L4 - Gastric Reservoir
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
The relaxation of the gastric reservoir is mainly regulated by ________
reflexes
3 types of gastric relaxation
receptive, adaptive and feedback-relaxation
All 3 types of gastric relaxation involve sending signals to where
The vagus centre of the brain
What triggers receptive gastric relaxation
Mechanical stimuli in the pharynx
How does receptive gastric relaxation work
Triggered by mechanical stimuli in the pharynx (e.g., swallowing).
Signals are sent to the vagus centre in the brain.
This initiates vagal-mediated inhibition, leading to the relaxation of the gastric reservoir in preparation for incoming food.
What triggers adaptive gastric relaxation
Triggered by gastric distension (stretching) due to food intake.
How does adaptive gastric relaxation work
Triggered by gastric distension (stretching) due to food intake.
Tension receptors in the stomach detect distension and send signals to the vagus centre.
The vagus nerve activates inhibitory vagal fibres, which release non-adrenergic, non-cholinergic (NANC) neurotransmitters like NO (nitric oxide) and VIP (vasoactive intestinal peptide).
This leads to the relaxation of the proximal stomach, allowing it to accommodate more food.
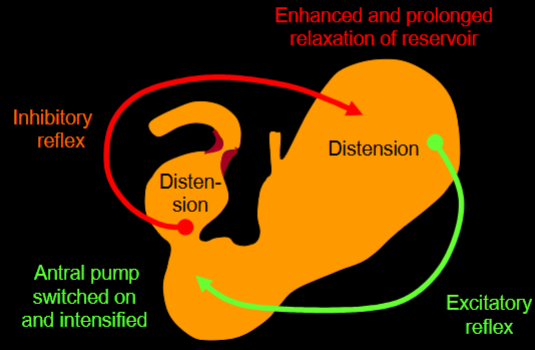
What triggers feedback gastric relaxation
Triggered by nutrients in the small intestine.
How does feedback gastric relaxation work
Triggered by nutrients in the small intestine.
Signals are sent back to the stomach via neural and hormonal pathways.
This feedback mechanism helps modulate gastric emptying by further relaxing the stomach to prevent rapid entry of food into the small intestine.
It causes enhanced relaxation of the gastric reservoir, inhibition of the antral pump, and reduced opening of the pyloric sphincter
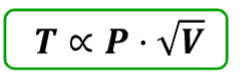
How do tension in the wall of the stomach, internal pressure of the stomach & the distending volume relate to each other
Tension developed circumferentially in the wall (T) is proportional to the internal pressure (P) multiplied by the square root of the distending volume (√V).
If either V or P increase, T also increases
What do some pufferfish have that can cause poisoning
TTX (tetrodotoxin)
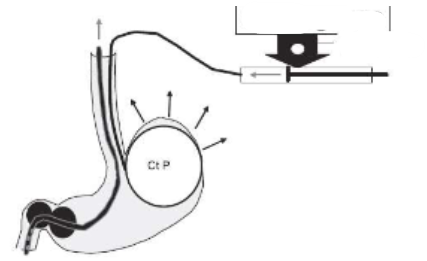
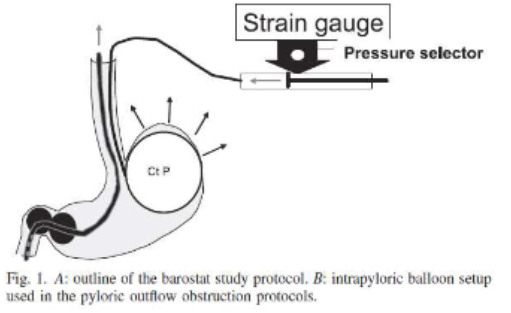
What is this setup used for
An Intragastric Balloon (Ct P) is placed inside the stomach, usually in the proximal region. It expands in response to pressure changes, mimicking food intake. Measures stomach compliance (the ability to stretch and accommodate).
A strain gauge measures pressure changes within the balloon.
The pressure selector ensures controlled inflation and deflation of the balloon.
