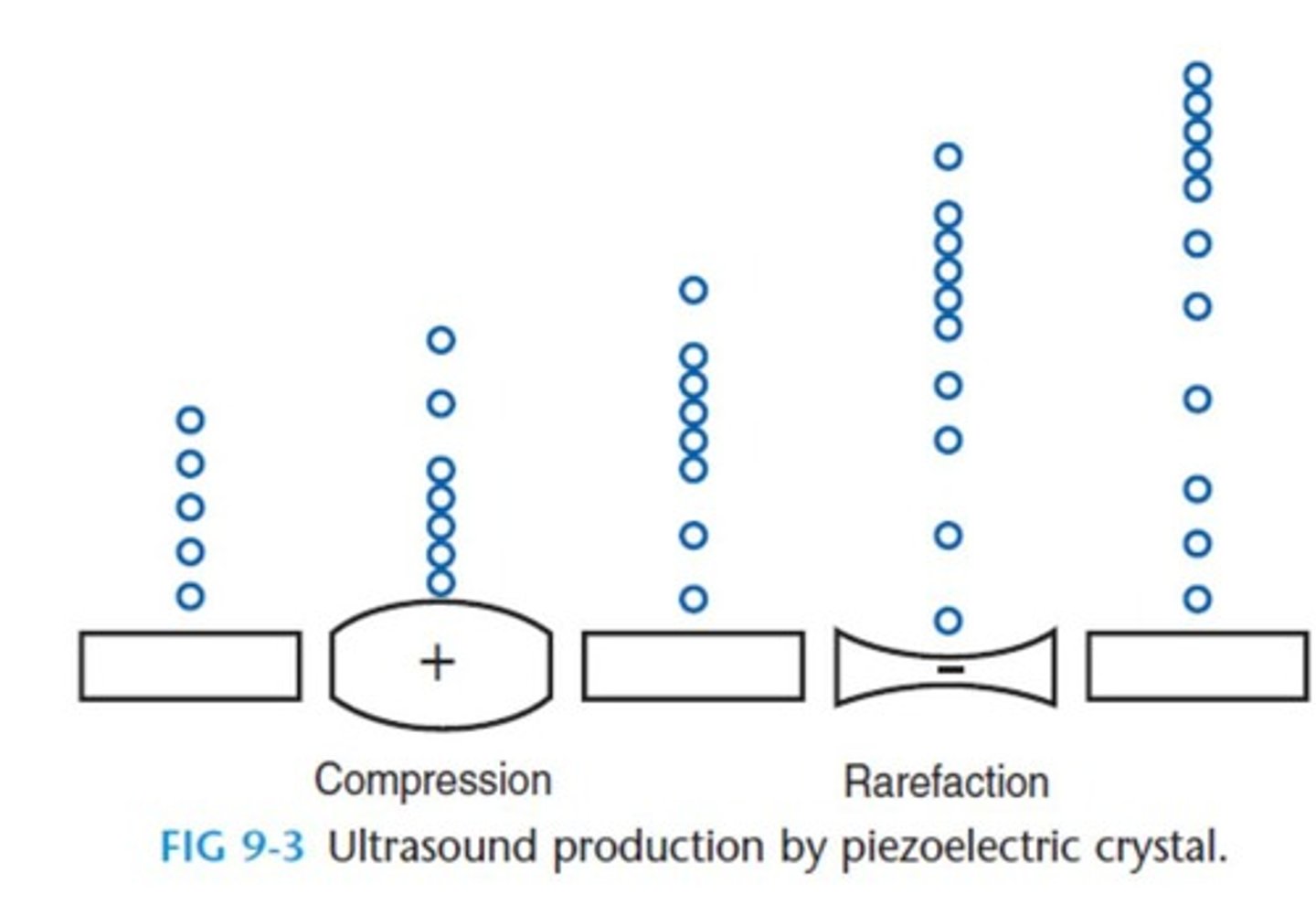
Compression Phase
Phase where sound waves compress material.
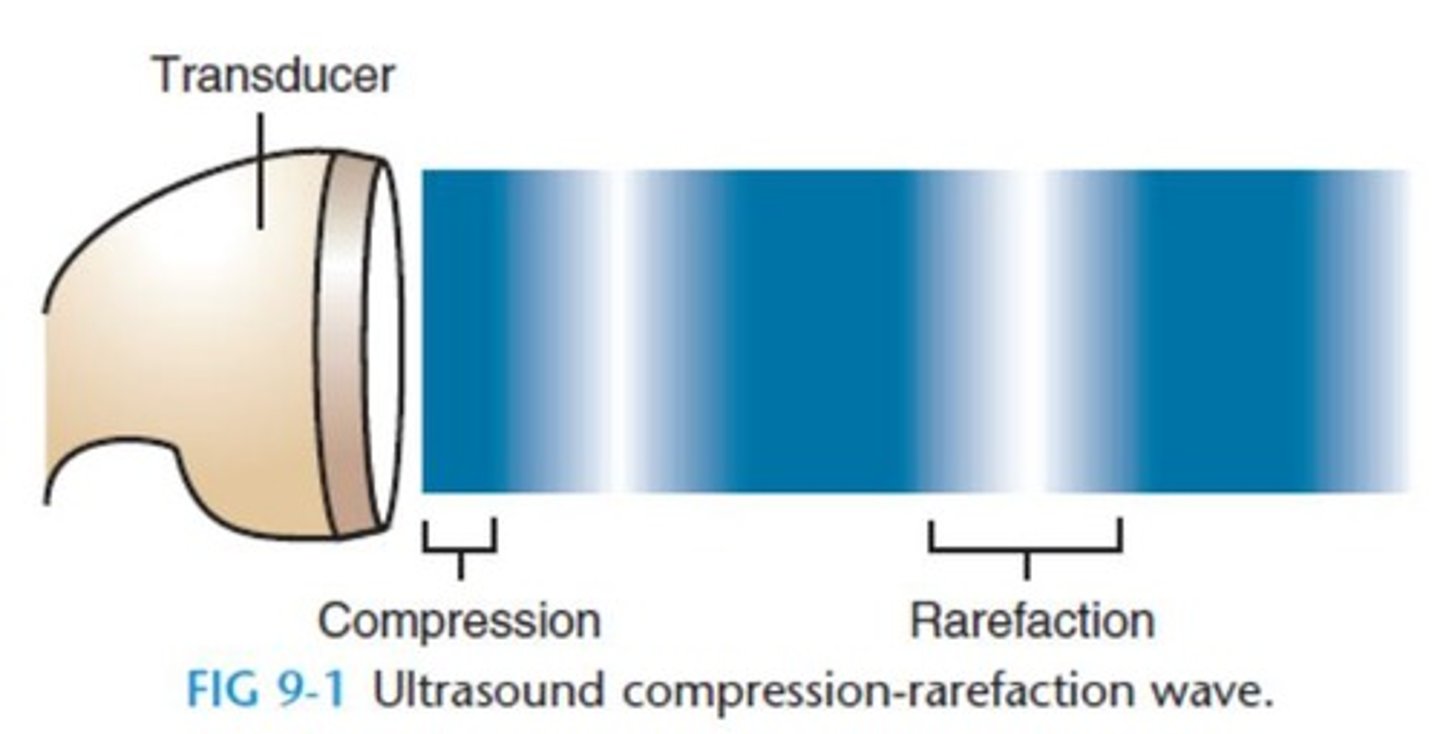
Rarefaction Phase
Phase where sound waves expand material.
Cyclic Compression-Rarefaction
Cycles per second measured in hertz (Hz).
Therapeutic US Frequency Range
1 to 3 million cycles per second (1 to 3 mHz).
Depth of Penetration
Increases with lower frequency ultrasound.
Concentration of Energy
Higher frequency ultrasound concentrates energy superficially.
Cell Membrane Permeability
Altered by nonthermal effects of ultrasound.