The 2 balloons setup (1 before & 1 after the sphincter) may be used to simulate conditions like delayed gastric emptying. By inflating the balloons near the pylorus, it can artificially create pyloric obstruction, allowing researchers to study gastric motility disorders and accommodation responses
Can sham feeding have an effect on gastric accommodation
Yes
(sham feeding = chewing food but not swallowing)
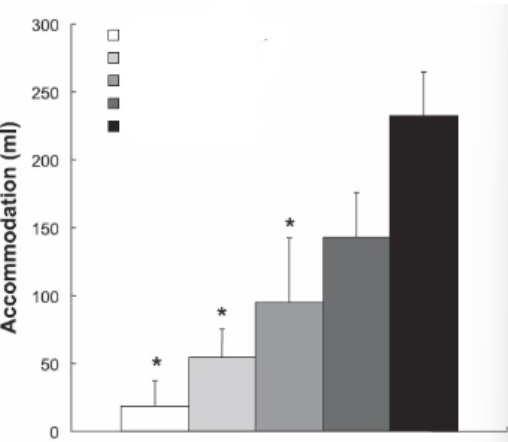
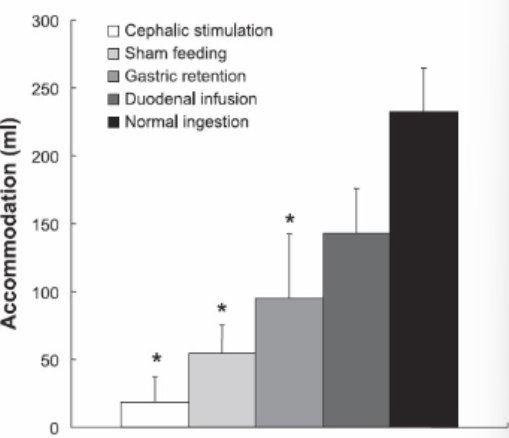
What could each of these columns of increasing gastric accommodation reflex represent
Name of sphincter at entrance to stomach
Lower oesophageal sphincter
Name of sphincter at exit from stomach
Pyloric
True/False: Each wave cycle of the stomach results in only a small amount of material into the duodenum
True
How can gastric emptying affect insulin secretion
Faster emptying leads to faster glucose absorption, triggering higher insulin release to manage blood sugar levels
Why is gastric motility important in clinical settings
Plays a crucial role in glucose metabolism, diabetes management & drug absorption
is faster/slower gastric emptying beneficial for T2Ds
Faster gastric emptying is often seen in early Type 2 diabetes and contributes to postprandial hyperglycaemia.
Medications are used to slow gastric emptying to reduce glucose spikes.
3 anatomical regions of the stomach
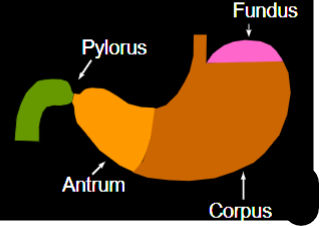
2 functional regions of the stomach
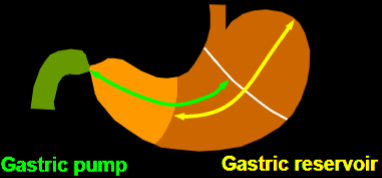
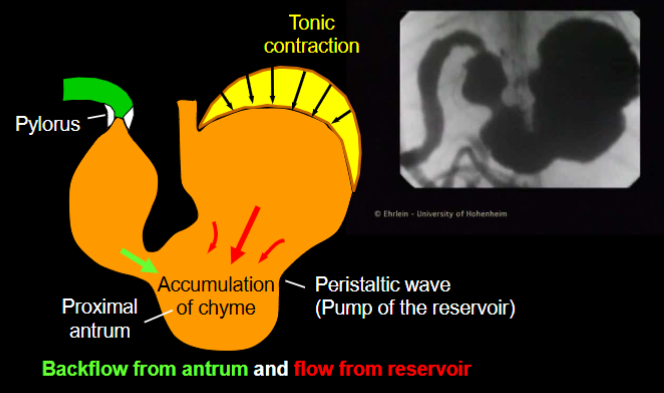
Difference in contractions between the 2 different functional regions of the stomach
Tonic contractions: Sustained contractions that last for minutes to hours that maintain compartmentalization and regulate movement between sections.