Transducer
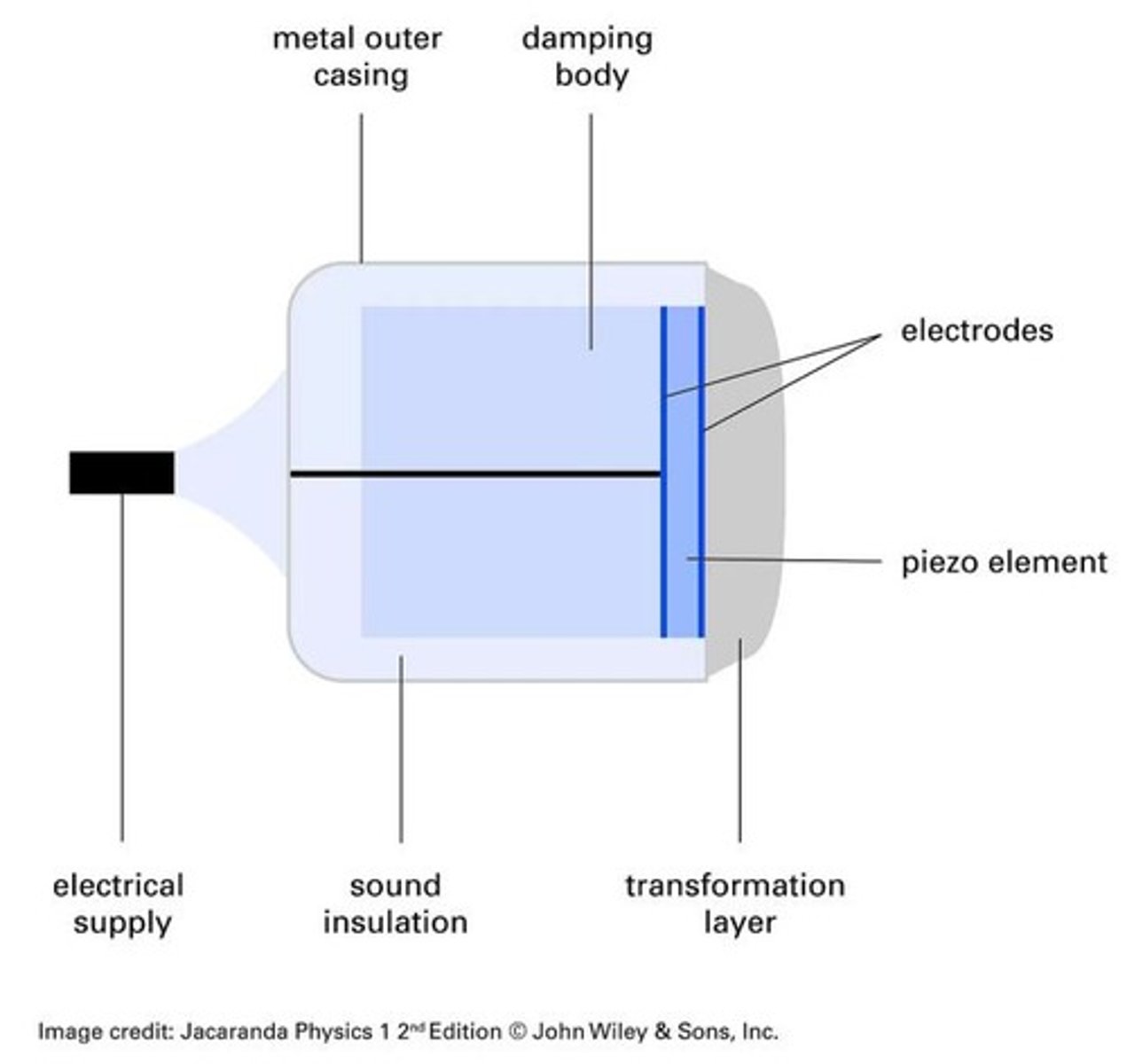
Device converting electrical energy to ultrasound waves.
Beam Nonuniformity Ratio (BNR)
Maximum spatial peak intensity to spatial average intensity.
Spatial Average Intensity
Average power per unit area in W/cm².
Spatial Peak Intensity
Maximum intensity within the ultrasound field.
WHO Intensity Limit
Therapeutic ultrasound output limited to 3 W/cm².
Attenuation
Reduction of ultrasound intensity in tissues.