Phasic contractions: Rhythmic, short-duration contractions that mix and propel contents through the GI tract
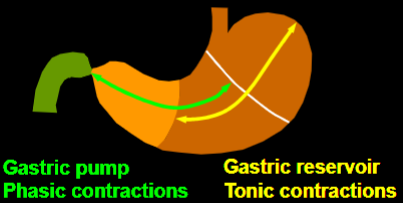
The transport of digesta from the gastric reservoir into the antral pump is caused by two mechanisms, what are they
tonic contractions and peristaltic waves in the region of the gastric corpus
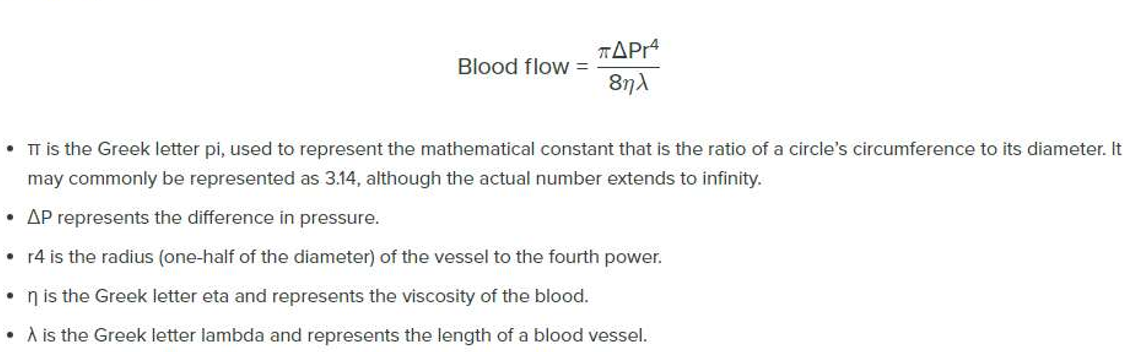
Who’s formula is this & what does it tell us
Poiseuille’s equation
it helps explain how fluids (such as gastric contents, bile, pancreatic secretions, and blood in the GI vasculature) move through tubular structures like the esophagus, intestines, and blood vessels.
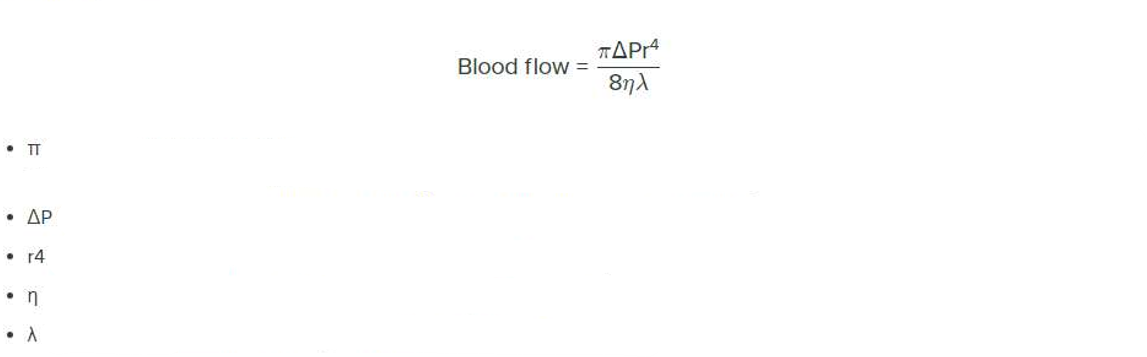
What does each value in Poiseuille’s equation mean
Replace blood with chyme
Blood flow → Flow rate of chyme through the pylorus
ΔP = Pressure gradient between the antrum and duodenum
r = Radius of the pyloric sphincter (to the 4th power effect!)
η = Viscosity of chyme
L (λ) = Length of the pyloric sphincter
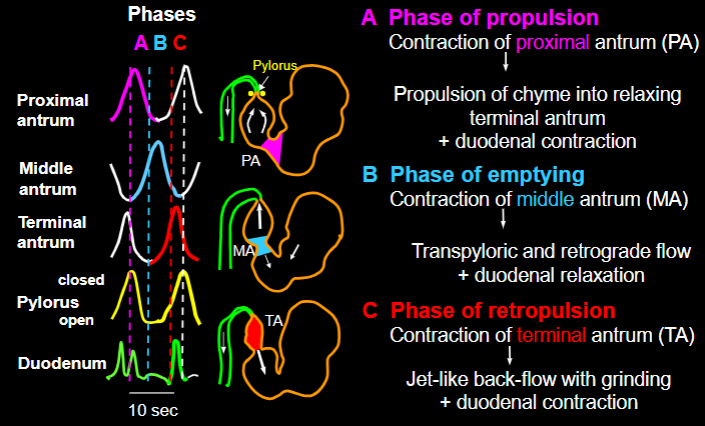
The function of the gastric pump can be differentiated into three phases ………
A: phase of propulsion,
B: phase of emptying,
C: phase of retropulsion and grinding
How do each of the 3 phases of gastric pump work
In the propulsion phase the duodenum contracts to temporarily resist the incoming chyme from the stomach and to regulate how much is accepted.