Absorption
Conversion of ultrasound energy into heat in tissues.
Reflection
Redirection of ultrasound beam at tissue interfaces.
Refraction
Change in ultrasound wave direction at an interface.
Attenuation Coefficients
Tissue-specific and frequency-specific measures of attenuation.
Continuous Ultrasound
Steady release of ultrasound energy during treatment.
Pulsed Ultrasound
Intermittent release of ultrasound energy for nonthermal effects.
Piezoelectric Materials
Materials that convert electrical energy to ultrasound.
Natural Quartz
Common piezoelectric material for thermal ultrasound effects.
Synthetic PZT
Efficient piezoelectric material used in ultrasound transducers.
Barium Titanate
Less costly piezoelectric material for ultrasound applications.
Near Field
Region where ultrasound beam converges.
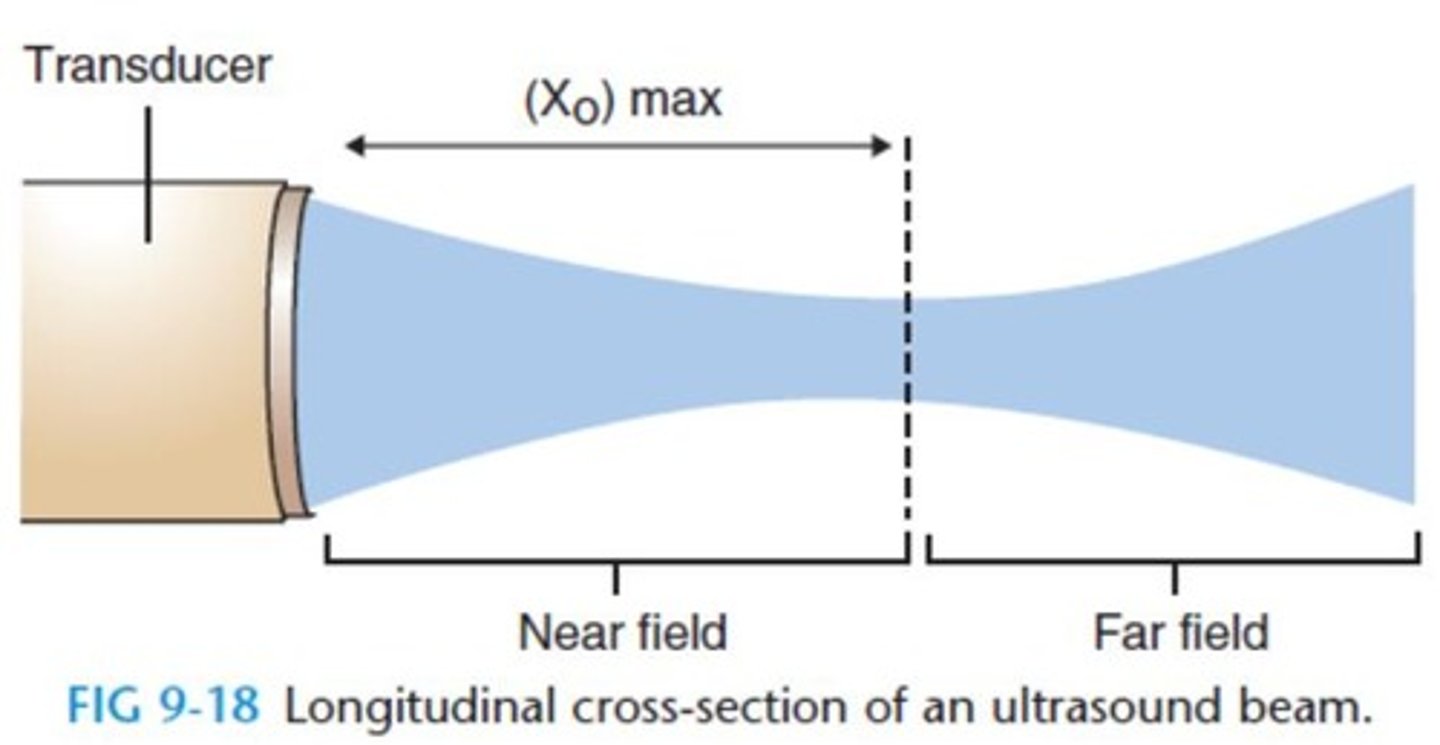
Far Field
Region where ultrasound beam diverges.