How does the sieving function of the stomach work
Liquids and small particles leave the stomach more rapidly than large particles.
This discrimination is called “sieving function“
What materials are moved in each of the phases of the gastric pump
“sieving effect”
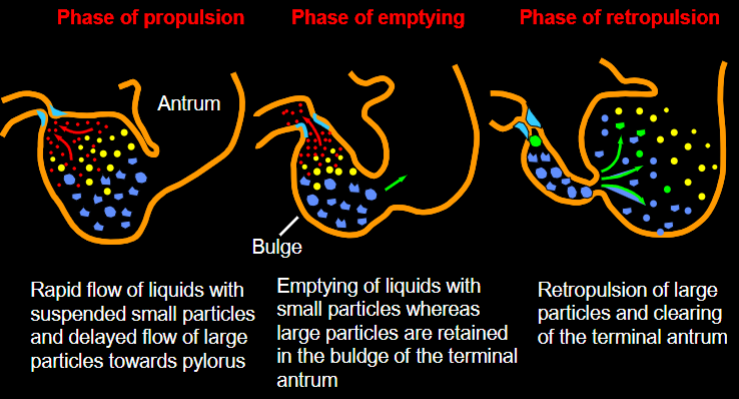
Grinding of solid particles is caused by what
forceful jet-like retropulsion through the small orifice of the terminal antral contraction
How do contractions of the proximal duodenum & gastric emptying coordinate
Antro-duodenal co-ordination: Contractions of the proximal duodenum cease during the phases of gastric emptying.
(contraction of the terminal antrum & pylorus happen together to push food back into the stomach)
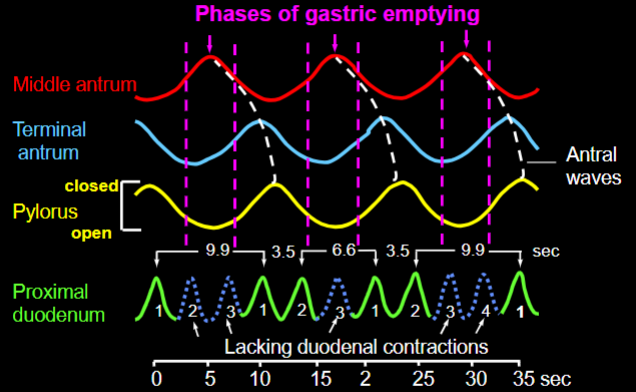
How can the duodenum contract three to four times during an antral wave
Because of different frequencies between antral and duodenal contractions, the duodenum can contract three to four times during an antral wave
Regulation of gastric emptying depends on what
Balance between gastric reservoir and antral pump
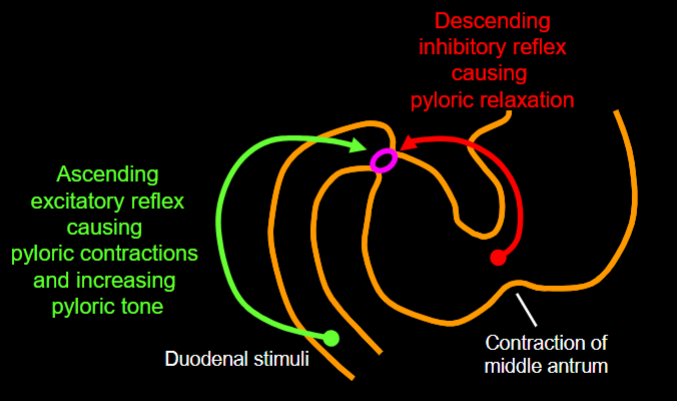
Pyloric activity is modulated by what reflexes
antral inhibitory and duodenal excitatory reflexes
What causes rapid gastric & duodenal emptying
Rapid emptying is caused by tonic contractions of the reservoir (1a), deep peristaltic waves along the gastric body (1b), deep constrictions of the antral waves (2), a wide opening of the pylorus (3), a duodenal receptive relaxation (4) and peristaltic duodenal contractions (5).
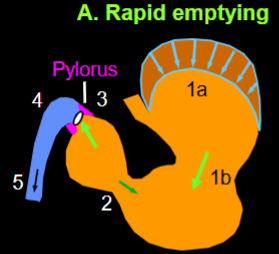
What causes delayed gastric & duodenal emptying
Delayed emptying due to feedback inhibition is caused by a prolonged relaxation of the reservoir (6a), shallow peristaltic waves along the gastric body ( 6b), shallow antral waves (7), a small pyloric opening (8), a lacking duodenal relaxation (9) and segmenting duodenal contractions (10).