Fresnel Zone
Another term for the near field of ultrasound.
Fraunhofer Zone
Another term for the far field of ultrasound.
Intensity Variations
Changes in ultrasound intensity due to refraction.
Generation of Ultrasound
Produced by high-frequency alternating current to crystal.
Cooling Conduction Medium
Decreases heating rate during ultrasound application.
Thermal Effects of Ultrasound
Includes pain reduction and increased metabolic rate.
HMP Temperature Increase
Heating medium to 25°C enhances heating rate.
Soft Tissue-Bone Reflection
35% reflection at soft tissue-bone interfaces.
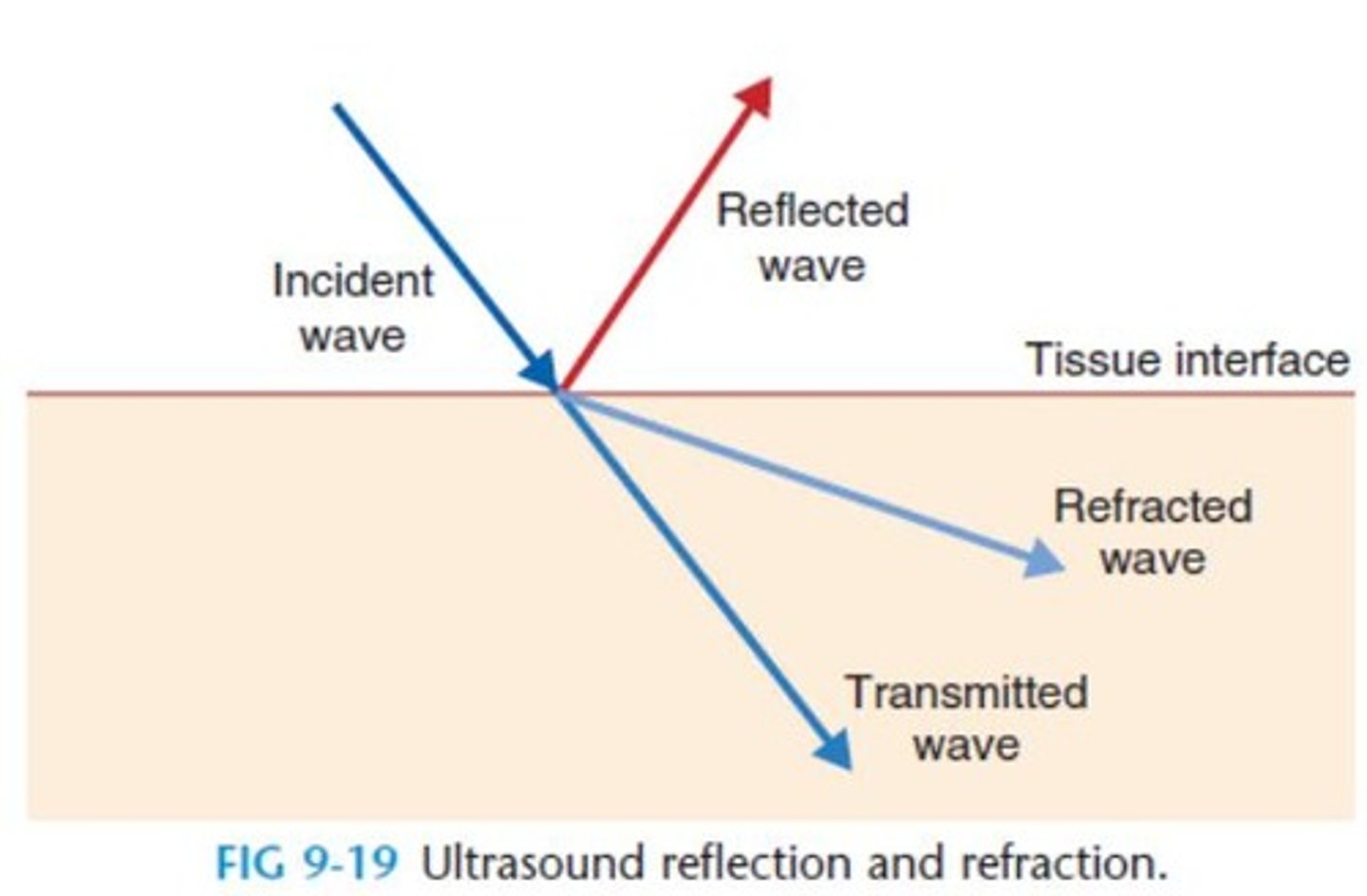
Air-Skin Reflection
100% reflection at air-skin interface.