How do liquids empty from the stomach
Liquids empty exponentially, meaning a large volume empties early, then slows over time.
Liquids empty exponentially because they do not require grinding and pass through the pylorus based on a pressure gradient between the stomach and duodenum.
Do solids empty from the stomach at the same rate as liquids
No, solids have a lag phase before emptying begins
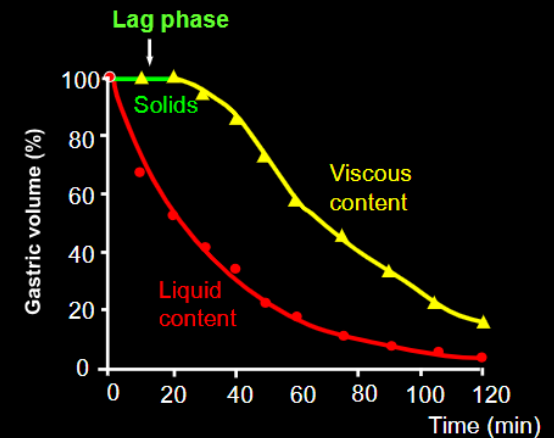
What happens during the lag phase of solid emptying from the stomach
The antrum grinds food into small particles (~1-2 mm) before they can pass through the pylorus
How does gastric emptying of solids occur after the lag phase
Once the solid is sufficiently broken down, the viscous chyme empties in a linear fashion (a fixed amount per unit time
Difference in force of antral contractions with a non-caloric meal & a nutrient meal
A nutrient meal reduces the force of antral contractions.
(Prevents overloading the duodenum with too much nutrient-rich chyme at once)
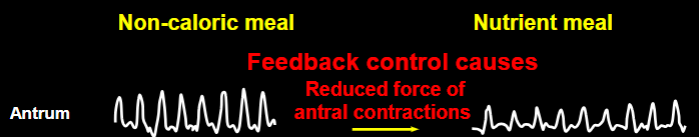
How does pyloric opening change after a nutrient meal compared to a non-caloric meal
A nutrient meal reduces pyloric opening
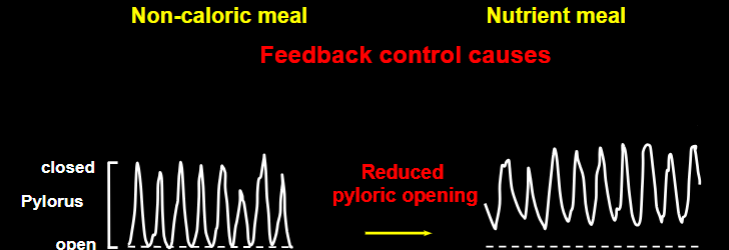
How does peristalsis in the duodenal bulb change after a nutrient meal compared to a non-caloric meal
A nutrient meal reduces peristaltic waves in the duodenal bulb.
How does segmental activity in the middle duodenum change after a nutrient meal compared to a non-caloric meal
A nutrient meal enhances segmenting activity in the middle duodenum.
(segmenting activity is for mixing - not like peristalsis which is for movement along the tract)(we would need more segmenting activity for a nutrient meal to make sure we get all of the nutrients out)


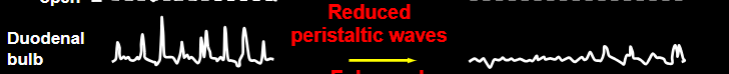
What does this image represent
gastric emptying scintigraphy images at different time points (0 to 240 minutes), tracking the movement of a radiolabeled meal through the stomach.
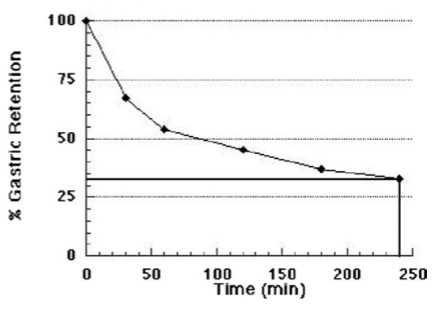
What does this graph depict
The graph shows the percentage of gastric retention over time, demonstrating the rate of gastric emptying.
What condition is commonly diagnosed by scintigraphy images and tracking gastric retention
Gastroparesis, a condition where the stomach empties slower than normal without an obstruction.