Superficial tissues
Increase in superficial tissue temperature and circulation.
Nerve conduction velocity
Alteration due to ultrasound application.
Soft tissue extensibility
Increased flexibility of soft tissues with ultrasound.
Nonthermal effects of US
Effects of ultrasound without significant temperature increase.
Pulsed US
20% duty cycle; no measurable temperature increase.
High absorption coefficient
Tissues that absorb ultrasound energy effectively.
Low absorption coefficient
Tissues that absorb ultrasound energy poorly.
Intracellular calcium levels
Increased by low-intensity ultrasound application.
Cell membrane permeability
Enhanced permeability of skin and cell membranes.
Mast cell degeneration
Increased release of histamine and chemotactic factors.
Macrophage responsiveness
Promoted by ultrasound, aiding in healing.
Protein synthesis
Increased rate by fibroblast and tendon cells.
Proteoglycan synthesis
Stimulated by ultrasound in chondrocytes.
Scar tissue
Increased collagen content in healing muscle.
Nutrient delivery
Enhanced by ultrasound for healing processes.
Inflammatory phase
Effective treatment during this phase of repair.
Absorption coefficient
Proportional to tissue type for ultrasound application.
Frequency
Higher frequency increases temperature in tissues.
Pain control
1-3 MHz frequency used for pain management.
Average intensity
Higher intensity leads to increased tissue temperature.
Phonophoresis
Ultrasound with medication delivery, specific parameters.
Soft tissue extensibility parameters
0.5-1.0 W/cm2 at 3 MHz for extensibility.
Healing rate
Increased by specific ultrasound application protocols.
Dermal ulcer treatment
0.5-0.8 W/cm2, pulsed for 3-5 minutes.
Ligament treatment
Low-dose pulsed ultrasound at 0.5-1.0 W/cm2.
Bone fracture treatment
Very low dose, 1.5 MHz, 0.15 W/cm2.
Contraindications
Conditions where ultrasound should not be applied.
Adverse effects
Rare but possible with incorrect ultrasound application.
Burn risk
High-intensity continuous ultrasound may cause burns.
Pregnancy risks
Maternal hyperthermia linked to fetal abnormalities.
US head movement
Always move to reduce burn risk during treatment.
Breast implants
High-dose ultrasound contraindicated over breast implants.
Thermal Level Ultrasound
Avoid on impaired circulation and sensation areas.
Superficial Bone
Reduce intensity when treating near superficial bone.
CNS Tissue
US may damage CNS, usually protected by bone.
Blood Cell Stasis
US standing waves can cause blood cell stasis.
Laminectomy Precaution
Avoid US over or near laminectomy sites.
Methylmethacrylate Cement
Used in fixation or prosthetic joints.
Endothelial Damage
US can damage endothelial lining of blood vessels.
Cemented Prosthesis
Avoid US over cemented prosthesis areas.
US Transducer Movement
Move transducer throughout treatment application.
Metal Implants
US can be applied over metal implants safely.
Pacemaker Risks
US may heat and interfere with pacemaker circuitry.
US Frequency Selection
Based on tissue depth for effective treatment.
Reproductive Organs
US may affect gamete development; avoid these areas.
1 MHz Frequency
Used for tissues up to 5 cm deep.
3 MHz Frequency
Used for tissues 1-2 cm deep.