What is the clinical significance of having more than 10% gastric retention at 240 minutes?
It suggests delayed gastric emptying, which is a diagnostic criterion for gastroparesis.
what is a 13CO2 breath test used for
A non-invasive diagnostic test used to assess various metabolic and gastrointestinal conditions. It works by measuring the amount of ¹³C-labeled carbon dioxide in a person’s breath after they ingest a substrate (a substance labeled with the stable carbon-13 isotope). The breakdown and absorption of this substrate release ¹³CO₂, which is then exhaled and measured.
Used to detect Helicobacter pylori, a bacterium associated with ulcers and gastritis. The patient ingests ¹³C-urea, and if H. pylori is present, it breaks down the urea, releasing ¹³CO₂ in the breath.
Assesses how quickly the stomach empties by tracking the breakdown of ¹³C-labeled octanoic acid or ¹³C-labeled spirulina.
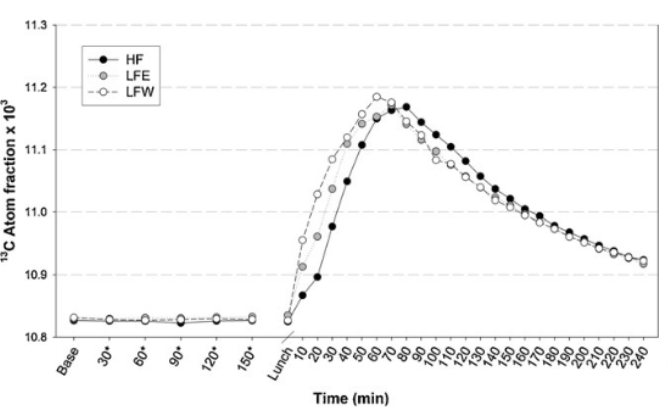
Interpret this graph
This graph represents the results of a ¹³C-CO₂ breath test over time, measuring the ¹³C atom fraction (×10³) in exhaled breath after a labeled meal.
The Y axis represents the concentration of ¹³C-labeled CO₂ in the breath, indicating how much of the ingested ¹³C-labeled substrate has been metabolized and exhaled.
Different Test Conditions (HF, LFE, LFW)
HF (High-Fat, black circles)
Shows a slower rise but maintains a higher peak for a longer duration.
LFE (Low-Fat, Energy-Matched, gray circles)
Peaks faster than HF but declines slightly quicker.
LFW (Low-Fat, Weight-Matched, open circles)
Has the fastest rise to peak and also declines the quickest.
Before the meal (baseline), all three groups have similar low ¹³C levels.
After eating the labeled meal, the ¹³C fraction rapidly increases, reaching a peak around 60-90 minutes post-meal.
The different meal compositions affect the rate of metabolism and CO₂ excretion, with low-fat meals (LFE, LFW) being metabolized faster than high-fat meals (HF).
HF has a delayed response but sustains higher levels longer, suggesting slower digestion and metabolism of the labeled substrate.
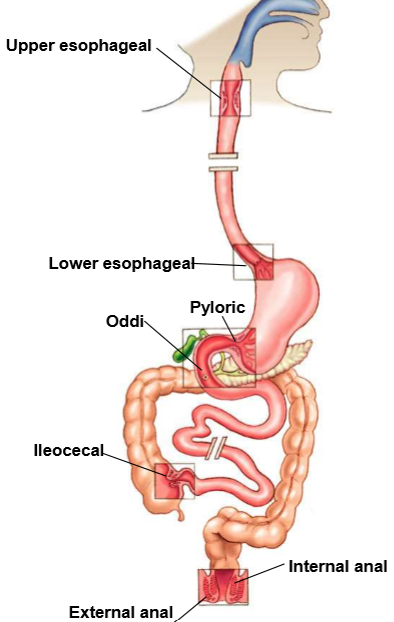
Name all the sphincters of the GI tract
What prevents duodeno-gastric reflux
pyloric sphincter
Effect of duodenal stimuli like oleic acid on antral contractions, duodenal contractions, pyloric tone & pyloric contractions
inhibit antral contractions
evoke duodenal contractions
increase pyloric tone
elicit frequent pyloric contractions
Gastric motility is mostly
Peristaltic waves
glucose disposal rate (how quickly glucose is cleared from the blood) is influenced by two main factors - what are they
65% is due to insulin muscle mass
35% is due to gastric emptying
Why do we regulate gastric emptying
to prevent infection, for absorption & digestion